AUTONOMICNERVOUS SYSTEM
Dr. Faehaa Azher Al-MashhadaneANATOMY OF THE AUTONOMICNERVOUS SYSTEM
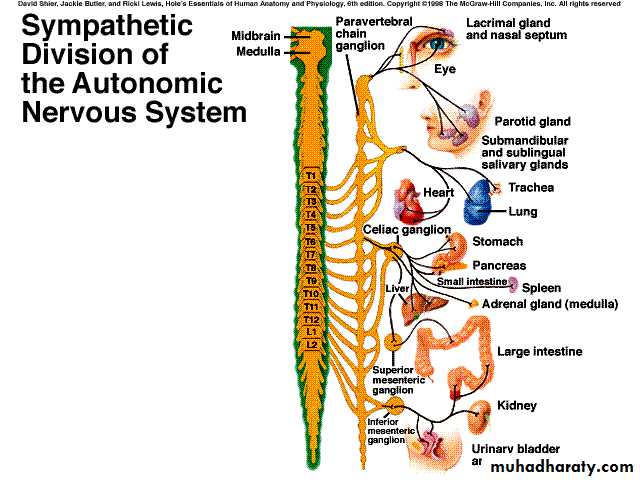
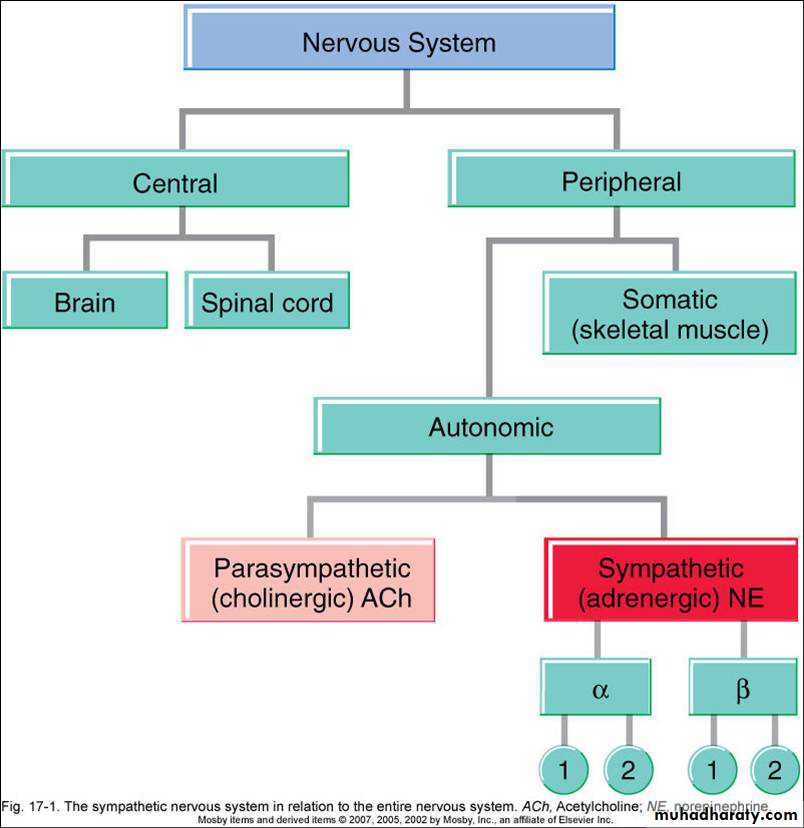
The ANS lends itself to division on anatomic grounds into two major portions:sympathetic (thoracolumbar) division
parasympathetic
= Thoracolumbar
division (T1 to L2)Preganglionic neurons (N1)from thoracolumbar region of spinal cord
Pre and paravertebral ganglia
Long postganglionic neurons (N2) secrete NE onto adrenergic receptors
Most thoracic and lumbar sympathetic preganglionic fibers are short and terminate in ganglia located in the paravertebral chains that lie on either side of the spinal column.
Most of the remaining sympathetic preganglionic fibers are somewhat longer and terminate in prevertebral ganglia, which lie in front of the vertebrae, usually on the ventral surface of the aorta.
From the ganglia, postganglionic sympathetic fibers run to the tissues innervated.
Adrenergic Transmission
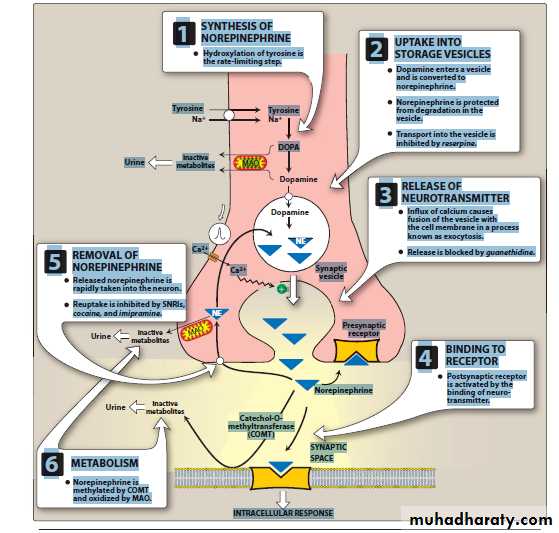
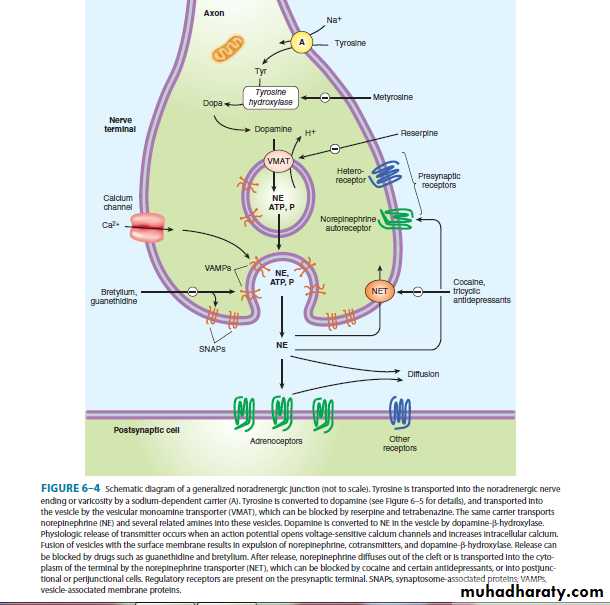
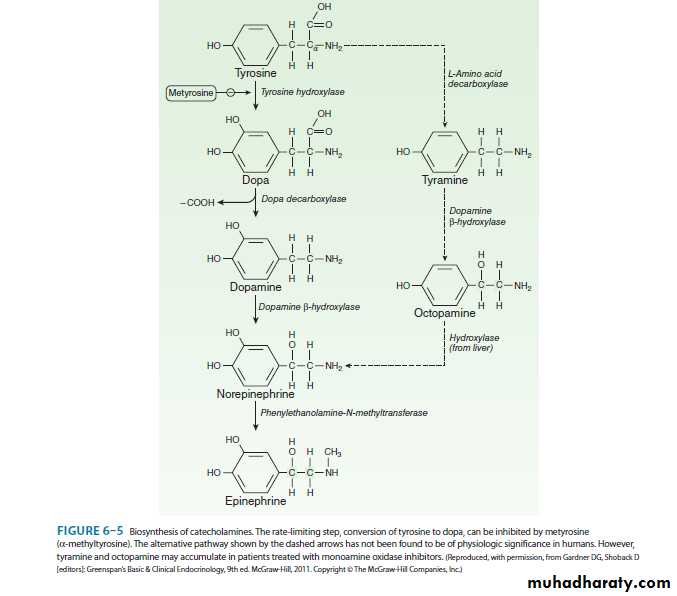
Adrenergic neurons transport the precursor amino acid tyrosine into the nerve ending, convert it to dopa, and then synthesize a catecholamine transmitter dopamine, norepinephrine, or epinephrine, and store it in membrane-bound vesicles.
In most sympathetic postganglionic neurons, norepinephrine is the final
product.In the adrenal medulla and certain areas of the brain, some norepinephrine is further converted to epinephrine.
In dopaminergic neurons, synthesis terminates with dopamine.
Adrenergic TransmissionAutonomic nervous system
Adrenergic agonistsCLASSIFICATION OF ADRENERGIC DRUGS AND RECEPTORS
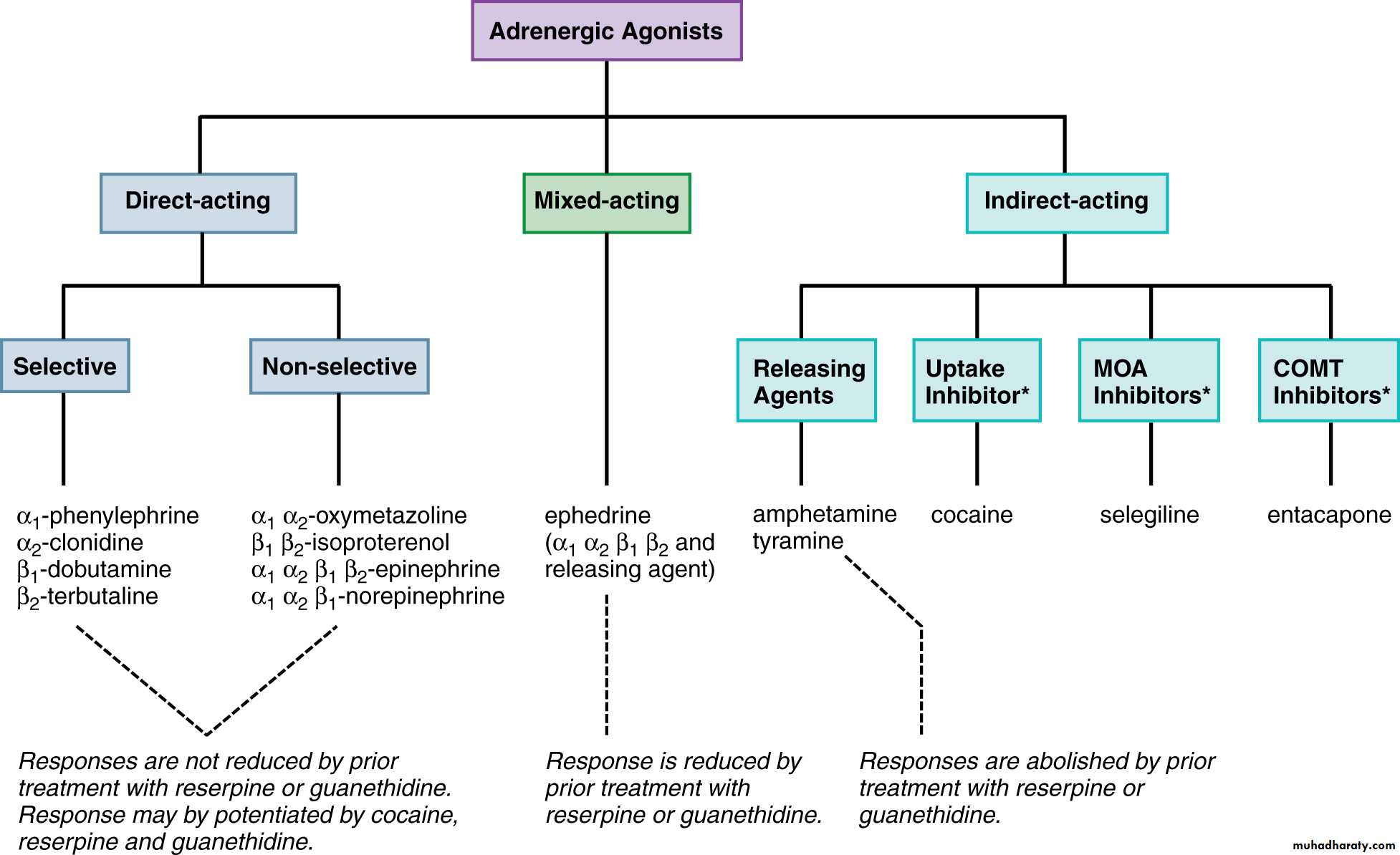
One common feature of all adrenergic drugs is that their effects are mediated through activation of adrenergic receptors.Direct-acting adrenergic agonists bind to adrenergic receptors and activate the receptors to produce their effects.
Indirect-acting agonists act by increasing the amount of norepinephrine available to stimulate adrenergic receptors
The most common action of indirect-acting agonists
is to cause the release of the neurotransmitter norepinephrine from sympathetic nerve terminals.
Mixed-acting adrenergic agonists have direct and indirect mechanisms of action.
Adrenergic receptors have been classified into three major types:
α1-adrenergic, α2-adrenergic, and β-adrenergic receptors.
In recent years, numerous receptor subtypes (α1A, α1B, α1D; α2A, α2B, α2C; β1, β2, β3) have been discovered by molecular cloning and pharmacologic
techniques.
Several dopamine receptors have also been identified (D1, D2, D3, D4, D5).
Endogenous Catecholamines
EpinephrineVascular effects
The net effect of systemic administration of norepinephrine or epinephrine on the cardiovascular system depends on various factors, includingthe route and rate of administration,
the dose given, and
the presence or absence of interacting drugs
When injected locally, norepinephrine and
epinephrine cause contraction of vascular smooth muscle and vasoconstrictionin the surrounding tissues by stimulating α-adrenergic receptors.
Systemic effects on the vasculature occurring after absorption of these catecholamines into the circulation depend on the plasma concentrations
achieved and on the drugs’ actions at α-adrenergic and β-adrenergic receptors
Cardiac effects
Norepinephrine and epinephrine stimulate β1-adrenergic receptors located in cardiac muscle, pacemaker, and conducting tissues of the heart; β2 receptors, also located in these tissues but in smaller numbers, contribute to the cardiac effects of epinephrine.
Effects on nonvascular smooth muscle
Generally, α1-adrenergic receptoractivation leads to contraction, whereas
β2 receptor activation leads to relaxation.
In either case, these effects require doses of epinephrine or norepinephrine that result in significant cardiovascular stimulation.
Effects on salivary glands
Secretory cells of the major salivary glands contain α1-adrenergic, β1-adrenergic, and some β2-adrenergic receptors.The Principal adrenergic receptor linked to protein secretion is the β1 receptor, although α1 receptors also play a secretory role.
Metabolic responses
Metabolic responses to β2-adrenergic and β1-adrenergic receptor stimulationlead to a transitory increase in circulating blood glucose as a result of liver glycogenolysis and increased glucagon secretion.
An α2 receptor–mediated inhibition of insulin secretion contributes to the hyperglycemia caused by epinephrine.
Central nervous system effects
Although the catecholamines are extensively involved inneurotransmission in the CNS, peripherally administered catecholamines gain little access to the CNSIntravenous injection of epinephrine produces a variety of apparently central effects, however, including feelings of anxiety and apprehension.
Endogenous Catecholamines
Dopamine
Cardiovascular effects
Dopamine interacts with various receptor types to influence vascularfunction, and it is used therapeutically for maintaining renal function in cases of shock associated with compromised cardiac output.
With moderate doses, dopamine was thought to act at myocardial β1-adrenergic receptors to increase contractile force. At higher doses, dopamine also stimulates α1-adrenergic receptors, which produces vasoconstriction.
As with all catecholamines, excessive doses of dopamine can cause tachycardia and generate arrhythmias. In addition to stimulating α1 and β1 receptors directly, dopamine in moderate to high doses causes the release of norepinephrine from sympathetic nerve terminals.
α-Adrenergic Receptor Agonists
These drugs stimulate α-adrenergic receptors, but have low affinity forβ-adrenergic receptors.
Phenylephrine and methoxamine differ from epinephrine and norepinephrine by being
selective agonists at α1adrenergicreceptors.
Their primary pharmacologic effect is to cause contraction of
vascular smooth muscle, resulting in an increase in systolic and diastolicblood pressures and reflex bradycardia.
Midodrine
is a synthetic drug that
selectively activates α1-adrenergic receptors.
It also causes vasoconstriction, and it is used to treat postural
hypotension caused by impaired autonomic nervous system function.
The α2-adrenergic receptor agonists clonidine, guanabenz, guanfacine, and methyldopa effectively enter into the CNS and selectively stimulate α2-adrenergic receptors in the brain.
Methyldopa enters into the nerve terminal and is converted into the α2 receptor– selective agonist α-methylnorepinephrine.
Α Methylnorepinephrine is nearly equipotent to norepinephrine as a vasoconstrictor in humans.
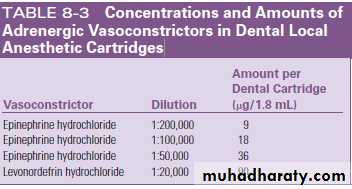
This agent has been developed as the drug levonordefrin, which is used as a vasoconstrictor in some local anesthetic solutions.
β-Adrenergic Receptor Agonists
IsoproterenolIsoproterenol, a synthetic catecholamine, is a potent nonselective β-receptor agonist.
It does not appreciably distinguish among the β1, β2, and β3 receptor subtypesCardiac and vascular effects
The actions of isoproterenol on the cardiovascular system are based solely on the stimulation of β-adrenergic receptorsIt causes a marked decrease in diastolic blood pressure from β2 receptor–
mediated vasodilation, primarily caused by relaxation of blood vessels in skeletal muscle, with some additional vasodilation in the renal and mesenteric vascular beds
Effects on bronchial smooth muscle
As an agonist of β2-adrenergic receptors, isoproterenol relaxes bronchial smooth muscle in the lungs to relieve or prevent bronchoconstriction.
Disadvantages of the use of isoproterenol for relief of bronchospastic disorders that limit its clinical use are its nonselectivity for β-adrenergic receptor subtypes (which can result in β1 receptor–induced tachycardia,
palpitation, and arrhythmias) and the development of tolerance with frequent use.
Metabolic and other effects
Although the β receptor agonist activity of isoproterenol stimulates glycogenolysis and gluconeogenesis in the liver, it is not as effective as epinephrine in elevating plasma glucose.Isoproterenol stimulates the secretion of saliva that is rich in amylase and other proteins.
The drug is also capable of causing CNS excitation at doses higher than used clinically.
β-Adrenergic Receptor AgonistsDobutamine
Cont.
A synthetic analogue of dopamine, dobutamine acts as an adrenergic receptor agonist with little or no effect on dopamine receptors.The primary action of dobutamine is to increase myocardial contractility and cardiac output without significantly increasing the heart rate. The
Selective β2-Adrenergic Receptor Agonists
Metaproterenol, terbutaline, albuterol, levalbuterol, pirbuterol, and salmeterol are relatively selective β2 receptor agonists that are effective in decreasing airway resistance without causing as much cardiac accelerationThese drugs are usually inhaled; however, oral administration of metaproterenol, albuterol,
and terbutaline may be useful under certain limited conditions. Systemic adverse effects are usually greater by the oral route.
Mixed-Acting and Indirect-Acting Adrenergic Agonists
Numerous adrenergic agonist drugs produce some or all of their effects by causing the release of norepinephrine from adrenergic nerve terminals.
They do so by being transported into the adrenergic nerve ending or adrenal chromaffin cells, where these drugs displace catecholamines from the vesicular storage sites into a cytoplasmic pool in the nerve endings or chromaffin cells. This cytoplasmic pool is distinct from that of the storage vesicles from which release occurs during nerve stimulation.
These drugs have a pharmacologic profile similar to that of norepinephrine. In contrast to norepinephrine, these drugs are generally not subject to rapid inactivation and are usually effective by the oral route.
Cont.
Ephedrine is an example of an orally active, mixed-acting drug.In addition to releasing norepinephrine, ephedrine is a direct α and
β receptor agonist. It can cause bronchodilation, vasoconstriction,
increased heart rate, and modest CNS stimulation.
Cont.
Amphetamine is primarily an indirect-acting drug that easily enters the brain and stimulates the release of catecholamines in the CNS.Amphetamine is a potent CNS stimulant that causes numerous effects, including increased alertness, relief of fatigue, enhanced athletic performance, and euphoria.
β-Adrenergic Receptor Agonists
ABSORPTION, FATE, AND EXCRETIONCont.
The route for administering adrenergic agonists is determined by the chemical structure.All catecholamines and certain other drugs, unless specifically modified, are subject to enzymatic destruction in the gastrointestinal tract.
Catecholamines are usually administered systemically by parenteral injection or intravenous infusion.
Topical instillation and inhalation are the preferred routes of administration for ocular and respiratory applications, respectively.
β-Adrenergic Receptor Agonists
GENERAL THERAPEUTIC USESClinical applications of the adrenergic agonists can be divided into eight major categories:
local vasoconstriction,
vasoconstriction in the treatment of hypotension and shock,
bronchodilation,
Relaxation of uterine smooth muscle,
ophthalmic uses,
relief of allergic states (including anaphylaxis),
CNS stimulation,
and control of hypertension.
Local Vasoconstriction
Various drops, sprays, aerosols, and oral dosage forms of several adrenergic agonists have proved useful in providing temporary symptomatic relief of nasal congestion.These compounds are agonists at α receptors (α1 or α2 or both) and have minimal CNS stimulant effects.
Common examples include phenylephrine, pseudoephedrine, and oxymetazoline.
Cont.
An adverse effect associated with the local administration of nasal decongestants is rebound congestion, a chronic swelling of the nasal mucous membranes after the effect of the drugs wears off.
Cont.
Adrenergic agonists are often used to produce hemostasis for surgery and to enhance local anesthesia. Whether applied topically or administered by injection with or without a local anesthetic, adrenergic agonists can significantly improve visibility in the operative field in certain situations.Because vasoconstriction is temporary, the use of these drugs is no substitute for the adequate surgical control of bleeding.
Adrenergic agonists must often be used with special caution during general anesthesia
because certain inhalation anesthetics (e.g., halothane) predispose the heart to the arrhythmogenic action of the adrenergic agonists.Treatment of Hypotension and Shock
Shock is a condition caused by inadequate tissue perfusion. It is usually associated with a decrease in arterial blood pressure and, if not treated, may quickly lead to multiorgan system failure.Adrenergic agonists may prove useful in restoring blood pressure and in correcting the distribution of blood flow, especially to the vital organs, whenever shock develops under normovolemic conditions
Cont,
α-Adrenergic receptor agonists (e.g., phenylephrine), which increase blood pressure by causing vasoconstriction, are most useful during episodes of inadequate sympathetic nervous system function that may result from spinal anesthesia or hypotensive drug overdose.Such drugs are less beneficial in other shock states associated with hypotension, however, because they may impair blood flow to the kidneys and mesenteric organs.
Bronchodilation
Acute and chronic obstructive pulmonary diseases are marked by increased inspiratory and expiratory resistance, and the adrenergic agonists have historically played an important role in the relief of
these conditions.
Currently, the adrenergic agents most useful in the treatment of bronchospastic disease are agonists with selectivity for β2- adrenergic receptors because they produce marked bronchodilation with less effect on the heart than nonselective β receptor agonists
Cont.
The selective β2 receptor agonists used for bronchodilation include metaproterenol, terbutaline, albuterol, levalbuterol, pirbuterol, salmeterol,and formoterol.Salmeterol and formoterol have durations of action of about 24 hours.
Treatment of Allergic StatesAdrenergic agonists, especially epinephrine, are especially useful in reversing the effects of histamine and other mediators associated with allergic reactions.
In contrast to the antihistamines, adrenergic
agonists are physiologic antagonists, producing responses oppositeto the acute effects produced by histamine and associated autacoids.
Cont.
For acute allergic reactions such as urticaria, subcutaneous injection of 0.1 to 0.5 mL of 1:1000 (i.e., 1mg/mL) epinephrine should be adequate. Fulminating disturbances such as anaphylactic shock require a faster absorption of epinephrine than provided by subcutaneous injection,especially if circulation is impaired.Intramuscular (intralingual)injection of 0.3 to 0.5 mL of 1:1000 epinephrine or, if the patient haspreviously been prepared for intravenous injections, slow intravenous administration of 1:10,000 epinephrine (0.1 mg in 5 minutes) is recommended.
With this latter route of administration, there is a considerable risk of precipitating serious cardiac arrhythmias and ventricular fibrillation. Because of the rapid metabolism of epinephrine, reinjection at intervals of 5 to 15 minutes may be required. Subcutaneous administration generally provides the longest duration of action, and intravenous injection provides the shortest.
Central Nervous System Stimulation
For many years, selected adrenergic agonists have been used clinicallybecause of their ability to produce stimulation of certain functions
of the CNS that result in increased alertness and attention span and
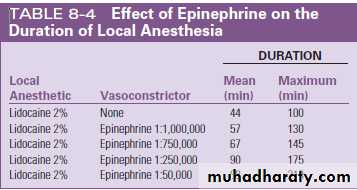
THERAPEUTIC USES IN DENTISTRY
Vasoconstrictors are widely often used in local anesthetic solutions.The vasoconstrictor most commonly used in dentistry is epinephrine,
with levonordefrin (the l isomer of nordefrin) being used less
frequently, usually with mepivacaine.
Cont.
The maximum recommended strength of thevasoconstrictor is 1:100,000 epinephrine equivalency for routine nerve
block anesthesia.
When local tissue hemostasis is required for surgical procedures, such as periodontal surgery, the dentist may additionally
choose to infiltrate the area with local anesthetic solution containing 1:50,000 epinephrine, but repeated injections of 2% lidocaine with 1:50,000 epinephrine may cause tissue necrosis and microscarring.
Cont.
Vasoconstrictors serve several useful purposes when used with local anesthetic solutions. First, they prolong the duration of local anesthesia several-fold and may improve the frequency of successful nerve block.
Second, systemic toxicity of the local anesthetic may be minimized by reducing the peak blood concentration of the anesthetic agent.
Third, when anesthetic solutions are given by infiltration, vasoconstrictors tend to reduce blood loss associated with surgical procedures
One issue of potential toxicity is the systemic effects of vasoconstrictors after intraoral injection in patients with cardiovascular disease.
Some older reports recommend that cardiac patients be given local anesthetics with vasoconstrictors if needed for adequate anesthesia because the benefits of satisfactory pain control were greater than the risks of small amounts of vasoconstrictor.
The validity of this statement depends on the level of stress on the patient and the amount, rate, and manner in which the epinephrine-containing solution is injected.
Cont.
It is often necessary to produce gingival retraction for operative
procedures on teeth and for making impressions.
Besides astringents such as zinc and aluminum salts, retraction cord impregnated With epinephrine, containing as much as
1.2 mg of drug per inch of cord, is commercially available.
Systemic absorption is marked by signs of anxiety, elevated blood pressure, increased heart rate, and occasional arrhythmias.
These effects can be extremely serious in a patient with cardiovascular disease or in a patient who is taking medication that reduces the uptake or otherwise enhances the
activity of adrenergic agents.
Because of this concern, epinephrine-impregnated
retraction cord is used much less often than other typesof retraction cord.
gingival retraction cord
Cont.
Various products are available to control capillary bleeding occurring with surgical procedures on gingival tissues.Topical epinephrine hydrochloride (1:1000) and phenylephrine (1:100) are most common.
β-Adrenergic Receptor AgonistsADVERSE EFFECTS
Cont.
Almost all adverse effects of the adrenergic agonists are dose related.Toxic reactions can result from
the administration of too large a dose,
accidental intravascular injection,
impaired uptake of the drug,
a heightened sensitivity or number of adrenergic receptors,
or therapeutic doses given to a patient with preexisting cardiovascular disease.
Most serious of the toxic effects of epinephrine are cardiac disturbances, with increased stimulation of the heart leading to myocardial
ischemia, possibly heart attack, and arrhythmias, including ventricular fibrillation.
Patients with a history of uncontrolled hyperthyroidism, hypertension, or angina pectoris are particularly susceptible.
Cont.
Drugswith primarily α-adrenergic receptor stimulation can cause excessive
vasoconstriction in overdose.
Local tissue necrosis may result from any
vasoconstrictor injected into a region where ischemia is likely, such as
the digits of the hands or feet.
Cont.
CNS reactions to classic sympathomimetic drugs include nervousness, excitability, insomnia, dizziness, and tremors.The most common side effects of centrally acting α2-agonist antihypertensive agents are dizziness, drowsiness, and xerostomia.
The xerostomia seems to be most severe with clonidine and guanabenz. Constipation, sexual dysfunction, CNS disturbances, bradycardia, and excessive hypotension have also been reported.
Adrenergic Antagonists
We now know that there are at least nine adrenergic receptors (α1A, α1B, α1D, α2A, α2B, α2C, β1, β2, and β3).
Selective antagonists against each of these receptors have been developed with the goal of obtaining drugs capable of specifically interfering with the receptor involved in a pathophysiologic condition without blockade of other receptors that could lead to unwanted side effects.
Adrenergic Antagonists
SELECTIVE α1-ADRENENERGIC RECEPTORANTAGONISTS
α1-adrenergic receptors are located predominantly
on the post junctional membranes of glands and smooth muscle.The α1-adrenergic receptors associated with smooth muscle of
arteries and veins play an important role in promoting vasoconstrictionThe α1-adrenergic receptors are also important in regulating
the tone of nonvascular smooth muscle, such as in the neck of theurinary bladder and capsule of the prostate.
More recent evidence has suggested that the α1-adrenergic receptor plays a role in the regulation of hypertrophic growth, the generation of reactive oxygen species, and apoptotic cell death.
Antagonism of these cellular events may also be the reason that α1-adrenergic receptor blockers are effective in the treatment of benign prostatic hyperplasia.
Prazosin and Analogues
The first antagonists that targeted the α1-adrenergic receptor were nonselective and also blocked the α2-adrenergic receptor.These drugs were unsuitable as antihypertensive agents, presumably because of the α2-adrenergic receptor blockade.
The disadvantages associated with the nonselective blockade of α receptors inspired a search for agents with receptor selectivity
Cont.
The first therapeutically useful α1-adrenergic receptor antagonistdeveloped was prazosin .
Terazosin and doxazosin are structural analogues that were subsequently introduced. Although these agents differ in pharmacokinetic properties, their mechanism of action is the same.
Cont.
As a result of blocking smooth muscle α1-adrenergic receptors, prazosin dilates arterioles and veins.Each of these actions contributes to the hypotension seen with this drug. Blockade of arterial smooth
muscle produces hypotension by reducing peripheral resistance.
The venodilation resulting from blocked venous α1-adrenergic receptors decreases cardiac preload. Compared with the nonselective α receptor antagonists, prazosin causes less tachycardia, a smaller increase in cardiac output, and less renin release.
Therapeutic uses
Prazosin, terazosin, and doxazosin can be used in monotherapy for the treatment of hypertensionTerazosin and doxazosin, which are given once a day, may have advantages over prazosin, which requires more frequent administration.
prazosin is effective for treating nightmares and improving sleep and reducing the severity of posttraumatic stress disorder.
Adverse effects
Orthostatic or postural hypotension is a concern with prazosin analogues.The effect is most likely to occur with initial administration and is known as “first-dose” syncope.
Hypotension ensues when the systemic arterial blood pressure decreases by more than 20 mm Hg on standing. In this situation, cerebral perfusion decreases, and an individual may become lightheaded, dizzy, or faint. In changing from the supine to the standing position, gravity tends to cause blood to pool in the lower extremities. However, several reflexes, including sympathetically mediated venoconstriction, minimize this pooling, and maintain cerebral perfusion.
NONSELECTIVE α-ADRENERGIC RECEPTOR ANTAGONISTS
The nonselective α-adrenergic receptor–blocking drugs prevent the action of adrenergic transmitters and sympathomimetic agonists at allα-adrenergic receptors.
Although many drugs exhibit some α-blocking activity, only phentolamine and phenoxybenzamine are currently
used clinically for their nonselective α-adrenoceptor antagonist action.
More recently, phentolamine mesylate has been approved for the reversal of soft tissue anesthesia after administration of local anesthetics with vasoconstrictors for nonsurgical dental procedures.
The drug is formulated in dental cartridges
(0.4 mg/1.7-mL cartridge) and is injected in the same manner as the local anesthetic when pain relief is no longer needed. The median duration of post treatment anesthesia in the upper and lower lips of adults and children is reduced by 85 minutes when phentolamine mesylate is injected at the end of restorative and dental hygiene procedures lasting about 45 minutes. Return of normal function (e.g., speaking, smiling, drinking) occurs in concert with return of normal sensation.
It is unlikely that the phentolamine is acting
by reversing the vasoconstrictor effect of injected epinephrine, which should have already disappeared from the local tissues.Instead, the phentolamine probably increases local blood flow by blocking sympathetic
tone, which hastens the removal of the local anesthetic from local neurons.
Doses of phentolamine used for this purpose (0.2 to 0.8 mg) (0.5 to 2.0 cartridges), are approximately 10 times less than doses injected intravenously for treatment of hypertensive emergencies.
β-ADRENERGIC RECEPTOR ANTAGONISTS
The β-adrenergic receptor antagonists, also called β-adrenergic receptorblockers or simply β blockers are an important and versatile class of drugs widely used in cardiovascular therapeutics. The β blockers
are also used to treat numerous non-cardiovascular disorders.
First-Generation β-Adrenergic Receptor Blockers,Nonselective Antagonists
These drugs are competitive antagonists with equal affinity at both the β1-adrenergic and β2-adrenergic receptors and as such are referred to as nonselective β blockers.Propranolol was the first β-blocking drug to be approved in the United States and is considered the prototype for this class of compounds.
The beneficial effects of propranolol and
other nonselective β blockers are mostly attributable to blockade of the β1-adrenergic receptor.
Second-Generation β-Adrenergic Receptor Blockers,β1-Selective Antagonists
Once it became apparent that there were subtypes of the β-adrenergic receptor, subtype selective antagonists were developed.
Metoprolol, the first selective β1 receptor antagonist, and its successors (e.g., atenolol, acebutolol, and esmolol) have attracted considerable attention because of their relative freedom from the unwanted effects of β2-adrenergic receptor blockade.
This β1 selectivity is relative with existing agents, and these drugs lose much of their selectivity
at higher doses. Presently, both nonselective and selective β blockers are used clinically.
Third-Generation β-Adrenergic Receptor Blockers,Antagonists with Additional Actions
As typified by labetalol and carvedilol, these drugs not only block theβ-adrenergic receptors but have additional actions such as blockade of
the α1-adrenergic receptor, generation of nitric oxide, and decrease in
reactive oxygen species, which contribute to their unique pharmacologic actions.
Cont.
Labetalol combines nonselective β-blocking propertieswith α1-adrenergic antagonism.
It is five to seven times more potent at blocking β-adrenergic receptors compared to α1 receptors.
Because of actions at β-adrenergic and α1-adrenergic receptors, labetalol decreases peripheral resistance and blood pressure.
The drug has some direct vasodilatory properties not mediated by interaction at adrenergic receptors.
Because of these actions, labetalol can be used to treat hypertensive emergencies.
The pharmacologic effects of the β blockers
The pharmacologic effects of the β blockers occur as a result of preventing binding and subsequent receptor activation byepinephrine, norepinephrine, and exogenously administered adrenergic agonists in tissues regulated by β adrenergic receptors
Effects on the cardiovascular system
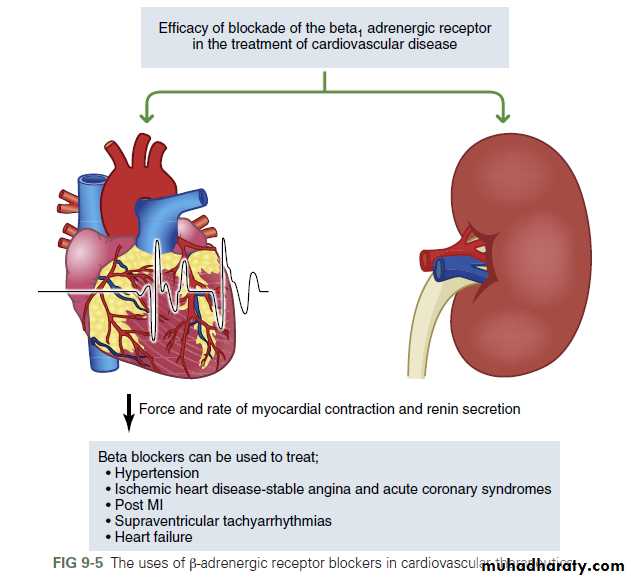
The β blockers decrease the rate and force of myocardial contraction.
The major sites of action for the negative chronotropic effects are the
β1-adrenergic receptors associated with the sinoatrial (SA) node, the
atrioventricular (AV) node, and the His-Purkinje system.
Cont.
In normotensive patients, β blockers do not normally reduce bloodpressure; however, they are highly effective in reducing blood pressure in
hypertensive patients. These agents reduce blood pressure equally in the
supine and standing positions, with little or no orthostatic hypotension.
Effects on smooth muscle
Pulmonary smooth muscleBy blocking the β2-adrenergic receptors associated with airway smooth muscle, propranolol and othernonselective β blockers prevent sympathetic stimulation of bronchiolar smooth muscle, while leaving parasympathetic activity and other bronchoconstrictive influences unchecked.
This imbalance can lead to a marked increase in airway resistance in patients with bronchospastic disorders such as asthma, chronic bronchitis, and emphysema.
Propranolol and other nonselective β blockers are contraindicated in patients with bronchospasticdisease
Cont.
Vascular smooth muscle. β2-Adrenergic receptors are also expressed on vascular smooth muscle and account for additional
unwanted side effects of nonselective β blockers. For example, these agents can exacerbate peripheral vascular disease by blocking the vasodilatory effects of the β2-adrenergic receptor. In addition, they can
potentiate the vasoconstrictor actions of neurotransmitters or drugs that activate the α1-adrenergic receptor. This includes epinephrine given with local anesthetic agents.
Gastrointestinal tract effects
Similar to other adrenergic antagonists, propranolol tends to producea relative preponderance of parasympathetic activity in the gastrointestinal
tract. The net effect is related to the amount of sympathetic
activity that is blocked, but it is usually of little importance.
Metabolic effects
Propranolol and other nonselective β blockers antagonize the β2-adrenergic receptors responsible for initiating glycogenolysis in the liver and inskeletal muscle. Hypoglycemia may result from this action, but it is rare in the nondiabetic individual.
The release of fatty acids from adipocytes by epinephrine is mediated by β1-adrenergic or β3-adrenergic receptors.
Central nervous system effects
β blockers can be used to treat a variety of disorders that have CNS involvement, including migraine headache, performance anxiety (stage fright), and benign essential tremor.Absorption, Fate, and Excretion
Most clinically approved β blockers are available in oral dosage forms.Esmolol, a selective β1 receptor antagonist with a very brief duration of action, is limited to intravenous use for the treatment of acute hypertension
and to control ventricular rate in patients with supraventricular tachyarrhythmias. Levobunolol and metipranolol are available only in solutions suitable for ophthalmic use.
Cont.
In its first pass through the liver, approximately 50% of propranolol is metabolized. The first-pass extraction can vary widely among patients, necessitating individualized dosing regimens.
Peak plasma concentrations of propranolol occur approximately 90 minutes after oral administration, with 90% of the drug bound
to plasma proteins. The half-life after oral administration is 3 to 5 hours; intravenous administration results in a half-life of 1.5 to 2 hours
Therapeutic Uses
Hypertensionβ Blockers have long been regarded as first-line agents in the treatment of hypertension
The β blockers can be used as monotherapy to control hypertension or used in combination with other drugs, such as diuretics, to produce a more vigorous antihypertensive response.
Many of the side effects associated with the
use of other antihypertensives, such as Na+ and water retention or the development of tolerance, do not occur with β blockers.The only systemic β blockers not approved for use in
hypertension are esmolol and sotalol.
Ischemic heart disease
The β blockers are first-line agents in the treatment of angina pectoris associated with atherosclerotic coronary artery disease.In this condition, there is an imbalance between the oxygen demand of the myocardium and the ability of the partially occluded coronary arteries to deliver oxygen-rich blood to the myocardial muscle.
This imbalance leads to cardiac ischemia and development of the characteristic chest pain of angina pectoris.
Cont.
Two of the major determinants of myocardial work and oxygen consumption—the force and rate of contraction—are decreased by β blockade.
Both selective and nonselective β blockers can be used effectively for this indication
Myocardial infarction
In addition to stable angina pectoris the β blockers are also drugs of choice in treatment of acute coronary syndromes to prevent myocardial infarction and the prophylaxis of reinfarction. The favorable action for this indication is related to the decrease in cardiac work and on myocardial oxygen consumption produced by the β blockers. These drugs can limit the likelihood and reduce the severity of reinfarction.The antiarrhythmic activity of the β blockers may also contribute to reducing mortality rates after myocardial infarction.
Heart failure
several clinical trials demonstratedthat β-adrenergic receptor blockers improve left ventricular function
and the symptoms of heart failure as well as decrease the progression of
the disease and, most importantly, increase patient survival.
Treatment of arrhythmias
The β blockers can be used to treat various supraventricular tachyarrhythmias,including atrial flutter and atrial fibrillation. The sympathetic nervous system richly innervates the SA and AV nodes, and the β1-adrenergic receptor is the major regulatory receptor at these sites.
Cont.
Esmolol has a short plasma halflifeand is used intravenously for rapid action in the acute management
of supraventricular tachyarrhythmias. Propranolol and acebutolol are
other members of this class widely used for their antiarrhythmic action.
Non-cardiovascular uses
Β blockers can be used to treat a wide variety of non-cardiovascular disorders
including: pheochromocytoma (administered with an α-adrenergic receptor– blocking drug) thyrotoxicosis migraine headache prophylaxis open-angle glaucoma performance anxiety (stage fright) essential tremors variceal bleeding prophylaxis
Adverse Effects
Effects on the heartAs an extension of their actions on SA and AV nodal function, β blockers
can induce bradycardia and partial to complete AV conduction
block. The abrupt withdrawal of propranolol has been linked to attacks
of angina pectoris, myocardial infarction, and sudden death, especially
in patients with angina. The chronic blockade of the β-adrenergic
receptor may induce β receptor supersensitivity, which contributes to
a rebound exacerbation of these clinical problems. Withdrawal from
β-blocking drugs should be done slowly, over 1 to 2 weeks.
In additionto the effects on conduction, β blockers can decrease myocardial contractility. The negative inotropic and chronotropic effects can contribute to the fatigue that is associated with the use of these drugs.
Effects on smooth muscle Because of the blockade of β2 receptors in blood vessels, nonselective β blockers tend to reduce adrenergic vasodilator responses of the vasculature to epinephrine. This effect is of little consequence in most
patients, even though cold hands and feet may result. In patients with peripheral vascular disease, such as Raynaud disease, worsening of the condition is likely, and β blockers, especially nonselective ones, should
be used cautiously in such patients
Bronchospasm resulting from blockade of β2 receptors is apt to
occur in patients with asthma and chronic obstructive airway diseases
such as chronic bronchitis and emphysema. This is more problematic
for nonselective β blockers. Selective β1 blockers are less likely to affect
bronchial smooth muscle and produce decreases in airways resistance.
Nevertheless, the risk of bronchoconstriction with these drugs is still
present because there is a limit to the selectivity for the β1 receptor.
Metabolic effects
A common warning sign of hypoglycemia to a diabetic patient is an increase in heart rate. Because this action is largely mediated by the β1-adrenergic receptor, this early sign of hypoglycemia is blunted by all clinically used β blockers. In addition, the effects of compensatory sympathetic stimulation and epinephrine release resulting from reduced blood glucose concentrations may be blocked in patients receiving β blockers.Central nervous system effects
Patients receiving β blockers may experience CNS depression, weakness, fatigue, sleep disturbances including insomnia and nightmares, hallucinations, dizziness, and depression.As noted earlier, a component of the fatigue symptomatology could be due to the decrease in myocardial contraction.
Cont.
Special note should be made of methyldopawhich is used to treat hypertension in pregnancy
Monoamine Oxidase Inhibitors
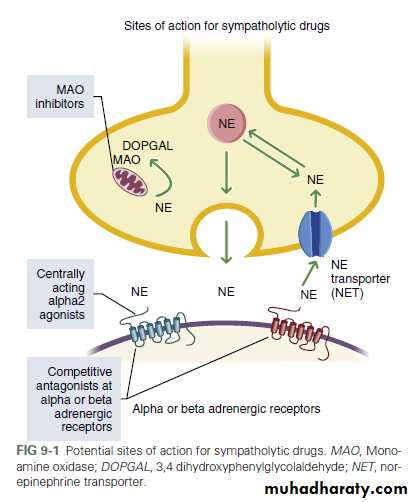
Monoamine oxidase (MAO) inhibitors are another example of drugs that have sympatholytic actions by a unique, non-receptor action.MAO is the intracellular enzyme responsible for inactivation of norepinephrine by
converting it to 3,4 dihydroxyphenylglycolaldehyde (DOPGAL
MAO is expressed in two isoforms, MAO-A and MAO-B, both in the periphery and CNS
Cont.
By poorly understood mechanisms,
MAO inhibitors reduce systemic arterial blood pressure and once were
developed with the idea of treating hypertension. Because of the potentially
serious side effects, these drugs are no longer used for this indication
Cont.
MAO inhibitors are associated with a wide constellation of sideeffects, including orthostatic hypotension, dizziness, weakness, xerostomia,
and syncope. Tremors and hallucinations have also been
reported. Most serious is the hypertensive crisis that can occur after
eating or drinking food stuffs containing substantial amounts of tyramine.
Aged cheese, liver, beer, and wines are among the most common
of these tyramine-containing foods.
Cont.
Hypertension is the result of three factors:(1) the metabolism of tyramine by MAO that would normally
occur in the gastrointestinal tract is blocked by the MAO inhibitors;(2) tyramine is an indirect-acting amine and causes release of neurotransmitter from the cytoplasmic pool of adrenergic nerve endings;
And
(3) large amounts of the transmitter accumulate in the cytoplasmic
pool of adrenergic nerve endings as a result of the inhibition of MAO.IMPLICATIONS FOR DENTISTRY
Considering the wide range of therapeutic indications for the drugs discussedin this chapter, dental practitioners are quite likely to encounter
patients taking one or more of these drugs in their practices. Dentists
must pay heed to the potential risks associated with these pathologic
conditions and the therapeutic agents used to manage them.
Physical Implications
A consideration for patients being treated with certain sympatholytics is the patient’s position during and after dental procedures.Suddenly standing upright after being in a supine position in the dental chair is apt to cause syncope.
This problem is particularly likely for the drugs more prone to cause orthostatic hypotension (e.g., α1-adrenergic receptor–blocking drugs and drugs with combined α-blocking and β receptor–blocking activity, MAO inhibitors).
Accidents ranging from chipped teeth and restorations to fractured mandibles and worse have resulted from falls.
Drug Interactions
Because nonselective β blockers inhibit β2-adrenergic receptor– mediated vasodilation, there is a risk of a hypertensive episode after administration of local anesthetic agents that contain vasoconstrictors.In this situation, the vasoconstrictor actions of epinephrine at α-adrenergic receptors are not opposed by the vasodilator actions of
β2-adrenergic receptors, resulting in an exaggerated increase in blood pressure that could be deleterious in patients with hypertension or ischemic heart disease.
Clonidine is well known to cause xerostomia. The use of clonidine- like drugs may result in clinical symptoms related to dry mouth, such as difficulty in swallowing and speech.
Long-term use of xerostomia- causing drugs is associated with a higher incidence of oral candidiasis and dental caries.