Infectious Diseaseslec. 2By: dr. Zahraa Marwan
Chronic Bacterial infectionTuberculosis: it is the single most important infectious cause of death on earth after HIV.
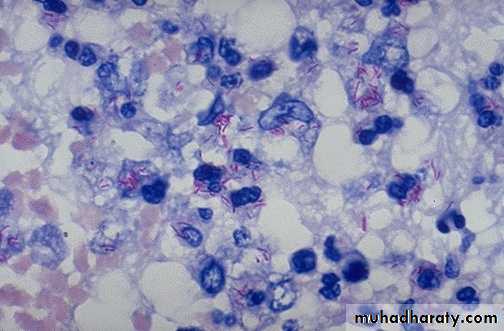
*Caused by Mycobacterium tuberculosis & Mycobacterium bovis. (gram +ve aerobic bacilli), the bacilli have waxy coat that cause them to retain red dye when treated with acid, that is why they are called Acid fast bacilli.
This is an acid fast stain of Mycobacterium tuberculosis Which appear as red rods.
Transmission
possible entry sites exist: -• Respiratory tract by inhalation (Mycobacterium tuberculosis)
• Alimentary tract, through a milk of diseased cows. (Mycobacterium bovis).
Mycobacterium avium & mycobacterium intracellulare cause infection in AIDS patients.
Tissue Reaction to T.B. bacilli
TB bacilli produce no Exotoxin, Endotoxin or enzymes.The Lesion of T.B is mainly due to the delayed hypersensitivity reaction (type IV) to an antigenic protein component of the organism.
T.B. at first cause minimal non specific inflammatory response in the tissue at the site of infection then T-lymphocytes appear at the site of infection within two weeks and secret lymphokines which responsible for arrival of macrophages by chemo taxis and ,CD4 (helper) T-lymphocytes produce IFN-γ which activate & differentiate macrophages into the “epithelioid histiocytes” that aggregate to form granulomas; Gaseous necrosis caused by CD8 (suppressor) T-lymphocyte.
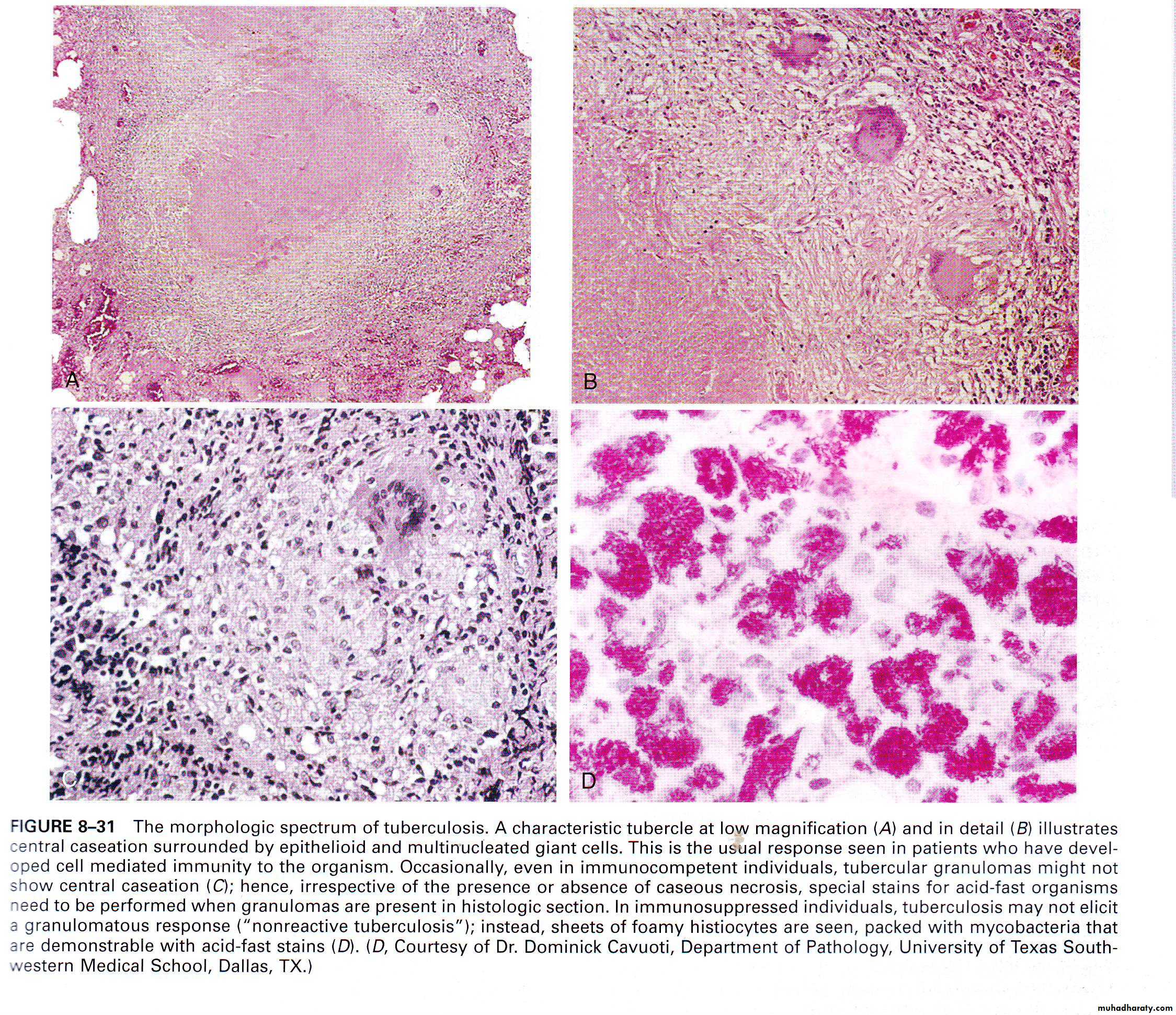
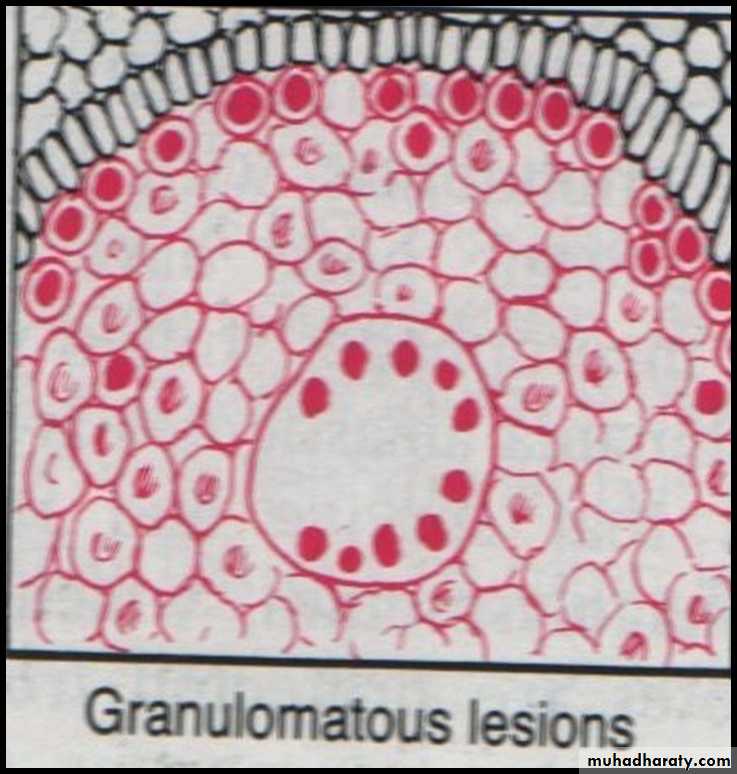
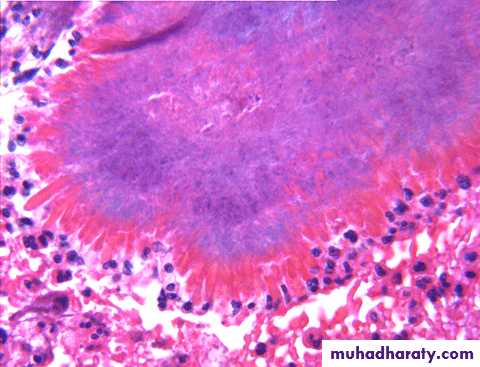
So the final lesion of TB (microscopically) consist of :
central area of caseous necrosissurrounded by activated macrophages (epithelioid macrophages), some macrophages fuse to from multinucleated giant cells ( Langhans giant cells)
surrounded by rim of chronic inflammatory cells rich in lymphocytes .
at the periphery there is fibrosis.
This lesion is called tubercle which is the characteristic lesion of TB.
* Healing when present is by progressive fibrosis.
* Organisms may remain viable in apparently healed lesions, only to be reactivated years later if host resistance decreases.
Characteristic tubercle at low magnification (A) and high magnification (B) shows central granular caseation surrounded by epithelioid and multinucleate giant cells.
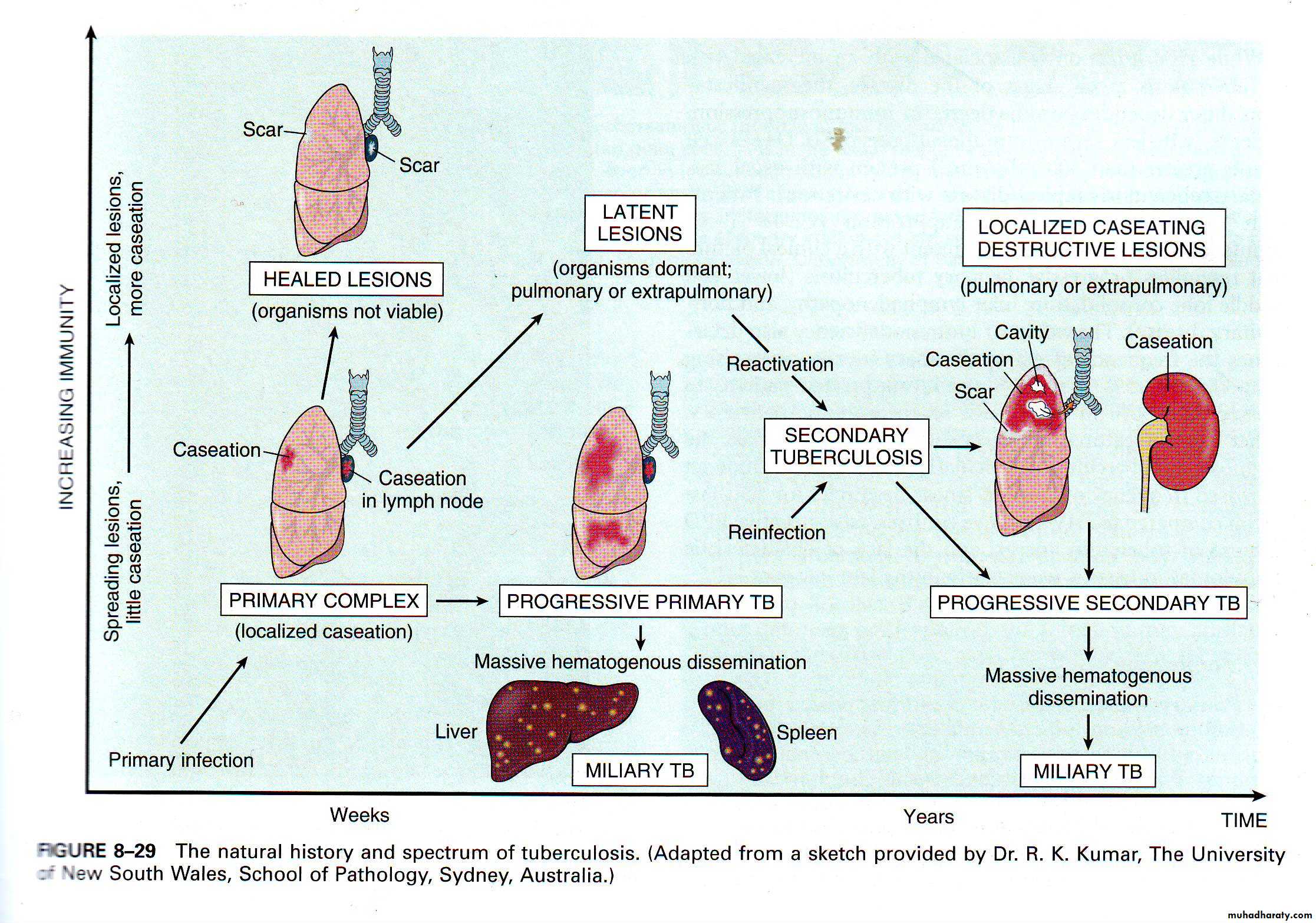
Primary tuberculosis
It follows initial exposure to TB bacilli in non immunized individuals of any age.Macroscopically: it forms a small sub pleural parenchymal lesion in the mid zone of the lung (Ghon focus) and spread to the hilar lymph nodes. Both lesions are called primary complex.(cheesy like material)
Microscopically: consist of epithelioid granuloma with central caseous necrosis.
95% of cases healed by fibrosis.
some may enter into dormant state & few may spread into the body forming progressive primary T.B.
Secondary T.B.
* Either occurs as a reinfection or reactivation of dormant bacilli from primary infection when there is impairment in the immunity of the patient.
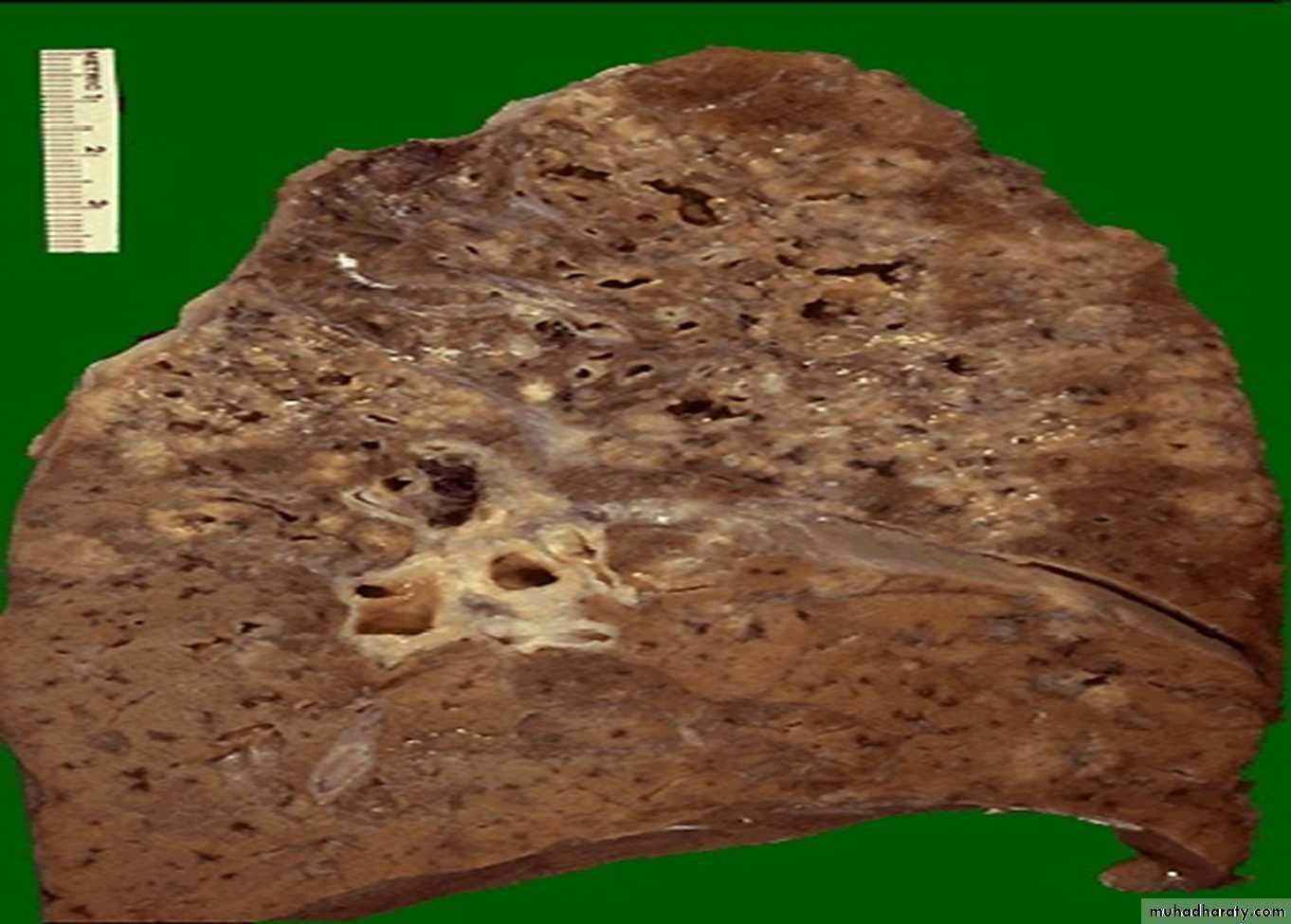
* Macroscopically : occurs at the apex of the lung with marked damage in the lung parenchyma with cavity formation
* Microscopical: epithelioid granulomatous with central caseous necrosis & cavity.
* Healing by fibrosis or may spread forming progressive secondary T.B.
primary complex of primary T.B.
Secondary T.B with Cavities
Progressive T.B.* Either from primary or secondary T.B.
* T.B. bacilli can be coughed into the larynx forming laryngeal T.B.
* or swallowed into the G.I.T causing intestinal T.B.
* or enter through bronchial tree leading to tuberculous bronchopneumonia or spread into the pleural cavity leading to pleural effusion.
• * or enter through the lymphatic channel or blood stream to produce either:
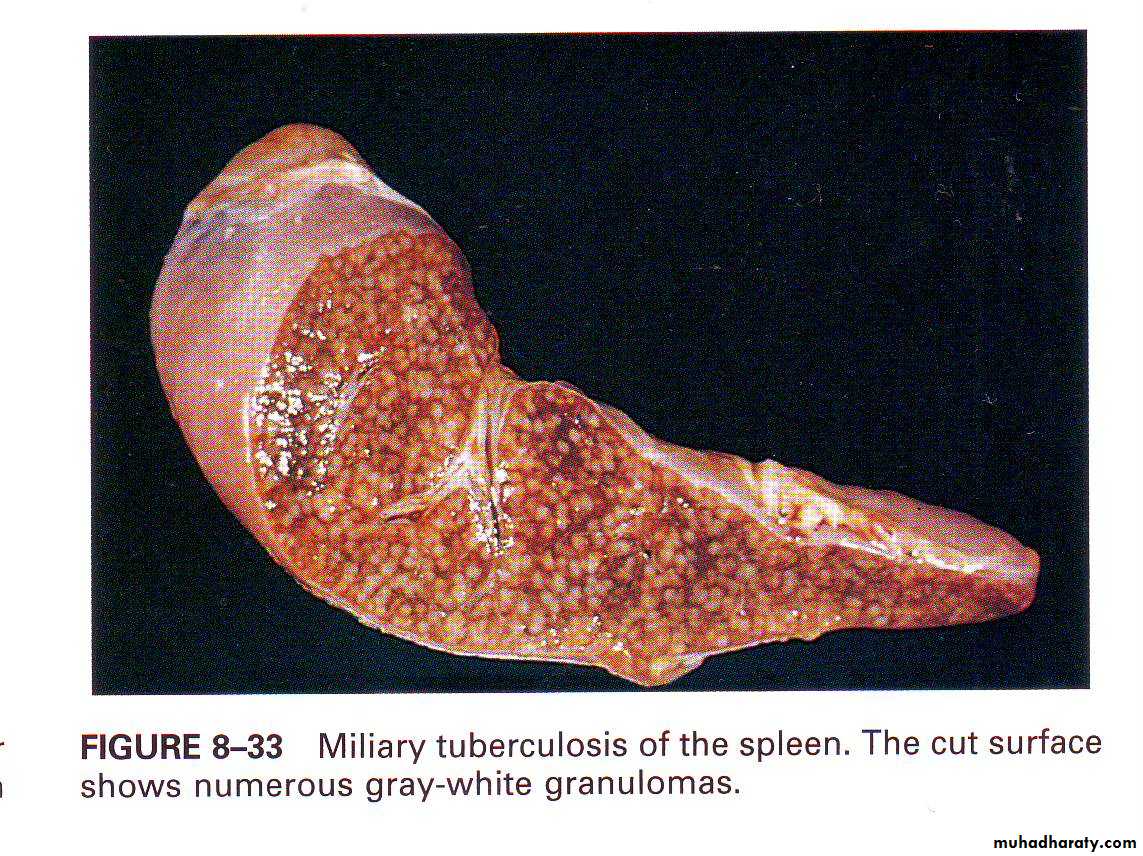
• 1)Miliary tuberculosis multiple small (2-mm) foci of yellow-white consolidation (“miliary” is derived from the resemblance of these foci to millet seeds) in numerous organs & tissues.
• 2)Isolated organ lesions e.g. in kidney, bone…….
Miliary tuberculosis of the spleen,cut surface show
numerous gray-white granulomasThe natural history and spectrum of tuberculosis
Clinical Features:
• Fever, cough, night sweating , hemoptysis and weight loss.Diagnosis:
• I- History.• II- Clinical examination.
• III- Investigation include :
• **X- ray
• **detection of the m.o in the specimen (sputum, in biopsy) by the use of Ziehl-Neelsen staining.
• **Biopsy of the infected tissue.
• **PCR amplification of T.B. bacilli
• .
Leprosy (Hansen ,S Disease)
-Caused by mycobacterium leprae
- Required long period of close contact with patients.
-Mode of infection is not clear probably by inhalation.
-it affects skin & peripheral nerves because the M.O. grows only in the cool tissue.
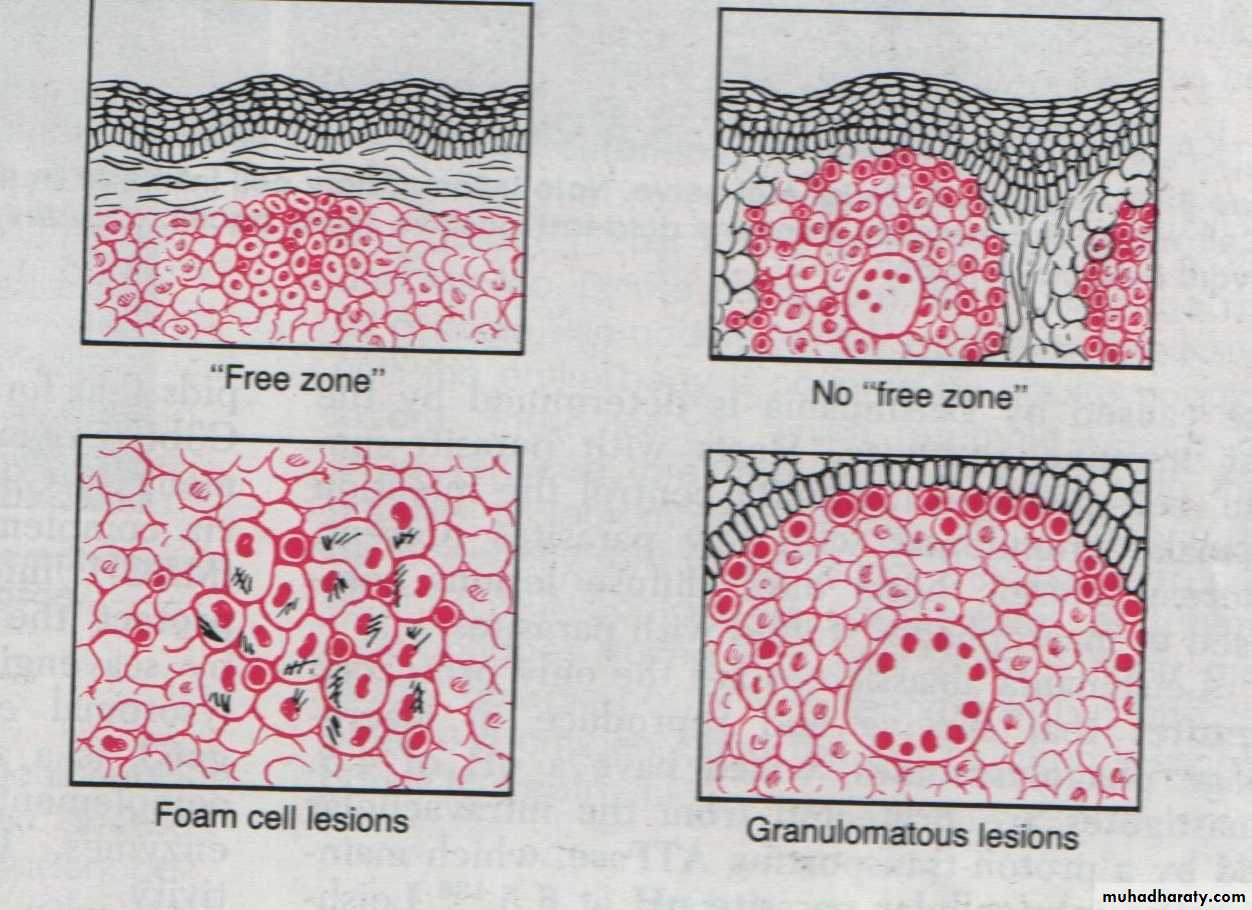
Pathogenesis of leprosy
Leprae bacilli produce no exotoxin or endotoxin, the lesion is produced by :distructive granuloma(type IV hypersensitivity)
interferance with metabolism of schwann cells.
2-Tuberculoid leprosy
1-Lepromatous leprosyIn patient with high immunity
In patients with low immunity
• Grossly: lesion consists of asymmetrical anesthetic macule & palpable thickened nerve.
• Grossly: lesion consists of symmetrical anesthetic nodules with deformity & ulceration, the lesions of the face lead leonine face.
not
may Involve the eye, larynx & testis
Coarse of the disease: Most of the patients get red of the bacilli by natural resistance , there are:
• Tuberculoid leprosy
• Microscopically:• Non caseating granuloma
• lymphocytes &bacilli are scanty
• Lepromatous leprosy Microscopically:
• The skin and nerve infiltrated by macrophages full of M. lepra bacilli,• Lymphocytes are few
• No granuloma
• 3- Borderline leprosy: the feature of this type is in between that of lepromatous and tuberculoid leprosy
Diagnosis of leprosy:
History of contact with patient.
Examination: anesthetic skin lesion, ulceration, deformity.
Investigation: take a biopsy and finding leprae bacilli using Modified Zeihl neelsen stain
Actinomycosis
ActinomycosisCaused by Actinomyces israellii
Virtually anaerobic, gram-positive, long filamentous bacteria.
It is a commensal m.o in the mouth , G.I.T., female genital tract., only occasionally they invade the tissues & produce infection.It may cause Cervicofacial lesion (70%), Abdomial lesion (15% ).
Pathology:Infection produces firm masses containing numerous abscesses ( honeycomb abscesses) bearing colonies as yellowish granules (sulfur granules) with sinuses & fistulae.
Histology:
• Chronic granulomatous inflammation with suppuration, bacterial colonies, surrounded by granulation tissue with thick walled capsule & septate.
The colony of actinomycosis at high magnification.The micro organism is filamentous & the filaments project
as red specular at the periphery of the colony which is surrounded by neutrophils (mycetoma).
Spirochetes
SyphilisCaused by spirochete ( treponema pallidum)It is a chronic venereal disease.
• (Spirochete: it is a gram negative, coiled, unicellular spiral shaped m.o.)
Transmission:
syphilis is a sexually transmitted disease. Also the disease may transmit through the placenta to the fetus (transplacental transmission)
Stages of syphilis :
Primary syphilis: -* Lesion (chancre) develops few days or approximately 3 weeks after infection on the external genital
* Chancre is a solitary, slowly enlarging, hard, painless nodule with superficial ulceration associated with enlarged regional lymph nodes.
* Healing occurs in 3-6 weeks either spontaneously or after treatment.
Secondary syphilis: -
Usually develops 1-3 months after infection& it occurs in approximately 75% of untreated patients.
Lesions appear as :
*flat or slightly elevated papules on external genitalia,
• *shallow buccal , lingual & pharyngeal ulcerations
*generalized skin rash,
*generalized lymphadenophathy.
Healing may occur spontaneously or after treatment.
Tertiary syphilis: -
It appears several years after primary infection (5-30) years. Tertiary syphilis has 3 main manifestations:
1-CVS syphilis
2-CNS neurosyphilis :
3-Gumma: formation firm to rubbery, multiple, nodular masses most commonly found in the liver , bones & testes.
(Gumma: it is Granuloma with central coagulative necrosis)
Histology of syphilis:
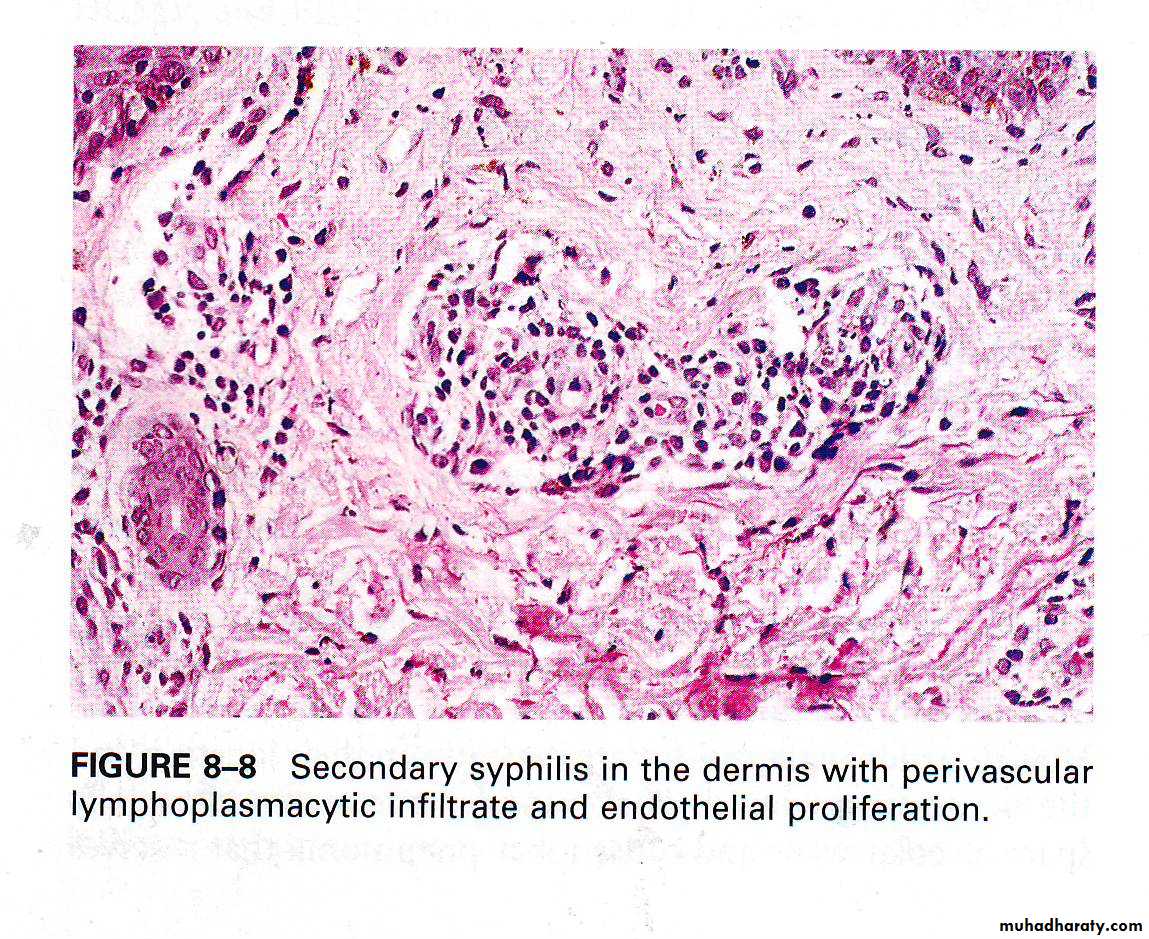
Proliferative endarteritis (endarteritis obliterance) affecting small vessels (endothelial hypertrophy & proliferation → intimal fibrosis) with a surrounding plasma cell infiltration are characteristic of all stages of syphilis.
In Tertiary syphilis in addition to this there is gumma (Granuloma with central coagulative necrosis).
Secondary syphilis, in the dermis with perivascular lymphoplasmacytic infiltrate & endarteritis obliterance.
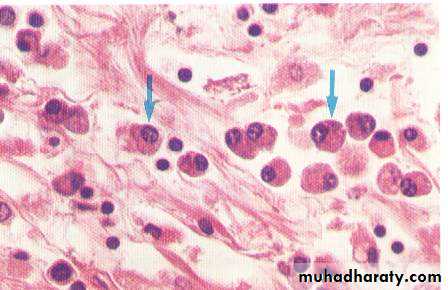
Plasma cells infiltration in syphilis
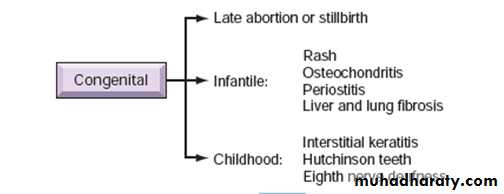
Congenital syphilis* It is due to transplacental spread, which occurs most frequently during primary & secondary syphilis, when the spirochetes are most numerous.
* May cause:
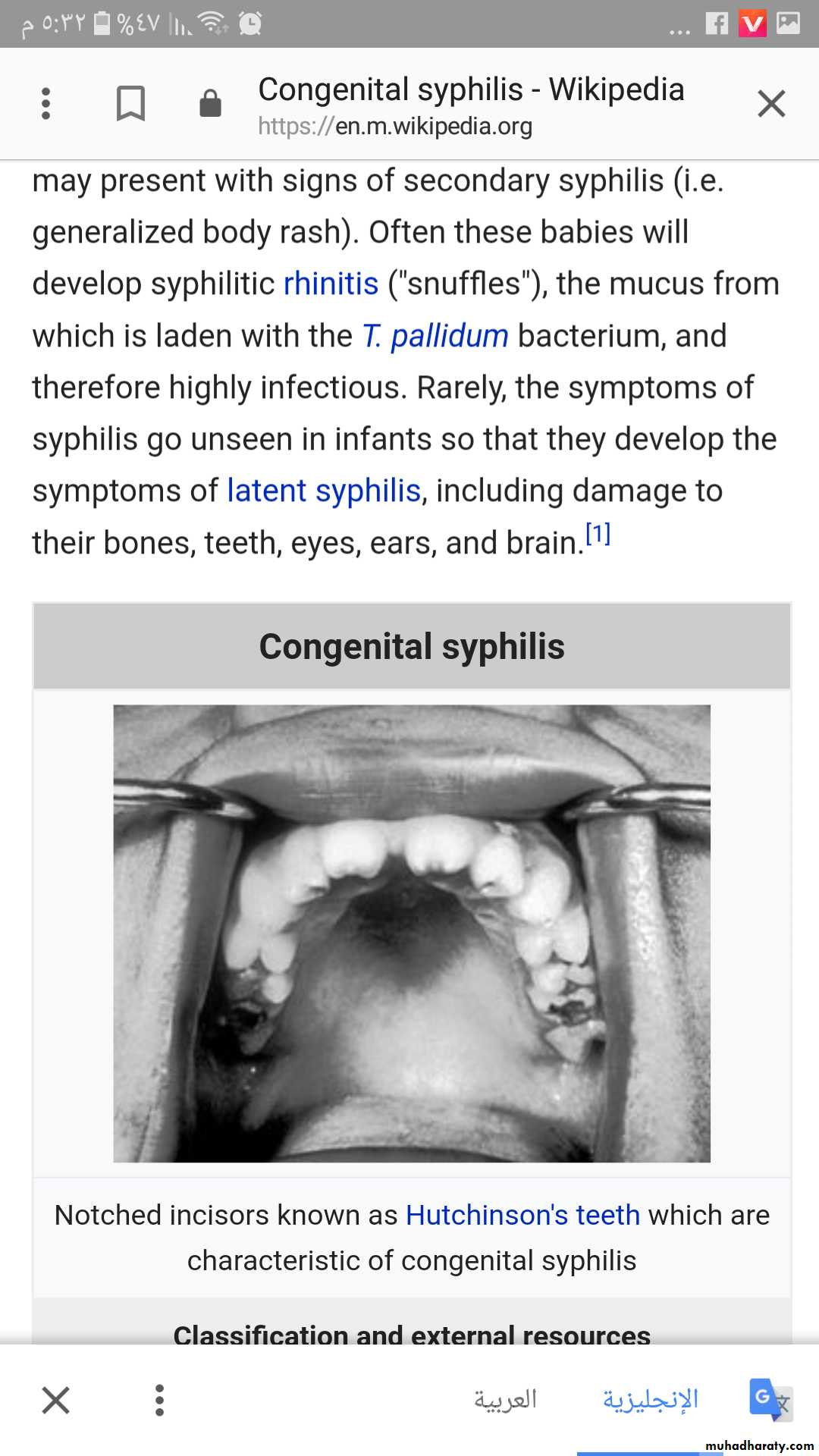
‘notched incisor Known as Hutchinson's teeth which are characteristic of congenital syphilis
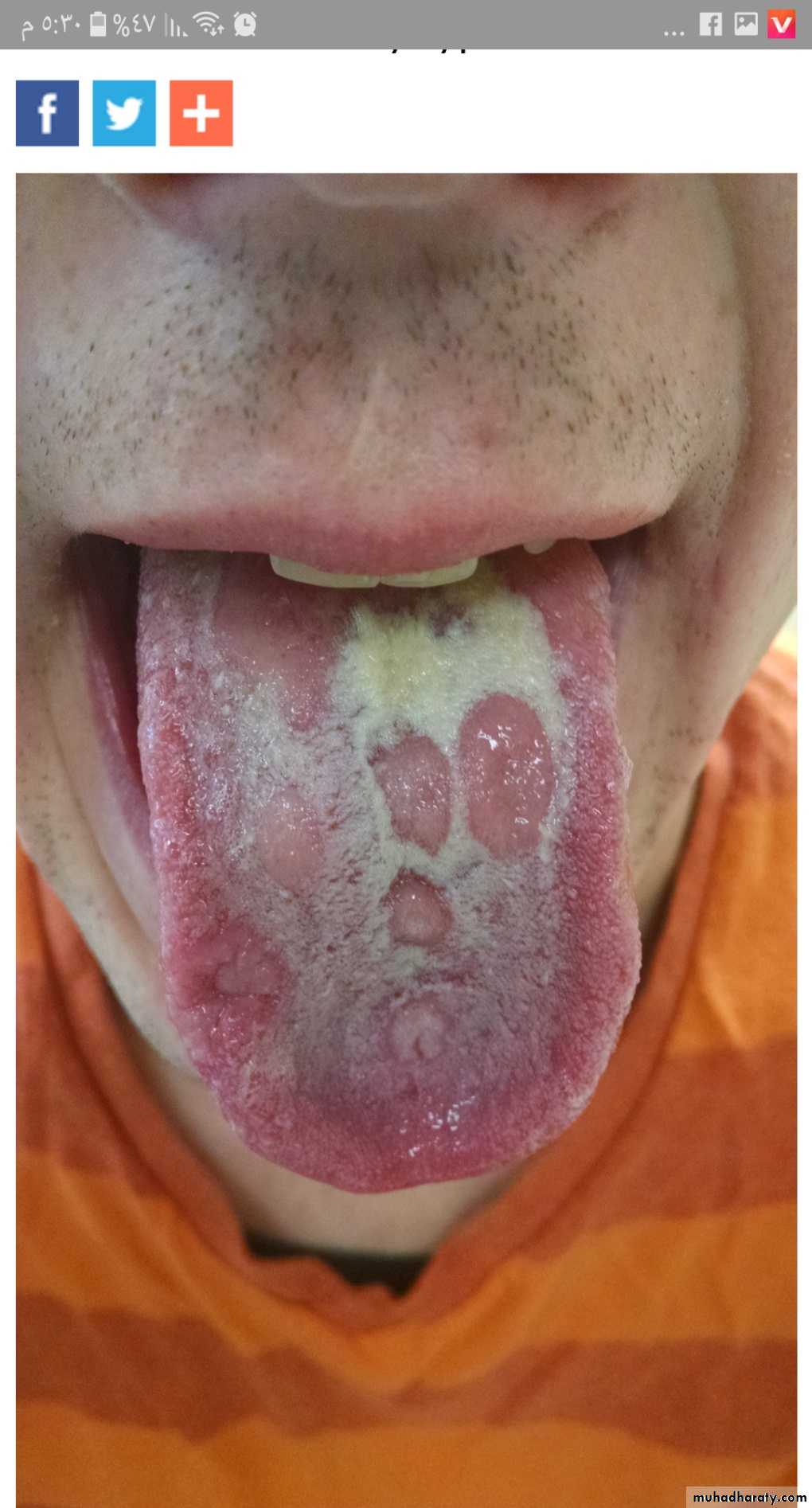
Multiple shallow, lingual
ulcerations in patient withsecondary syphilis
Diagnosis of syphilis:-
I- History.II- Clinical examination
III-Investigations: demonstrate the spirochetes,
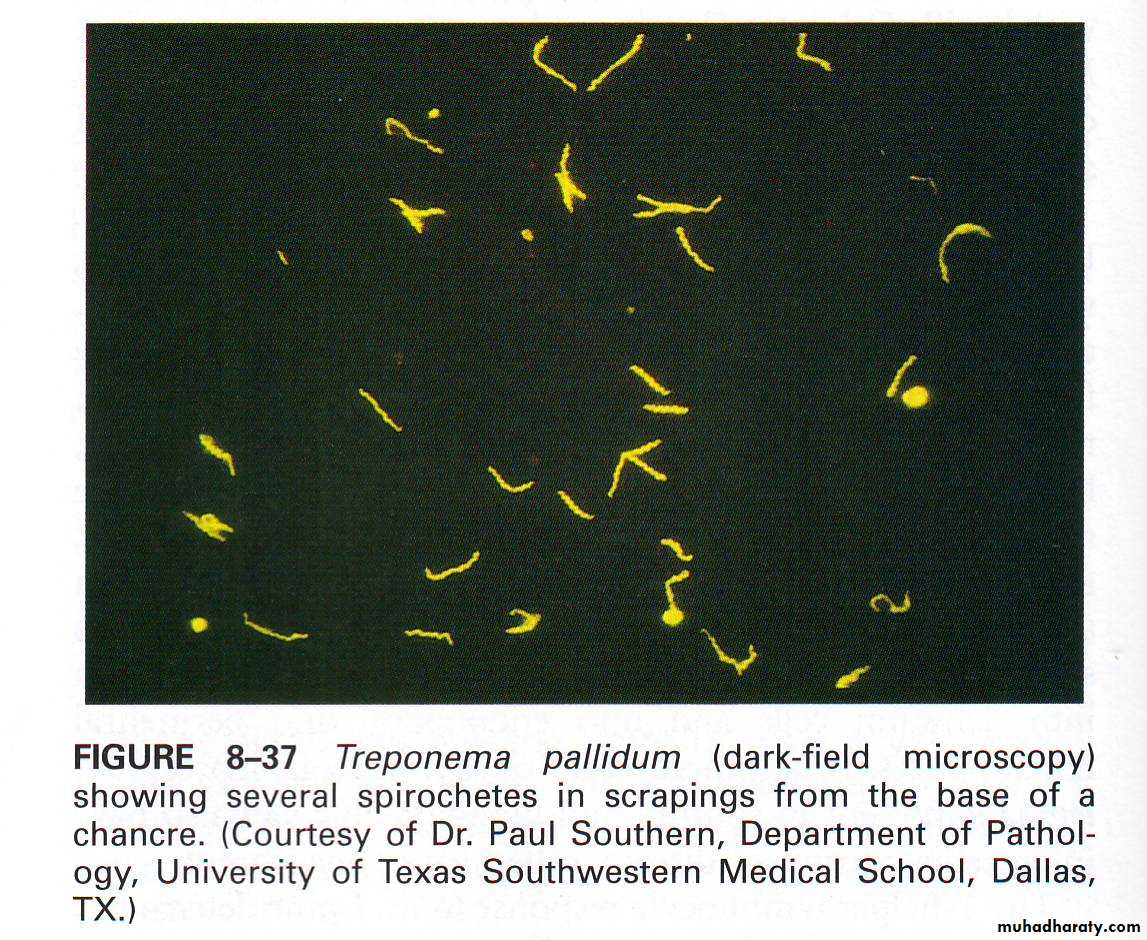
T. pallidum , is too slender to be seen in Gram stain, but it can be visualized by silver stains , dark field or by immunofluorescence.
-Serological tests
• -PCR test for syphilis.
Long, spiraling spirochetes are seen with a silver stain.
Treponema pallidum (dark field microscopy) showing
several spirochetes scraping from the base of a chancre