• The Periodontal Examination and Diagnosis
Dr . HUSSEIN AL DABBAGH• Periodontal Examination
• Objectives:
• Identify the pathological changes of the periodontal tissues• Accurately collect/chart following clinical data:
• » Probing depth.
• » Bleeding on probing points/Suppuration
• » Furcation involvements.
• » Tooth mobility/ fremitus.
• » Gingival recession.
• » Mucogingival defects.
• » Plaque score.
• Analyze the clinical data and develop an overall diagnosis for the patient.
• Periodontal Examination
• Review of medical/dental history.
• Gingival Examination.• Probing Depth (PD).
• Clinical Attachment Level (CAL). Bleeding upon Probing (BOP).
• Mobility Assessment/fremitus. Furcation Assessment
• Periodontal Examination
• Occlusal Assessment Mucogingival Assessment Radiographs
• Tooth vitality Etiologic/risk factors• Periodontal Examination
• Gingival Examination.• – Evaluate tissue changes in terms of:
• » Color.
• » Consistency.
• » Contour.
• Healthy vs. Diseased Tissues
• Normal
• Diseased• Color
• Pale pink ± pigmentation
• Acute: Red
• Chronic: bluish pink bluish red (cyanotic)
• contour
• Marginal gingiva Knife- edge margin ± stippling
• Follows a curved line about the tooth.
• Marginal gingiva: Rounded Rolled bulbous• Healthy vs. Diseased Tissues
• Normal
• Diseased• Contour (Cont.)
• Papillae: (1)Normal contact, papilla is pointed
• and pyramidal, fills the interproximal area.
• (2)Space(diastema): flat or saddle -shape
• Papillae:
• Bulbous Flattened blunted Cratered
• Consistency
• Firm, resilient
• Edematous Fibrotic
• Periodontal Examination
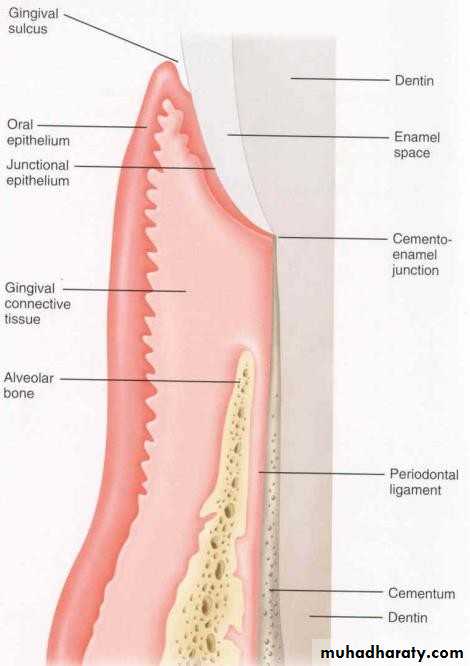
• Normal Healthy Gingival Unit
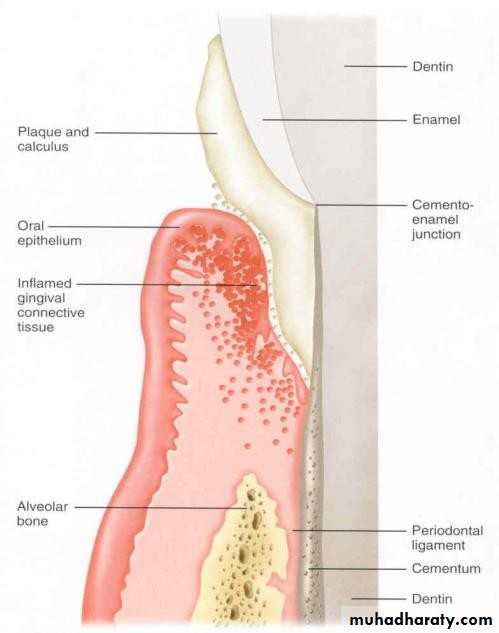
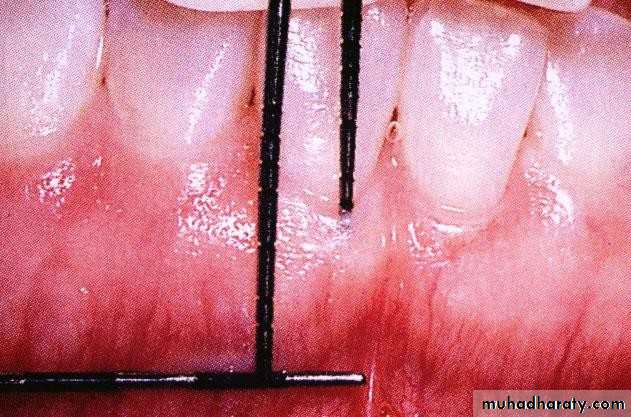
• Periodontal Examination Diseased Periodontium• Inflamed Gingival Unit - Changes in Color, Contour and Consistency
• Inflamed Interdental Papillae and Rolled Gingival Margins• Periodontal Examination
• :Gingival Indices
• Used for evaluation and quantitation of gingivitis.• Used for epidemiological studies.
• Periodontal Examination
• Gingival Indices: (cont’)• :(Gingival Index (GI) (Loe & Silness
• Widely used in epidemiological studies.• Scores gingival inflammation from 0-3 on the facial, lingual and mesial surfaces of all teeth.
• Gingival Index (GI) (Loe & Silness)
• Grade• 0
• Normal gingiva, no inflammation,
• No discoloration, no bleeding.
• 1
• Mild inflammation, Slight color change, mild alteration of gingival surface, no bleeding.• 2
• Moderate inflammation, erythema, swelling, bleeding on probing or when pressure applied.
• 3
• Severe inflammation, severe erythema and swelling, tendency toward spontaneous hemorrhage, some ulceration.• Periodontal Examination
• Review of medical/dental history.
• Gingival Examination.• Probing Depth (PD).
• Clinical Attachment Level (CAL Mobility Assessment/fremitus.
• Occlusal Assessment Furcation Assessment
• Periodontal Pocket
• Intact Periodontal Pocket
Red area indicates
Remaining attachment
• Red area indicates Remaining attachment
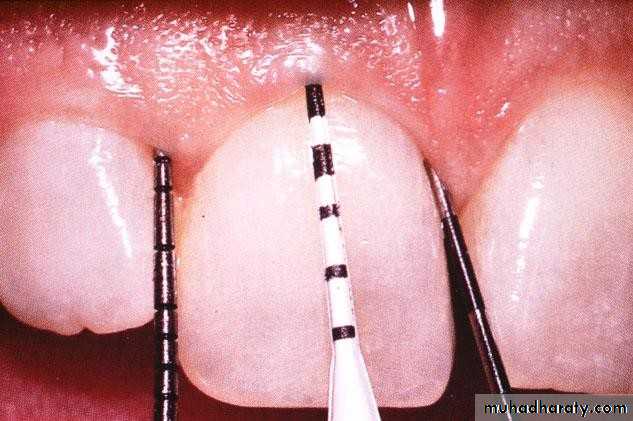
• Periodontal Examination• Probing Depth:
• The distance from the soft tissue (gingiva or alveolar mucosa)
• margin to the tip of the periodontal probe during usual periodontal diagnostic probing.
• the health of attachment can affect the measurement.
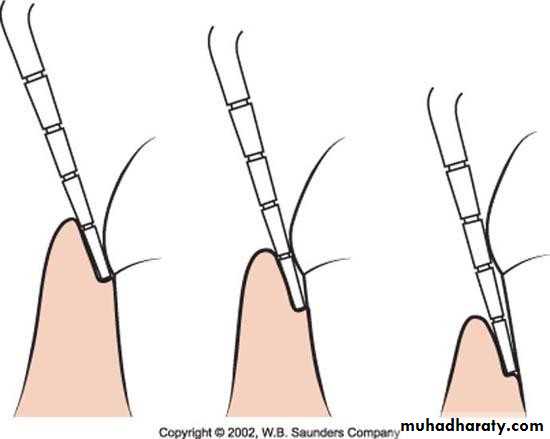
• Periodontal Examination Probing
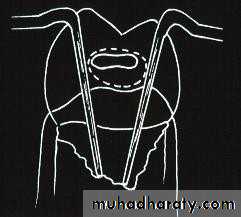
Correct Angulation of Probe• Periodontal pocket
• AA
• A• B
• C
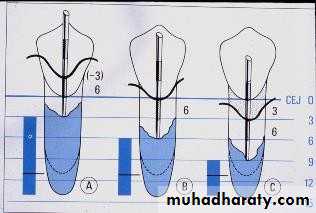
• A: gingival pocket.
• B: suprabony pocket.
• C: intrabony pocket
• Periodontal pocket
• A
• B• C
• A: simple pocket.
• B: compound pocket.
• C: complex pocket.• Periodontal Examination
• Factors Affecting Probing Depth:
• Inflammation.• Presence of subgingival calculus. Angulation of probe.
• Probing force.
• Probe tip diameter.
• Patient comfort and tolerance.
• Periodontal Examination
• This probe is said to deliver a known force (20g).
• The 20g is delivered when the the two part of the probe meet. (Pro-Dentec, Batesville, AR)
Constant force probe
• Periodontal Examination
:Clinical Attachment level
Definition:the distance from CEJ to the tip of a periodontal probe (base of the pocket) during usual periodontal diagnostic probing. The health of Attachment apparatus can affect The measurement
• Periodontal Examination
• Clinical Attachment level• Measuring Clinical Attachment Level
• Periodontal Examination• Bleeding on Probing (BOP)
• Objective sign of gingival Inflammation.
• Periodontal Examination
• Bleeding on Probing (BOP)• Causes of BOP: -
• -Gingival inflammation.
• - Multiple repeated probe insertion at a single site.
• - Excessive probing force.
• - Probing force >0.25N results in BOP in healthy sites..
• Periodontal Examination
• Bleeding on Probing (BOP)• Clinical significance
• - At a single examination, presence BOP from a site is not strongly related to progression of
• Periodontitis.
• - In treated patients on recall program continual absence of BOP is an excellent predictor of periodontal stability..
• Periodontal Examination
• Bleeding on Probing (BOP)• Clinical significance
• . In patients on recall/maintenance program, sites that exhibit BOP on consecutive visits are at a threefold greater risk for progression than sites that only occasionally bleed.
•
• Periodontal Examination Tooth Mobility
• Causes of mobility:• 1\Trauma from occlusion.
• 2\ Inflammation.
• 3\ Loss of support.
• 4\ Non-periodontal causes.
• Periodontal Examination
• Scale for Mobility Assessment• Grade I
• Grade II
• Slight• Moderate
• Up to 1 mm• Between
• 1-2mm• Grade III
• Advanced
• Over 2 mm and Tooth depressible
• Periodontal Examination Fremitus
• Palpable or visible movement of a tooth when subjected to occlusal forces.
• Associated with increase bone and attachment loss.• Periodontal Examination Fremitus
• Place index finger on labial Surface of maxillary teeth.
• Ask the patient to grind in lateral and protrusive Movement.• Any movement seen or felt is termed fremitus.
• Periodontal Examination
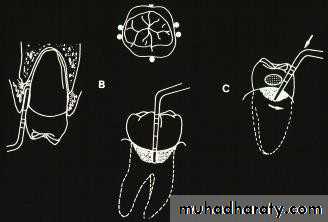
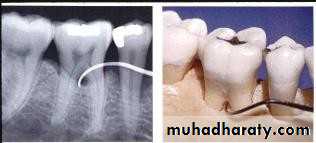
• Furcation Assessment• How do you evaluate and diagnose furcation Involvement?
• Probing Radiographs• Periodontal Examination
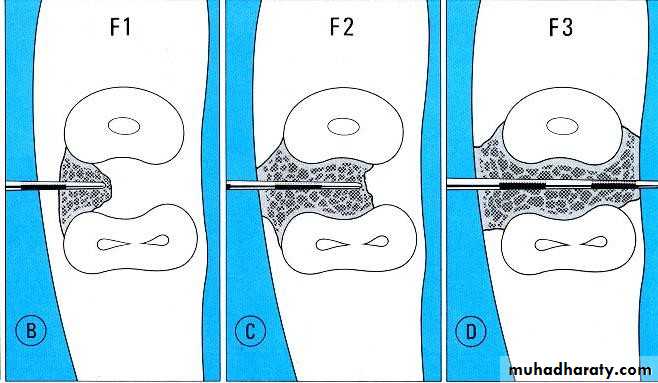
• Furcation Assessment• Furcation Classification:
• Hamp et al.1975
• Grade I: horizontal penetration
• < 3mm• Grade II: horizontal penetration
• > 3mm but not through and
• through.
• Grade III: through and through
• Periodontal Examination
• Furcation Assessment• What is the prevalence of furcation involvement
What is the prevalence of furcation involvement?
*In periodontal patients > 40 years old, all second molars had furcation involvement.
*Maxillary molars > mandibular molars
*Highest frequency of involvement, U6 Distal
*Greater severity of furcation involvement in smokers
• Periodontal Examination
Etiology of furcation invasion: -
* Extension of inflammatory periodontal disease.
*- Pulpal disease.
*- Defective plaque retentive restorations.
*- Anatomical variations:
Enamel pearl.
Cervical enamel projections
. Existence of accessory
pulpal canals.
• Periodontal Examination
• Furcation Assessment• What is the Prevalence of CEPs?
• Masters & Hoskins 1964
• – 29% of mandibular & 17% of maxillary molars
• – mostly found in buccal furcations
• Grewe & Meshkin 1965
• 20% L7 > U7 > L6 > U6.
• Lieb et al.1965
• 25% mandibular & 22% maxillary molars
• Hou & Tsai 1987
• 45% of molars; L6 > U6 > L7 > U7 >L8 > U8
• Periodontal Examination
• Furcation Assessment
Cervical Enamel Pearl: – Incidence: 1.1%-9.7% (mean 2.69 %).
– Predilection for maxillary third and second molars.
• Periodontal Examination
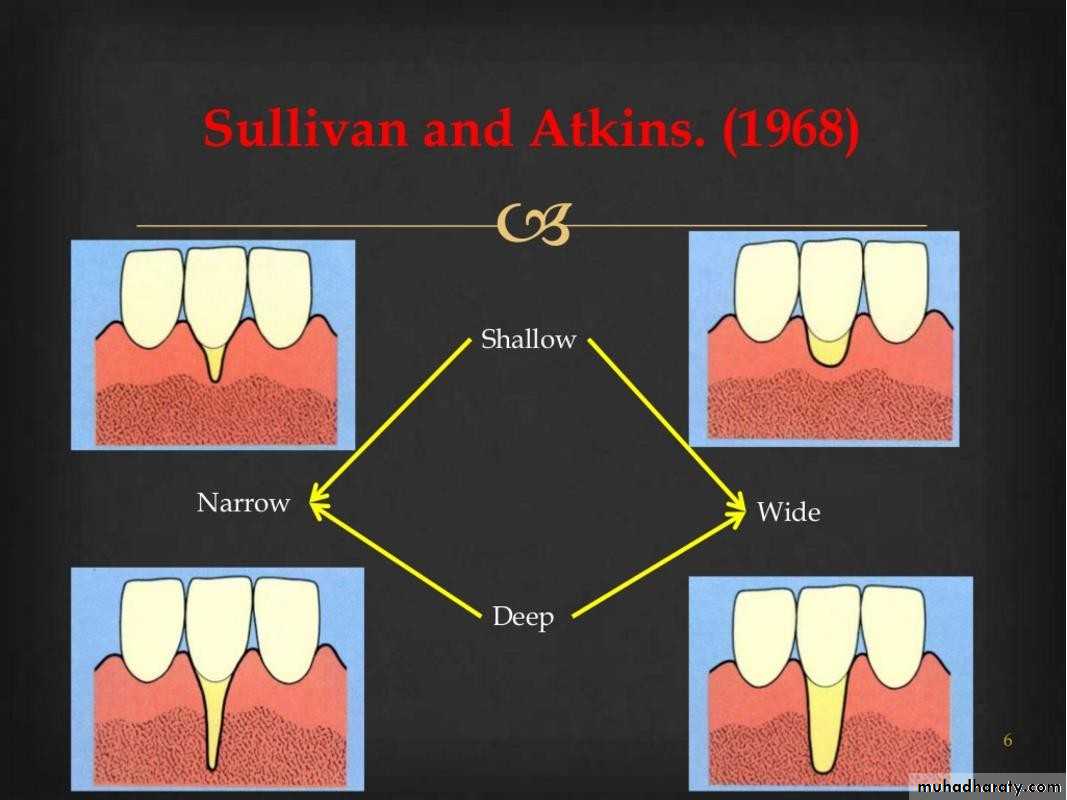
• Mucogingival Assessment• Includes:
• Marginal tissue recession.
• Inadequate attached gingiva.
• High frenum.
• Periodontal Examination
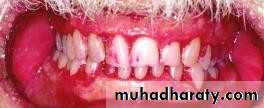
• Muccogingival Assessment• Mucogingival problem: Mrginal tissue recession high frenum
• inadequate attached gingiva.
• Periodontal Examination
• Muccogingival Assessment
• Marginal tissue recession and lack of keratinized gingiva on Mandibular anterior teeth.
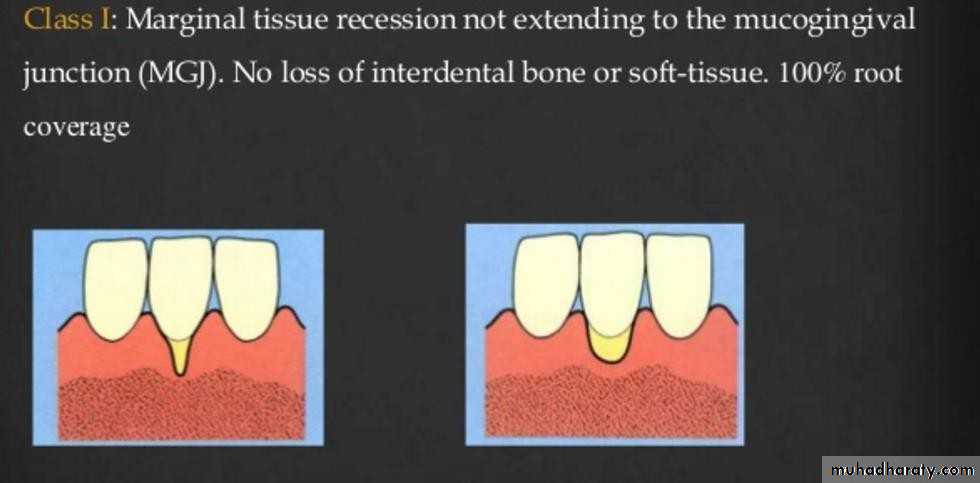
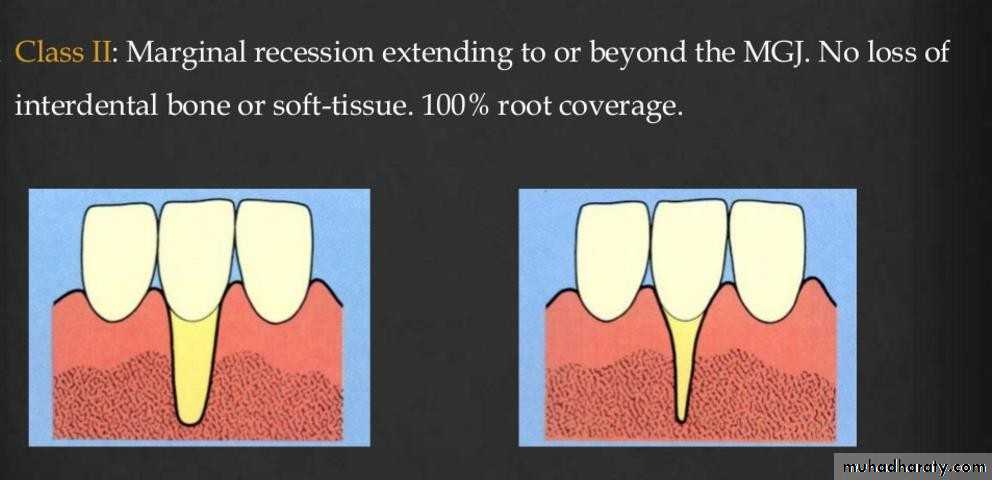
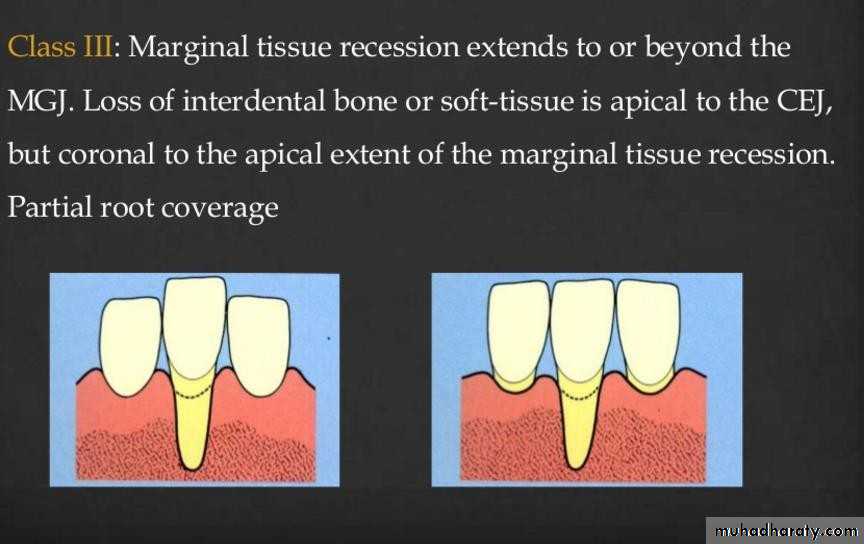
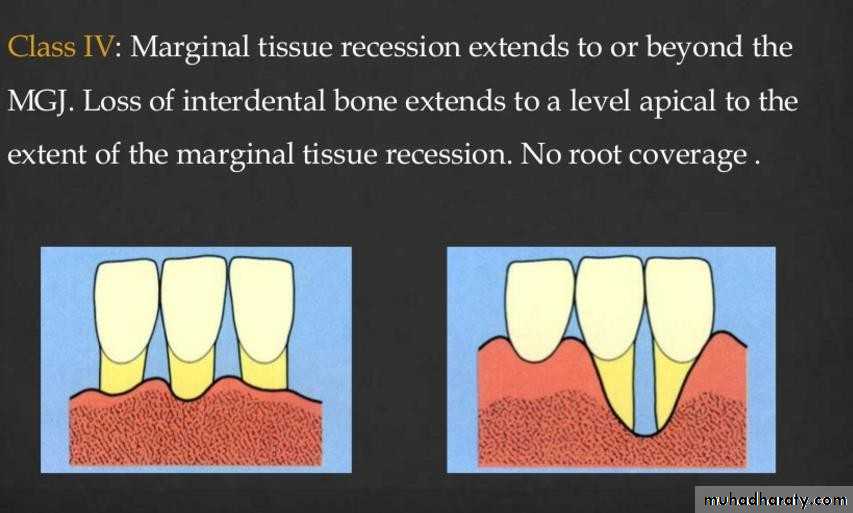
• Miller’s Classification of
Marginal Tissue Recession• Periodontal Examination
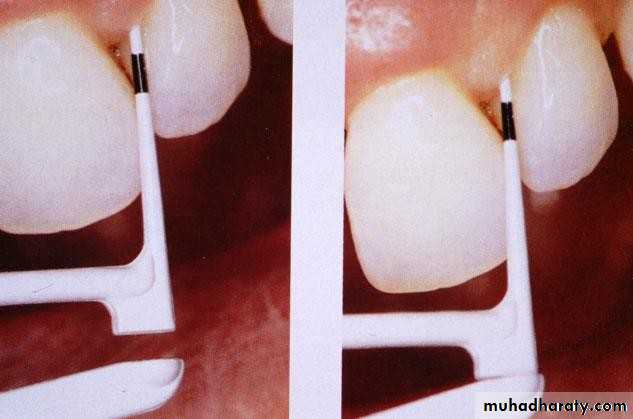
• Muccogingival Assessment• Measuring the width of Attached gingiva
• Periodontal Examination• Muccogingival Assessment
• Site with inadequate Attached gingiva (arrow)
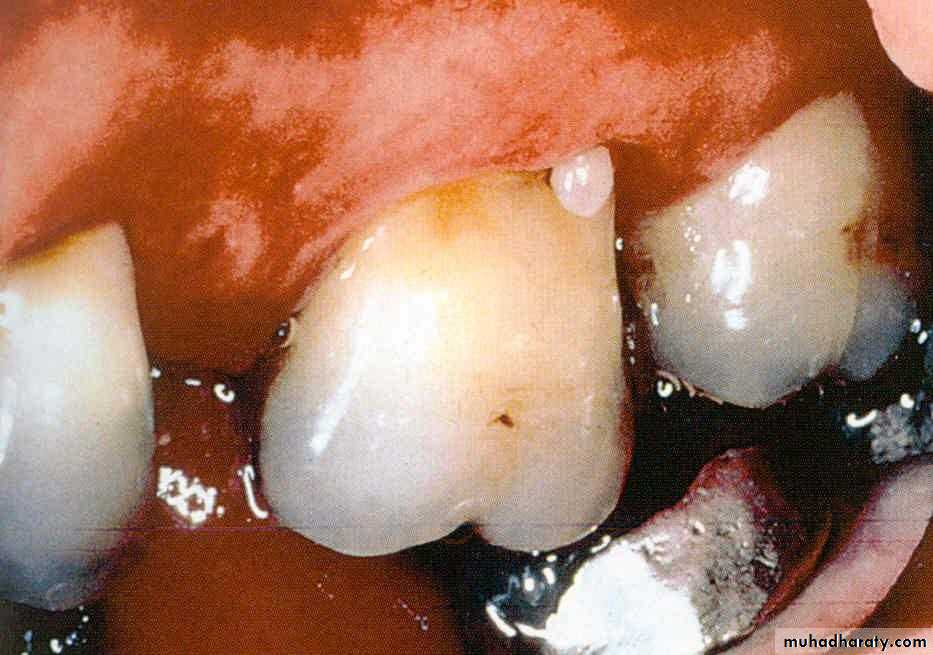
• Periodontal Examination• Muccogingival Assessment
• Multiple frenum associated With:
• Inadequate attached gingiva.
• Gingival recession.
• Inadequate oral hygiene
• Periodontal Examination
• Mucogingival Assessment• High frenum
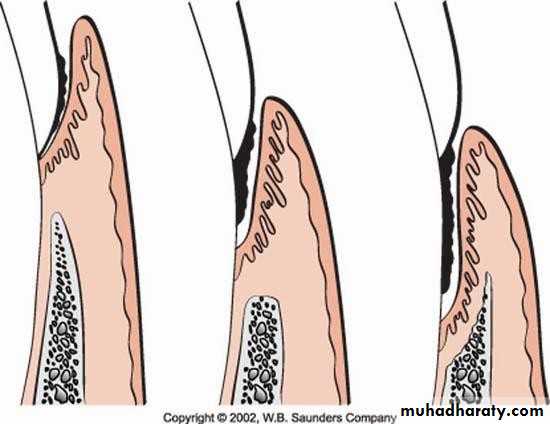
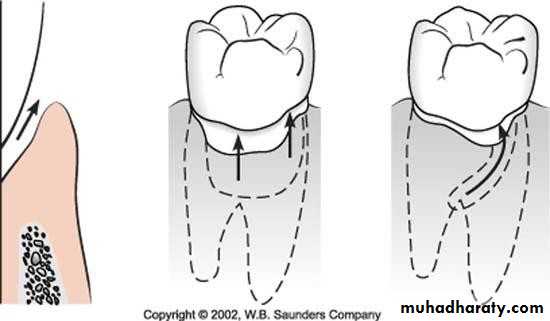
• Periodontal Examination Occlusal Trauma• An injury to the periodontal ligament and alveolar bone as a result of excessive forces.
• types of occlusal trauma:
• Primary
• Secondary
• Periodontal Examination Occlusal Trauma
• Primary occlusal trauma results from excessive occlusal forces applied to a tooth with normal support. Note that the center of rotation is near the middle of the root.
• Periodontal Examination Occlusal Trauma
• Secondary occlusal trauma: results from excessive/normal occlusal forces applied to a tooth with reduced periodontium..• Periodontal Examination Occlusal Trauma
• Clinical indicators of occlusal trauma:
• Mobility (progressive(• Fremitus
• Premature occlusal contacts.
• Wear facets in presence of other clinical indicators.
• Tooth migration.
• Fractured tooth
• Thermal sensitivity.
• Periodontal Examination Occlusal Trauma
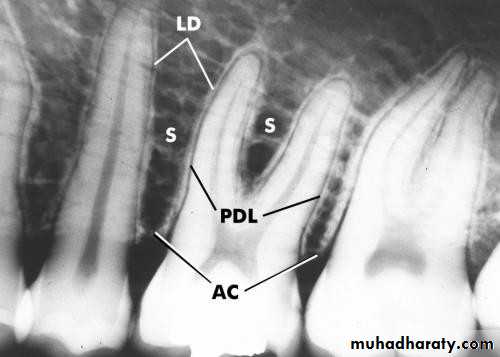
• Radiographic indicators of occlusal trauma :
• Widened PDL.
• Bone loss.• Root resorption.
• Periodontal Examination Radiographic Assessment
• Periodontitis
• Healthy Periodontium
• Periodontal Examination• Radiographic Assessment
• Bone Loss• Horizontal Vertical
• Endodontic involvement Root deposits
• Root anatomy Root length
• Periodontal Examination
• Radiographic Assessment• Periodontal Examination
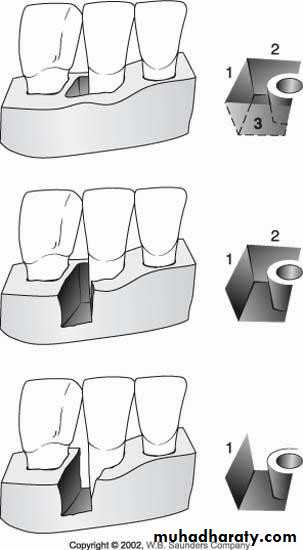
• Radiographic Assessment• three-wall vertical defect
• two-wall vertical defect
• one-wall vertical defect
• Periodontal Examination
• Plaque Control Record• Gives the dentist, hygienist a simple
• method of recording plaque on individual tooth surface
• Establishes an oral hygiene a baseline.
• Patient education.
• Requires a short time to perform.
• Periodontal Examination Plaque Control Record
• Disclosing tablets
• Disclosed plaque• Periodontal Examination
• Plaque Control Record
• Factors that hinder patient’s plaque control:
• Calculus.• Poor restoration margins. Over-contoured restorations. Removable partial appliances.
• Plaque Index (PI) (Silness & Loe)
• Concerns thickness of plaque along gingival margin.
• Used in epidemiological studies.along with Gingival index.• Time consuming.
• Less useful for routine charting.
• Plaque Index (Sliness &Loe)
• Scores• Criteria
• 0
• No plaque
• 1
• A film of plaque adhering to the free gingival margin and adjacent area of the tooth. The plaque may be seen in situ only after application of disclosing solution or by using the probe on the tooth surface.
• 2
• Moderate accumulation of soft deposit s within the gingival pocket, or the
• tooth and gingival margin which can be seen with the naked eye.
• 3
• Abundance of soft matter within the gingival pocket and/or on the tooth and gingival margin.
• Thanks