DIPHTHERIA
Session objectives• Definition
• Signs and symptoms
• Complications
• Agents
• Diagnosis
• Epidemiology (Occurrence, Reservoir, Transmission, incubation period, Communicability, Susceptibility and resistance)
• Methods of control(Preventive measures &Control of pt and contacts)
Is an acute infectious disease characterized by fever, sign and symptoms of toxemia, with an asymmetrical adherent grayish white membrane with surrounding inflammation primarily involving tonsils, pharynx, larynx, nose, S.T other MM or skin (cutaneous diphtheria), occasionally, conjunctivae or vagina.
In faucial or pharyngotonsillar diphtheria there is moderate to sever sore throat with enlarged & tender L.N. there may be swelling or oedema of the neck that may progress to air way obstruction. In nasal diphtheria it may be mild or chronic with unilateral nasal discharge.
Agent:
Corynebacterium diphtheria of mitis, gravis or intermedius biotypes.The bacilli multiply at site of entry, and elaborate a powerful cytotoxin which is responsible for
(1) local tissue destruction & formation of such membrane that is cannot be wiped away.
(2) LN enlargement and toxemia.
The inapparent infection outnumber clinical cases.
CFR: 5-10% IN UNTREATED CASES.Diagnosis: clinical suspicion, then swab for bacteriological examination. The Rx should be started even with –ve result.
Occurrence:
It is a disease of cold months in temperate zones.In tropics seasonal trends less distinct.
It is a disease of children < 15 yrs.
Adults can be affected in population with neglected immunization program.
Unapparent, cutaneous & wound diph. Are more common in tropics.
Susceptibility and resistance:
Passive maternal immunity for 6 months.Disease or inapparent infection usually but not always, induces lifelong immunity.
Immunization with toxoid produces prolonged but not lifelong immunity.
Antitoxic immunity protect against systemic disease but not against colonization in nasopharynx.
epidemics can occur in disruption of immunization program, and large scale movement of susceptible population
Reservoir: human
Mode of transmission:direct contact with case or carriers.
indirect that include; articles or raw
milk (by infected hands).
IP: 2-6 DAYS.
Period of communicability:
2-4 wks after start of illness. Antibiotic promptly terminate shedding, rarely chronic carrier may develop and shed MO for 6 months or more.
• Methods of control:
• Preventive measures.• Control of pt, contacts, environment.
• Preventive measures:
• Health education; mode of transmission, hazards and effect of vaccination.• Widespread active immunization initiated in infancy, with a formulation containing diphtheria toxoid, tetanus toxoid & either a cellular pertussis antigens (DTaP) has no SE, or a whole cell pertussis vaccine (DTP) more SE.
• 3. The following schedule are recommended for use in Iraq:
• Children <7 yrs of age (DPT):• age dose
• 2 ms 1st dose
• 4 ms 2nd dose
• 6 ms 3rd dose
• 18 ms 1st booster dose
• school entry 2nd booster dose
• * This schedule doses not need to restarted if any of them delayed. If there is side effects (DT) should be given.
For person >=7 yrs (adult Td is used, highly purified toxoid):
1st, 2nd doses at 4-8 wks interval.
3rd dose after 6 ms-1 yr after the 2nd dose.
maintenance dose of Td every 10 yrs for active protection.
4. Protection of high risk groups as; doctors & health workers by vaccination every 10 yrs.
5. Immunocompromised, HIV should be vaccinated according to same schedule (DTaP).
What's the difference between all the vaccines containing diphtheria and tetanus toxoids and pertussis vaccine?It's like alphabet soup! Here is a listing of the various products:
DTaP: Diphtheria and tetanus toxoids and acellular pertussis vaccine; given to infants and children ages 6 weeks through 6 years.
DT: Diphtheria and tetanus toxoids, without the pertussis component; given to infants and children ages 6 weeks through 6 years who have a contraindication to the pertussis component.
Tdap: Tetanus and diphtheria toxoids with acellular pertussis vaccine; given as a one-time dose to adolescents and adults.
Td: Tetanus and diphtheria toxoids; given to children and adults ages 7 years and older. Note the small “d” which indicates a much smaller quantity of diphtheria toxoid than in the pediatric DTaP formulation.
• Control of pt, contacts, environment:
• Pt. reporting: immediate.• Isolation: strict isolation for pharyngeal diph. and contact isolation in cut. diph. Until 2 –ve cultures from throat, nose, or skin taken not less than 24 hrs a part & not less than 24 hrs after cessation of antibiotic therapy. And if no lab. Facility, isolation can be end after 14 days course of appropriate antibiotic therapy.
• Concurrent then terminal disinfection of all articles.
• Specific Rx: sensitivity testing before giving antitoxin. 20,000-100,000 unit according to the severity & site of the disease.• 5. Antibiotics are not a substitute for antitoxin. Penicillin G (25,000-50,000 units/kg/day for children & 1.2 million units/kg/day for adults, IM), or Erythromycin (40-50 mg/kg/day) for 14 days.
• 6. Modified quarantine of contact by exclusion from food handling, or work with children until bacteriological examination proves them not to be carriers (modified quarantine).
• 7. Nasal & throat culture for all close contact.
• 8. Surveillance of contact for 7 days (daily examination).
9. Single dose of benzathine penicillin, 600,000 units for<6yrs, &1,200,000 units for older. {sensitive, 10 days erythromycin is recommended for all those with household exposure, regardless to their immunization status.
Tetanus
Session objectives• Definition
• Signs and symptoms
• Complications
• Agents
• Diagnosis
• Epidemiology (Occurrence, Reservoir, Transmission, incubation period, Communicability, Susceptibility and resistance)
• Methods of control(Preventive measures &Control of pt and contacts)
Tetanus is an acute disease induced by an exotoxin of the tetanus bacillus ,which grows anaerobically at the site of an injury.
*Characterized by :
1.Painful muscular contractions
Primarily of the masseter and neck muscles secondarily of trunk muscles.
2.Generlized spasms frequently induced by sensory stimuli. The spores release bacteria that spread and make a poison called tetanospasmin. This poison blocks nerve signals from the spinal cord to the muscles, causing severe muscle spasms.
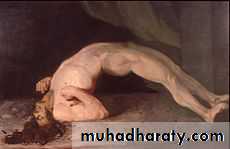
3.Typical features are position of opisthotonus and risus sardonicus expression.
Back muscle spasms often cause arching, called opisthotonos.
*Case – fatality rate = 10 – 90% according to:1.Age (high among infants and elderly).
2.Incubation period (inverse relation ).
3.Availability of experienced intensive care.
*Laboratory confirmation is of little help.
*Infections agent is clostridium tetani.
Occurrence :
*World wide sporadic disease.*More common in agriculture regions and underdeveloped areas.
*In rural and tropical areas people are especially at risk & tetanus neonatorium is common.
• *Addiction on parentral drugs can result in individual cases.
• Reservoir:
• Intestine of horses and other animals including humans.
• Soil contaminated with animal and human feces.
Mode of transmission:
1.Tetanus spores usually introduced through contaminated wound puncture .
2.Through lacerations ,burns and trivial or unnoticed wounds.
3.Through injectable contaminated street drugs.
4.Occasionaly follows surgical procedures including circumcisions.
Incubation periods:
Usually (3 -21) days .However its range is (1 day – several months .
Average is 10 days.
The shorter period means the worst prognosis.
Period of communicability :
No person to person transmission .Susceptibility and resistance :
Susceptibility is general.
Active immunity is by tetanus toxoid which persist for (10 years) after full immunization.
Transient passive immunity by tetanus immunoglobulin (TIG) or tetanus antitoxin (equine origin ).
Infants of actively immunized mothers acquire passive immunity against neonatal tetanus.
Recovery from tetanus may not result in life long immunity , thus a second attack can occur .Primary immunization after recovery is indicated.
Preventive Measures:
1.Educate public about necessity of complete immunization and risk of puncture wounds contamination that need active or passive prophylaxis.2.Universal active immunization with adsorbed tetanus toxoid protection for at least (10 years).
• 3.Prophylaxis in wound management through:-
• Careful assessment of wound state of contamination.
• Immunization status of patient.
• Proper use of tetanus toxiod and /or tetanus immunoglobulin
• Wound cleaning.
• Surgical debridement and antibiotics use.
• Control Measures:
• 1.Report to local health authority.• 2.Investigation of contacts and source of infection ( case investigation to determine circumstances of injury).
• 3.Specific treatment:-
• TIG (3000 - 6000)IU intramuscularly .( if not available give tetanus antitoxin equine origin in single large dose I.V.
• I.V. metronidazole large doses for (7-14) days.
• Wound debridment if possible
d. Maintain adequate airway and give sedation.
e. Muscle relaxant drugs with tracheotomy or nasotracheal intubation and mechanical respiration may be life saving .f. Active immunization should be initiated.
Pertussis
Whooping coughSession objectives
• Signs and symptoms
• Complications
• Agents
• Diagnosis
• Epidemiology (Occurrence, Reservoir, Transmission, incubation period, Communicability, Susceptibility and resistance)
• Methods of control(Preventive measures &Control of pt and contacts)
Pertussis, also known as whooping cough ,is an acute infection of the tracheobronchial tree a highly contagious disease caused by the bacterium Bordetella pertussis. It is known to last for a duration of approximately 6 weeks before subsiding. The disease derives its name from the "whoop" sound made from the inspiration of air after a cough.
Acute bacterial infection of respiratory system, characterized by:
catarrhal Stage; insidious onset with fever, irritating cough of 1-2 wks, thenParoxysmal stage; attacks of repeated many violent coughs without intervening inhalation, followed by characteristic whoop (loud crowing inspiration), paroxysms may end with expulsion of clear tenacious mucus, or may end with vomiting (2-8 weeks, or sometimes longer).
convalescent stage (stage of decline) (2-3 wks).
Complications:
Pneumonia, Hemorrhage, Encephalopathy, earache, or seizuresCFR: in developing countries=3.7% <1 yr.
And 1% for 1-4 yrs.Sever type &deaths occur more in:
<6 ms.
Malnourished with multiple enteric & resp. infection.
Non-immunized population.
Female more than male.
Agents
Bordetella Pertussis
B. Parapertussis which cause similar but milder disease.
Diagnosis : depend on clinical features
& culture of MO from nasopharyngeal specimens during catarrhal and early paroxysmal stage of the diseases on appropriate culture media., polymerase chain reaction (PCR), direct immunofluorescence (DFA), and serological methods.Occurrence:
Disease occur endemically&epidemically.Commonly among children <5 yrs.
Worldwide dramatically dropping in dis incidence & deaths with;
Active immunization program.
Improved nutrition.
Improved medical care.
Reservoir: human
Mode of transmission:Direct contact with respiratory discharge or droplets by airborne route.
Indirect by contaminated objects or through the air.
I.P: 6-20 Days.
Period of communicability:
Highly communicable during catarrhal stage and 1st 2 wks of paroxysmal stage without Rx.
In treated Pt; 5 days after starting erythromycin.
Susceptibility and resistance:
Universal for all non-immunized persons.No trans placental immunity (no passive maternal immunity).
One attack confers prolonged immunity.
Subsequent attack can occur.
Vaccine efficacy varies from70-90% (3 doses) then increase with the 2 booster doses.
• Methods of control
• Preventive measures:• Health education.
• Active immunization with 3 doses of DTP vaccine IM, (each dose 0.5ml), at 1-2 ms interval, starting when the infant is about 8 wks old, with other 2 booster doses at 18 ms & school entry.
• The pertussis vaccine consisting of either a killed whole cell (wP in DTP) or acellular preparation (Ap in DTP) in same doses & boosters (have less side effects & can be given to>7yrs).
• Protection of health workers during outbreaks using 7 days course of erythromycin.
DTP vaccine can be given simultaneously with: OPV, IPV
HB vaccineHib vaccine
Side effects of DTP vaccines:
1) local reactions, or sever reaction.
2) mild fever and irritability.
3) febrile seizures
4) Persistent sever screaming
5) collapse or anaphylactic reaction.
Contraindications of DTP vaccination:
The only true contraindication to immunization with ap or wp is an sever reaction, collapse or anaphylactic reaction to previous dose of vaccination.
B) Control of pt, contacts:
1. early reporting.2. respiratory isolation for pt. while suspected cases should be removed from non-immunized young infants until 5 days after starting antibiotic, or for3 wks for those not receive antibiotic
3. concurrent disinfection of articles.
4. modified quarantine: inadequately immunized household contacts<7 yrs may be excluded, from schools, for 21 days after exposure or until 5 days of a minimum 7 days course of antibiotic.5. Protection of contacts;
*by a dose DTP vaccine as soon as possible after exposure for those <7 who have not received 4 DTP doses or not received a DTP dose within 3 yrs.*by prophylactic antibiotic therapy in the early IP may prevent the disease, & to prevent antibiotic resistance cases so this measure is limited to children <1 yr, and pregnant women in the last 3 wks of pregnancy (risk of transmission to the newborn).
6. Investigation of contacts.
7. Specific Rx. By erythromycin, azithromycin, clarithromycin. For 14 days (↓communicability, but not the course of disease except in early IP and early paroxysmal stage).*Epidemic measures
1. protect preschool children by looking for unrecognized cases, and ensure adequate preventive measures for exposed children<7 yrs.2. acceleration of immunization program staring 1st dose at age of 4-6 wks of age and at 4 wks intervals, & doses should be completed.