Cardiac Lectures Dr. Ahmed Moyed Hussein
Supraventricular arrhythmias:Sinoatrial nodal rhythms:
Sinus arrhythmia: Phasic alteration of the heart rate during respiration (the sinus rate increases during inspiration and slows during expiration) is a consequence of normal parasympathetic nervous system activity and can be pronounced in children. Absence of this normal variation in heart rate with breathing or with changes in posture may be a feature of autonomic neuropathy.
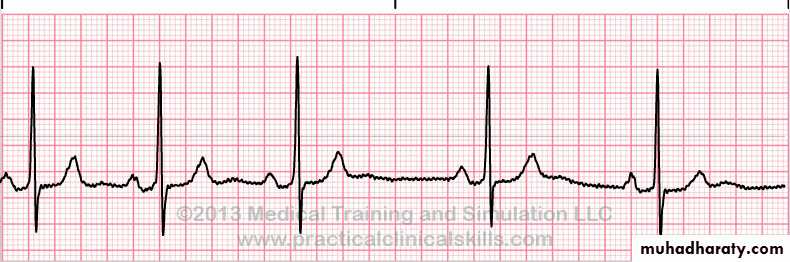
Fig: sinus arrhythmia
Sinus bradycardia: A sinus rate of less than 60/min may occur in healthy people at rest and is a common finding in athletes. Some pathological causes include:Myocardial Infarction
Sinus node disease (sick sinus syndrome)
Hypothermia
Hypothyroidism
Cholestatic jaundice
Raised intracranial pressure
Drugs, e.g. β-blockers, digoxin, verapamil
Fig: sinus bradycardia
sinus bradycardia requires no treatment. Symptomatic acute sinus bradycardia usually responds to intravenous atropine 0.6–1.2 mg.
Sinus tachycardia:
This is defined as a sinus rate of more than 100/min, and is usually due to an increase in sympathetic activity associated with exercise, emotion, pregnancy or pathology, like:Fever
Anaemia
Heart failure
Thyrotoxicosis
Phaeochromocytoma
Drugs, e.g. β-agonists (bronchodilators)
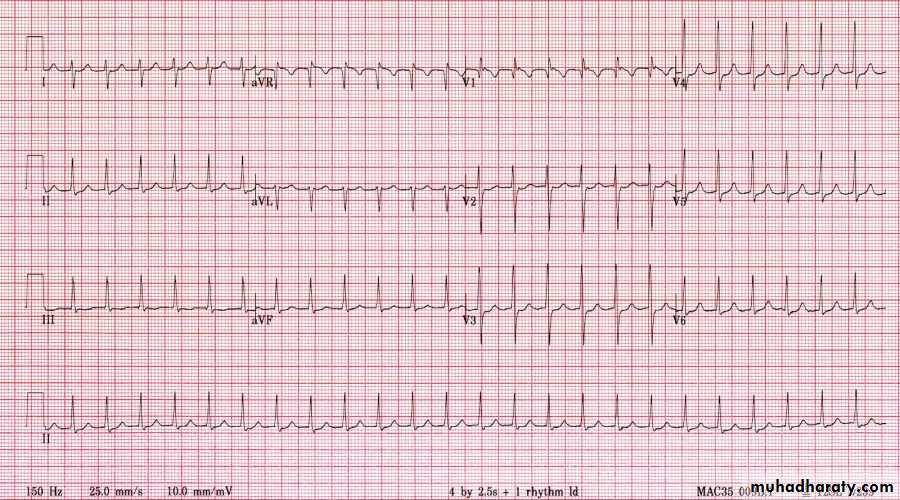
Fig: sinus tachycardia
Treatment of sinus tachycardia is the treatment of underlying cause.Sinoatrial (SA node) disease (sick sinus syndrome):
Sinoatrial disease can occur at any age but is most common in older people. The underlying pathology involves fibrosis, degenerative changes or ischemia of the SA (sinus) node. The condition is characterized by a variety of arrhythmias:and may present with palpitation, dizzy spells or syncope.
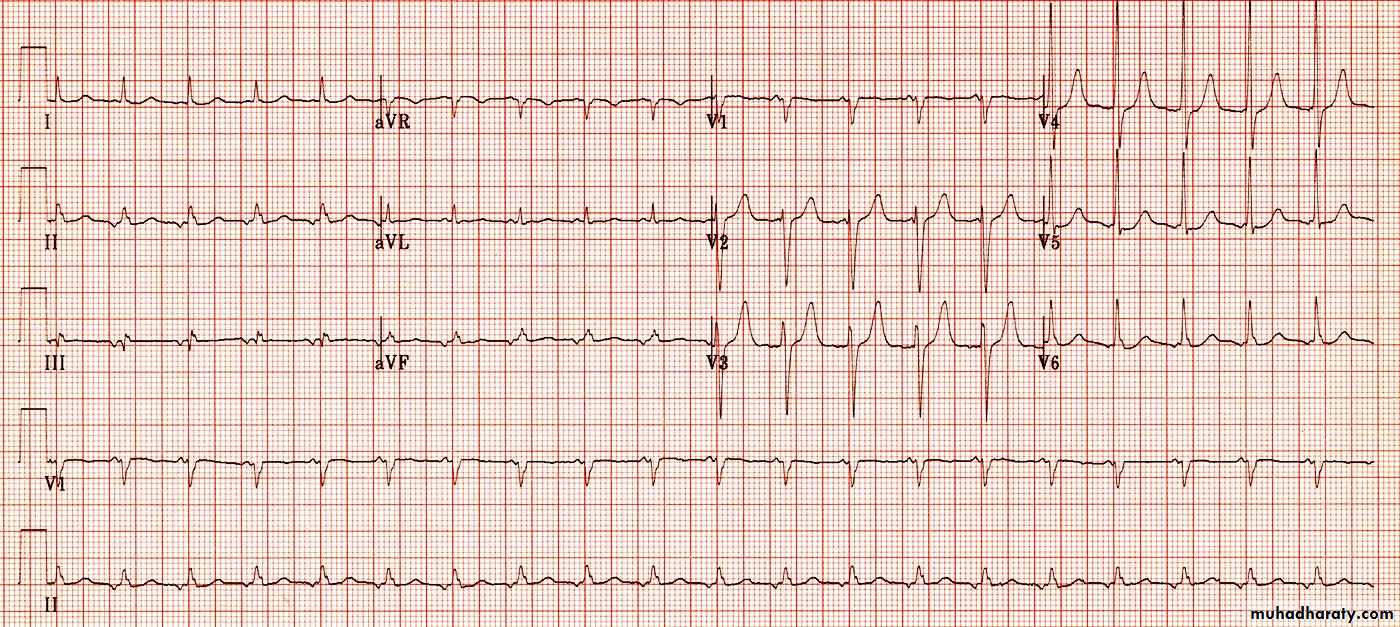
Fig: sick sinus syndrome
A permanent pacemaker may benefit patients with troublesome symptoms due to spontaneous bradycardias. Pacing improves symptoms but not prognosis, and is not indicated in patients who are asymptomatic. Attacks of tachycardia can controlled by drug therapy.
Atrial tachyarrhythmias
Atrial ectopic beats (extrasystoles, premature beats):These usually cause no symptoms but can give the sensation of a missed beat or an abnormally strong beat. The ECG shows a premature but otherwise normal QRS complex; if visible, the preceding P wave has a different morphology because the atria activate from an abnormal site.
Fig: atrial ectopic beats (second and 7th beat)
In most cases, these are of no consequence. Treatment is rarely necessary but β-blockers can be used if symptoms are intrusive.Atrial tachycardia:
Atrial tachycardia may be a manifestation of increased atrial automaticity, sinoatrial disease or digoxin toxicity. It produces a narrow-complex tachycardia with abnormal P-wave morphology, sometimes associated with AV block if the atrial rate is rapid. It may respond to β-blockers, which reduce automaticity, or class I or III anti-arrhythmic drugs.Fig: atrial tachycardia (rate= 120 BPM, narrow QRS complex, inverted P wave)
Supraventricular tachycardias:
The term ‘supraventricular tachycardia’ (SVT) is commonly used to describe regular tachycardias that have a similar appearance on ECG. These are usually associated with a narrow QRS complex and are characterized by a re-entry circuit or automatic focus involving the atria.
Atrioventricular nodal re-entrant tachycardia (AVNRT):
is due to re-entry in a circuit involving the AV node, This produces a regular tachycardia with a rate of 120–240/min. It tends to occur in the absence of structural heart disease and episodes may last from a few seconds to many hours. The patient is usually aware of a rapid, very forceful, regular heart beat and may experience chest discomfort, lightheadedness or breathlessness. Polyuria, mainly due to the release of atrial natriuretic peptide, is sometimes a feature. The ECG usually shows a tachycardia (regular) with normal QRS complexes.Fig: SVT
Management:Episode may be terminated by carotid sinus pressure or by the Valsalva manoeuvre (vagal stimulation). Adenosine (3–12 mg rapidly IV) or verapamil (5 mg IV over 1 min) will restore sinus rhythm in most cases. Intravenous β-blocker or flecainide can also be used. In rare cases, when there is severe haemodynamic compromise (systolic BP< 90mmhg, impaired sensorium, chest pain or pulmonary oedema) the tachycardia should be terminated by DC cardioversion.
In patients with recurrent SVT, catheter ablation is the most effective therapy and will permanently prevent SVT in more than 90% of cases. Alternatively, prophylaxis with oral β-blocker, verapamil or flecainide may be used.
Wolff–Parkinson–White syndrome(WPW) and atrioventricular re-entrant tachycardia (AVRT):
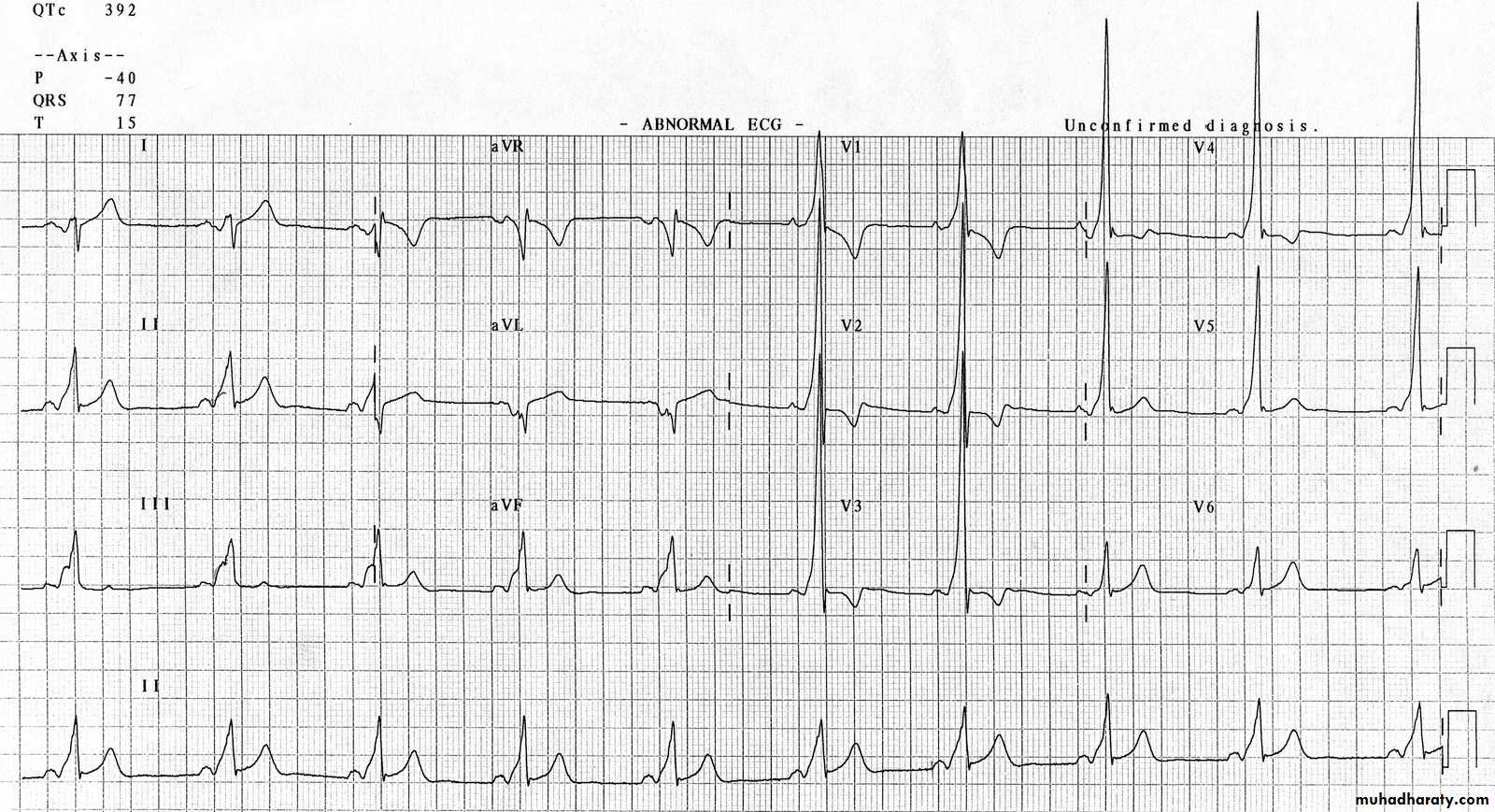
Here, an abnormal band of conducting tissue connects the atria and ventricles. This ‘accessory pathway’ comprises rapidly conducting fibers which resemble Purkinje tissue. Premature ventricular activation via the pathway shortens the PR interval and produces a ‘slurred’ initial deflection of the QRS complex, called a delta wave. As the AV node and accessory pathway have different conduction speeds and refractory periods, a re-entry circuit can develop, causing tachycardia, The ECG during this tachycardia is almost indistinguishable from that of AVNRT.
Carotid sinus pressure or intravenous adenosine can terminate the tachycardia. Catheter ablation is first-line treatment in symptomatic patients and is nearly always curative. Alternatively, prophylactic anti-arrhythmic drugs, such as flecainide or propafenone, can be used to slow conduction in the accessory pathway.