
1
Gynecology L5
Menopause
The menopause and the post menopause is the condition of the 20
th
and 21th
centuries due to the increase in the life expectancy reaching now 82 years in
UK , so the majority of women can therefore expect to live over a third of their
lives in menopausal state .
Menopause definitions :
Menos = month , pauses – cessation , both are Greek words means last
menstrual period .
Menopause : Last menstrual period , the diagnosis can only be made
retrospectively after a minimum of 1 year , the average age is ( 51 years ) but the
physiological changes which result in the final menstrual period ( FMP ) can
start 10 years prior to this .
Hormonal changes continue long after FMP , this episode of dynamic neuro-
endocrine change is characterized by climacteric period ( Climb to the
menopause ).It is often used synonymously with "perimenopause" or "the
change" .It marks the transition from the reproductive to the non-reproductive
State, the menopause being a specific event within that phase .
2
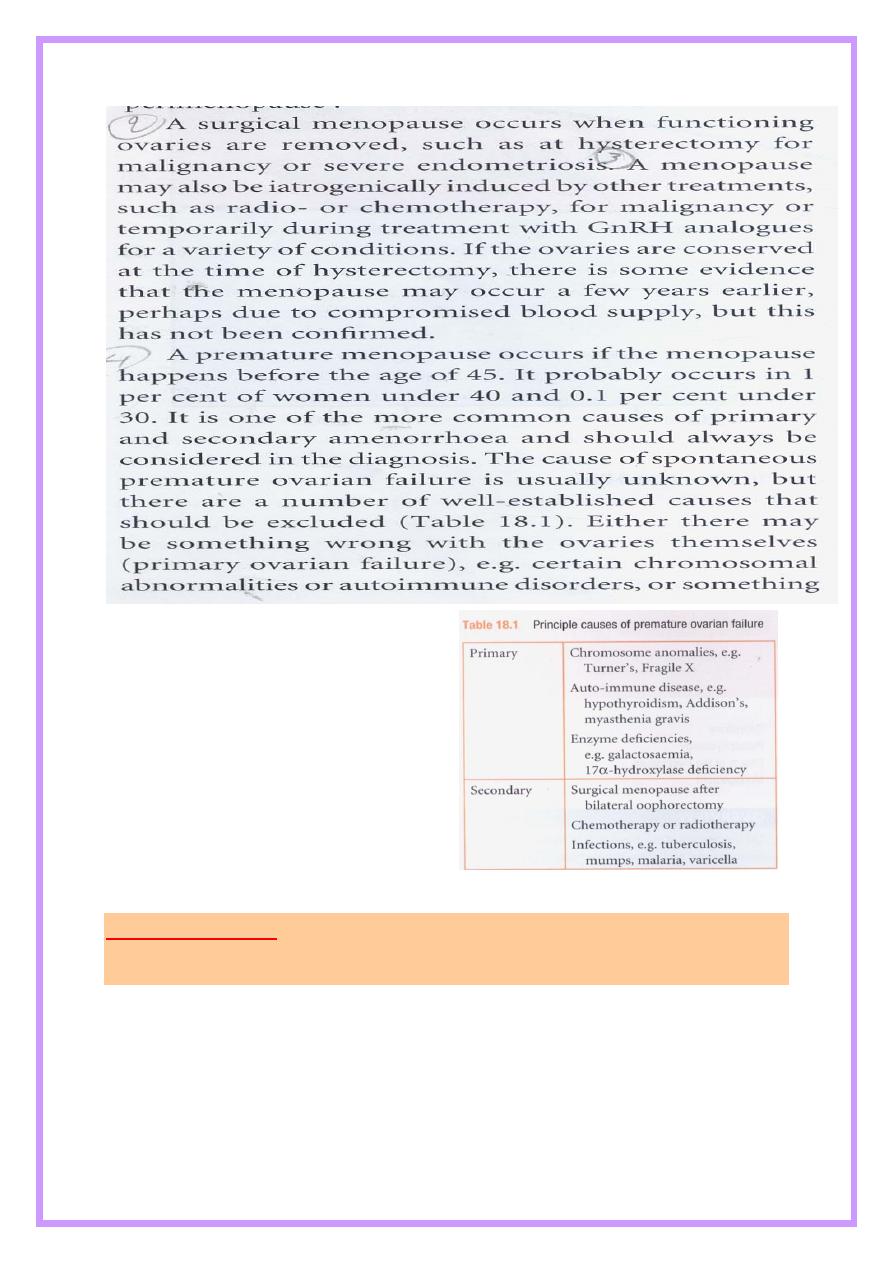
happens to the ovary e.g. oophorectomy .
Pathopysiology :
The Declining Oocyte pool :
Female fetus has 1.5 million oocytes, but these oocytes shrinks throughout
life reaching 400000 at puberty and it is estimatedthat for every follicle which
matures to ovulation ,up to 1000 follicles fail & become atretic leaving only
few thousand oocyte as the female enter forties and few or none in the post
menopause . There are 2 landmarks in the ovarian failure process first ; there is
3
marked decline in fertility with no cycle dysfunction .And second cyclic changes
become noticeable as the follicular phase shortens and luteal phase dysfunction
occurs .
Hormonal changes :
Initially the ovarian failure is compensated by gonadotrophin levels starting to
rise in some women from age of 30 years .
During this time there is decrease in number of gonadotrophin receptors in
perimenopause ovaries and inhibin production from granulosa cells falls leading
to reduce inhibin : FSH ratio .
Decompensated failure occurs due to the critical decline in oocyte pool leading
to further rises in FSH ( 10 to 20 folds ) and LH raises only 3 times the normal
due to shorter half life , thus FSH is more important in assessing menopause .
Estrogen ( estradiol E2 ) Levels drop due to a reduction in follicle number.
Further decline in oestradiol levels over subsequent years has effects on all
oestrogen –responsive tissues( which are widespread throughout the body) .
Progesterone Permanent cessation . some testosterone continue to be
produced by ovarian theca cells .
Main menopausal estrogen is Osterone ( E1 ) which is produced mainly in
peripheral adipose tissue and the post menopausal ovary by aromatization of
adrenal androstensione .
The menstrual cycle :
Anovulatory cycles become progressively common , so there can be
continued estrogen production in the absence of progesterone leading to
endometrial proliferation , hyperplasia and at its extreme carcinoma , as a result
menstrual cycle can be heavy prolonged and unpredictable with intermenstrual
bleeding .
Effects of menopause :
1. Short term(0-5 years).
2. Intermediate(3-10 years) .
3. Long tearm (more than 10 years) .

4
Short term consequences
:
Hot flashes and night sweats : commonest menopausal symptoms , hot
flushes are thought to be arising due to loss of estrogenic induced opoid
activity in the hypothalamus leading to thermo-dysregulation , it is though
that noradrenalin and serotonin mediate this activity ,leading to cutaneous
vasodilation &heat loss .Classically ,it only affects the upper trunk &neck.
Certain triggers can be identified, such as stress, spicy foods, caffeine&
hot
drinks.
Obese are protected from these symptoms due to their production of large
amounts of oestrone and their low sex horm
one binding globulin levels which leaves more of the free active form .
Insomnia , anxiety , irritability ,labile mood, tearfulness, memory loss ,
poor concentration , depression ; these symptoms mainly due to fall in
serotonin .
Decrease in sexuality and libido .
Hair changes ,dry &itchy skin.
Joint aches.
Intermediate consequences :
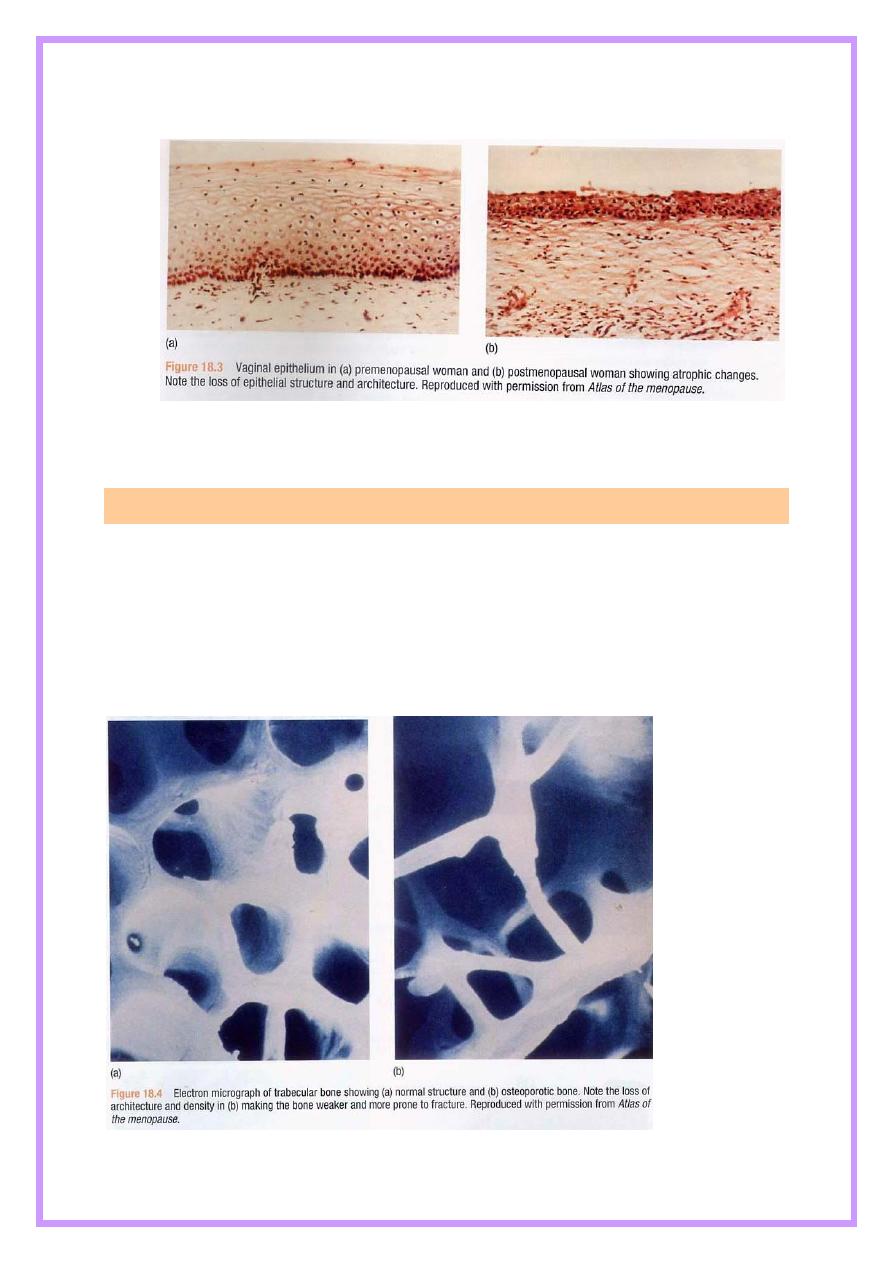
Generalized atrophy due to rapid loss of collagen &loss of normal
architecture within the vaginal epithelium, reducing its secretions
&elasticity due to oestrogen deficiency , in the genital tract this is
manifested by vaginal dryness, soreness ,dysparunia , urogenital prolapse
and vaginal bleeding from fragile atrophic skin .
Atrophy of lower genital tract leads to dysuria , urgency and frequency
( urethral syndrome ) &recurrent urinary tract infection.
5
Los of collagen also leads to generalized aches and pains .
Long term consequences
":
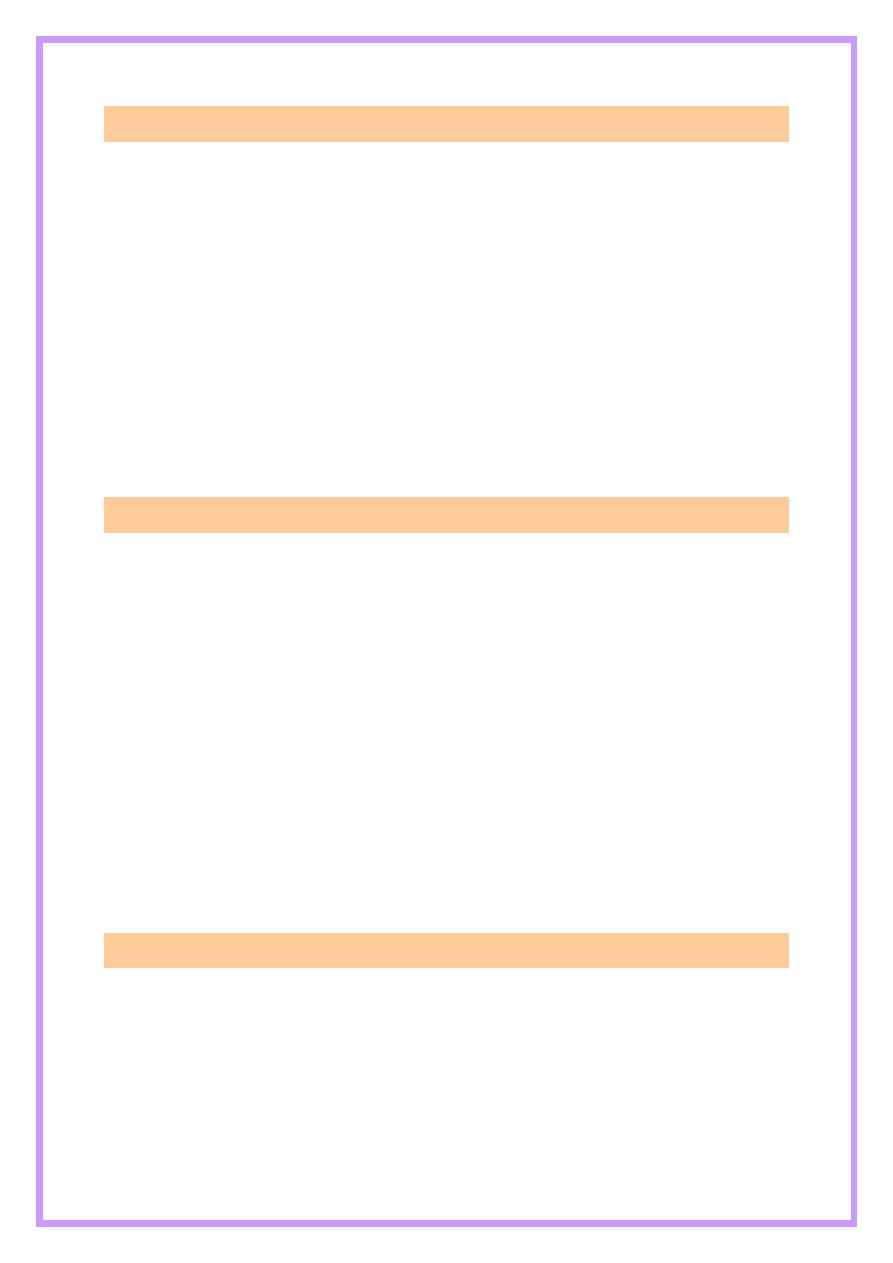
Osteoporosis : Significant decrease in bone matrix ( due to increase bone
resorption ) leading to increase risk of fractures .
Cardiovascular : decrease estrogen leads to increase cholesterol and
triglycerides , LDL and decrease HDL ; thus increase risk of coronary
heart disease.
CNS : dementia and Alzheimer .
6
Patient assessment :
The diagnosis of menopause can usually ascertained from the classical
history of vasomotor symptoms , hot flushes and sweating plus prolonged
period of amenorrhea .
Increase level of FSH more than 15 IU/L ( regarded as climacteric ) , it
more than 30 IU/L considered diagnostic of menopause .
Assessment of weight , blood pressure , cervical cytology , lipid profile .
Breast and pelvic examination , mammography if clinically indicated .
Endometrial biopsy if had post menopausal bleeding or irregular
perimenopausal bleeding .
Bone assessment by DEXA ( dual energy X-ray absorptiometry ) of
lumbar spine and hip .
Therapeutic options :
1. Hormone replacement therapy ( HRT )
Estrogen ; has many forms :
Oral ( conjugated equine estrogen 0.3 – 0.625 ) .
Transdermal estradiol .
Implanted estradiol .
Estradiol silicon ring .
Estriol cream locally .
Lowest effective dose should be used to decrease risk of breast cancer , heart
disease , or deep venous thrombosis , but risk of endometrial hyperplasia in
nonhysterectomized and progesterone should be added to estrogen in continuous
or sequential manner .
Contraindications to HRT :
1. coronary heart disease .
2. Stroke .
3. Venous thrombosis .
4. Endometriosis ( may cause flaring ) .
5. Patient with uterine fibroid ( ??? ) .
6. Patient with past history of endometrial CA .
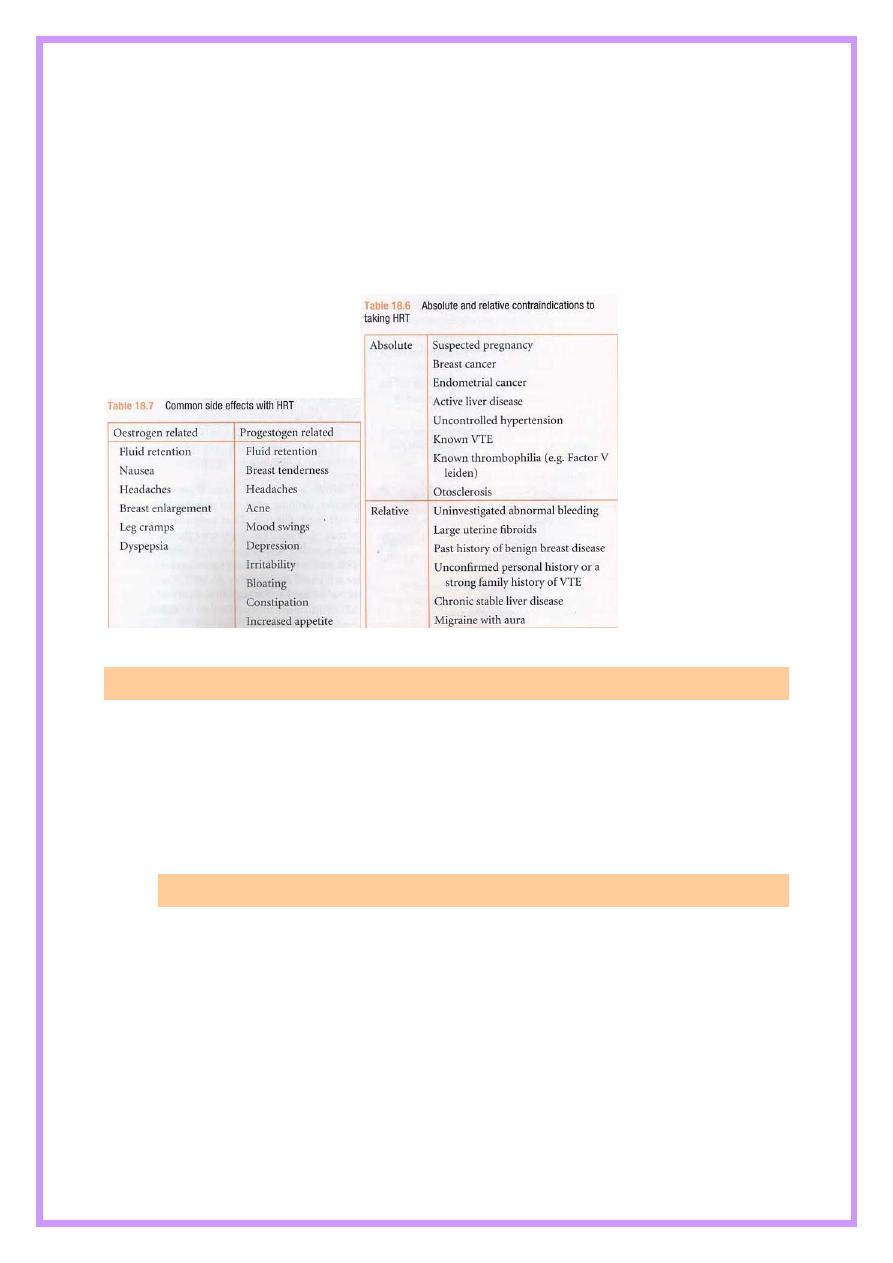
7
7. Breast CA .
8. Undiagnosed vaginal bleeding .
9. Severe liver disease .
10. Severe uncontrolled hypertension .
Risks of HRT :
1) Breast cancer :
2) Endometrial cancer
3) DVT
4) CAD
5) Overian cancer
6) Strock
Practical considerations for prescribing HRT :
HRT is only one option for dealing with menopausal symptoms and other
options can be considered .
Treatment should be started at the lowest appropriate dose and can be
increased if there is no symptomatic improvement after a few months .
Side effects from the reintroduction of oestrogen and progesterone may be
common particularly if it has been several years since the menopause .
The duration of HRT use depends on the individual circumstances and
indication for taking it . The 'average' menopausal woman in her early 50s
8
will probably only take it for two or three years , but there is no reason
why she should not take it for longer if indicated ... They exception to
these recommendations is women who have undergone a premature
menopause . In this group , the risk/benefit balance is strongly in favour
of them taking HRT at least up until the age of 50 as a true physiological
replacement .
Once stabilized on treatment , women should be reviewed every six
months or so . Their individual risk of VTE , stroke and breast cancer
should be appraised regularly and balanced against the benefits they are
gaining from the treatment .
2. Alternatives to HRT :
Indications :
1. Female doesn’t wish to use HRT because they are concerned about side
effects and risks .
2. Personal or family history of CVD , DVT or breast CA .
Duration of HRT :
Require careful judgments of benefits and risks and based on individual
basis .
3. Alternatives :
1. Life style measure : decrease alcohol , caffeine plus regular exercise .
2. Vaginal moisturizer .
3. Alpha 2 agonist ( clondine ) used to treat vasomotor symptoms .
4. Selective serotonin re-uptake inhibitors ( SSRIs ) . Selective nor-adrenaline
re-uptake inhibitors (SNRIs) , fluoxetine ( SSRIs ) + ventafazine ( SNRIs ) :
used to treat vasomotor symptoms , with treatment 60% decrease in hot
flushes , main side effect is nausea .
5. Complementary therapy : phyto-estrogen , vitamins and minerals ( vit E,C,
semenium , Ca
+2
mg/day + vit. D ) . for skeletal protections .
6. Bisphosphonates + SERM ( selective estrogen receptor modulator ;
raloxifene ) .
9
New developments :
There is ongoing research into development of the ideal postmenopausal
treatment that will control symptoms , prevent bone loss , reduce cardiovascular
disease risk , but at the same time not increases risks of breast cancer ,
endometrial cancer and VTE .
To this end , a new generation of selective tissue receptor modulators are
being developed which will have selective action against oestrogen ,
progesterone and testosterone receptors . Currently ,
raloxifene
is the
only SERM commercially available . Reloxifene is a benzothiphene. It
acts by locking into the oestrogen receptors , but as it does so its side
chain deactivates one of the activation functions of the receptor . This
specific action only occurs in certain tissues , such as the breast and
endometrium . In other tissues , such as tissues , such as skeleton , the
side arm does not deactivate the receptor and raloxifene behaves like an
oestrogen. At present , these products do not relieve menopausal
symptoms so are primarily restricted for women at risk of osteoporosis .
Further work is ongoing with similar preparations , in combination with
small amounts of oestrogen , which from initial studies appear
promising .
There is also renewed interest in the cause of hot flushes and the
development of some newer drugs that may act on the serotonin pathway
and reduce vasomotor symptoms .
Objective
The student should be know :
The menopausal consultation.
Management options.
11
Risks & benefits of each option.
Practical considerations for prescribing HRT.
*New developments
