Fifth Stage
Internal Medicine
Dr. Dhyiaa – Lecture 5
1
ACUTE RENAL FAILURE
DEFINITION:
It is abrupt decrease in renal function which developed over a period of days or weeks
and usually accompanied by reduction in urine volume and retention of nitrogenous
waste (( eg. Blood urea and createnin ))
CAUSES:
1. Pre renal:
a. Absolute decrease in effective blood volume eg. Hemorrhage, burns, diarrhea,
vomiting.
b. Relative decrease in effective blood volume eg. Congestive heart failure, sepsis,
anaphylaxis
c. Arterial occlusion
2. Renal:
a. Acute tubular necrosis (( ATN ))
1.
Ischemic insult
( prolonged hypotension )
2.
Nephrotoxic insult
which is either:
▪
Exogenous nephrotoxins
eg. Aminoglycosides, amphotericin B, contrast
agents.
▪
Endogenous substances
: Haemoglobuline, myoglobulin, uric acid,
bacterial toxins.
b. Acute interstitial nephritis
c. Acute glomerulonephritis
3. Post renal
a. Obstructive uropathy
b. Bladder neck obstruction.
Clinical presentations & evaluation
Reversible pre renal ARF:
•
Marked hypotension and signs of poor peripheral perfusion
•
Postural hypotension
(fall > 20/10 mmHg )
•
Evidence of the underlying cause but some time concealed blood loss can occur
eg GI-bleeding, pelvic fracture
•
Metabolic acidosis and hyperkalaemia are often present
•
Significant oliguria with concentrated urine
•
Elevated blood urea level with no or minimal increase in serum creatinine.
(B.urea/S.creatinine ratio
> 40
).
2
•
Low urine sodium
< 20 meq/L.
Management:
1. Establish and correct the underlying cause of ARF.
2. If the patient is hypovolaemic, restore the blood volume as rapidly as possible with
blood, plasma or normal saline.
3. Vital signs monitoring and central venous pressure monitoring.
4. Correct metabolic acidosis by:
a. Restoration of blood volume.
b. Isotonic Sodium bicarbonate may be used.
* If the treatment given sufficiently early, renal function will improve rapidly but
in some cases the treatment is ineffective and renal failure become established.
Established ARF:
CLINICAL FEATURES:
1. Features of the
underlying
cause
eg. Trauma, sepsis
2.
Alteration in urine volume
usually started as oliguric phase followed by polyuric
phase which carry better prognosis and may indicate regeneration and recovery
from ATN.
3. GIT symptoms
((early uremic symptoms)) include: anorexia, nausea, vomiting and
hiccoughs.
4. Neurological manifestations:
drowsiness,apathy,confusion, fit, muscle twitching and
comma.
5.Cardiovascular features:
: pericarditis and arrhythmias which may be due to uremia
itself or as a resut of electrolyte disturbances.
6. Electrolytes and metabolic abnormalities:
a. Hyperkalemia:
particularly with massive tissue break down or haemolysis, ECG
changes ((tinted T-wave, absence of P-wave, wide QRS complex and Sine wave)),
elevated serum potassium.
b. Metabolic acidosis.
c. Dilutional hyponatermia.
d.Hypocalcaemia& Hyperphosphatemia.
7.Increased
respiratory rate
due to acidosis, pulmonary oedema or respiratory
infection.
8.
Anaemia
may be present due to excessive blood loss or it may indicate acute
exacerbation on CRF.
9.Severe infection
may complicate ARF due to decreased immunity.
10. Volume overload:
bilateral leg oedema,
3
Pulmonary oedema,
Pericardial effusion.
Clinical approach to the diagnosis of ARF:
The clinical evaluation of ARF is achieved by answering the following
five questions
:
Is it ARF or an
acute on chronic
renal failure?
Is there renal tract
obstruction
?
Is there
reduction in effective ECF
volume?
Has there been a major
vascular occlusion
?
Is there
parenchymal renal disease
other than ATN?
A complete history, physical examination and chart review, as well as a careful
urinalysis, a renal ultrasound, and a few routine blood tests should be performed in all
patients with ARF .
This approach will reveal the likely cause of ARF in most patients. In a few carefully
selected patient ,additional ,selected special investigations-imaging, serology, renal
biopsy-may be necessary to establish the cause of renal dysfunction.
History
The diagnosis of prerenal failure is often facilitated by careful evaluation of the patient
fluid balance during the few days preceding the onset of ARF.
H/O vomiting or diarrhea
provides useful clues to the source of loss of ECF volume.
Symptoms of dry
cough,orthopnea, or ankle swelling
may indicate the possibility of
early volume overload.
Frequency, urgency, and hesitancy
are important symptoms in patient with bladder
dysfunction or bladder neck obstruction.
H/O ingestion of a nephrotoxic drugs
Systemic symptoms
such as fever, malaise or fatigue, and joint pain or skin rash raise
the possibility of ARF caused by acute GN associated with SBE, vasculitis or connective
tissue disease like SLE
H/O previous renal disease or hypertension
may point to pre-existing chronic renal
insufficiency .
Chart review
Since most ARF occurs in patients in hospital,the hospital record represent an
extremely an important source of information regarding the possible cause. A
4
chart review should be considered as an extension of the
history
, daily record of
vital signs
, changes in body
weight
and records of
fluid intake and out put.
The
record of all
drugs taken by the patient
must be examined for potentially
nephrotoxic drugs.
PHYSICAL EXAMINATION
*
Loss of skin turgor and postural hypotension when fluid loss exceed
5-10% of ECF volume.
*
Supine hypotension when the fluid loss exceed 20% of ECF volume.
*
Raised JVP ,pedal edema and pulmonary crackles indicate cardiac failure.
Skin:
* Jaundice
and other evidence of acute or chronic liver disease
*Maculopapular
skin rash may indicate drug induced AIN or acute GN.
*Malar rash
or photosensitivity in SLE
*Livedo reticularis
associated with cryoglobulinemia or atheroembolic disease
*Palpable purpura
commonly caused by cutaneous vasculitis or atheroembolic disease
*Nonpalpable purpura
may suggests the presence of thrombocytopenia associated with
SLE or thrombotic microangiopathy.,
Eye examination
*Jaundice, hypertensive retinopathy, Roth spots (endocarditis)or cholesterol emboli
(atheroembolic disease)
Abdominal examination:
*Ascites
may indicate chronic liver disease or congestive cardiac failure
*Bruits
over the anterior abdomen or confirmed to the renal angles
*
Any evidence of bladder neck obstruction
*
Rectal or pelvic examination
*
The presence of large postvoid residual (more than 200-300 ml) is strongly suggestive
of functionally significant urinary retention.
Urine volume
Patient with prerenal azotemia almost always have oliguria, but non oligureic ARF
seen in :
1. diabetes insipidus
2. sodium wasting disease such as adrenal insufficiency
3. hyperglycemia
5
4. malnutrition
5. chroniclly ill patient
6. urinary tract obstruction ( unilateral or partial )
7. contrast induced ARF
8. aminoglycosid induced ARF
*Anuria is unusual in patient with ATN but it is more common with rapidly progressive
GN, acute interstitial nephritis or vascular catastrophes such as renal artery embolism
or renal vein thrombosis .
If patient thought to have ATN have persistent anuria lasting more than
24 -48
hours,
the other causes of ARF must be reconsidered.
SERUM CHEMISTRY
Blood urea nitrogen
*
The clearance of urea is always less than the GFR. This is because of the back
diffusion of urea which is inversely related to the rate of urine flow and is
enhanced by vasopressin.
*
BUN rises more rapidly than the creatinine in patient with Prerenal failure
The ratio BUN : Cr is normally
15:1
(mg:mg) (
60:1
mmol:mmol)
High ratio > 20:1 caused by:
1. Prerenal failure
2. GI bleeding
3. increased protein intake
4. catabolic state
5. infusion of amino acids
6. corticosteroid therapy
7. tetracycllines
Low ratio < 5-10 :1 caused by:
1. severe liver disease
2. malnutrition
3. rhabdomyolysis
4. cimetidine
5. trimethoprim
6. cephalosporins
SERUM CREATININE
*As renal function deteriorates ,the Cr becomes progressively less reliable as an index
of GFR..
6
*BUN rarely exceeds 30mg/dl.and serum Cr > 2 mg/dl.unless there is concurrent
underlying chronic renal insufficiency.
OTHER SERUM CHEMISTRY:
*They are usually unhelpful in the diagnostic process.
Hyperkalemia, hyperuricemia,
hypocalcemia and hyperphosphatemia
are all common in ARF of any cause also
they are
not
useful in distinguishing ARF from CRF
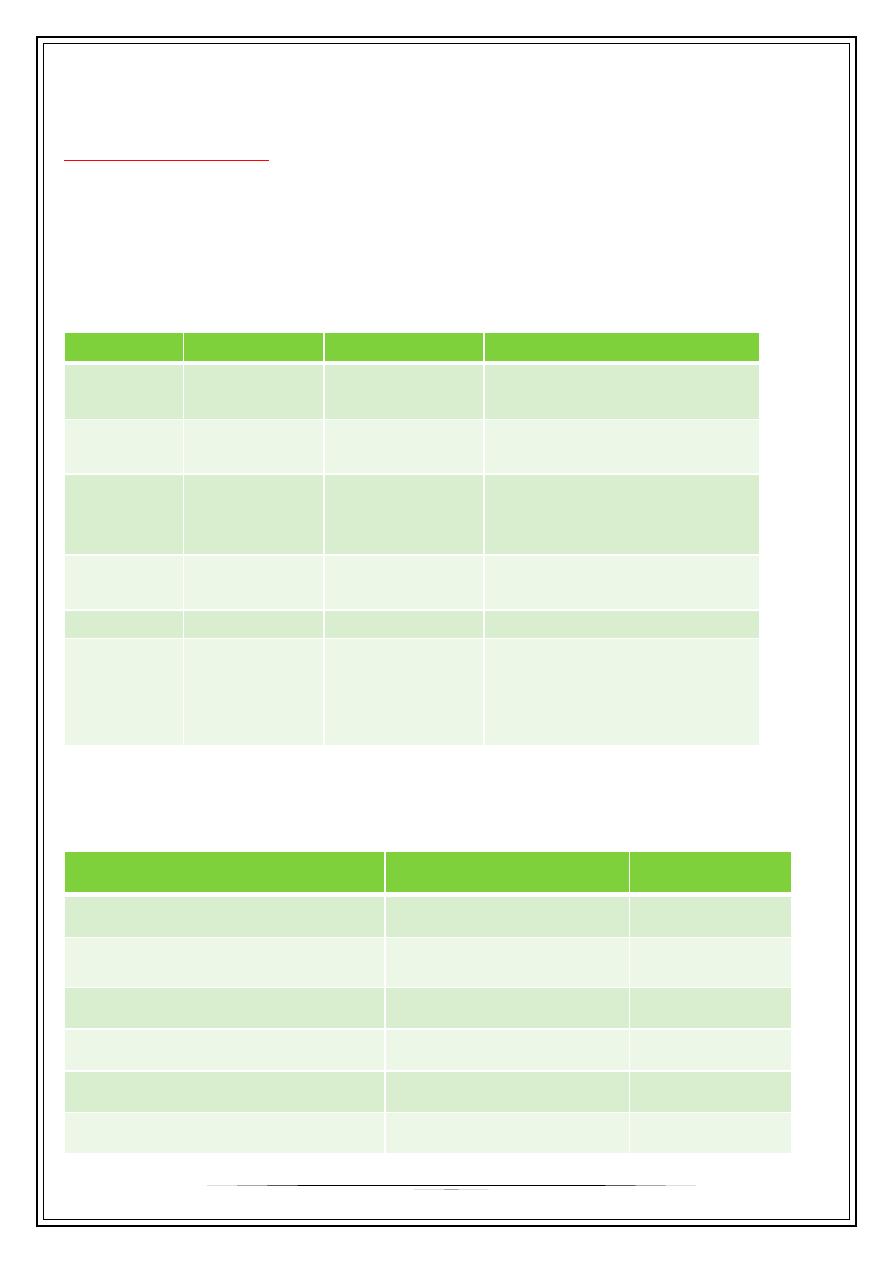
URINALYSIS:
Microscopy
Hematuria
protienuria
condition
normal
-
-
Prerenal
azotemia
normal
-
-
Vascular
occlusion
Dysmorphic RBC
RBC cast
Granular cast
+++
+++
GN
Pyuria,WBC cast
eosinophiluria
+
++
AIN
Normal
+
-
/
+
HUS/TTP
Muddy brown granular
cast,epithelial cast,
sometime NONE in
nonoliguric ATN
-
-
ِATN
GUE may shows evidence of underlying renal pathology eg. GN, Interstitial nephritis or
evidence of underlying cause eg DM, Multiple myeloma
URINE CHEMISTRY
ATN
Prerenal
Index
>40
<20
Urine sodium
<20
>40
U. cr / P.cr. (mg/dl)
<300-350
>500
U.osm
<1.1
>1.5
U./ P. osmolality
<1.015
>1.018
Specific gravity
<3
>8
U. / P. urea
7
.>2
<1
FeNa=U.Na/Ucr×Pcr/PNa×100
>1
<1
RFI=U.Na/ (U.cr/P.cr)
Hematological indices
-the
hematocrit is not useful
discriminate between ARF and CRF.
-
High WBC
count may point to systemic infection, lymphoma and leukemia
-
Eosinophelia
may suggest a drug induced ATN or atheroembolic disease
-
Thrombocytopenia
suggest HUS,TTP, SLE, myeloma, sepsis, and DIC.
RENAL ULTRASOUND
- It is a
key investigation
for the diagnosis of obstruction or CRF.
- It is
not a reliable method
for identifying the anatomical site of obstruction
-
Even
if the kidneys are reduced in size , the possibility of Prerenal ARF or ATN
superimposed on CRF must always be considered.
SEROLOGY
- ANA, ANCA, anti GBM, RF, C3 & complement levels
- They are useful for vascullitic or glomerular process
- Hepatitis and HIV serology (especially if dialysis is indicated)
: may shows Pulmonary oedema, pericardial effusion
CXR
: evidence of pericarditis, arrhythmia, Hyperkalemia
ECG
CT scan
It can delineate the level of obstruction and define retroperitoneal inflammation or
retroperitoneal malignant mass
RENAL ANGIOGRAPHY:
*It is
indicated
when renal artery occlusion is suspected
or
as a useful investigation in
diagnosing classical PAN
*
Renal venography
may be indicated to confirm the diagnosis of renal vein
thrombosis.
RENAL BIOPSY
*
It is unnecessary in ARF but can be useful in patient in whom parenchymal renal
disease other than ATN is suspected.( AIN or RPGN)
8
*
Renal biopsy also indicated in presence of systemic illness manifestations or for
unexplained ARF. or for unexpected cause for ARF.
After 4-6 weeks , a renal biopsy may be considered In patient with ATN who do not
recover renal function, renal biopsy indicated to determine the cause of ARF and clarify
the prognosis.
Treatment of ARF
1. Fluid balance
(input and output chart) with central venous pressure monitoring,
daily body weight and treatment of fluid over load with diuretics.
2.
Emergency
treatment of Hyperkalemia
with ca-gluconate
3.
Correction of acidosis
by giving Sodium bicarbonate.
4.
Bolus dose of
loops diuretics
to initiate dieresis but if it fail, No farther diuretics
5. Restriction of salt intake &
protein intake into
40-60 gm/day
.
6. vigorous treatment of infection
. should be given.
7. Drugs
that are nephrotoxic should be omitted or dose adjustment.
8. Dialysis
( When ever indicated should not be delayed ) Which is
indicated
in:
a. Severe Hyperkalemia
b. Severe acidosis
not corrected by sodium bicarbonate.
c. Fluid overload
not corrected by diuretics.
d. Blood urea > 200mg/dL
. Or rapidly rising blood urea
more than 40mg/dL
. over 24hr.
e. Uremic encephalopathy
f. uremic pericarditis
g. severe uremic symptoms
not controlled by medical treatment.
Outcome & Prognosis
-The oliguric phase last 1-2 weeks.
- Those with oliguria more than 3 weeks carry poor prognosis.
- Uncomplicated ARF due to simple hemorrhage or drug carry better prognosis and low
mortality.
*ARF associated with serious infection and multiple organ failure carry poor prognosis
with 50-70% mortality
* Outcome is usually determined by the severity of the underlying disorder other
complication rather than by renal failure itself..
Thank you,,,
