Inflammation
Dr Mustafa Salah FadhilChemical Mediators of Inflammation
A substances which play a role in genesis and modulation of inflammatory reactionThey are responsible for:
1. Vasodilatation2. Increased permeability
3. Emigration of WBC (Chemotactic agent).
Chemical Mediators of Inflammation
Chemical Mediators of InflammationA/ Vasoactive Amines
1) Histamine: secreted from mast cells, basophils & platelets
2) Serotonin: secreted from platelets
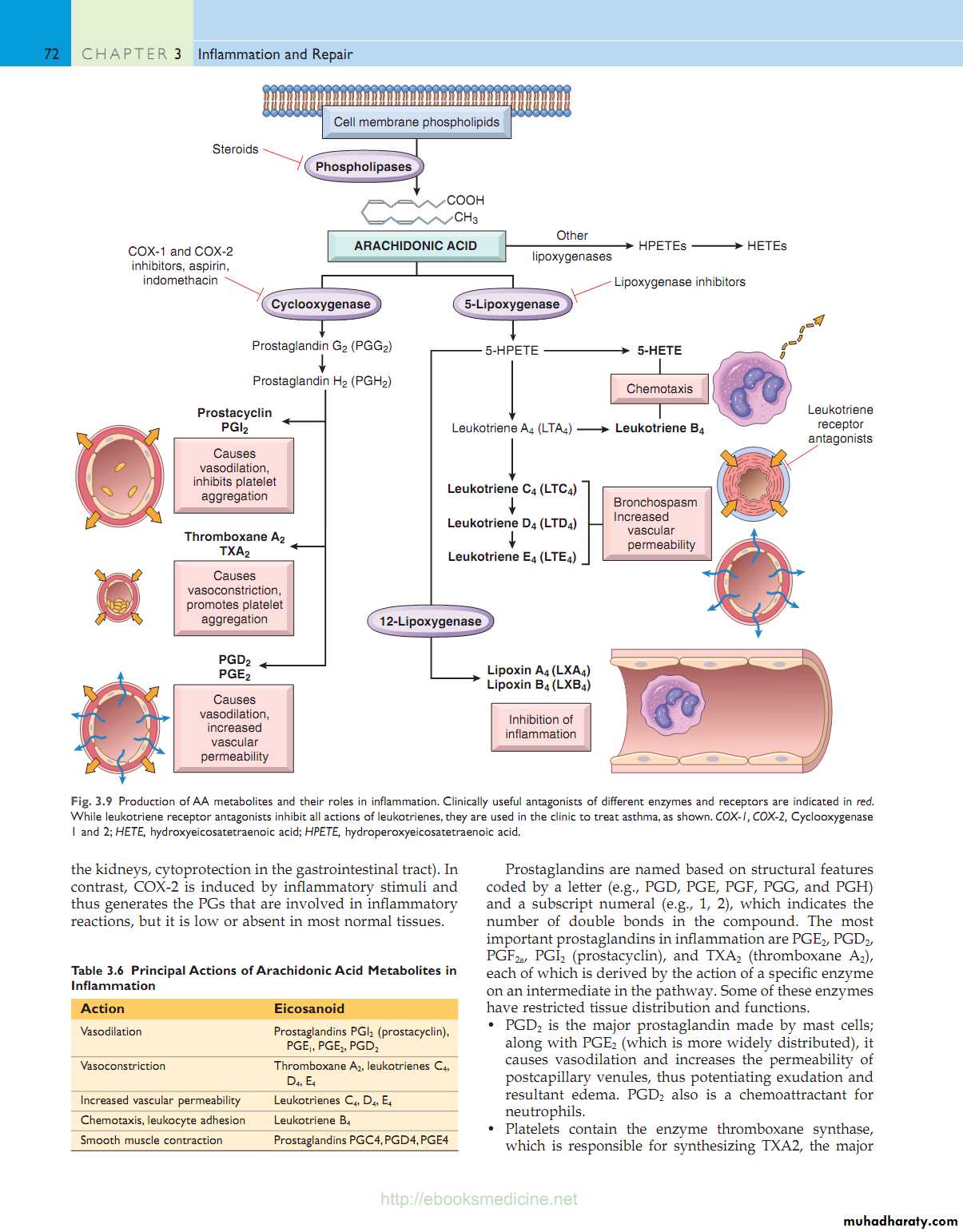
Effects: arteriolar vasodilation & increase vascular permeabilityB/ Arachidonic Acid (AA) Metabolites
AA present in the cell membrane phospholipidsRelease from phospholipids through the action of phospholipase enzyme by mechanical, chemical & physical stimuli
AA metabolism proceeds along 1 of 2 pathways
Cyclooxygenase pathway---------- PostoglandinsLipooxygenase pathway------------Leukotriens
Arachidonic Acid Metabolites
Thromboxane A2Vasoconstriction
Platelet aggregation
Protacyclin (PGI2)
Vasodilatation
Inhibits Platelet aggregation
PGD2, PGE2 & PGF2
VD & edema
PGE2:
Fever
Pain
5-HETE:
Chemotaxis
LTB4:
ChemotaxisAggregation of neutrophils
LTC4, LTD4, LTE4
Vasoconstriction
Bronchospasm
Increase vascular permeability
Cyclooxygenase pathway
Lipooxygenase pathwayC) Cytokines
Polypeptides produced by activated lymphocytes & macrophages.Involved in cellular immunity & inflammatory responses.
• IL-1 & TNF
• IL-6
• IL-8
Chemotactant & neutrophil activating agent
D) Nitric Oxide (NO)
Soluble free radical gas synthesized by endothelial cells, macrophages & specific neurons in the brain
Effects:
Vascular smooth muscle relaxation causing VDDecreased platelet aggregation & adhesion
Microbicidal agentE) Oxygen Free Radicals
Superoxide (O2-), OH-, H2O2 & NOEffects
kill bacteriaEndothelial cell damage causing increase vascular permeability
Activation of proteinases
Injury to surrounding cells
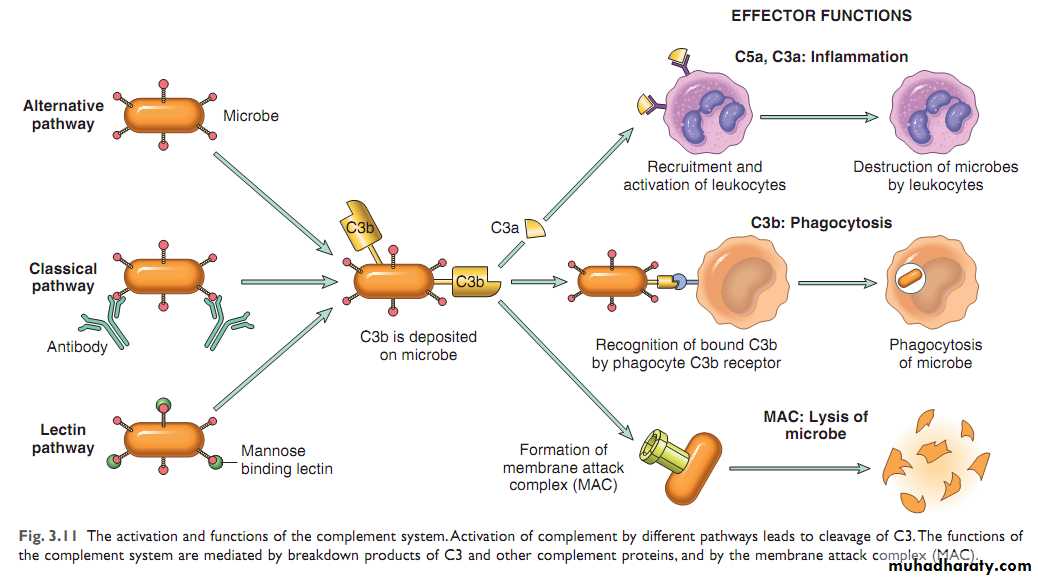
F) Complement SystemPresent as inactive form in the plasma
Vascular effect (anaphylotaxins): C3a, C5a & C4a causing VD & increase vascular permeabilityLeukocyte adhesion, chemotaxis & activation: C5a
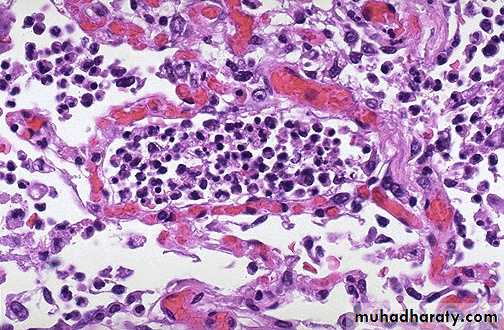
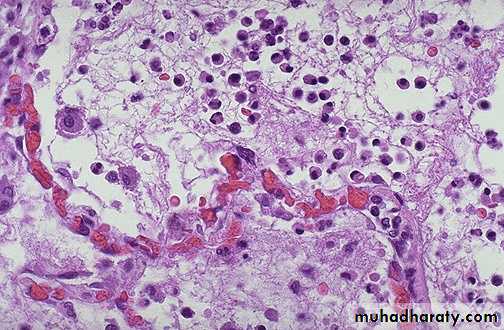
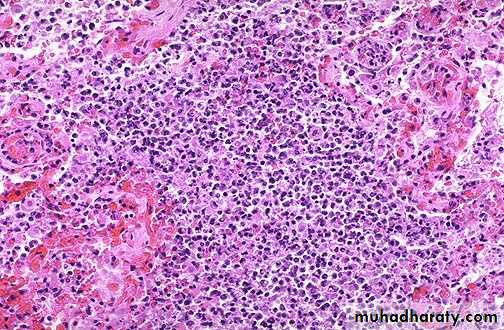
Phagocytosis: C3b & C3b1 act as opsoninsMicroscopic appearance of acute inflammation
Congestion of blood vesselsExudation of fluid
Exudation of inflammatory cells mainly neutrophils
Special macroscopic appearances of acute inflammation
1. Serous inflammation:There is abundant protein-rich fluid exudate with a relatively low cellular content. Examples include inflammation of the serous cavities, such as peritonitis, and inflammation of a synovial joint, acute synovitis.
2. Catarrhal inflammation:
When mucus hypersecretion accompanies acute inflammation of a mucous membrane. The common cold is a good example.3. Fibrinous inflammation :
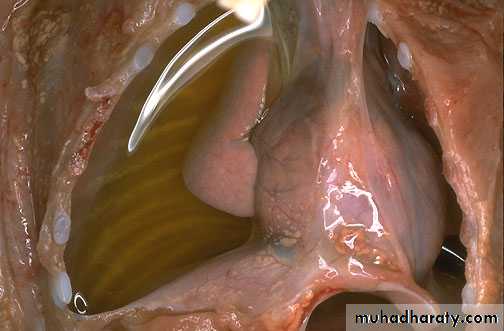
When the inflammatory exudate contains plentiful fibrinogen, this polymerises into a thick fibrin coating. This is often seen in acute pericarditis and gives the parietal and visceral pericardium a 'bread and butter' appearance.Special macroscopic appearances of acute inflammation
4. Suppurative (purulent) inflammation:
Means: pus
Consists of dying and degenerate neutrophils, infecting organisms and liquefied tissues and exudate.
Abscess (a localised collection of pus in a tissue).
Empyema is accumulationof pus in a hollow viscus, e.g. empyema of the gallbladder or of the appendix
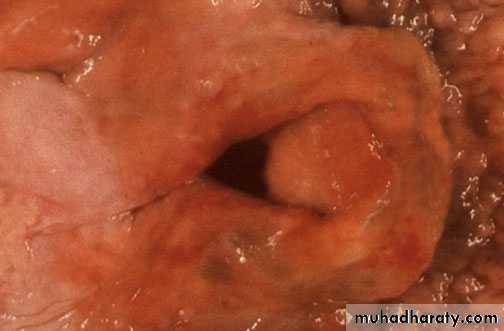
5. Membranous inflammation:
An epithelium becomes coated by fibrin, desquamated epithelial cells and inflammatory cells. e.g. grey membrane seen in pharyngitis or laryngitis due to Corynebacterium diphtheriae.Fates (outcomes) of acute inflammation
1. Complete resolution: return to normalIt involve:
removal of the exudate, fibrin & debris
reversal of the microvascular changes
regeneration of lost cells
2. Healing & organization: connective tissue replacement.
Occurs in:
substantial tissue destruction
tissue cannot regenerate
extensive fibrinous exudate
3. Suppuration:
(It may be diffuse in tissue, localized in tissue (abscess) , on the surface of a wound, or in serous cavity)
4. Progression to chronic inflammation:
when there is persistent infection
when there is foreign body, …etc
Complete resolution
Effects of Acute Inflammation
Dilution of toxinsEntry of antibodies
Drug transport
Fibrin formation
Delivery of nutrient & O2
Stimulation of immune system
Digestion of normal tissue
Swelling & painInappropriate inflammatory response
BENIFITIAL EFFECTS
HARMFUL EFFECTS