Infectious Diseaseslec. 1By: dr. Zahraa Marwan
Infection: is defined as the invasion of living tissue by m.o. or its products (commensals or pathogenic) followed by local reaction which may be associated with general reaction.Commensals microorganisms: are those can infect human body and be harmless to the body ( some are present normally within the human body ). When commensal microorganisms cause diseases at that time they called opportunistic infections.
The microorganisms cause diseases called pathogens
The outcome of infection depends on the complex balance between the aggressive mechanisms of the m.o. & the defense mechanisms of the host
Factors influencing the infection:
1- Microorganism factors :1. Dose: number of m.o entering the body
2. virulence: their capacity to cause diseases.
3. Invasiveness: ability of m.o to multiply & spread in the body.
4.Transmission: ability of m.o to pass to another suitable host (microbes enter the host through: inhalation, ingestion, sexual intercourse, inoculation, bite and injection).
2-Host Factors:
(defense mechanisms)A- Nonspecific defense mechanism:
1. Mechanical barriers: e.g. intact skin & mucous membrane of GIT, respiratory system…..
2. Glandular secretion: acidity of gastric juices ,acidity of sweat ,secretory IgA antibodies found in saliva , tear ,intestinal contents & milk.
3. Secretion currents: flow of tear, mucus, flow of urine & saliva. diarrhea , movement of cilia.
4. Phagocytosis: by macrophages & neutrophils.
B- Specific defense (Immune response): by cell-mediated & humeral immunity.
3- Other factors:
Local factors: e.g. ischemia & foreign body promote infection.Systemic factors: e.g., malnutrition, diabetes mellitus, chronic alcoholism & malignancy.
Age: both very young & very old have increasing risk of infection.
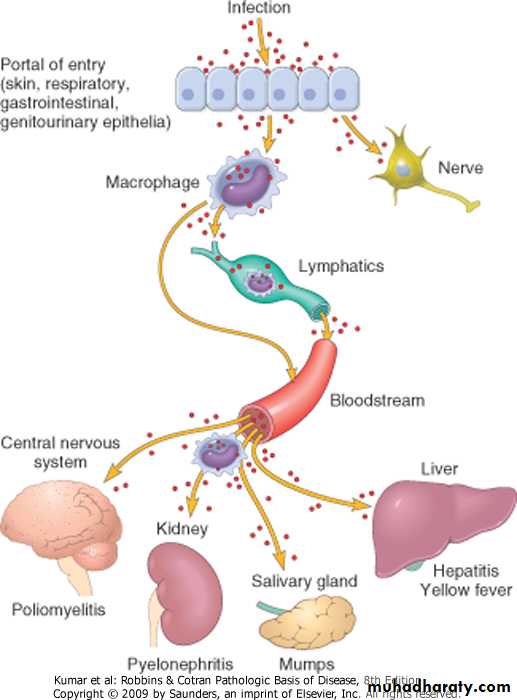
Drugs: e.g. appropriate antimicrobial drugs eradicate many susceptible microorganism.Routes of entry and dissemination of microbes
Results of infection:
1.Eradication: most infections end by total eradication at the site of entry.2. Persistence of infection: either in form of carrier state or mild chronic forms .
3. Spread: to other parts of the body:-direct spread as in cellulitis.
-lymphatic spread
-blood spread
4. Host death: in severe infection e.g. tetanus & diphtheria.
Tissue response ( microsopical ) responses to infections
There are 5 major histological patterns of tissue reaction in infections:1-Suppurative inflammation: characterized by production of pus (pyogenic bacteria) .
2-Chronic inflammation & scarring, is the final common pathway of many infections as in viruses, schistosomiasis & tuberculosis. .
3-Mononuclear& Granulomatous characterized by formation of granuloma as TB, chronic abscess.
4-Cytopathic- Cytoproliferative inflammation.
, usually produced by viruses.
5-Necrotizing inflammation caused by powerful toxins e.g. Cl. Perfringens lead to gangrene & parasite (Entamoeba histolytica).
Bacterial infections
Classification of BacteriaBacteria are classified on several criteria:
Gram stain: bacteria are either gram (-) or gram(+)
Shape: bacteria are classified as cocci, bacilli (rods), vibrios, spirochetes.Growth requirements: bacteria are classified as:
-Aerobic-Anaerobic
• Bacteria damage the tissue through several mechanisms:
1- Release toxins that kill cells. (exotoxin & Endotoxin)
2- Release lytic enzymes, includes proteases, hyaluronidase, coagulase & fibrinolysins that destroy the tissue & facilitate the spread of bacteria
3- Elicit an inflammatory reaction that may destroy not only the bacteria but also the infected tissue.
4-Elicit an immune reaction that may damage the tissues carrying the same antigen as the bacterium (“cross reactivity”).
Bacterial infection is divided into:
1- Acute.2- Chronic.
Acute Bacterial Infection:1-Catarrhal: affect mucus membrane.
• 2-Serous: Affect serous cavities and produce serous fluid
3-Pseudomembranous: Characterized by formation of peudomembrane as in diphtheria.
4-Pyogenic or suppurative (Pus producing) e.g. abscess. M.O stimulate the secretion of IL 1 & TNF which stimulate complement, this attract neutrophil which secrets lytic enzyme, destroy tissue & form abscess.
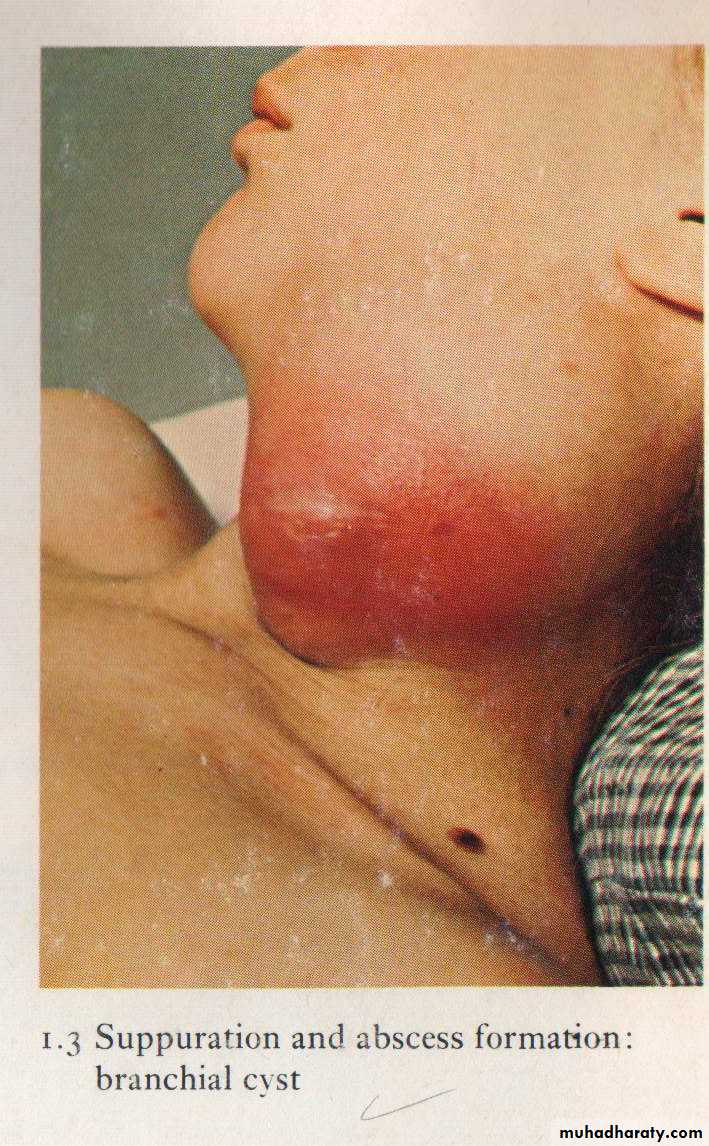
Localization of pus leads to abscess formation which appear here as red congested Swelling at the side of the neck
Perimandibular abscess in the chin region (redness, swelling)
This is an example of pseudomembranous of the colon.
The mucosal surface is hyperemic and is partially covered by a thick membrane like yellow-green exudate.Bacterial infection of the blood
* Classified into:-Bacteraemia
-Septicaemia
-Pyaemia-Toxaemia : presence of toxin in blood e.g. Diphtheria.
1-Bacteraemia
Presence of small numbers of bacteria in the blood without multiplication.
Patients have sub clinical or minor symptoms & lesion.
E.g., Strept. viridans in blood after vigorous brushing of teeth with dental sepsis. These bacteria(low virulent) are destroyed rapidly in blood because of antibodies, complement, & circulating macrophages.
It is important because it may settle in various parts of the body & cause localized lesion e.g. infective endocarditis.
2-Septicemia
Multiplication of bacteria in the blood of highly pathogenic bacteriaSerious infection with profound toxemia in which bacteria have overwhelmed the host defenses. It results in serious consequences which may end in death.
Cliniclly: Tachycardia, hypotension, multiple small hemorrhages due to capillary endothelial damage &
shock
3-Pyaemia (pus in the blood)
* Bacteria invade & multiply in a thrombus which then becomes heavily infiltrated by neutrophils & broken down by their digestive enzymes.* Small fragments of the soften septic thrombus may then break away & be carried off in the blood
Results in the developing of multiple & wide spread abscesses in the affected organs.
Abscess containing pusWall of abscess compose of fibrous tissue
Gangrene
GangreneDigestion of dead tissue by saprophytic bacteria in living body (necrosis with putrefaction ) .
Types of gangrene :
Primary
Secondary
1) Primary Gangrene
It is brought about by infection with Clustridia species (anaerobic gram-positive spores forming bacteria) which both kill the tissue by secreting potent exotoxins & then invade & digest the dead tissue.• Cl perfringes (welchii) & Cl. septicum→cellulitis & gas gangrene(life-threatening).
• Cl. Septicum are intestinal commensals in man and animals and because they are anaerobic they can’t multiply in oxygenated environment , so they need dead tissue (as in dirty wound or lacerated wounds) in order to multiply and cause gas gangrene. .
Pathogenesis
Cl. produce different strong types of exotoxins like:1- Lecithinase → causing cell wall damage by lyses of phospholipids .
2- Collagenase & hyaluronidase → digest extracellular matrix protein and collagen .
• Clinically a black discoloration and bad odor at the affected site like the skin and subcutaneous tissue , intestine ……etc
Cl. welchii ferments sugar producing H2 & CO2 which collect as bubbles in the dead tissue and can easily be detected by palpation ( gas gangrene).
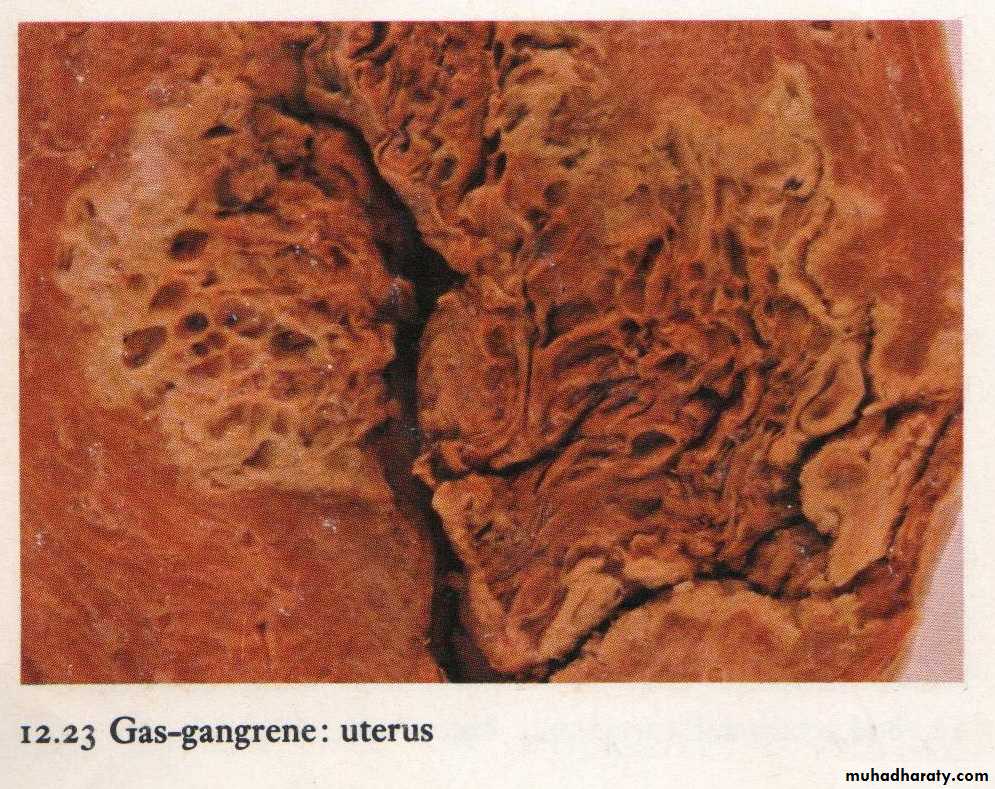
Gas gangrene of the uterus, note the gas within the necrotic tissue produced by clostridia species.
2) Secondary Gangrene
This type of gangrene is characterized by necrosis due to some other causes, usually loss of blood supply from vascular obstruction or tissue laceration & saprophytic bacteria then digest the dead tissue.2 types:
1) wet gangrene
2) dry gangrene
Types of secondary gangrene
.• 2) Dry gangrene
• 1) Wet gangrene
Contagious childhood bacterialdiseases:
Haemophilus influenzae caused Meningitis, upper- and lower-respiratory tract infectionsBordetella pertussis caused Whooping cough
Corynebacterium diphtheriae caused Diphtheria
• Diphtheria:
Diphtheria is an acute, communicable disease caused by Corynebacterium diphtheriae.The disease is generally characterized by local growth of the bacterium in the pharynx with pseudomembrane formation or, less commonly, in the stomach or lungs; systemic dissemination of toxin then invokes lesions in distant organs.
Acute disease of the upper respiratory tract usually involves one or more of the following: tonsillar zones, larynx, soft palate, uvula, and nasal cavities.
Diphtheritic laryngitis has fortunately become uncommon because of the widespread immunization of young children against diphtheria toxin.
After it is inhaled, Corynebacterium diphtheriae implants on the mucosa of the upper airways, where it elaborates a powerful exotoxin that causes necrosis of the mucosal epithelium, accompanied by a dense fibrinopurulent exudate, to create the classic superficial, dirty-gray pseudomembrane of diphtheria.
The major hazards of this infection are sloughing and aspiration of the pseudomembrane (causing obstruction of major airways) and absorption of bacterial exotoxins (producing myocarditis, peripheral neuropathy, or other tissue injury).
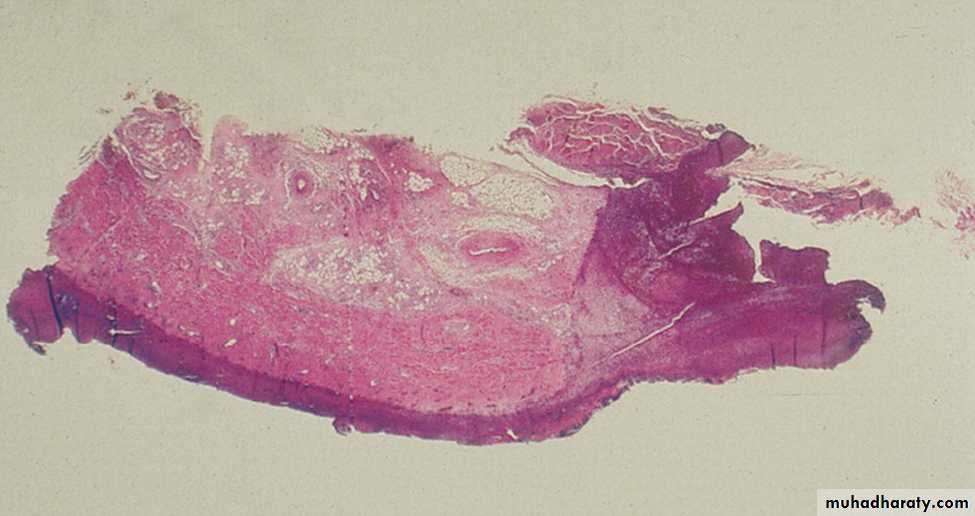
Pharyngeal pseudomembrane. Epithelium is absent; at one side, inflammatory exudate extends to underlying muscle