Measles
rubeolaSession objectives
• Signs and symptoms• Diagnosis
• Complications
• Epidemiology (Agent, Occurrence, Reservoir, Mode of transmission, Period of communicability, Susceptibility and resistance )
• Methods of control(Preventive measures & Control of pt, contacts & Epidemic measures)
Measles is an endemic disease, meaning that it has been continually present in a community.
The first scientific description of measles and its distinction from smallpox and chickenpox is credited to the Persian physician, Muhammad ibn Zakariya ar-Razi (860-932), known to the West as "Rhazes", who published a book entitled The Book of Smallpox and Measles (in Arabic: Kitab fi al-jadari wa-al-hasbah).
An alternative name for measles in English-speaking countries is rubeola, which is sometimes confused with rubella (German measles)
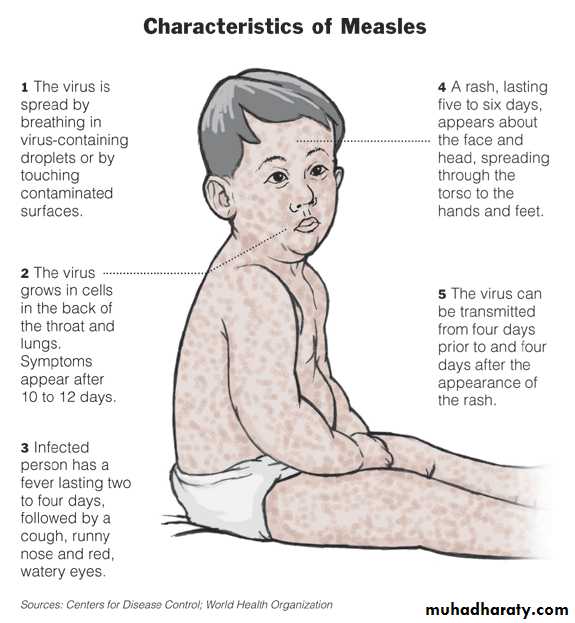
• Prodromal stage (take 3-7days): fever, the three Cs—cough, coryza (runny nose) and conjunctivitis (red eyes). Koplik's spots seen inside the mouth are pathognomonic (diagnostic) for measles but are not often seen, (1-2 days before rash).
Clinically characterized by 3 stages:
• eruptive or rash stage (a generalized, maculopapular, erythematous rash that begins several days after the fever starts. It starts on the head before spreading to cover most of the body, often causing itching. The rash is said to "stain", changing colour from red to dark brown, before disappearing).
• Post measles stage; child have loss of wt. & remain weak for several days.
• Diagnosis:
• Clinical & epidemiological• Leukopenia, specific measles IgM antibodies, isolation of virus by cell culture.
• Severe cases occur in:
• 1) infant
• 2) adults
• 3) malnourished children
• Associated (Hemorrhagic rash, protein-losing enteropathy, blindness, dehydration & sever skin infections).
• Complications:
• ranging from relatively mild and less serious diarrhea, to pneumonia and encephalitis (subacute sclerosing panencephalitis), corneal ulceration leading to corneal scarring. Complications are usually more severe amongst adults who catch the virus.CFR: 3-5% in developing countries,
< 0.2 per 10’000 cases in developed countries.10-30% in very poor countries,
Agent:
Measles virus, a member of the genus Morbilli-virus of the family paramyxoviridae.
Occurrence:
1. In temperate climates, late winter and early spring. In tropical climate mainly in dry season.
2. pre-vaccine era 90% 0f people by age of 20, endemic disease and attained epidemic every 2-3 years with a high CFR.
• 3. Effect of active immunization program on measles epidemiology:
• a. Epidemics widely spaced.• b. Worldwide incidence decreased.
• c. Overall CFR dropped.
• d. Despite that, measles remains the leading vaccine preventable killer of children worldwide because:
• Failure of sero-conversion after one dose.
• Age of vaccination; 9 months still there is passive maternal immunity that interfere with formation of active immunity.
• Immunity degradation .
• Improperly handled or stored vaccine (freeze dried vaccine)
Reservoir : human
IP: 10-14 days.Mode of transmission:
Direct contact with throat and nasal secretions.Air borne
Soiled articles with secretions.
Period of communicability:
It is highly communicable infectious disease, 4 days before rash onset (prodromal stage) to 4 days after the rash appearance.
Susceptibility and resistance:
All persons who have not had the disease & and not immunized.lifelong acquired immunity after illness.
long lasting Immunity after vaccination (2doses).
Passive maternal immunity for 6-9 months or beyond
Maternal anti body interferes with response to vaccine:
Vaccine efficacy at 9 ms is 85%.Vaccine efficacy at 12-15 ms induced immunity in 94-98% of recipients.
Reimmunization 99%.
Children born to mothers with vaccine induced immunity receive less passive antibody.
• Methods of control
• Preventive measures:• 1. public health education.
• 2. immunization: by a single dose of live attenuated measles vaccine (SC, 0.5ml), recommends dose at 9 ms age (in developing countries) another single dose measles vaccine combined with mumps & rubella (MMR) administered at age of 15 months may increase immunity level up to 99%.
• in measles outbreak at 6 ms. a second dose should be administered as soon as possible.
• Side effects of measles vaccine:
• Mild measles illness, fever& rash,(15-20%) after 5-10 days.
• Febrile convulsion.
• Encephalitis & encephalopathy occur in 1/million doses.
• TSS
• Contraindications of live virus vaccine:
• Immunocompromised pt.( T-cell dysfunction, Bd diseases, malignancies, use corticosteroid, antimetabolites therapy, irradiation). HIV?• Pt with sever acute illness with or without fever (mild illness?).
• Anaphylactic hypersensitivity.
• Pregnant women, and the women should advised not to become pregnant 1 month after receiving vaccine.
B) Control of pt, contacts:
1. reporting; obligatory.2. isolation; in hospital, respiratory isolation, and cases should be excluded from school to the 5th day of rash appearance.
3. concurrent disinfection
4. quarantine; usually impractical , quarantine of institutions or wards can sometimes be of value.
5. immunization of contacts; vaccines within 72 hrs of exposure.
IG (0.25 ml/Kg)- within 3-6 days of exposure.
For: imunocompromised persons (0.5ml/Kg), pregnant women and where the measles vaccine is contraindicated.
6. Investigation of contacts; searching and immunize exposed contacts.
• 7. Specific Rx; none.
• but management steps includes:
• 1) supplementary Rx.
• 2) additional nutritional support.
• 3) promote BF
• 4) giving Vit. A which is recommended in the following situations;
• » areas where measles CFR>1%, where?.
• » areas of known Vit. A deficiency.
• » in all cases of severe complicated measles.
Vit. A supplementation have the following advantages:
1. replaces body reserves of Vit. A.2. Prevents blindness due to corneal ulceration and keratomalacia
3. Significantly reduces measles fatality.
The following Vit. A schedule is recommended:
infant<6 ms → 50 000 IUinfant 6-11ms → 100 000 IU
12 ms + → 200 000 IU
* Vit. A given in 2 doses , 1st dose given immediately, the 2nd dose in the next day. 3rd dose can be given 2-4 wks later if the child has any sign of (night blindness, corneal dryness, clouding, ulceration).
• Epidemic measures:
• Prompt reporting (within 24 hrs) even of suspected cases.
• comprehensive immunization programs for all susceptible.
• In institutional outbreaks, new admissions should receive vaccine or IG