The normal menstrual cycle
The external manifestation of a normal menstrual cycle is the presence of regular vaginal bleeding. This occurs as a result of the shedding of the endometrial lining following failure of fertilization of the oocyte or failure of implantation. The term menstrual cycle (m.c), since menstruation is the obvious monthly event during reproductive life, the normal m.c is mostly a reflection of hypothalamo- pituitary- ovarian axis (HPO).Hypothalamus:
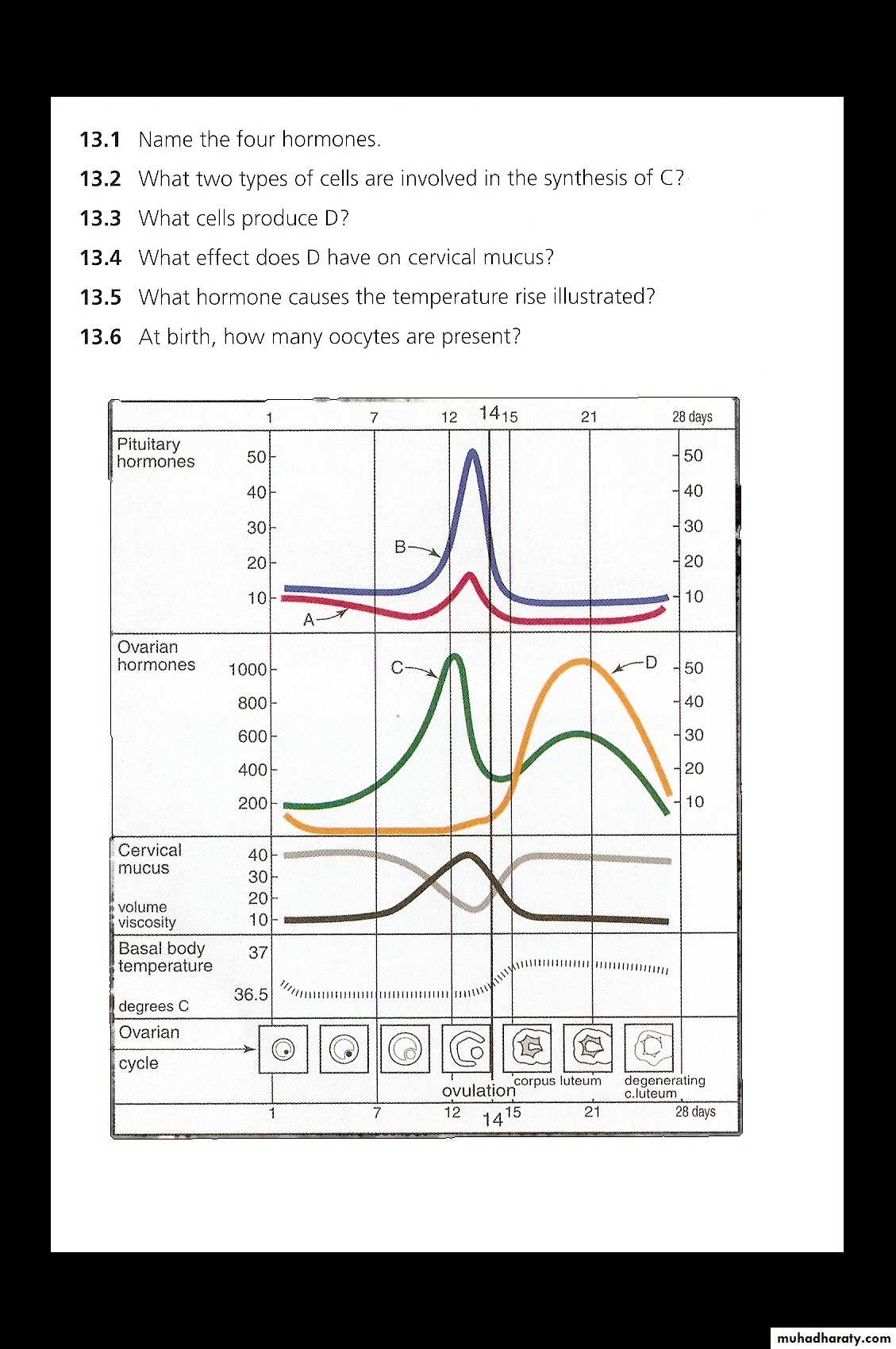
The hypothalamus in the forebrain secretes the peptide hormone gonadotrophin-releasing hormone (GnRH), which in turn controls pituitary hormone secretion. GnRH must be released in a pulsatile fashion to stimulate pituitary secretion of luteinizing hormone (LH) and follicle stimulating hormone (FSH). When GnRH administered continuously, they will downregulate the pituitary and consequently decrease LH and FSH secretion.
Pituitary gland:
GnRH stimulate of the basophile cells in the anterior pituitary gland causes synthesis and release of the gonadotrophic hormones, FSH and LH. This process is modulated by the ovarian sex steroid hormones oestrogen and progesterone. Low levels of oestrogen have an inhibitory effect on LH production (negative feedback), whereas high levels will increase LH production (positive feedback). The mechanism of action for the positive feedback effect of oestrogen involves an increase in GnRH receptor concentrations, while mechanism of negative feedback effect is uncertain. The high levels of circulating oestrogen in the late follicular phase of the ovary act via the positive feedback mechanism to generate a periovulatory LH surge from the pituitary.
Unlike oestrogen, low levels of progesterone have a positive feedback effect on pituitary LH and FSH secretion ( as seen immediately prior to ovulation) and contribute to the FSH surge. High levels of progesterone, as seen in the luteal phase, inhibit pituitary LH and FSH production. Positive feedback effects of progesterone occur via increasing sensitivity to GnRH in the pituitary. Negative feedback effects are generated through both decreased GnRH production from hypothalamus and decreased sensitivity to GnRH in the pituitary. It is known that progesterone can only have these effects on gonadotropic hormone release after priming by oestrogen.
In addition to these well-known hormones, there are other hormones which are involved in pituitary gonadotrophin secretion. Inhibin and activin are peptide hormones produced by granulosa cells in the ovaries, with opposing effects on gonadotrophin production. Inhibin inhibits pituitary FSH secretion, whereas activin stimulates it.
Ovary:
With the onset of menarche, the primordial follicles containing oocytes will activate and grow in a cyclical fashion, causing ovulation and subsequent menstruation in the event of non-fertilization.
In the course of a normal m.c, the ovary will go through three phases:
1.Follicular phase
2.Ovulation.
3.Luteal phase.
Follicular phase:
At birth, the human ovaries contain approximately 1 million primordial follicles, arrested at prophase of the first meiotic division. Of the original pool of 1 million primordial follicles, only about 400 will ever acquire gonadotrophin receptors and the possibility of ovulation. This dramatic attrition defines the female arm of natural selection, mirrored by the huge wastage of spermatogenesis in the male, in which millions of sperm are produced each day during fertile life, with only a tiny proportion ever fertilizing an oocyte. The initial stages of follicular development are independent of hormone stimulation.
FSH levels rise in the first days of the menstrual cycle, when oestrogen, progesterone and inhibin levels are low. This stimulates a cohort of small antral follicles on the ovaries to grow. Within the follicles, there are two cell types which are involved in the processing of steroids, including oestrogen and progesterone. These are the theca and the granulosa cells, which respond to LH and FSH stimulation, respectively. LH stimulates production of androgens from cholesterol within theca cells. These androgens are converted into oestrogen by the process of aromatization in granulosa cells, under the influence of FSH. As the follicles grow and oestrogen secretion increase, there is negative feedback on the pituitary to decrease FSH secretion. This assists in the selection of one follicle to continue in its development towards ovulation – the dominant follicle. In the ovary, the follicle which has the most efficient aromatase activity and highest concentration of FSH- induced LH receptors will be the most likely to survive as FSH levels drop, while smaller follicles will undergo atresia. The dominant follicle will go on producing oestrogen and also inhibin, which enhances androgen synthesis under LH control. There are other mediators playing a role in the follicular phase of the menstrual cycle. These include inhibin and activin. Inhibin is secreted by the granulosa cells within the ovaries. It participates in feedback to the pituitary to downregulate FSH release, and also appears to enhance ongoing androgen synthesis. Activin is structurally similar to inhibin, but has an opposite action. It is produced in granulosa cells and in pituitary, and acts to increase FSH binding on the follicles.
Ovulation:
By the end of the follicular phase, which lasts an average of 14 days, the dominant follicle has grown to approximately 20 mm in diameter. As the follicle matures, FSH induces LH receptors on granulosa cells to compensate for lower FSH levels and prepare for signal for ovulation. Production of oestrogen increase until they reach the necessary threshold to exert a positive feedback effort on the hypothalamus and pituitary to cause the LH surge. This occurs over 24 – 36 hours, during which time the LH-induced luteinization of granulosa cells in the dominant follicle causes progesterone to be produced, adding further to the positive feedback for LH secretion and causing a small periovulatory rise in FSH. Androgens, synthesized in the theca cells, also rise around the time of ovulation and this is thought to have an important role in stimulating libido, ensuring that sexual activity is likely to occur at the time of greatest fertility. The LH surge is one of the best predictors of imminent ovulation, and this is the hormone detected in urine by 'ovulation predictor' tests. The LH surge initiates final maturation of the oocyte with completion of meiosis and extrusion of the first polar body. The LH surge also induces an inflammatory- type reaction at the apex of the follicle adjacent to the outer surface of the ovarian cortex. The physical ovulation of the oocyte occurs after breakdown of the follicular wall occurs under the influence of LH, FSH and progesterone-controlled proteolytic enzymes, such as plasminogen activators and prostaglandins. A chemotactic effect of ovarian cytokines drawn the fimbria of the fallopian tube to within close proximity of the rupturing follicle. A thin mucus strand seems to join the mouth of the fallopian tube to the oocyte into the tube.
Luteal phase:
After the release of oocyte, the remaining granulosa and theca cells on the ovary rapidly fill with blood and form the corpus luteum. The granulosa cells have a vacuolated appearance with accumulated yellow pigment, hence the name corpus luteum (yellow body). Ongoing pituitary LH secretion and granulosa cell activity ensures a supply of progesterone which stabilizes the endometrium in preparation for pregnancy. Progesterone levels are at their highest in the cycle during the luteal phase (above 25nmol/l), these concentrations rise further if pregnancy follows. This also has the effect of suppressing FSH and LH secretion to a level that will not produce further follicular growth in the ovary during that cycle. The luteal phase lasts 14 days in the most women, without great variation. In the absence of βHCG being produced from an implanting embryo, the corpus luteum will regress in a process known as luteolysis. The mature corpus luteum is less sensitive to LH, produces less progesterone, and will gradually disappear from the ovary. The withdrawal of progesterone has the effect on the uterus of causing shedding of the endometrium and thus menstruation. Reduction in levels of progesterone, oestrogen and inhibin feeding back to the pituitary cause increased secretion of gonadotrophic hormones, particularly FSH. New preantral follicles begin to be stimulated and the cycle begins again.
Menstruation:
Menstruation refers to the shedding of the superficial layers of the endometrium, with subsequent repair in preparation for regrowth from basalis layer. The endometrium is under the influence of sex steroids that circulate in female of reproductive age. During the ovarian follicular phase, the endometrium undergoes proliferation ( proliferative phase), during the ovarian luteal phase, it has its ( secretory phase). Decidualization, the formation of a specialized glandular endometrium, is an irreversible process and apoptosis occurs if there no embryo implantation. Menstruation (day 1) is the shedding of the dead endometrium and ceases as the endometrium regenerates (which normally happens by day 5-6 of the cycle). A fall in circulating levels of oestrogen and progesterone about 14 days after ovulation leads to loss of tissue fluid, vasoconstriction of spiral arterioles and distal ischaemia. This results in tissue breakdown, and loss of the upper layer along with bleeding from fragments of the remaining arterioles is seen as menstrual bleeding. Enhanced fibrinolysis reduces clotting. Vaginal bleeding will cease after 5-10 days as arterioles vasoconstrict and the endometrium begins to regenerate. The invasion of leucocytes and subsequent expression of inflammatory mediators has led to menstruation being likened to an inflammatory event. The prostaglandins of the E and F series are present in high concentrations in the endometrium, and their synthesis is regulated by the ovarian steroids. Increased production of PGF2α produces the myometrial contractions and vasoconstriction seen at menstruation, while E series increase pain and oedema, and are vasodilatory. The end result of this cascade of events is constriction of the spiral arterioles with contraction of the uterine muscle, leading to expulsion of the shed tissue.
The proliferative phase:
Menstruation will normally cease after 5-7 days, once endometrial repair is complete. After this time, the endometrium enters the proliferative phase, when glandular and stromal growth occur. The epithelium lining the endometrial glands changes from a single layer of columnar cells to a pseudostratified epithelium with frequent mitosis. Endometrial thickness increases rapidly, from 0.5 mm at menstruation to 3.5-5 mm at the end of the proliferative phase.
The secretory phase:
After ovulation (generally around day 14), there is a period of endometrial glandular secretory activity. Following the progesterone surge, the oestrogen induced cellular proliferation is inhibited and the endometrial thickness does not increase any further. However, the endometrial glands will become more tortuous, spiral arteries will grow, and fluid is secreted into glandular cells and into the uterine lumen. Later in the secretory phase, progesterone induces the formation of a temporary layer, known as the decidua, in the endometrial stroma.
Immediately prior to menstruation, three distinct layers of endometrium can be seen. The basalis is the lower 25% of the endometrium, which will remain throughout menstruation and shows few changes during the m.c. the mid –portion is the stratum spongiosum with oedematous stroma and exhausted glands. The superficial portion (upper 25%) is the stratum compactum with prominent decidualized stromal cells. On the withdrawal of both oestrogen and progesterone, the decidua will collapse, with vasoconstriction and relaxation of spiral arteries and shedding of the outer layers of the endometrium.
Measurement of ovarian reserve:
Female reproductive potential is directly proportionate to the remaining number of oocytes in the ovaries. This number decreases from birth onwards, and the rate of loss accelerates after the age of 37 in an average healthy women, or at an earlier age following long-term gonadotrophin deficit or exposure to toxins, e.g. chemotherapy. Research using ultrasound markers has looked at measurements of ovarian volume, mean ovarian diameter and antral follicle count to calculate ovarian reserve. Biochemical markers include FSH, Oestradiol, inhibin B, anti-Mullerian hormone (AMH). AMH is produced in the granulosa cells of ovarian follicles and does not change in response to gonadotrophins during the m.c. Serum AMH is high in patient with PCOS who are in danger of over response and hyperstimulation, and low in patients who are closer to menopause with low ovarian reserve.
o strual maining arterioles is seen as the upper layer along with bleeding from fragements