Acute Kidney Injury
Acute kidney injury (AKI) (formerly called acute renal failure) is a clinical syndrome in which there is sudden deterioration in renal function results in inability of the kidney to maintain fluid and electrolyte homeostasis.Classification:
AKI is classified by pediatric-modified RIFLE criteria according to reduction in the creatinine clearance and urine output in to:Risk of AKI
Injury
Failure
Loss
End stage renal disease
• CRITERIA
• CREATININ CLEARANC• URINE OUTPUT
• Risk
• by 25%
• <0.5 mL/kg/hr for 8 hr
• Injury
• by 50%
• <0.5 mL/kg/hr for 16 hr
• Failure
• by 75%
• <0.3 mL/kg/hr for 24 hr or anuria for 12 hr
• Loss
• Persistent
• failure >4 wk
•
• End-stage
• ESRD
• (persistent failure >3 mo)
•
•
• Other classification of AKI according to rise in serum creatinine:
• stage 1: S. creatinine >150% of normal
• stage II: S. creatinine >200% of normal• stage III: S. creatinine >300% of normal
Etiology and Pathogenesis:
• Characterized by decreased effective circulating arterial volume, causing inadequate renal perfusion and a decreased GFR.• Absent evidence of kidney damage.
Prerenal AKI (prerenal azotemia)
Causes:
• Dehydration• Sepsis
• Hemorrhage
• Severe hypoalbuminemia
• Cardiac failure.
• If the underlying cause of renal hypoperfusion is reversed, renal function returns to normal.
• If hypoperfusion is persist, intrinsic renal parenchymal damage will develop
• characterized by renal parenchymal damage, most commonly due to ischemic/ hypoxic injury and nephrotoxic insults.
Causes:
• GN: postinfectious GN, SLE nephritis, HSP nephritis, membranoproliferative GN
• Acute tubular necrosis and Cortical necrosis
• Renal vein thrombosis
Intrinsic (Renal) AKI
• Acute interstitial nephritis (hypersensitivity to drugs or infectious agents)
• Tumor infiltration• Tumor lysis syndrome.
• characterized by obstruction of the urinary tract.
• Obstruction must be bilateral to result in AKI.• Relief of the obstruction usually results in recovery of renal function, except in renal dysplasia or prolonged UT obstruction.
Postrenal AKI:
Causes:
• posterior urethral valves• bilateral UPJ obstruction
• urolithiasis (stones)
• tumor (intra-abdominal or renal)
• hemorrhagic cystitis
• neurogenic bladder
CLINICAL MANIFESTATIONS:
History:
• Infant with a history of vomiting and diarrhea most likely has prerenal AKI caused by dehydration, or hemolytic-uremic syndrome.
• A neonate with a history of hydronephrosis on prenatal ultrasound and a palpable bladder most likely has congenital urinary tract obstruction, mostly due to posterior urethral valves.
• child with a history of recent pharyngitis who presents with periorbital edema, hypertension, and gross hematuria most likely has intrinsic AKI due to acute postinfectious glomerulonephritis.
Physical examination:
• Tachycardia, dry mucous membranes, and poor peripheral perfusion suggest hypovolemia and the possibility of prerenal AKI.• HT, edema, rales, and a cardiac gallop suggest volume overload and possibility of intrinsic AKI from GN or ATN
• Rash and arthritis indicate SLE or HSP
• Palpable flank masses may be seen with renal vein thrombosis, tumors or cystic disease
1. Urinalysis:
• In prerenal azotemia, the GUE is unremarkable with a high specific gravity which indicate good renal retention of water in case of renal hypoperfusion.• The presence of hematuria, proteinuria, and RBC or granular urinary casts suggests intrinsic AKI, especially glomerular disease and ATN.
Investigations:
• The presence of WBCs and WBC casts with low-grade hematuria and proteinuria suggests tubulointerstitial disease.
• Urinary eosinophils may be present in drug-induced interstitial nephritis.
CBC: shows:
• Anemia: dilutional or hemolytic, as in SLE, renal vein thrombosis, HUS
• Leukopenia: in SLE, sepsis.
• Thrombocytopenia: in SLE, renal vein thrombosis, sepsis, HUS
3. Other blood tests:
• hyponatremia (dilutional)• metabolic acidosis
• increased BUN, creatinine, uric acid, potassium, phosphate ( due to diminished renal function) hypocalcemia (due to hyperphosphatemia).
• The serum C3 level may decreased as in postinfectious GN, SLE, or membranoproliferative GN.
6. Renal biopsy indicated in patients who do not have clearly defined prerenal or postrenal AKI.
4. Chest XR may shows cardiomegaly, pulmonary congestion or pleural effusions.
5. Renal ultrasonography can reveal hydronephrosis and/or hydroureter, which suggest urinary tract obstruction, or hydronephrosis due to intrinsic renal disease.
• Lab & C\F
• Prerenal• Renal
• Postrenal
• Urine output
• Low
• Low, normal, or high
• Low or N
• Urinalysis
• Normal
• RBCs, WBCs, protein, casts
• Variable
• Urine Na+ (mEq/L)
• Child <15
• Neonate <20–30
• Child >40
• Neonate >50
• Variable, may be >40
• FENa (fractional Na excretion
• Child <1
• Neonate <2.5
• Child >2
• Neonate >2.5
• Variable, may be >2
• Lab & C\F
• Prerenal
• Renal
• Postrenal
• Urine osmolality
• (mOsm/L)
• Child >500
• Neonate >350
• Child ∼300
• Neonate ∼300
• Variable, may be
• <300
• Renal U\S
• Normal
• Increased echogenicity, decreased
• corticomedullary differentiation
• Hydro-nephrosis
•
Treatment of AKI:
2. Fluid and diuretics therapy:• Normal saline( bolus) 20ml\kg\30 min in hypovolemic patients after exclusion of heart failure and fluid overload. It might repeated 2-3 times.
Patients usually pass urine within 2 hours after rehydration. Failure of passing urine suggest intrinsic or postrenal AKI.
1. Bladder catheterization for patient with U.T. obstruction to ensure urinary drainage and for accurate monitoring of UOP.
B. Diuretic therapy (in hypervolemic patients):
• Furosemide 2mg\kg with manitol 0.5g\kg as a single dose.
• If the UOP not improved, continuous diuretic infusion may be indicated.
• Dopamine 2-3Mg\kg\min PLUS furosemide to increase renal cortical perfusion.
• There is little evidence that diuretics or dopamine can prevent AKI or facillate the recovery but manitol may be effective in prevention of pigment-induced AKI (myoglobin, hemoglobin)
• If there is no response to diuretic therapy, it should be stopped and fluid daily intake should be limited to 400ml\m2\24 hr (insensible loss) Plus the urine output and extrarenal loss (blood and GIT).
• Close monitoring of fluid intake, UOP, stool OP, B. weight, S. electrolytes.
3. Management of hyperkalemia:
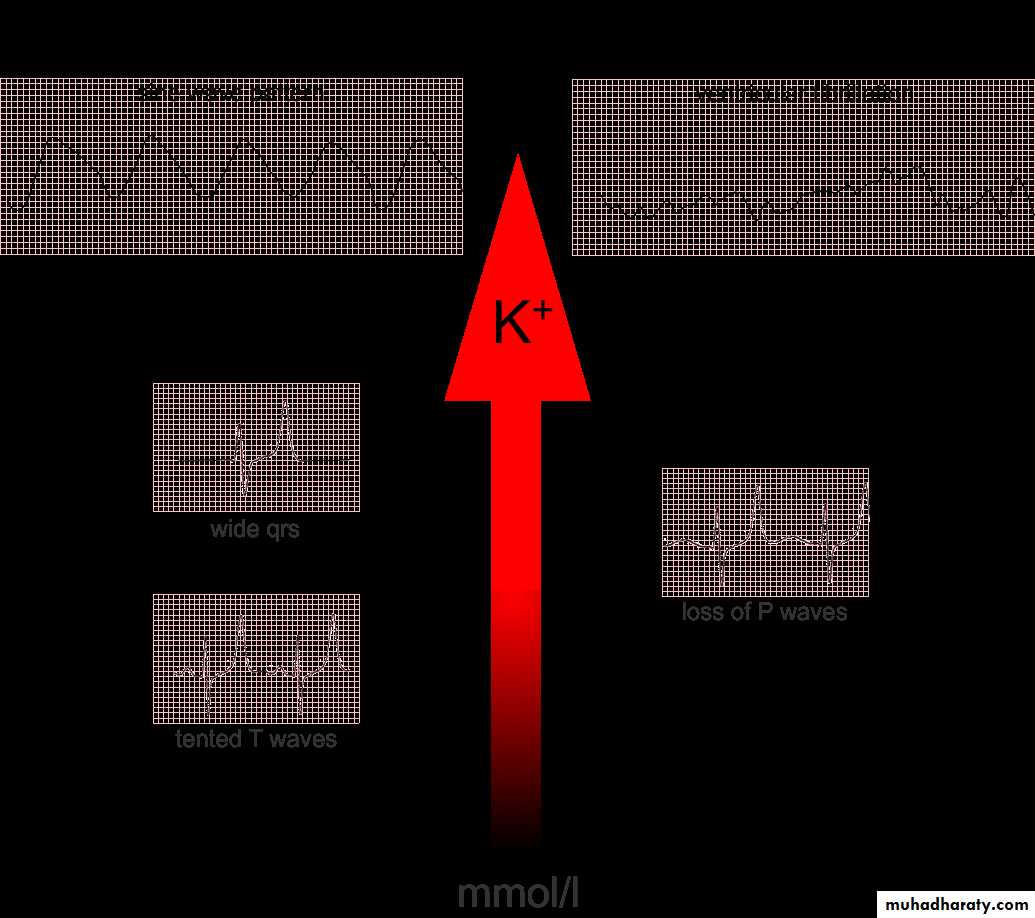
• Rapid development of hyperkalemia (S. K >6 mEq/L) can lead to cardiac arrhythmia, cardiac arrest, and death.• The earliest ECG change is peaked T waves, followed by widening of the QRS, ST segment depression, ventricular arrhythmias, and cardiac arrest.
Treatment:
• Eliminate exogenous K sources (dietary, IV fluids, total parenteral nutrition).• Sodium polystyrene sulfonate resin (Kayexalate), 1 g/kg, orally or by enema.
• It exchanges Na for K in the GIT enhancing its excretion but it take several hr to take its effect.
• A single dose of 1 g/kg can be lower S. K level by about 1 mEq/L. It may be repeated every 2 hr. according to the severity
• Severe cases (S. K >7 mEq/L), especially if associated with ECG changes, require emergency treatment in addition to Kayexalate. This include:
• Calcium gluconate 10% solution, 1 mL/kg IV, over 3-5 min. It counteracts the increase in myocardial irritability induced by hyperkalemia but does not lower the S. K
• NaHco3 1-2 mEq/kg IV, over 5-10 min
• Regular insulin, 0.1 units/kg, with glucose 50% solution, 1 mL/kg, over 1 hr
• β-adrenergic agonists (Salbutamol) in adults, but there are no controlled data in pediatric patients.
• Sodium bicarbonate, insulin, and glucose and β-adrenergic agonists lowers the S. K. level by shifting K from the extracellular to the intracellular compartment
• Dialysis indicated in persistent hyperkalemia despite the previous treatments.
4. Treatment of severe metabolic abnormalities including metabolic acidosis, hypocalcemia, and hyponatremia.
5. Treatment of anemia: It is usually mild dilutional anemia (Hb 9-10g\dl) but severe anemia (Hb < 7g\dl) might occur with SLE, HUS, active bleeding or prolong AKI required packed RBCs transfusion 10 ml\kg over 4-6 hr to avoid hypervolemia.
7. Nutritional therapy:
• Restriction of Na, K, and Ph intake.• Protein intake moderately restricted to avoid accumulation of nitrogenous waste products.
• Parenteral hyperalimenation with essential AA in critically ill patients.
6. Treatment of hypertension: by salt and water restriction, diuretics, Ca. channel blocker or B-blockers.
8. Dialysis: indicated in:
• Anuria/oliguria• Volume overload with HT and/or pulm. edema refractory to diuretic therapy
• Persistent hyperkalemia
• Severe metabolic acidosis unresponsive to medical management
• Uremia (encephalopathy, pericarditis, neuropathy)
• BUN >100-150 mg/dL (or rapidly rising)
• Ca: Ph imbalance, with hypocalcemic tetany refractory to other treatments.
Thank you for your attention