Investigations in heart failure
Blood tests. Full blood count, liver biochemistry, urea and electrolytes, cardiac enzymes in acute heart failure, BNP or N-terminal portion of proBNF (NP proBNP),Natriuretic peptides (ANP, BNP)
Atrial natriuretic peptide (ANP) is released from atrial myocytes in response to stretch. ANP induces diuresis, natriuresis, vasodilatation and suppression of the renin-angiotensin system. Levels of circulating ANP are increased in congestive cardiac failure and correlate with functional class.
Brain natriuretic peptide (BNP) (so called because it was first discovered in brain) is predominantly secreted by the ventricles, and has an action similar to that of ANP but greater diagnostic and prognostic value .
Chest X-ray
A rise in pulmonary venous pressure from left-sided heart failure first shows on the chest X-ray as an abnormal distension of the upper lobe pulmonary veins (with the patient in the erect position). The vascularity of the lung fields becomes more prominent, Subsequently, interstitial oedema causes thickened interlobular septa and dilated lymphatics. These are evident as horizontal lines in the costophrenic angles (septal or ‘Kerley B’ lines). More advanced changes due to alveolar oedema cause a hazy opacification spreading from the hilar regions, and pleural effusions.
Electrocardiogram for ischaemia, hypertension or arrhythmia.
Echocardiography. Cardiac chamber dimension, systolic and diastolic function, regional wall motion abnormalities, valvular heart disease, cardiomyopathies.
Cardiac catheterization. Diagnosis of ischaemic heart failure (and suitability for revascularization), measurement of pulmonary artery pressure, left atrial (wedge) pressure, left ventricular end-diastolic pressure.
Cardiac biopsy. Diagnosis of cardiomyopathies, e.g. amyloid, follow-up of transplanted patients to assess rejection.
Ambulatory 24-hour ECG monitoring (Holter). In patients with suspected arrhythmia. May be used in patients with severe heart failure or inherited cardiomyopathy to determine if a defibrillator is appropriate.
Management of acute pulmonary oedema
This is urgent:
• Sit the patient up in order to reduce pulmonary congestion.
• Give oxygen (high-flow, high-concentration). Noninvasive positive pressure ventilation (continuous positive airways pressure (CPAP).
• Administer nitrates, such as i.v. glyceryl trinitrate or buccal glyceryl trinitrate 2–5 mg, titrated upwards every 10 minutes, until clinical improvement occurs or systolic BP falls to < 110 mmHg.
• Administer a loop diuretic such as furosemide 50–100 mg i.v.
If these measures prove ineffective, inotropic agents may be required to augment cardiac output, particularly in hypotensive patients.
Management of chronic heart failure
Treatment is aimed at relieving symptoms, prevention and control of disease leading to cardiac dysfunction and heart failure, retarding disease progression and improving quality and length of life.
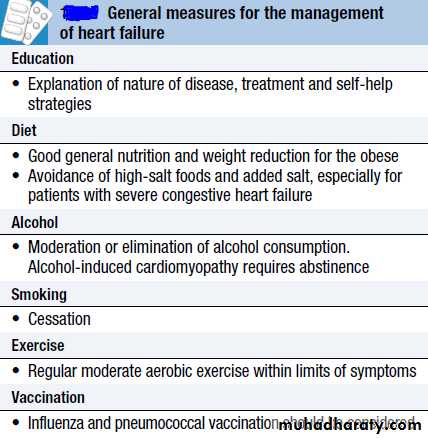
General measure
Drug management
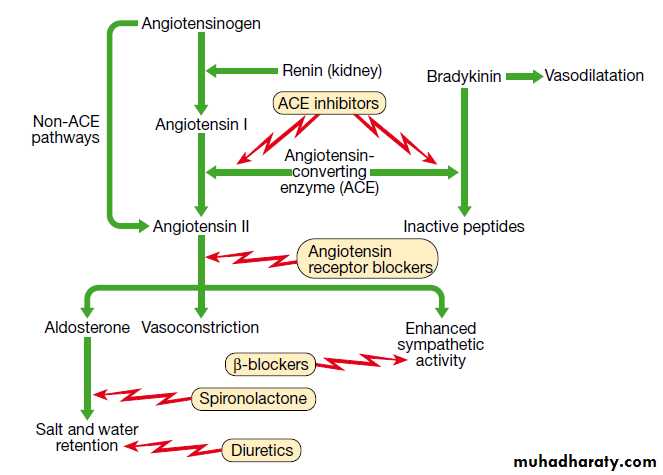
DiureticsThese act by promoting the renal excretion of salt and water by blocking tubular reabsorption of sodium and chloride. Loop diuretics (e.g. furosemide and bumetanide) and thiazide diuretics (e.g. bendroflumethiazide, hydrochlorothiazide) should be given in patients with fluid overload.
Although diuretics provide symptomatic relief of dyspnoea and improve exercise tolerance, there is limited evidence that they affect survival. In severe heart failure patients, the combination of a loop and thiazide diuretic may be required.
Angiotensin-converting enzyme inhibitors (ACEI)
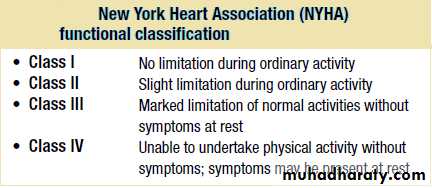
Trials have shown that in addition to producing considerable symptomatic improvement in patients with symptomatic heart failure, prognosis is markedly improved and development of heart failure is slowed. ACEI also benefit patients with asymptomatic heart failure following myocardial infarction. Thus ACEI improve survival in patients
in all functional classes (NYHA I-IV) and are recommended in all patients at risk of developing heart failure.
Angiotensin II receptor antagonists (ARA)
The angiotensin II receptor antagonists (ARA) (candesartan and valsartan) are indicated as second-line therapy in patients intolerant of ACEI. Unlike ACEI they do not affect bradykinin metabolism and do not produce a cough.
Beta-blockers
Beta-blockade helps to counteract the deleterious effects of enhanced sympathetic stimulation and reduces the risk of arrhythmias and sudden death.Beta-blockers have been shown to improve functional status and reduce cardiovascular morbidity and mortality in patients with heart failure. Bisoprolol and carvedilol reduce mortality in any grade of heart failure.
Nebivolol is used in the treatment of stable mild–moderate heart failure in patients over 70 years old.
In patients with significant heart failure, beta-blockers are started at a low dose and gradually increased.
Aldosterone antagonists
The aldosterone antagonists spironolactone and eplerenone have been shown to improve survival in patients with heart failure, gynaecomastia
or breast pain occurred in 1 in 10 men taking spironolactone. .
Cardiac glycosides
Digoxin is a cardiac glycoside that is indicated in patients in atrial fibrillation with heart failure. It is used as add-on therapy in symptomatic heart failure patients already receiving ACEI and beta-blockers. Studies demonstrated that digoxin reduced hospital admissions in patients with
heart failure.
Vasodilators and nitrates
The combination of hydralazine and nitrates reduces afterload and pre-load and is used in patients intolerant of ACEI or ARA. Studies demonstrated that the combination of hydralazine (with nitrates) improved survival in patients with chronic heart failure.
Inotropic and vasopressor agents
Intravenous inotropes and vasopressor agents are used in patients with chronic heart failure who are not responding to oral medication. Although they produce haemodynamic improvements they have not been shown to improve long-term mortality when compared with placebo.
Amiodarone
This is a potent anti-arrhythmic drug that has little negative inotropic effect and may be valuable in patients with poor left ventricular function. It is only effective in the treatment of symptomatic arrhythmias, and should not be used as a preventative agent in asymptomatic patients.
Other medications
In hospital, all patients require prophylactic anticoagulation. Heart failure is associated with a four-fold increase in the risk of a stroke. Oral anticoagulants are recommended in patients with atrial fibrillation and in patients with sinus rhythm with a history of thromboembolism, left ventricular thrombus or aneurysm. In patients with known ischaemic heart disease antiplatelet therapy (aspirin, clopidogrel) and statin therapy
should be continued.
Arrhythmias are frequent in heart failure and are implicated in sudden death. Although treatment of complex ventricular arrhythmias might be expected to improve survival, there is no evidence to support this and it
may increase mortality.Patients with heart failure and symptomatic ventricular arrhythmias should be assessed for suitability for an ICD.
Non-pharmacological treatment of heart failure
Revascularization
While coronary artery disease is the most common cause of heart failure, the role of revascularization in patients with heart failure is unclear. Patients with angina and left ventricular dysfunction have a higher mortality from surgery (10– 20%), but have the most to gain in terms of improved symptoms and prognosis. Factors that must be considered
before recommending surgery include age, symptoms and
evidence for reversible myocardial ischaemia.
Hibernating myocardium and myocardial stunning
‘Hibernating’ myocardium can be defined as reversible left ventricular dysfunction due to chronic coronary artery disease that responds positively to inotropic stress and indicates the presence of viable heart muscle that may recover after revascularization.
Myocardial stunning is reversible ventricular dysfunction that persists following an episode of ischaemia when the blood flow has returned to normal, i.e. there is a mismatch between flow and function.
The clinical relevance of the hibernating and stunned myocardium is that ventricular dysfunction due to these mechanisms may be wrongly ascribed to myocardial necrosis and scarring which seems untreatable, whereas reversible hibernating and stunning respond to coronary Revascularization.
Implantable cardiac defibrillators
and resynchronisation therapyPatients with symptomatic ventricular arrhythmias and heart failure have a very poor prognosis. Irrespective of their response to anti-arrhythmic drug therapy, all should be considered for implantation of a cardiac defibrillator Intracardiac defibrillator( ICD).
In patients with marked intraventricular conduction delay, prolonged depolarisation may lead to uncoordinated left ventricular contraction. When this is associated with severe symptomatic heart failure, cardiac
resynchronisation therapy (CRT) should be considered.
Here, both the LV and RV are paced simultaneously in an attempt to generate a more coordinated left ventricular contraction and improve cardiac output.
Cardiac transplantation
Cardiac transplantation has become the treatment of choice for younger patients with severe intractable heart failure, whose life expectancy is <6 months. With careful recipient selection, the expected 1-year survival for patients following transplantation is over 90%, and is 75% at 5 years. Irrespective of survival, quality of life is dramatically improved for the
majority of patients. The availability of heart transplantation is limited.
Ventricular assist devices
Because of the limited supply of donor organs, ventricular assist devices (VADs) have been employed as:
• a bridge to cardiac transplantation
• potential long-term ‘destination’ therapy
• short-term restoration therapy following a potentially reversible insult such as viral myocarditis.