Dr. Ahmed Saleem
FICMS
TUCOM / 3rd Year / 2015
SURGICAL INFECTIONS
Historical Background
The body of knowledge that led to the present field of surgical infectious disease was derived from
the evolution of germ theory and antisepsis.
A number of observations by nineteenth-century physicians and investigators were critical to our
current understanding of the pathogenesis, prevention, and treatment of surgical infections:
Ignaz Semmelweis, noticed that the mortality from puerperal ("childbed") fever.
Louis Pasteur and the germ theory.
Joseph Lister and the use of carbolic acid as antiseptic.
Robert Koch and the Koch's postulates
Charles McBurney and source control surgery
The discovery of sulphonamide chemotherapy in the mid-twentieth century and the discovery of the
antibiotic penicillin that was attributed to Alexander Fleming in 1928, but it was not isolated for
clinical use until 1941 by Florey and Chain.
William Osler and the body's response to infection
Definitions
Sterilization is removal of all viable microorganisms, vegetative, and spores.
1) Heat: Dry heat (e.g. incineration, flaming to red hot) is effective, but rarely useful. Dry heat requires
temperatures of 160°C for at least 60min. Moist heat (e.g. autoclave heating using pressurized steam
121 C
o
, at 15min) is effective and useful, especially in operating theatres.
2) Irradiation: Gamma radiation: Effective for inorganic materials.
3) Filtration: Air or fluids can be sterilized by ultrafine membrane filters.
Disinfection is the removal of actively dividing vegetative microorganisms.
Acids/alkalis e.g. bleach. Effective for non-human contact use.
Alcohols/phenols, e.g.
Ethyl alcohol—skin swabs.
Alcohol solutions (Aqagel)—hand disinfection.
Carbolic.
Chloroxylenols (Dettol).
Phenol (Clearsol).
Oxidizers, e.g.
Povidone–iodine (Betadine)—skin disinfection/surgical scrubbing.
Hydrogen peroxide (H
2
O
2
)—superficial wound cleansing.
Aldehydes (Cidex)—surgical instruments such as endoscopes.
Cationic solutions, e.g. Chlorhexidine—antiseptic washes.
Organic dyes, e.g. Proflavine.
Antisepsis is the process whereby the risk of medical cross-infection by microorganisms is reduced.
Always remove gross contamination with simple soap first.
Use high potency acid/alkali disinfection on inert surfaces.
Use less corrosive oxidizers on delicate inert materials.
Use weak alcohols, oxidizers for skin cleansing.
Page 1 of 11

Pathophysiology
Infection is defined by identification of microorganisms in host tissue or the bloodstream, plus an
inflammatory response to their presence.
Microorganisms are normally prevented from causing infection in tissues by intact epithelial surfaces, most
notably the skin. These surfaces are broken down by trauma or surgery. In addition to these mechanical
barriers, there are other protective mechanisms, which can be divided into:
chemical: low gastric pH
humoral: antibodies, complement and opsonins
cellular: phagocytic cells, macrophages, polymorphonuclear cells and killer lymphocytes.
All these natural mechanisms may be compromised by surgical intervention and treatment.
Reduced resistance to infection has several causes:
Metabolic: malnutrition (including obesity), diabetes, uremia, jaundice
Disseminated disease: cancer and acquired immunodeficiency syndrome (AIDS)
Iatrogenic: radiotherapy, chemotherapy, steroids
Gut failure and Bacterial translocation: When enteral feeding is suspended during the perioperative
period, and particularly with underlying disease such as cancer, immunosuppression, shock or sepsis,
bacteria (particularly aerobic Gram-negative bacilli) tend to colonize the normally sterile upper
gastrointestinal tract. They may then translocate to the mesenteric nodes and cause the release of
endotoxins (lipopolysaccharide in bacterial cell walls), which can be one cause of a harmful systemic
inflammatory response through the excessive release of proinflammatory cytokines and activation of
macrophages.
Opportunistic infection: In the circumstances of reduced host resistance to infection, microorganisms that
are not normally pathogenic may start to behave as pathogens. This is known as opportunistic infection.
Opportunistic infection with fungi is an example, particularly when prolonged and changing antibiotic
regimens have been used.
Decisive period: There is a delay before host defenses can become mobilized after a breach in an epithelial
surface, whether caused by trauma or surgery. The acute inflammatory, humoral and cellular defenses take
up to 4 hours to be mobilized. This is called the ‘decisive period’, and it is the time when the invading
bacteria may become established in the tissues. Strategies aimed at preventing infection from taking a hold
become ineffective after this time period. It is therefore logical that prophylactic antibiotics should be given
to cover this period and that they could be decisive in preventing an infection from developing.
Microbiology of Infectious Agents
Bacteria
Bacteria are responsible for the majority of surgical infections. Specific species are identified using Gram's
stain and growth characteristics on specific media. The Gram's stain is an important evaluation that allows
rapid classification of bacteria by color. This color is related to the staining characteristics of the bacterial
cell wall: gram-positive bacteria stain blue and gram-negative bacteria stain red. Bacteria are classified
based upon a number of additional characteristics including morphology (cocci and bacilli), the pattern of
division [e.g., single organisms, groups of organisms in pairs (diplococci), clusters (staphylococci), and chains
(streptococci)], and the presence and location of spores.
Page 2 of 11

Streptococci
Streptococci form chains and are Gram positive on staining. The most important is the β-
hemolytic Streptococcus, which resides in the pharynx of 5–10 % of the population. In the
Lancefield A–G carbohydrate antigens classification, it is the group A Streptococcus, also called
Streptococcus pyogenes, that is the most pathogenic. It has the ability to spread, causing
cellulitis, and to cause tissue destruction through the release of enzymes such as streptolysin,
streptokinase and streptodornase. Streptococcus faecalis is an enterococcus in Lancefield group
D. It is often found in synergy with other organisms, as is the γ-haemolytic Streptococcus and
Peptostreptococcus, which is an anaerobe. Both Streptococcus pyogenes and Streptococcus
faecalis may be involved in wound infection after large bowel surgery.
Staphylococci
Staphylococci form clumps and are Gram positive. Staphylococcus aureus is the most important
pathogen in this group and is found in the nasopharynx of up to 15 % of the population. It can
cause exogenous suppuration in wounds (and implanted prostheses). Strains resistant to
antibiotics e.g. (Methicillin Resistant Staphylococcus aureus) MRSA can cause epidemics and
more severe infection. Infections are usually suppurative and localized. Most hospital
Staphylococcus aureus strains are now β-lactamase producers and are resistant to penicillin, but
most strains (MRSA) remain sensitive to flucloxacillin, vancomycin, aminoglycosides, some
cephalosporins and fusidic acid (used in osteomyelitis). Staphylococcus epidermidis (previously
Staphylococcus albus), also known as coagulase-negative staphylococci (CNS), was regarded as a
commensal but is now recognised as a major threat in prosthetic (vascular and orthopedic)
surgery and in indwelling vascular catheters.
Clostridia
Clostridial organisms are Gram-positive, obligate anaerobes, which produce resistant spores. C.
perfringens is the cause of gas gangrene, and C. tetani causes tetanus after implantation into
tissues or a wound. C. difficile is the cause of pseudomembranous colitis.
Aerobic Gram-negative bacilli (AGNB)
These bacilli are normal inhabitants of the large bowel. E. coli and Klebsiella spp. are lactose
fermenting; Proteus is non-lactose fermenting. Most organisms in this group act in synergy with
Bacteroides to cause surgical site infections (SSIs) after bowel operations (in particular,
appendicitis, diverticulitis and peritonitis). E. coli is a major cause of the health care associated
infection (HAI) of urinary tract infection, although most AGNB may be involved, particularly in
relation to urinary catheterization. Pseudomonas spp. tend to colonize burns and tracheostomy
wounds, as well as the urinary tract. Once Pseudomonas has colonized wards and intensive care
units, it may be difficult to eradicate. Hospital strains become resistant to β-lactamase as
resistance can be transferred by plasmids. The aminoglycosides are effective, but some
cephalosporins and penicillin may not be. Many of the carbapenems (e.g. meropenem) are
useful in severe infections, whereas the quinolones have been made ineffective through their
overuse.
Bacteroides
Bacteroides are non-spore-bearing, strict anaerobes that colonize the large bowel, vagina and
oropharynx. Bacteroides fragilis is the principal organism that acts in synergy with AGNB to
cause SSIs, including intra-abdominal abscesses, after colorectal or gynecological surgery. They
are sensitive to the imidazoles (e.g. metronidazole) and some cephalosporins (e.g. cefotaxime).
Page 3 of 11

Viruses
Due to their small size and necessity for growth within cells, viruses are difficult to culture, requiring a
longer time than is typically optimal for clinical decision making. Previously, viral infection was identified by
indirect means (i.e., the host antibody response). Recent advances in technology have allowed for the
identification of the presence of viral DNA or RNA using methods such as polymerase chain reaction. Most
viral infections in surgical patients occur in the immunocompromised host, particularly those receiving
immunosuppression to prevent rejection of a solid organ allograft. Relevant viruses include adenoviruses,
cytomegalovirus, Epstein-Barr virus, herpes simplex virus, and varicella-zoster virus. Surgeons must be
aware of the manifestations of hepatitis B and C virus, as well as HIV infections, including their capacity to
be transmitted to health care workers.
Local and systemic presentation
Cellulitis and lymphangitis: Cellulitis is the non-suppurative invasive infection of tissues. There is poor
localization in addition to the cardinal signs of inflammation. Spreading infection presenting in surgical
practice is typically caused by organisms such as β-hemolytic streptococci, staphylococci and C. perfringens.
Tissue destruction, gangrene and ulceration may follow, which are caused by release of proteases. Systemic
signs (the old-fashioned term toxemia) are common, with chills, fever and rigors. These follow the release
of toxins into the circulation, which stimulate a cytokine-mediated systemic inflammatory response even
though blood cultures are negative.
Lymphangitis is part of a similar process and presents as painful red streaks in affected lymphatics. Cellulitis
is usually located at the point of injury and subsequent tissue infection. Lymphangitis is often accompanied
by painful lymph node groups in the related drainage area.
Localization of infection/Abscess formation: An abscess presents all the clinical features of acute
inflammation originally described by Celsus: calor (heat), rubor (redness), dolour (pain) and tumour
(swelling). To these can be added functio laesa (loss of function: if it hurts, the infected part is not used).
They usually follow a puncture wound of some kind, which may have been forgotten, as well as surgery, but
can be metastatic in all tissues following bacteremia. Pyogenic organisms, predominantly Staphylococcus
aureus, cause tissue necrosis and suppuration. Pus is composed of dead and dying white blood cells that
release damaging cytokines, oxygen free radicals and other molecules. An abscess is surrounded
by an acute inflammatory response composed of a fibrinous exudate, edema and the cells of acute
inflammation. Granulation tissue (macrophages, angiogenesis and fibroblasts) forms later around the
suppurative process and leads to collagen deposition. If it is not drained or resorbed completely, a chronic
abscess may result. If it is partly sterilized with antibiotics, an antibioma may form. Abscesses contain
hyperosmolar material that draws in fluid. This increases the pressure and causes pain. If they spread, they
usually track along planes of least resistance and point towards the skin. Wound abscesses may discharge
spontaneously by tracking to a surface, but may need drainage through a surgical incision. Most abscesses
relating to surgical wounds take 7–10 days to form after surgery.
Page 4 of 11
Systemic inflammatory response syndrome (SIRS) and sepsis:
Systemic inflammatory response syndrome (SIRS) is a systemic manifestation of infection is mediated by
the production of a cascade of proinflammatory mediators produced in response to exposure to microbial
products e.g.
lipopolysaccharide (endotoxin) derived from gram-negative organisms.
Patients have developed sepsis if they have met clinical criteria for SIRS and have evidence of a local or
systemic source of infection.
Criteria for SIRS
Two of:
hyperthermia (>38°C) or hypothermia (<36°C)
tachycardia (>90/min, no β-blockers)
tachypnea (>20/min)
white cell count >12 × 10
9
/l or <4 × 10
9
/l
Infections of Significance in Surgical Patients
1 - Surgical Site Infections (SSI)
SSIs are infections of the tissues, organs, or spaces exposed by surgeons during performance of an invasive
procedure. SSIs are classified into incisional and organ/space infections, and the former are further
subclassified into superficial (limited to skin and subcutaneous tissue) and deep incisional categories. By
definition, an incisional SSI has occurred if a surgical wound drains purulent material or if the surgeon
judges it to be infected and opens it.
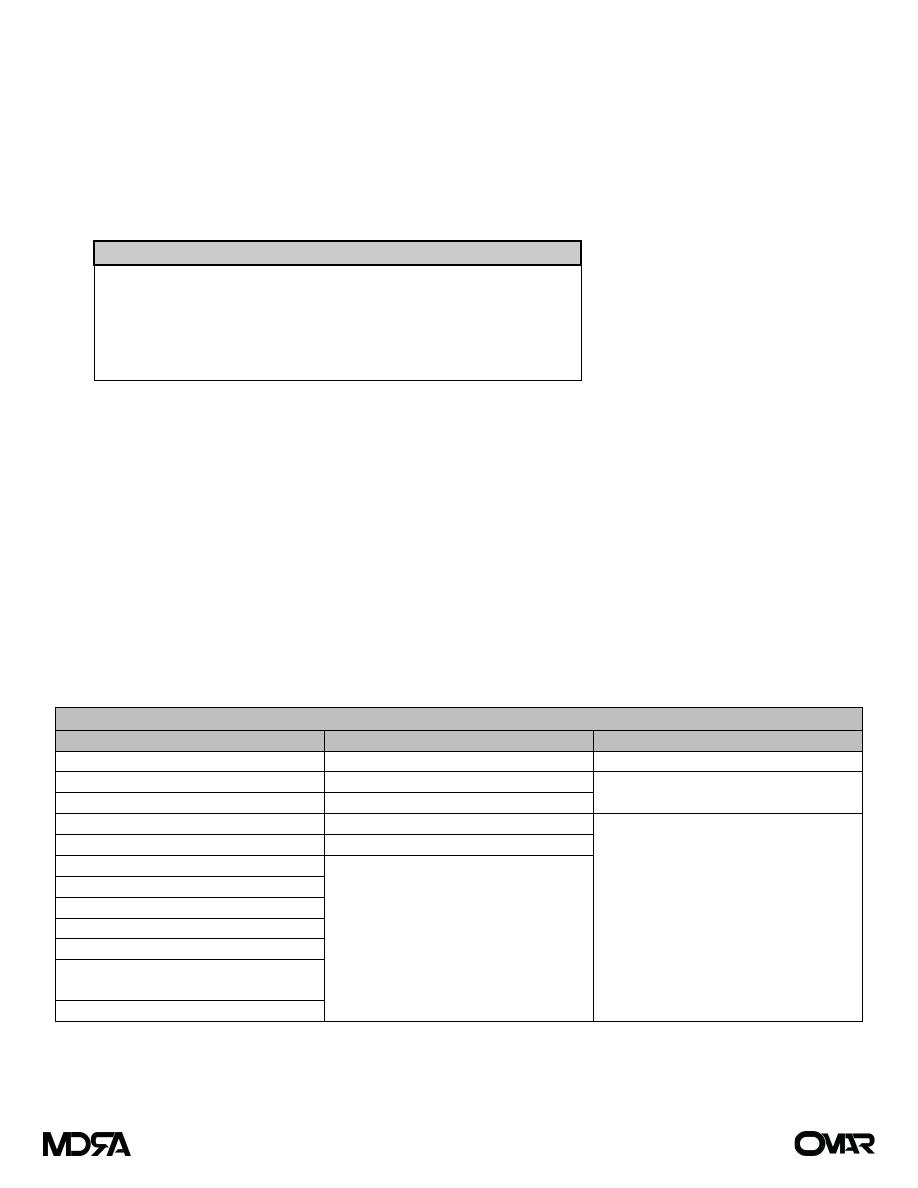
Risk Factors for Development of Surgical Site Infections
Patient factors
Local factors
Microbial factors
Older age
Poor skin preparation
Toxin secretion
Immunosuppression
Contamination of instruments
Prolonged hospitalization (leading to
nosocomial organisms)
Obesity
Inadequate antibiotic prophylaxis
Diabetes mellitus
Prolonged procedure
Resistance to clearance (e.g., capsule
formation)
Chronic inflammatory process
Local tissue necrosis
Malnutrition
Hypoxia, hypothermia
Peripheral vascular disease
Anemia
Radiation
Chronic skin disease
Carrier state (e.g., chronic
Staphylococcus carriage)
Recent operation
Page 5 of 11
Classification:
According to the presentation: A major SSI is defined as a wound that either discharges
significant quantities of pus spontaneously or needs a secondary procedure to drain it.
The patient may have systemic signs, such as tachycardia, pyrexia and a raised white
count. Minor SSI may discharge pus or infected serous fluid but should not be associated
with excessive discomfort, systemic signs or delay in return home.
The differentiation between major and minor and the definition of SSI is important in
audit or trials of antibiotic prophylaxis.
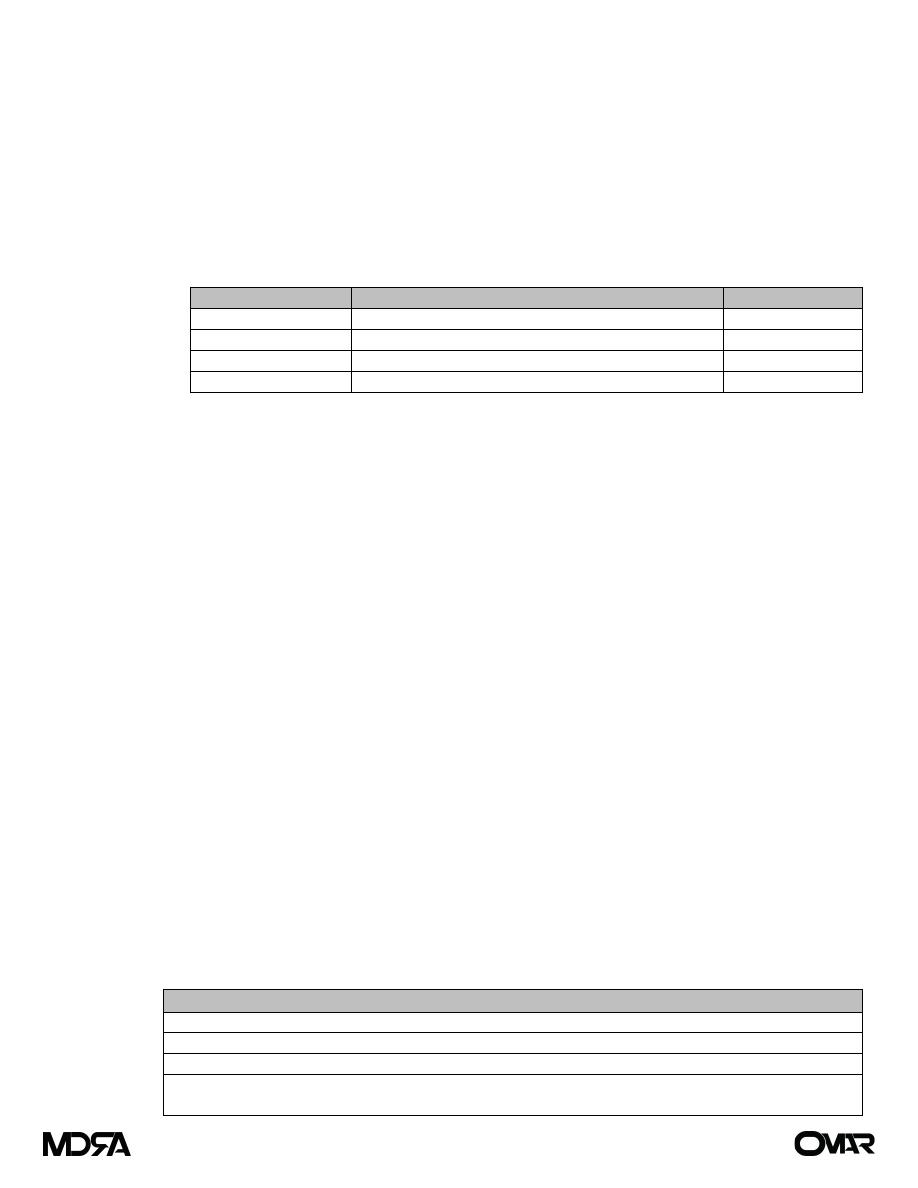
According to the presumed magnitude of the bacterial load at the time of surgery:
Wound Class
Type of surgery
Infection rate (%)
Clean
no viscus opened
1–2
Clean-contaminated
viscus opened, minimal spillage
<10
Contaminated
open viscus with spillage or inflammatory disease
15–20
Dirty
pus or perforation, or incision through an abscess
<40
Treatment of SSI:
Now that patients are discharged more quickly after surgery and many procedures are
performed as day cases, many SSIs are missed by the surgical team unless they undertake a
prolonged and carefully audited follow up with primary care doctors. Suppurative wound
infections take 7–10 days to develop, and even cellulitis around wounds caused by invasive
organisms (such as the β-hemolytic Streptococcus) takes 3–4 days to develop.
Major surgical infections with systemic signs, evidence of spreading infection, cellulitis or
bacteremia need treatment with appropriate empirical antibiotics. It is illogical to withhold
antibiotics until the results of culture and sensitivity are available.
If an infected wound is under tension, or there is clear evidence of suppuration, sutures or clips
need to be removed, with curettage if necessary, to allow pus to drain adequately. When taking
pus from infected wounds, specimens should be sent fresh for microbiological culture.
In severely contaminated wounds, such as an incision made for drainage of an abscess, it is
logical to leave the skin open. Delayed primary or secondary suture can be undertaken when
the wound is clean and granulating.
Prevention of SSI:
Maneuvers to diminish the presence of exogenous (surgeon and operating room environment) and
endogenous (patient) microbes are termed prophylaxis, and consist of the use of mechanical,
chemical, and antimicrobial modalities, or a combination of these methods.
Prophylactic antibiotics: If antibiotics are given to prevent infection after surgery or
instrumentation, they should be used when local wound defenses are not established (the
decisive period). Ideally, maximal blood and tissue levels should be present at the time at
which the first incision is made and before contamination occurs.
Criteria for choice of antibiotics for prophylaxis
Empirical cover against expected pathogens
Single-shot intravenous administration at induction of anesthesia
Repeat only during long operations or if there is excessive blood loss
Continue as therapy if there is unexpected contamination or if a prosthetic is implanted in a patient
with a septic source
Page 6 of 11

Preoperative preparation: *
Short preoperative hospital stay lowers the risk of acquiring multiply resistant organisms
and the acquisition of health care associated infections (HAI).
Medical and nursing staff should always wash/gel their hands after any patient contact.
Staff with open, infected skin lesions should not enter the operating theatre. Ideally,
neither should patients, especially if they are having a prosthesis implanted.
Antiseptic baths (usually chlorhexidine), although there is no hard evidence for their
value in reducing wound infections.
Preoperative skin shaving should be undertaken in the operating theatre immediately
before surgery as the SSI rate after clean wound surgery may be doubled if it is
performed the night before; minor skin injury enhances superficial bacterial colonization.
Cream depilation is messy and hair clipping is best, with the lowest rate of infection.
Scrubbing and skin preparation: For the first operation of the day, aqueous antiseptics
should be used for hand washing, and the scrub should include the nails. Subsequent
scrubbing should merely involve washing to the elbows, as repeated extensive scrubbing
releases more organisms than it removes.
One application of an alcoholic antiseptic is adequate for skin preparation of the
operative site. This leads to a more than 95 per cent reduction in bacterial count.
Intraoperative: *
Numbers of staff in the theatre and movement in and out of theatre should be kept
to a minimum.
Careful and regular surveillance is needed to ensure the quality of theatre ventilation,
instrument sterilization and aseptic technique.
Operator skill in gentle manipulation and dissection of tissues and dead spaces and
hematomas should be avoided and the use of diathermy kept to a minimum.
There is the high level of evidence that the perioperative avoidance of hypothermia
and supplemental oxygen during recovery can significantly reduce the rate of SSIs.
Postoperative care of wounds: * Similar attention to standards is needed in the
postoperative care of wounds. Secondary (exogenous) SSIs, as well as other HAIs, can be
related to poor hospital standards.
2 - Specific wound infections
Gas gangrene
This is caused by C. perfringens. These Gram-positive, anaerobic, spore-bearing bacilli are widely
found in nature, particularly in soil and feces. This is relevant to military and traumatic surgery and
colorectal operations. Patients who are immunocompromized, diabetic or have malignant disease
are at greater risk, particularly if they have wounds containing necrotic or foreign material, resulting
in anaerobic conditions. Military wounds provide an ideal environment as the kinetic energy of high-
velocity missiles or shrapnel causes extensive tissue damage. The cavitation which follows passage
of a missile through the tissues causes a ‘sucking’ entry wound, leaving clothing and environmental
soiling in the wound in addition to devascularized tissue. Gas gangrene wound infections are
associated with severe local wound pain and crepitus (gas in the tissues, which may also be noted
on plain radiographs).
Page 7 of 11

The wound produces a thin, brown, sweet-smelling exudate, in which Gram staining will reveal
bacteria. Edema and spreading gangrene follow the release of collagenase, hyaluronidase, other
proteases and alpha toxin. Early systemic complications with circulatory collapse and MSOF follow if
prompt action is not taken. Antibiotic prophylaxis should always be considered in patients at risk,
especially when amputations are performed for peripheral vascular disease with open necrotic
ulceration. Once gas gangrene infection is established, large doses of intravenous penicillin and
aggressive debridement of affected tissues are required.
Tetanus
Clostridium tetani is an anaerobic, terminal spore-bearing, Gram-positive bacterium that can cause
tetanus following implantation into tissues or a wound (which may have been trivial or unrecognized
and forgotten). The spores are widespread in soil and manure, and so the infection is more common
in traumatic civilian or military wounds. The signs and symptoms of tetanus are mediated by the
release of the exotoxin tetanospasmin, which affects myoneural junctions and the motor neurones
of the anterior horn of the spinal cord. A short prodromal period, which has a poor prognosis, leads
to spasms in the distribution of the short motor nerves of the face followed by the development of
severe generalized motor spasms including opsithotonus, respiratory arrest and death. A longer
prodromal period of 4–5 weeks is associated with a milder form of the disease. The entry wound
may show a localized small area of cellulitis; exudate or aspiration may give a sample that can be
stained to show the presence of Gram-positive rods. Prophylaxis with tetanus toxoid is the best
preventative treatment but, in an established infection, minor debridement of the wound may need
to be performed and antibiotic treatment with benzylpenicillin provided in addition. Relaxants may
also be required, and the patient may require ventilation in severe forms, which may be associated
with a high mortality.
The toxoid is a formalin-attenuated vaccine and should be given in three separate doses to give
protection for a five-year period, after which a single five-yearly booster confers immunity. It should
be given to all patients with open traumatic wounds who are not immunized. At-risk wounds are
those that present late, when there is devitalisation of tissue or when there is soiling. For these
wounds, a booster of toxoid should be given or, if not immunized at all, a three-dose course,
together with prophylactic benzylpenicillin. The use of antitoxin using human immunoglobulin
ought to be considered for both at-risk wounds and established infection.
Synergistic spreading gangrene (synonym: subdermal gangrene, necrotizing fasciitis)
This condition is not caused by clostridia. A mixed pattern of organisms is responsible: coliforms,
staphylococci, Bacteroides spp., anaerobic streptococci and peptostreptococci have all been
implicated, acting in synergy. Abdominal wall infections are known as Meleney’s synergistic hospital
gangrene and scrotal infection as Fournier’s gangrene. Patients are almost always
immunocompromised with conditions such as diabetes mellitus. The wound initiating the infection
may have been minor, but severely contaminated wounds are more likely to be the cause. Severe
wound pain, signs of spreading inflammation with crepitus and smell are all signs of the infection
spreading. Untreated, it will lead to widespread gangrene and MSOF. The subdermal spread of
gangrene is always much more extensive than appears from initial examination. Broad-spectrum
antibiotic therapy must be combined with aggressive circulatory support. Locally, there should be
wide excision of necrotic tissue and laying open of affected areas. The debridement may need to be
extensive, and patients who survive may need large areas of skin grafting.
Page 8 of 11

3 - Postoperative Nosocomial Infections
Surgical patients are prone to develop a wide variety of nosocomial infections during the
postoperative period, which include SSIs, UTIs, pneumonia, and bacteremic episodes, the latter
types of nosocomial infections are related to prolonged use of indwelling tubes and catheters for
the purpose of urinary drainage, ventilation, and venous and arterial access, respectively.
4 - Blood borne viruses and surgery *
Hepatitis B Virus:
Double-shelled DNA virus
May cause acute liver failure or chronic active hepatitis.
Infection is largely blood-borne and is transmitted by blood transfusion and transmission
from a contaminated sharps injury is 30%.
Antigens appear in the serum: HBsAg, the surface antigen; HBcAg, the hepatitis core antigen;
HBeAg, the (e) antigen; the Dane particle; double-stranded DNA; and DNA polymerase
activity.
Antibodies formed against these antigens (anti-HBs, anti-HBe) can be detected in the
peripheral blood:
HBsAg +ve. Failure to clear infection, residual infectivity.
HBsAb +ve. Protection marker from immunization or infection.
HBeAg +ve. Close correlation of infectivity.
Hospital staffs are routinely offered vaccination for hepatitis B.
Hepatitis C Virus: RNA virus which causes cirrhosis of the liver and primary liver cancer. There is no
vaccination. Transmission from a contaminated sharps injury is 2–3%. Surgeons must be tested for
hepatitis C and may not carry out exposure-prone procedures if hepatitis C +ve.
Human immunodeficiency virus (HIV)
Double-stranded RNA retrovirus transmitted by passage of infected body fluids from one
person to another by several methods, including: sharps and infected blood products.
HIV infection results in widespread immunological dysfunction, manifested by a fall in
CD4+ve lymphocytes, monocytes, and antigen presenting cells (APCs).
There is usually a 3-month asymptomatic, but infective viremia. During this period, ELISA
tests for HIV antibodies are negative. At seroconversion, an acute illness can occur.
The HIV risk from an HIV contaminated hollow needle is 0.3%.
The risk from splashes on broken skin or mucous membranes is 0.1%.
Page 9 of 11

Principles of antimicrobial treatment
Antimicrobials may be used to prevent (Prophylaxis) or treat established surgical infection.
Principles for the use of antibiotic therapy:
Antibiotics do not replace surgical drainage of infection
Only spreading infection or signs of systemic infection justifies the use of antibiotics
Whenever possible, the organism and sensitivity should be determined
There are two approaches to antibiotic treatment:
1) A narrow-spectrum antibiotic may be used to treat a known sensitive infection; for example, MRSA
(which may be isolated from pus) is usually sensitive to vancomycin or teicoplanin, but not
flucloxacillin.
2) Combinations of broad-spectrum antibiotics can be used when the organism is not known or when it
is suspected that several bacteria, acting in synergy, may be responsible for the infection. For
example, during and following emergency surgery requiring the opening of perforated or ischemic
bowel, any of the gut organisms may be responsible for subsequent peritoneal or bacteremic
infection. In this case, a triple-therapy combination of broad-spectrum penicillin (such as ampicillin
or mezlocillin) with an aminoglycoside (such as gentamicin) and metronidazole may be used per and
postoperatively to support the patient’s own body defenses. An alternative to the penicillins is a
cephalosporin, e.g. cefuroxime. In surgical units in which resistant Pseudomonas or other Gram-
negative species (such as Klebsiella) have become ‘resident opportunists’, it may be necessary to
rotate anti-pseudomonal and anti-Gram-negative antibiotic therapy.
In treating patients who have surgical infection with systemic signs (SIRS), a failure to respond to antibiotics
may indicate that there has been a failure of infection source control. If response is poor after 3–4 days,
there should be a re-evaluation with a review of charts and further investigations requested to exclude the
development or persistence of infection such as a collection of pus.
Antibiotics used in treatment and prophylaxis of surgical infection
Antimicrobials may be produced by living organisms (antibiotics) or by synthetic methods. Some are
bactericidal, e.g. penicillins and aminoglycosides, and others are bacteriostatic, e.g. tetracycline and
erythromycin. In general, penicillins act upon the bacterial cell wall and are most effective against bacteria
that are multiplying and synthesizing new cell wall materials. The aminoglycosides act at the ribosomal
level, preventing or distorting the production of proteins required to maintain the integrity of the enzymes
in the bacterial cell.
Penicillin
Benzylpenicillin has proved most effective against Gram-positive pathogens, including most streptococci,
the clostridia and some of the staphylococci that do not produce β-lactamase and may be used specifically
to treat spreading streptococcal infections. Penicillin is valuable even if other antibiotics are required as
part of multiple therapy for a mixed infection. All serious infections, e.g. gas gangrene, require high dose
intravenous benzylpenicillin.
Flucloxacillin
This is a β-lactamase-resistant penicillin and is therefore of use in treating most community-acquired
staphylococcal infections, but it has poor activity against other pathogens.
Page 10 of 11

Ampicillin and amoxicillin
These β-lactam penicillins can be taken orally or may be given parenterally. Both are effective against
Enterobacteriaceae, Enterococcus faecalis and the majority of group D streptococci, but not species of
Klebsiella or pseudomonads. Their use is now rare as there are more effective alternatives. Clavulanic acid
is available combined with amoxicillin (Augmentin) and can be taken orally. This anti-β-lactamase protects
amoxicillin from inactivation by β-lactamase producing bacteria. It is of value in treating infections caused
by Klebsiella strains and β-lactamase-producing E. coli but is not active against Pseudomonas spp. It can be
used for localized cellulitis or superficial staphylococcal infections and infected human and animal bites. It is
available for oral or intravenous therapy.
Cephalosporins
There are several β-lactamase-susceptible cephalosporins that are of value in surgical practice: cefuroxime,
cefotaxime and ceftazidime are widely used. The first two are most effective in intra-abdominal, skin and
soft-tissue infections, being active against Staphylococcus aureus and most Enterobacteriaceae. As a group,
the enterococci (Streptococcus faecalis) are not sensitive to the cephalosporins. Ceftazidime, although
active against the Gram-negative organisms and S. aureus, is also effective against P. aeruginosa. These
cephalosporins may be combined with an aminoglycoside, such as gentamicin, and an imidazole, such as
metronidazole, if anaerobic cover is needed.
Aminoglycosides
Gentamicin and tobramycin have similar activity and are effective against Gram-negative
Enterobacteriaceae. Gentamicin is effective against many strains of Pseudomonas, although resistance has
been recognized. All aminoglycosides are inactive against anaerobes and streptococci. Ototoxicity and
nephrotoxicity may follow sustained high toxic levels. These antibiotics have a marked post-antibiotic
effect, and single, large doses are effective and may be safer.
Vancomycin
This glycopeptide is most active against Gram-positive bacteria and has proved to be effective against
MRSA, although vancomycin resistance is increasingly being reported. However, it is ototoxic and
nephrotoxic, so serum levels should be monitored. It is effective against C. difficile in cases of
pseudomembranous colitis.
Imidazoles
Metronidazole is the most widely used member of the imidazole group and is active against all anaerobic
bacteria. It is particularly safe and may be administered orally, rectally or intravenously. Infections caused
by anaerobic cocci and strains of Bacteroides and clostridia can be treated, or prevented, by its use.
Metronidazole is useful for the prophylaxis and treatment of anaerobic infections after abdominal,
colorectal and pelvic surgery.
Carbapenems
Meropenem, ertapenem and imipenem are members of the carbapenems. They are stable to β-lactamase,
have useful broadspectrum anaerobic as well as Gram-positive activity and are effective for the treatment
of resistant organisms or serious mixed-spectrum abdominal infections (peritonitis).
Quinolones
Quinolones, such as ciprofloxacin, were active against a wide spectrum of organisms. Their widespread use
has been related to the development of resistant organisms, and their role in treating surgical infection is
limited.
Page 11 of 11
