Healing & repair
Dr Mustafa Salah Fadhil MSc, FIBMS pathCell types according to healing ability
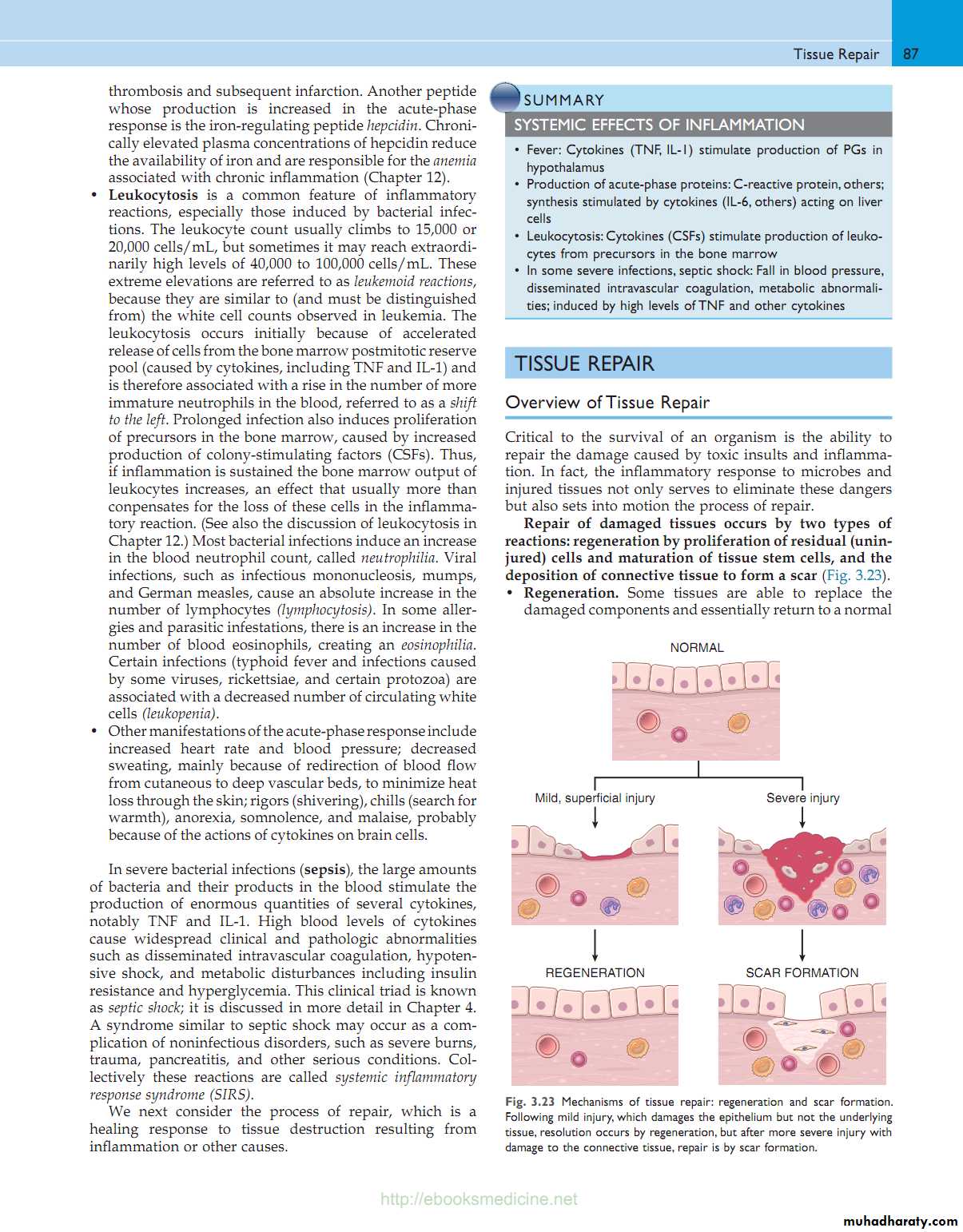
TISSUE REPAIRHealing: Replacement of dead cells & damaged ECM by healthy tissue.
2 processesRegeneration of specialized cells (same cells)
Repair: Replacement by connective tissue ( fibrosis)
TISSUE REPAIR
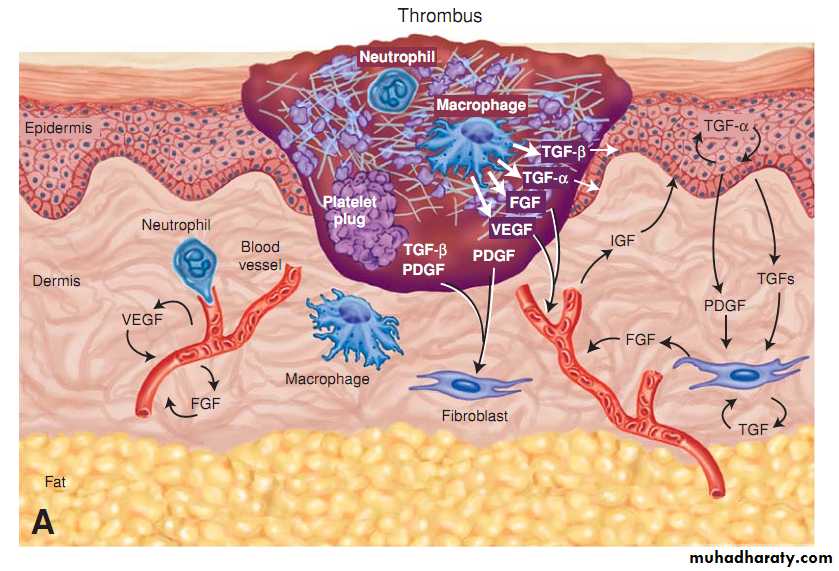
The healing process involves the production of chemical mediators that affect cell growth by binding to specific receptors. They are called growth factors
Causing:
cellular proliferation
influence cell migration & differentiationinfluence tissue remolding
Major Growth Factors (GF) Involved in Tissue RepairFactor
FunctionGrowth factors
Vascular endothelial cell growth factor (VEGF)
Stimulates angiogenesisBasic fibroblast growth factor (BFGF)
Stimulates angiogenesis
Epidermal growth factor (EGF)
Stimulates keratinocyte migrationStimulates granulation tissue formation
Platelet-derived growth factor (PDGF)
Stimulates proliferation of smooth muscle, fibroblasts, endothelial cells
Hormones
Insulin growth factor-1 (IGF-1)
Stimulates synthesis of collagenPromotes keratinocyte migration
Interleukins (IL)
IL-1
Chemotactic for neutrophilsStimulates synthesis of metalloproteinases (i.e., trace metal containing enzymes)Stimulates synthesis and release of acute phase reactants from the liverTISSUE REPAIR
1. Repair by RegenerationReplacement injured tissue by same type of original tissue cells
Labile & stable cellsinvolve 2 tissue components
Cellular proliferationECM deposition
TISSUE REPAIR
11. Repair by connective tissue, fibrosis, scar formationThree components
Granulation tissue (Angiogenesis)
Fibrosis (Migration & proliferation of fibroblast )Remodeling (fibrous tissue maturation & organization)
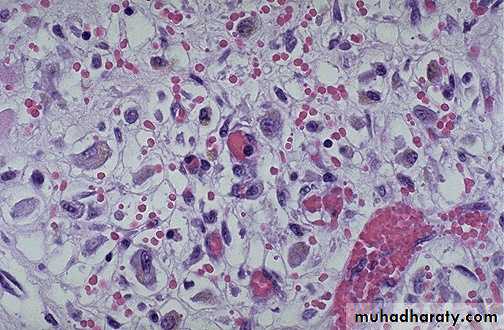
TISSUE REPAIRGranulation tissue:
“the hallmark of healing”Highly vascular tissue composed of newly formed blood vessels (i.e., angiogenesis) and activated fibroblasts
Essential for normal wound healing
Converted into scar tissue
Growth factors: FGF & VEGF
Fibrosis:
Fibroblast migration & proliferation
ECM deposition
Growth factors: PDGF, FGF, TGF-Beta, IL-1 & TNF
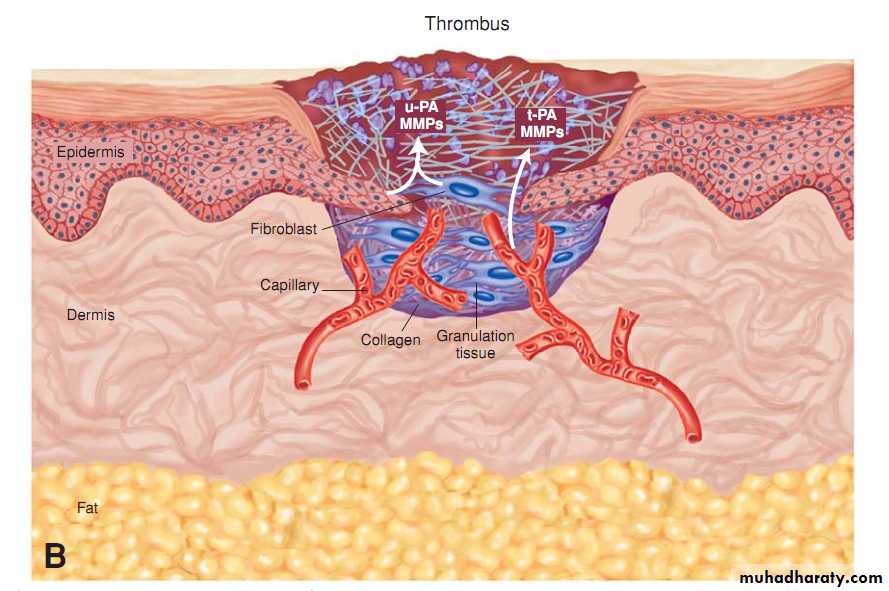
Remodeling:
Remodeling increases the tensile strength of scar tissue.
Fibrous tissue maturation & organization
Metalloproteinases (collagenases) replace type III collagen with type I collagen, increasing tensile strength to approximately 80% of the original.
Types of skin wound healing
1. Healing by primary intention (primary union):Wound edges are closely opposed by sutures
Used for clean surgical wounds
Heals in short duration
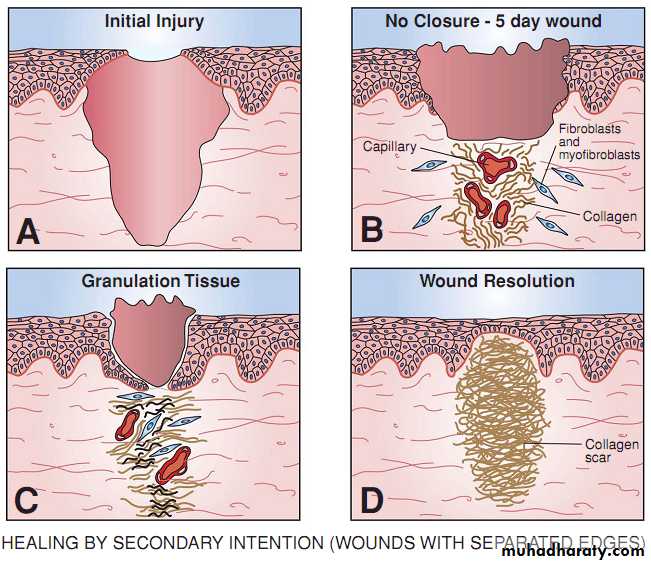
2. Healing by secondary intention (secondary union):
Wound is left openUsed for gaping (edges are widely separated) or infected & contaminated wounds
Wound takes longer to heal
1. Primary Intention
Sequence in primary intention healing of wound:
1. First day:
Blood clot develops in wound
Neutrophils infiltrate
2. Second day:
Squamous cells from basal cells layers of opposing skin migrate under the fibrin clot and seal off the wound after 48Macrophages emigrate into wound
1. Primary Intention
3. Third day:1: Beginning of granulation tissue formation:
A. Angiogenesis due to bFGF
B. Fibroblasts lay down type III collagen
II: fibronectin is key chemical mediator:
A. Derived from macrophages/ fibroblasts/ endothelial cells
B. Chemotactic to fibroblasts & macrophages
1. Primary Intention
4. 4th to 6th day: peaks of granulation formation
5. 7th -10th days: tensile strength 10% of normal
6. weeks to months:
A. Collagenization:
1. Collagenases are important in remodelization (Zn is cofactor)
2. Type III collagen is replaced by type 1 to increase tensile strength
B. Maximum tensile strength is 80 % after 3months
Scar tissue is devoid of adnexal structures (e.g., hair, sweat glands) and inflammatory cells.
2. Secondary Intention
More intense inflammatory reaction than primary healingIncreased amount of granulation tissue formation than in primary healing
Wound contraction caused by increased numbers of myofibroblasts
Occurs when injury is severe or persistent
Tissue in a third-degree burn cannot be restored to normal owing to loss of skin, basement membrane, and connective tissue infrastructure.
2 to 4 days
TISSUE REPAIR
Day 4 to 8TISSUE REPAIR
wound healing
E.g, surgical woundNarrow incisional space resulting in a limited inflammatory reaction
Small amount of granulation tissue in incisional space
Limited amount of wound contraction
Healing in short time
E.g. traumatic wound
Large tissue defect resulting in a more intense inflammatory reaction
Large amount of granulation tissue
More amount of wound contraction
Healing take long time
Primary Union
(Healing by 1st intention)Secondary Union
(Healing by 2ry intention)
TISSUE REPAIR
TISSUE REPAIR
Healing of bone fractures
I. Healing by primary union: rare e.g. in compression fracturesII. Healing by formation of callus. Similar to healing by secondary union which includes:
Injury----> Fracture----> formation of blood clot
Inflammation start-----> removal of blood clot
Replacement by granulation tissue consisting of capillary and mesenchymal cells (Osteoblast) (procallus)
Formation of collagen fibers and Osteomucin (Osteoid tissue) (callus)
Calcification----------> Woven bone
Removal of woven bone and replacement by lamellar bone
Complication of healing
1.Infections ( S aureus)2.Wound dehiscence
3.Implantation dermoid
4.Keloid & hypertrophic scars
5.Painful scar.
6.Pigmented scar.
7.Weak scar. ( incisional hernia)
8.Cicatrisation
9.Neoplastic changes (marjolin ulcer)
10.Exuberant granulation tissue
Factors That Adversely Affect Wound Healing.
• Infection
• Most common cause of impaired wound healing
• Staphylococcus aureus most common.
• Poor blood supply (ischemia)
• Presence of foreign material
• Presence of necrotic tissue
• Movement in injured area
• Irradiation
• Tension in injured area
• Advanced age
• Protein malnutrition
• Vitamin C deficiency :decreased cross-linking in collagen.
• Zinc deficiency :
• Corticosteroid :Interfere with collagen formation and decrease tensile strength
• Diabetes mellitus :increases susceptibility to infection by decreasing blood flow to tissue and increasing tissue levels of glucose.
• Cytotoxic (anticancer) drugs
• Severe anemia
Local
Systemic
Thanks
Classification of nerve injury & healingSlight injury affects myelin
More severe injury affects the axonThe most severe injury disrupts connective tissue.
Peripheral nerve transection
Distal degeneration of the axon (called wallerian degeneration) and myelin sheathProximal axonal degeneration up to the next node of Ranvier
Macrophages and Schwann cells phagocytose axonal/myelin debris.
Muscle undergoes atrophy in ∼15 days.
Nerve cell body undergoes central chromatolysis.
Nerve cell body swells.
Nissl bodies (composed of rough endoplasmic reticulum and free ribosomes) disappear centrally.
Nucleus is peripheralized.
Schwann cells proliferate in the distal stump.
Axonal sprouts develop in the proximal stump and extend distally using Schwann cells for guidance.
Regenerated axon grows 2 to 3mm/day.
Axon becomes remyelinated.
Muscle is eventually reinnervated.