1
Orthopedic Surgery
Dr.Khalid Ali zayer
5
th
Stage
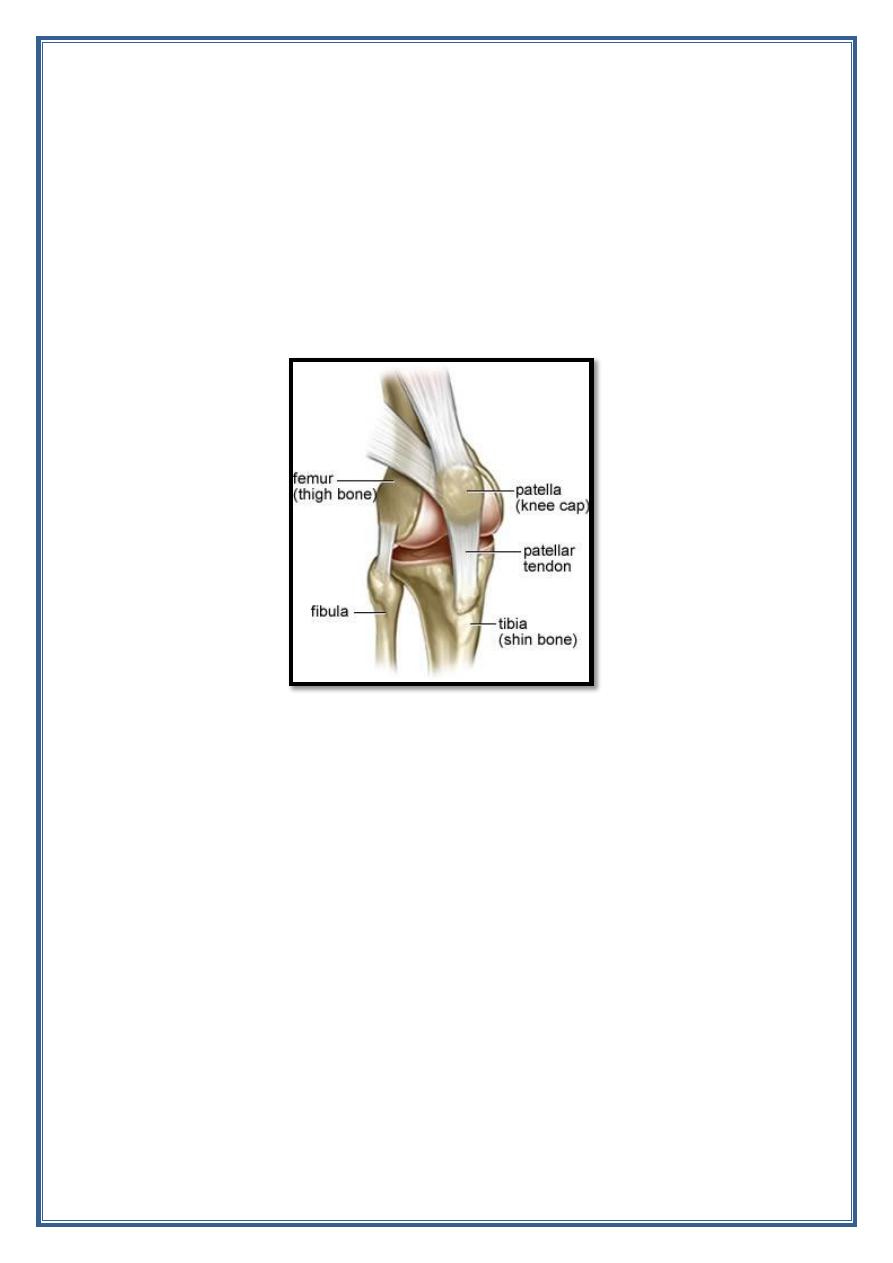
Knee joint
Knee dislocation
Traumatic knee dislocation are uncommon but serious that have variable
prognosis. It is describe complete disruption of the integrity of the tibio-
femoral articulation.
2
Incidence:
0.02% of orthopedic injury.
4 :1 male to female ratio.
Approximately 50% self reduce and misdiagnose.
Mechanism of injury:
o 50 % of the injury due to high energy trauma ( fall from height ,
RTA, dash board injury resulting in axial load to flexed knee) .
o 30 % low energy trauma (sport injury).
o 20% are from simple falls.
3
Classification:
Based on the direction of displacement of tibia:
1. Anterior ( 30-50%) most common due to hyper extension injury.
2. Posterior (30-40%) due to axial load to flexed knee ( dash board
injury).
3. Lateral 13 % due to varus or valgus force and associated with
highest rate of peronial nerve injury.
4. Medial 3 % due to varus or valgus force.
Presentation :
Symptoms:
History of trauma and deformity of the knee.
Knee pain and instability.
Physical examination:
Swelling, effusion , abrasion, echymosis.
Compartment syndrome is also a risk.
Vascular examination.
Neurological examination.
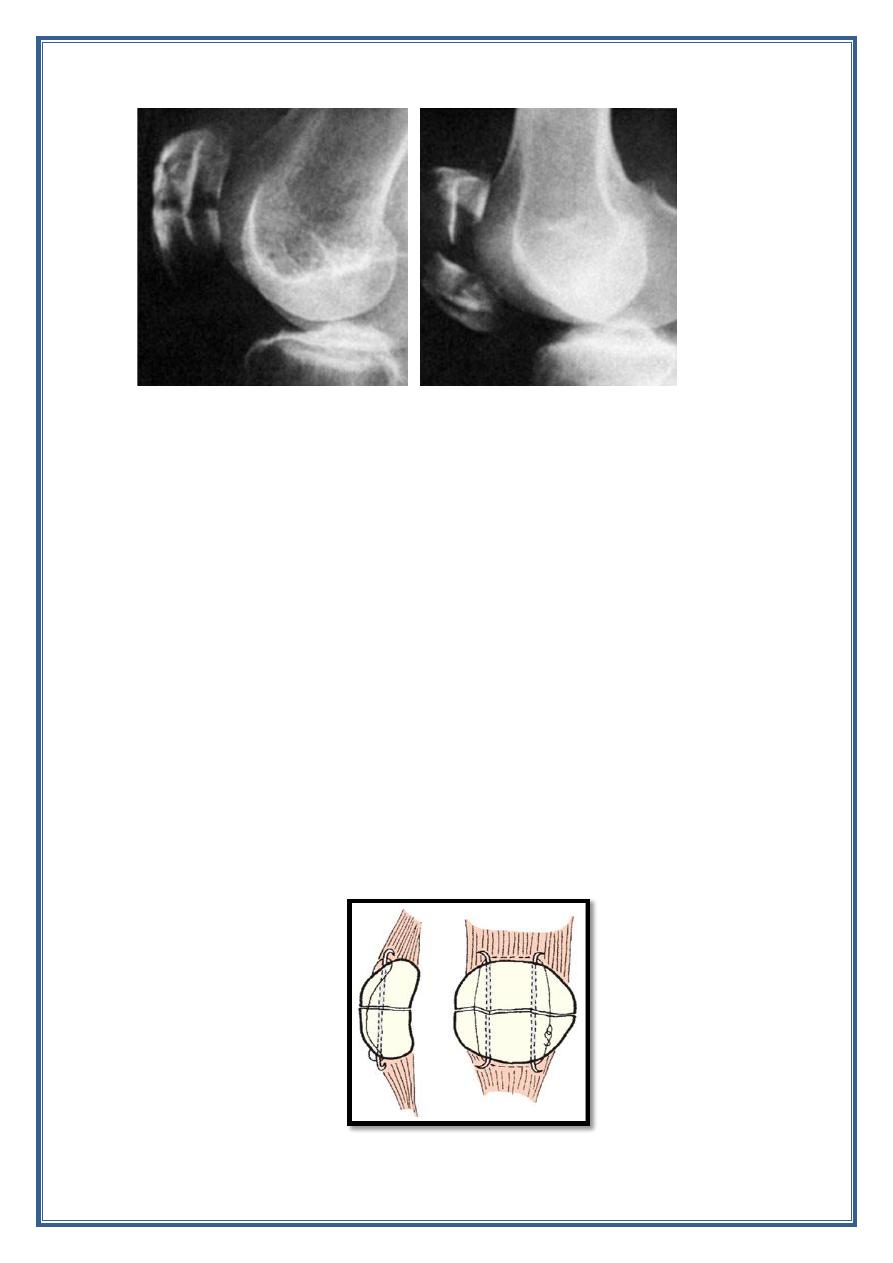
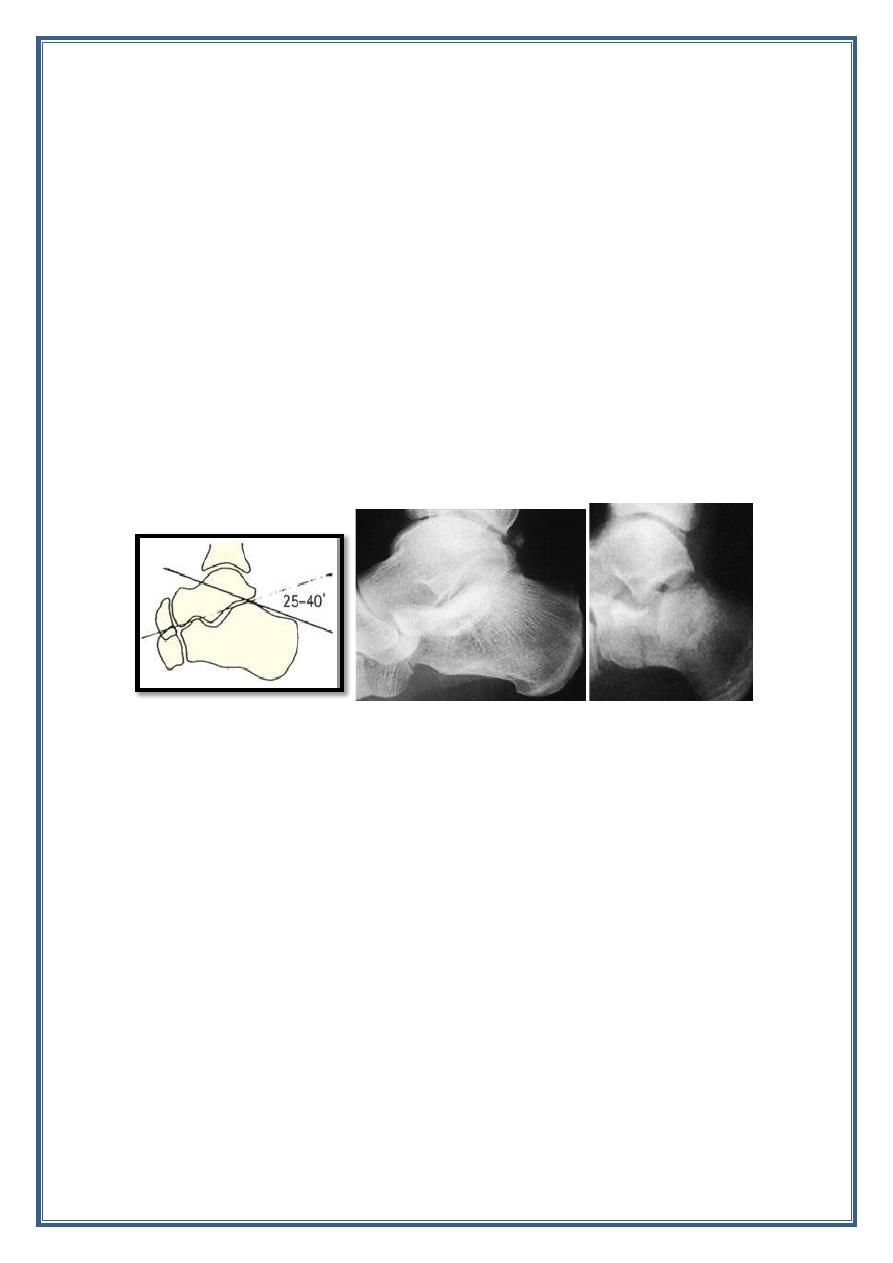
Imaging:
Radiographes:
1. Pre reduction AP and lateral view of the knee.
2. post reduction AP and lateral view of the knee.
3. 45 ̊ oblique view if fracture suspected.
Treatment:
1. Non operative treatment: emergent close reduction with
immobilization as definitive treatment indicated when successful
close reduction without vascular compromised.
2. Operative treatment:
Indication:
a. Irreducible knee dislocation.
b. Posterior lateral dislocation.
c. Open fracture dislocation.
d. Obesity patient ( may be difficult to obtain close reduction).
e. Vascular injury.
4
Complication:
Early:
1. Arterial damage.
2. Common peronial nerve injury.
3. Associated fracture.
4. Soft tissue injury.
Late:
1. Joint instability.
2. Joint stiffness.
Patella fracture:
- The patella is a sesamoid bone in continuity with the quadriceps
tendon and the patellar ligament.
-
The mechanical function of the patella is to hold the entire extensor
‘strap’ away from the centre of rotation of the knee, thereby
lengthening the anterior lever arm and increasing the efficiency of
the quadriceps.
-
Incidenc of patellar fracture account for 1% of all skeletal injury
.
- Male to female ratio 2:1.
- Most fractures occur in 20-50 years old.
Mechanism of the injury:
1. Direct injury occur from a fall onto the knee or blow against the
dish board of the car cause either undisplaced crack or comminuted
fracture.
2. Indirect injury occur from rapid knee flexion against contracted
quadriceps muscle cause transverse fracture with gap between
fragments.
Associated injuries:
1. Femur neck fracture.
2. Posterior wall acetabular fracture.
3. Knee dislocation.
Classification:
It can be classified as:
1. Transverse.
2. Longitudinal.
3. Comminuted.
4. Marginal.
Any of these fractures may be either undisplaced or displaced.
5
Presentation:
1. History of the trauma.
2. The knee becomes swollen and painful.
3. Abrasion or bruising over the front of the joint.
4. The patella is tendor and sometime gap can be felt.
5. Haemarthrosis.
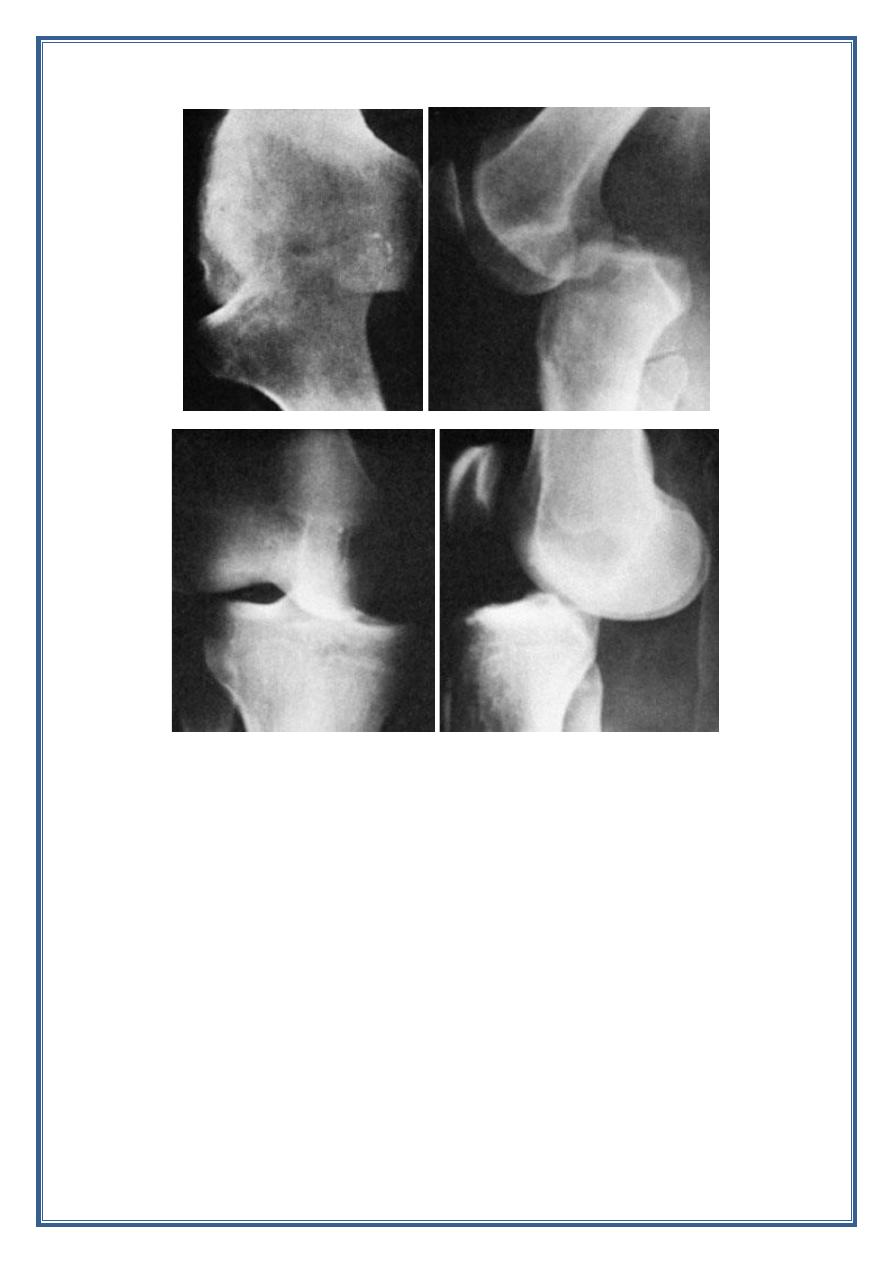
Imaging:
Radiographic : AP, and lateral view.
Treatment:
- Non operative treatment:
Knee immobilized in extension with brace or cylinder cast.
Indication:
1. Intact extensor mechanism( patient able to perform straight leg
raise).
2. Non displaced or minimally displaced fracture.
3. Vertical fracture pattern.
- Operative treatment:
With tension band fixation.
6
Indication:
1. Extensor mechanism failure (patient unable to perform straight
leg raise).
2. Open fracture.
3. Displaced patellar fracture > 3 mm.
- Partial pattellectomy indicated in comminuted superior or inferior
pole fracture when ORIF is not possible.
- Total pattellectomy
indicated
for
severe
and
extensive
comminution not amenable to salvage.
Tibial plateau fractures
Periarticular injuries of the proximal tibia frequently associated with soft
tissue injuries.
- males in 40s (high-energy trauma)
- females in 70s (falls)
-lateral > bicondylar > medial.
Mechanism of injuries:
- Varus/valgus load with or without axial load.
- High energy associated with soft tissue injuries.
- Low energy associated usually with insufficiency fractures.
Associated conditions:
1. Meniscal tears
- Lateral meniscal tear more common than medial and associated
with Schatzker 2 fracture.
- Medial meniscal tear most commonly associated with Schatzker 4
fracture.
2. ACL more common in type 4 and 6 fractures (25%)
3. compartment syndrome commonly associated with Schatzker 4
fracture-dislocaion.
7
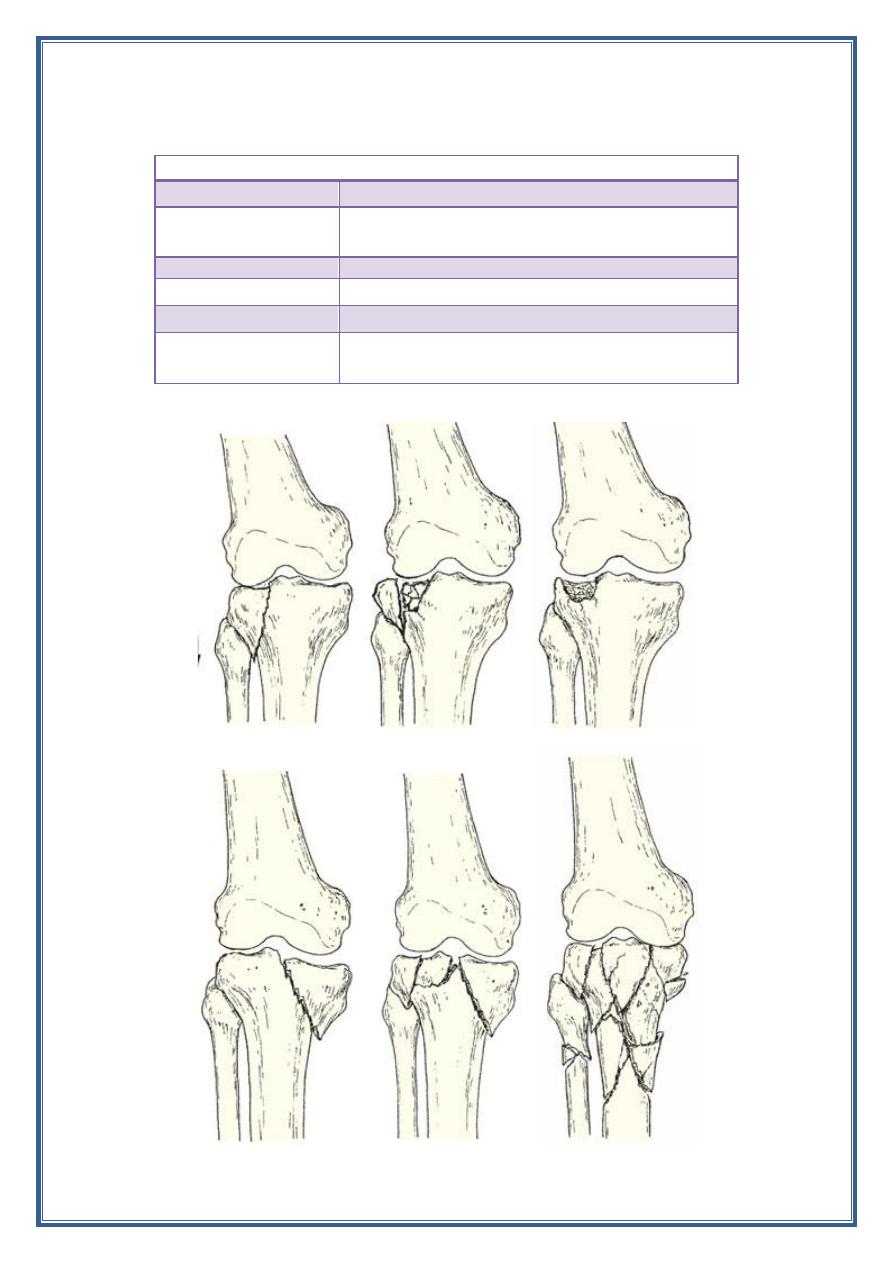
Classification
Schatzker classification
Type 1
A vertical split of the lateral condyle
Type 2
A vertical split of the lateral condyle combined with
depression fracture
Type 3
Lateral pure depression fracture of the articular surface
Type 4
Fracture of the medial condyle
Type 5
Fracture of both condyles
Type 6
Combined condylar and subcondylar fractures
8
Clinical features:
- Inspection :
Look circumferentially to roll out an open injury, swelling
,deformity ,and bruising.
- Palpation:
Varus/valgus stress test. Any laxity more than 10̊ indicated
instability.
Consider compartment syndrome when compartment are firm and
not compressable.
Neurovascular examination.
Imaging:
1. Radiographic
Recommended views:
AP.
Lateral.
Oblique: is help to determine amount of depression.
2. CT scan:
Important to identify articular depression and comminution.
3. MRI: useful to determine menesical and ligamentous pathology.
Treatment
The treatment of the tibial platue fracture either conservative or surgical
treatment depend on the type of fracture (Schatzker classification).
Type I fracture :
-undisplaced fracture can be treated conservatively by hinged cast brase
with weight bearing restriction.
-displaced fracture should be treated by open reduction and internal
fixation.
Type II fracture:
- Conservative treatment indicated if:
1. depression fracture slight (less than 5 mm) and the knee not unstable.
2. patient is old and frail or osteoporotic patient.
- Surgical treatment indicated if :
1. younger patient.
2. central depression more than (5 mm).
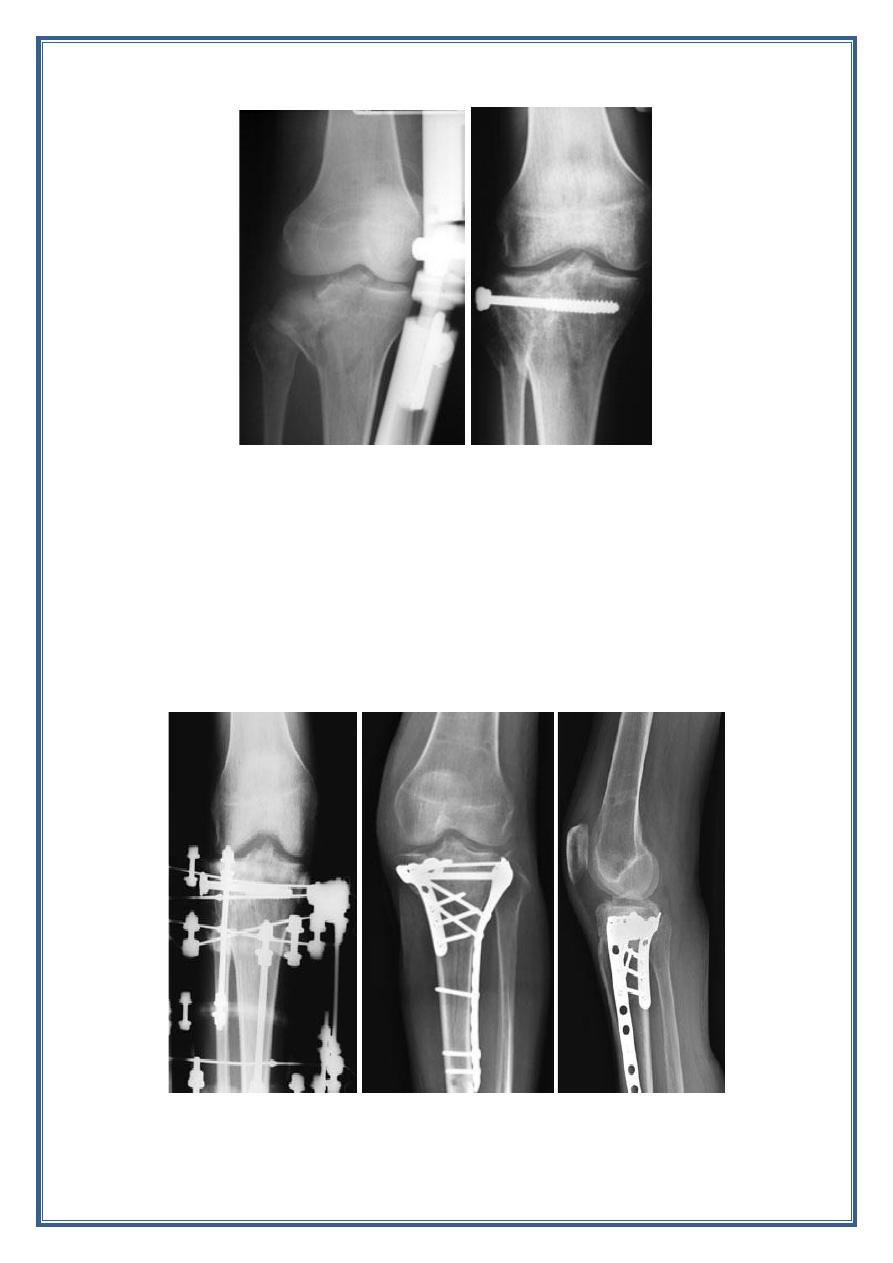
9
Type III and IV fracture:
The principle of the treatment are similar applying to type II fracture.
Type V and VI fractures:
These are severe injuries that carry the added risk of compartment
syndrome so the treatment at first by stabilization with splint , or external
fixation and waiting for the soft tissue condition to improve( 2-3 weeks)
then treated by open reduction and internal fixation.
10
Complications:
- Early: - compartment syndrome.
- Late:
Joint stiffness.
Deformity.
Osteoarthritis.
Tibia and fibula shaft fractures:
Most common long bone fracture because of its subcutaneous position
and more often sustains an open fracture( 23.5%) .
Mechanism of injury:
1. Indirect injury:
- Is usually low energy.
- Spiral or oblique fracture one of bone fragment may pierce the
skin from within.
2. Direct injury:
- Is usually high energy .
- Crush or splits the skin over the fracture.
- Most common cause motor cycle accident.
Tscherne's classification of skin lesion in closed fracture
Grade
skin lesion
Grade 0
No skin lesion
Grade 1
No skin laceration but contusion
Grade 2
Circumscribed degloving
Grade 3
Extensive, closed degloving
Grade 4
Necrosis from contusion
11
Gustilo’s classification of open fractures
Grade
wound
Soft tissue injury
Bone injury
I
< 1 cm long
minimal
Simple low-energy
fractures
II
>1 cm long
Moderate, some
muscle damage
Moderate comminution
IIIA
Usually >1 cm long
Severe deep
contusion;
+ compartment
syndrome
High-energy fracture
patterns; comminuted but
soft-tissue cover possible
IIIB
Usually >10 cm long
Severe loss of soft-
tissue cover
Requires soft-tissue
reconstruction for cover
IIIC
Usually >10 cm long
As IIIB, with need
for vascular repair
Requires soft-tissue
reconstruction for cover
Presentation
Symptoms
Pain, inability to bear weight, deformity.
Physical exam
Inspection and palpation
- Deformity / angulation / malrotation
- Contusions
- Open wounds
- Compartments
- Neurovascular exam.
Imaging
- full length AP and lateral views of affected tibia.
- AP , lateral and oblique views of ipsilateral knee and ankle.
Treatment
1- Non operative : closed reduction /cast immobilization.
-indication:
a. Closed low energy fracture with acceptable alignment.
< 5 ̊ varus – valgus angulation.
< 10̊ anterio / posterior angulation.
> 50 % cortical apposition.
< 1 cm shortening.
< 10̊ rotational malalignment.
b. Certain patients who may be non – ambulatory (paralyzed ).
c. Patient unfit for surgery.
12
2- Operative treatment:
-indication:
a. Unacceptable alignment with closed reduction and casting.
b. Soft tissue injury that will not tolerate casting.
c. Segmental fracture.
d. Comminuted fracture.
e. Ipsilateral limb injury(floating knee).
f. Polytrauma.
g. Bilateral tibial fracture.
h. Morbid obesity.
Type of the fixation:
1. Intramedullary nailing.
2. Plating and screw.
3. External fixation.
Treatment of open tibial fracture:
1. Antibiotic .
2. Irrigation.
3. Depredment.
4. Stabilization.
5. Promote soft tissue cover.
6. Rehabilitation.
Complication:
A. Early:
1. Vascular injury.
2. Compartment syndrome.
3. Infection.
B. Late:
1. Malunion.
2. Delayed union.
3. Nonunion.
4. Joint stiffness.
5. Osteoporosis.
6. Complex regional pain syndrome.
13
Ankle fractures:
Malleolar fractures of the ankle:
- Fractures and fracture dislocations of the ankle are Common.
- Ankle fractures are seen in skiers, footballers and climbers; an
older group includes women with postmenopausal osteoporosis.
Mechanism of injury:
1. The patient stumbles and falls. Usually the foot is anchored to the
ground while the body lunges forward.
2. The ankle is twisted and the talus tilts and/or rotates forcibly in the
mortise, causing a low-energy fracture of one or both malleoli.
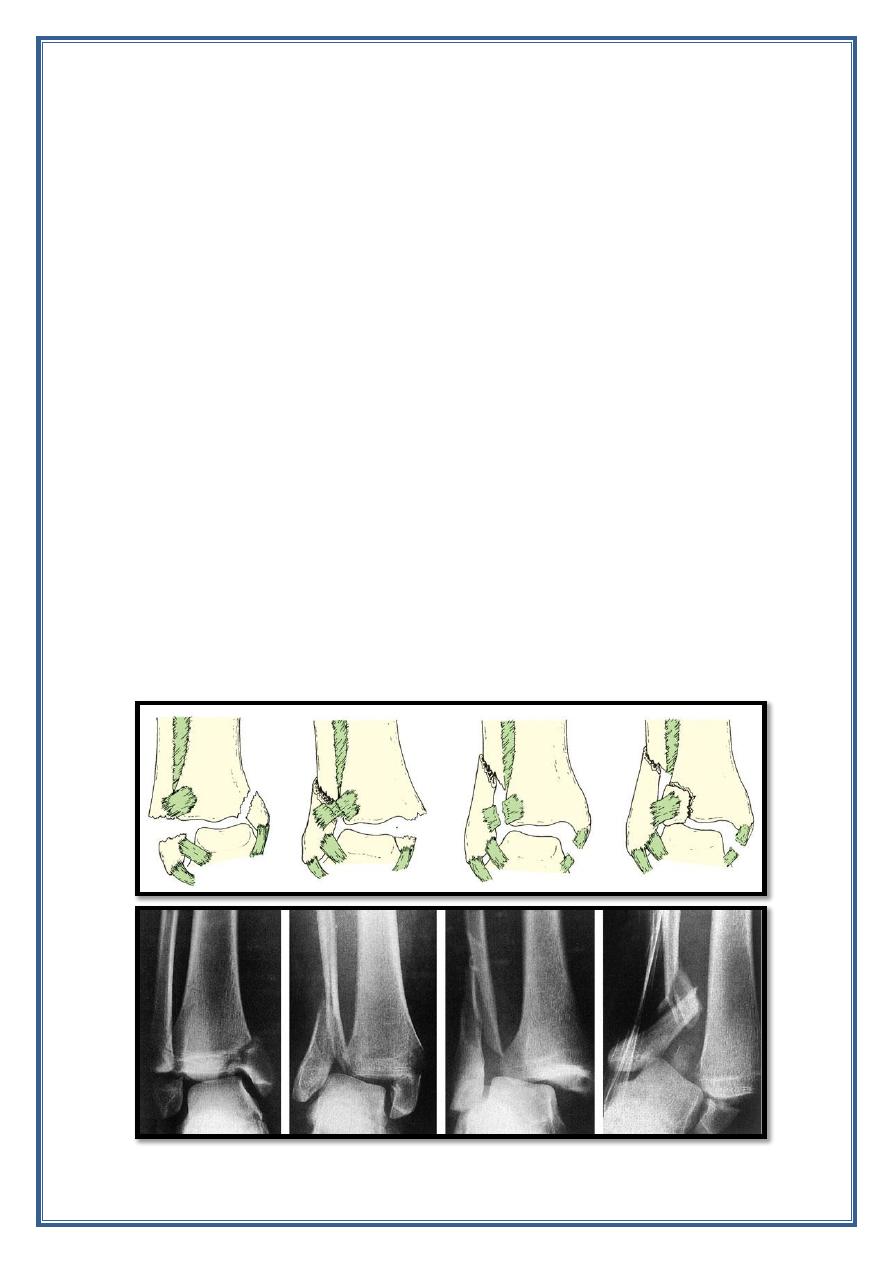
Classification of ankle fracture(Danis and Weber) :
Which focus on the fibular fracture.
Type A
: is a transverse fracture of the fibula below the tibiofibular
syndesmosis (adduction (or adduction and internal rotation) injury.
Type B
: is an oblique fracture of the and therefore better seen in
the lateral xray)at the level of the syndesmosis (an external rotation
injury).
Type C
: is a more severe injury, above the level of the
syndesmosis (severe abduction or a combination of abduction and
external rotation).
14
Clinical features:
1. history of a severe twisting injury.
2. intense pain and inability to stand on the leg.
3. The ankle is swollen and deformity may be obvious.
Imaging:
Recommendedal view
- AP.
- Lateral.
- 30 ̊ oblique view( Mortise view).
- Further X-ray may be needed to exclude proximal fibular
fracture.
Treatment:
- ankle fractures must be accurately reduced and held if later
mechanical dysfunction is to be prevented.
- In assessing the accuracy of reduction, four objectives must be
met:
1) the fibula must be restored to its full length
2) the talus must sit squarely in the mortise, with the talar and
tibial articular surfaces parallel.
3) the medial joint space must be restored to its normal width,
i.e. the same width as the tibio-talar space (about 4 mm).
4) oblique x-rays must show that there is no tibiofibular
diastasis.
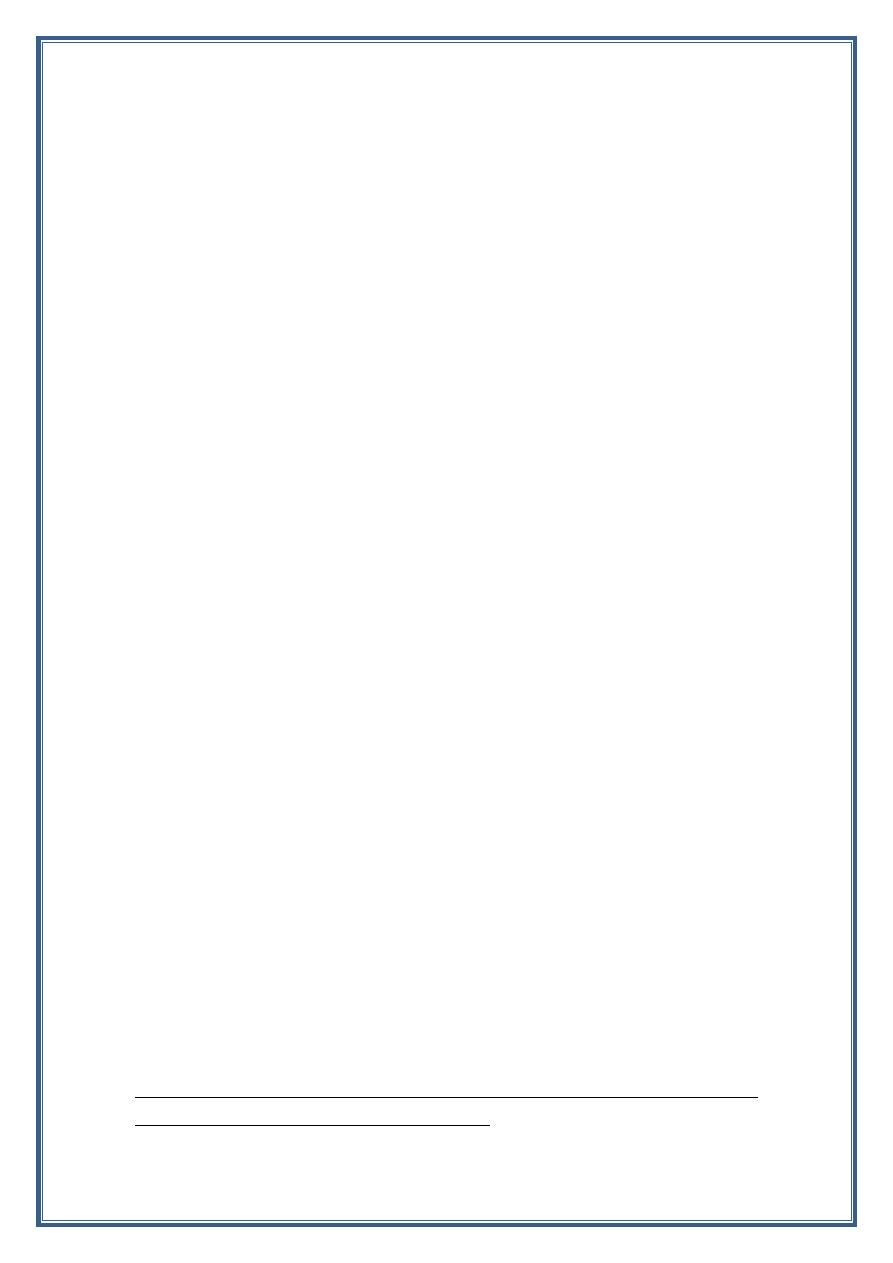
Type A:
- undisplaced fracture can be treated conservatively by firm
bandage or cast immobilization.
- Displaced fracture is often unstable so must be treated by open
reduction and internal fixation.
Type B:
- Undisplaced fracture if the x-ray show the syndesmosis is intact
(stable) can be treated by below knee cast imbolization with
ankle in neutral position.
- Undisplaced fracture and unstable must be treated by open
reduction and internal fixation.
Note: stability of the ankle joint depend on intact tibio-fibular ligament
and stability of the medial joint structure .
15
- Displaced fracture if close reduction success the cast is applied.
- Failure of close reduction so open reduction and internal
fixation.
Type C :
- are often accompanied by disruption of the medial joint
structures as well as the tibiofibular syndesmosis and
interosseous membrane. therefore, type C fractures are better
fixed from the outset.
Complication:
Early
1. vascular injury.
2. Wound breakdown and infection.
16
Late:
1. Incomplete reduction.
2. Nonunion.
3. Joint stiffness.
4. Complex regional pain syndrome.
5. Osteoarthritis.
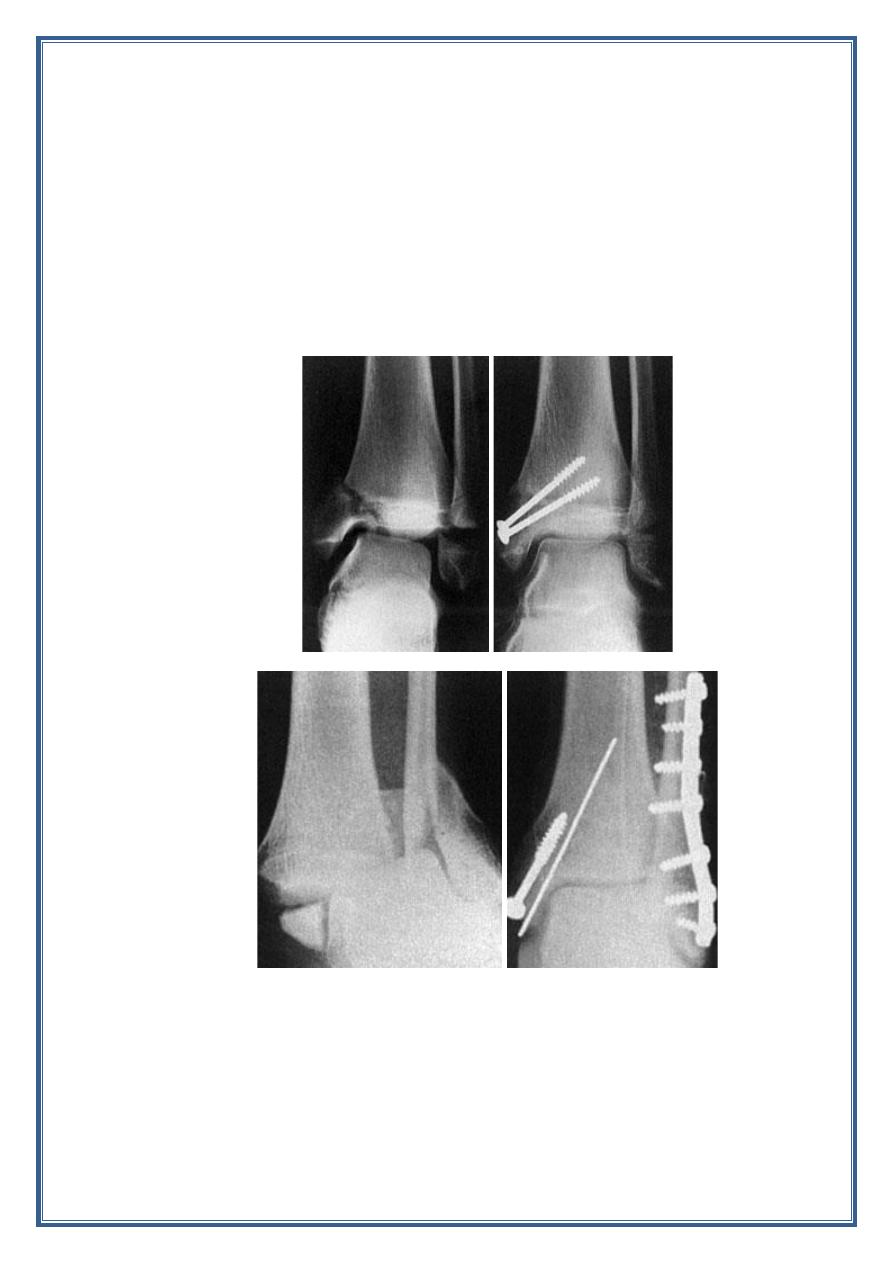
Pilon fractures:
Also known as Plafond fractures
Incidence:
account for < 10% of lower extremity injuries .
average patient age 35- 40 years.
More common in males than females.
Mechanism of the injury:
High energy axial load ( motor vehicle accident , fall from hight).
Articular impaction and comminution.
Metaphyseal bone comminution.
Soft tissue injury.
Associated musculoskeletal injury.
Classification:
Type I : non displaced.
Type II : simple displacement with incongruous joint.
Type III : comminuted articular surface.
17
Presentation:
- Symptoms:
Ankle pain, inability to bear weight, deformity.
- Physical examination:
Swelling, abrasion, ecchymosis, fracture blisters.
Examine for associated musculoskeletal injury.
Neurovascular examination.
Imaging:
Recommended view (radiographic):
- AP view.
- Lateral view.
- Mortise view.
- Full length tibia/ fibula and foot x-ray performed for fracture
extension.
CT scan :
- Delineate articular involvement.
- Surgical planning.
Treatment:
- Non operative treatment : immobilization by long leg cast for
six weeks followed by fracture brace and exercise.
Indication:
1. Stable fracture pattern without articular surface
displacement.
2. Critically ill or non ambulatory patients.
3. Significant risk of skin problem( diabetes, vascular disease,
neuropathy)
- Operative treatment:
1. Temporizing spanning external fixation cross ankle joint.

18
- Provide stabilization to allow soft tissue healing and swelling
subside.
- Fracture with significant joint depression or displacement.
2. ORIF. definitive fixation for majority of Pilon fracture.
Complication:
1. Wound slough.
2. Infection.
3. Varus malunion.
4. Nonunion.
5. Post traumatic arthritis.
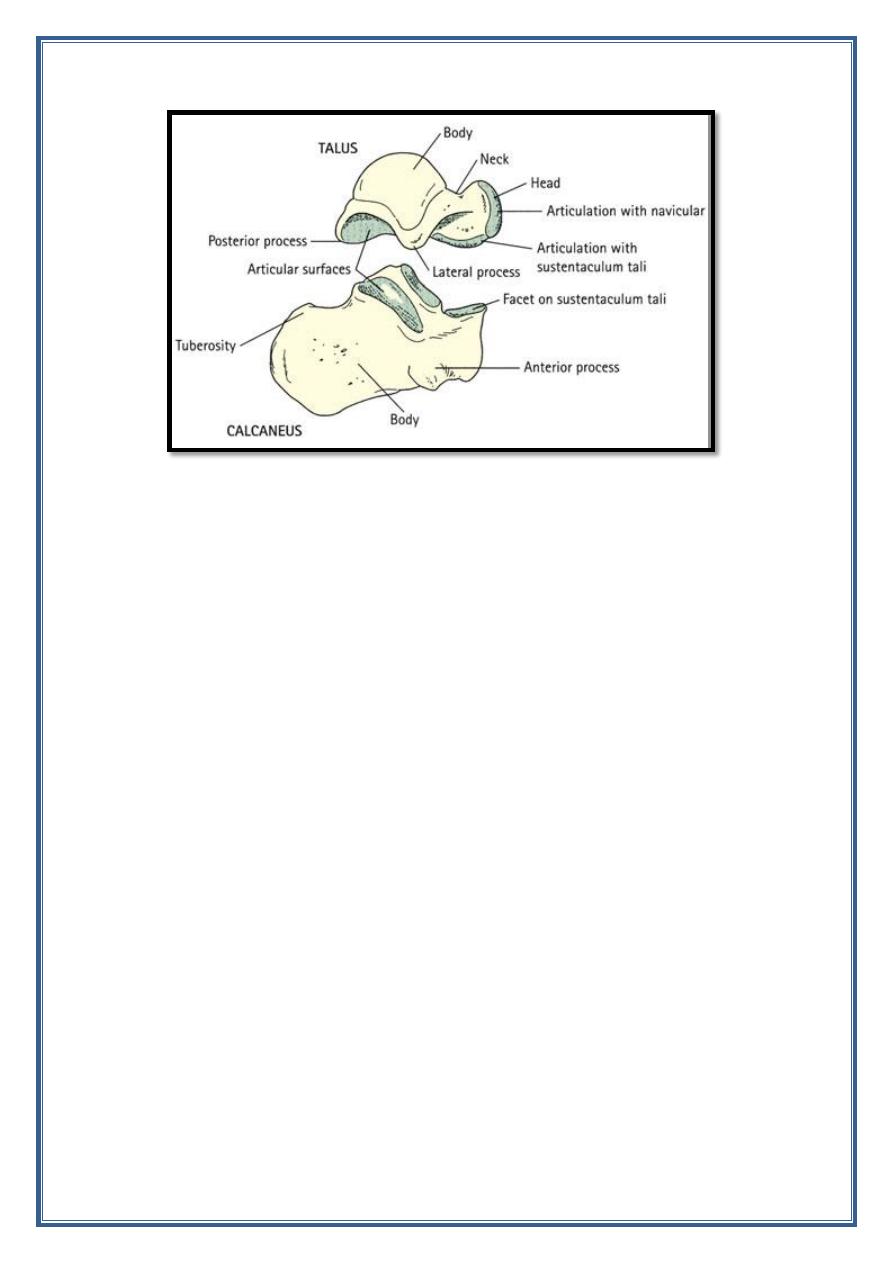
Injury of the talus:
The fracture and dislocation of the talus are relatively uncommon.
The injury include:
- Fracture of the neck.
- Fracture of the body.
- Fracture of the head.
- Fracture of the bone processes of the talus.
- Dislocation of the talus.
19
The fracture of the talus is more serious injury due to:
1. The talus is major weight bearing structure in the body.
2. It has avulnerable blood supply and is relatively common site for
post traumatic ischemic necrosis.
Mechanism of the injury:
Fracture of the talar neck is produced by high energy injury and force
dorsi -flexion with axial load associated with ipsilateral lower extremity
fracture (common).
Fracture of the body of the talus is usually compression injury due to fall
from hight.
Clinical features:
1. The foot and ankle are painful and swelling.
2. Obvious deformity if the fracture is displaced .
3. The skin may be tented or split.
Imaging:
- AP.
- Lateral.
- Oblique.
CT scan : help to identify associated injury of the ankle and foot.

20
Classification of Fractures of the neck of the talus
Type I
– undisplaced
Type II
– displaced (however little) and associated with subluxation or
dislocation of the subtalar joint
Type III
– displaced, with dislocation of the body of the talus from the
ankle joint
Type IV
– displaced vertical talar neck fracture with associated
talonavicular joint disruption.
Treatment:
- Nonoperative treatment: short leg cast for 8- 12 weeks (NWB
for the first 6 weeks) indicated in non displaced fracture.
- OPIF indicated in all displaced fracture.
Complication:
1. Malunion.
2. Vascular necrosis.
3. Osteoarthritis.
4. Non union.
5. Infection.
6. Wound dehiscence.
21
Fracture of the Calcaneum:
- It is the most commonly fractured tarsal bone.
- 5 -10% of the cases both heals are injured simultaneously.
- 17% open fracture.
Mechanism of the injury:
1. Traumatic axial loading is the primary mechanism of injury.
- Fall from a hight.
- Motor vehicle accident.
2. Avulsion fracture follow traction injuries of the tendo-achllis or
ankle ligament.
3. Direct trauma cause shattered of the bone.
Note: over 20 % of patient suffer from associated injuries of spine , pelvis
or hip.
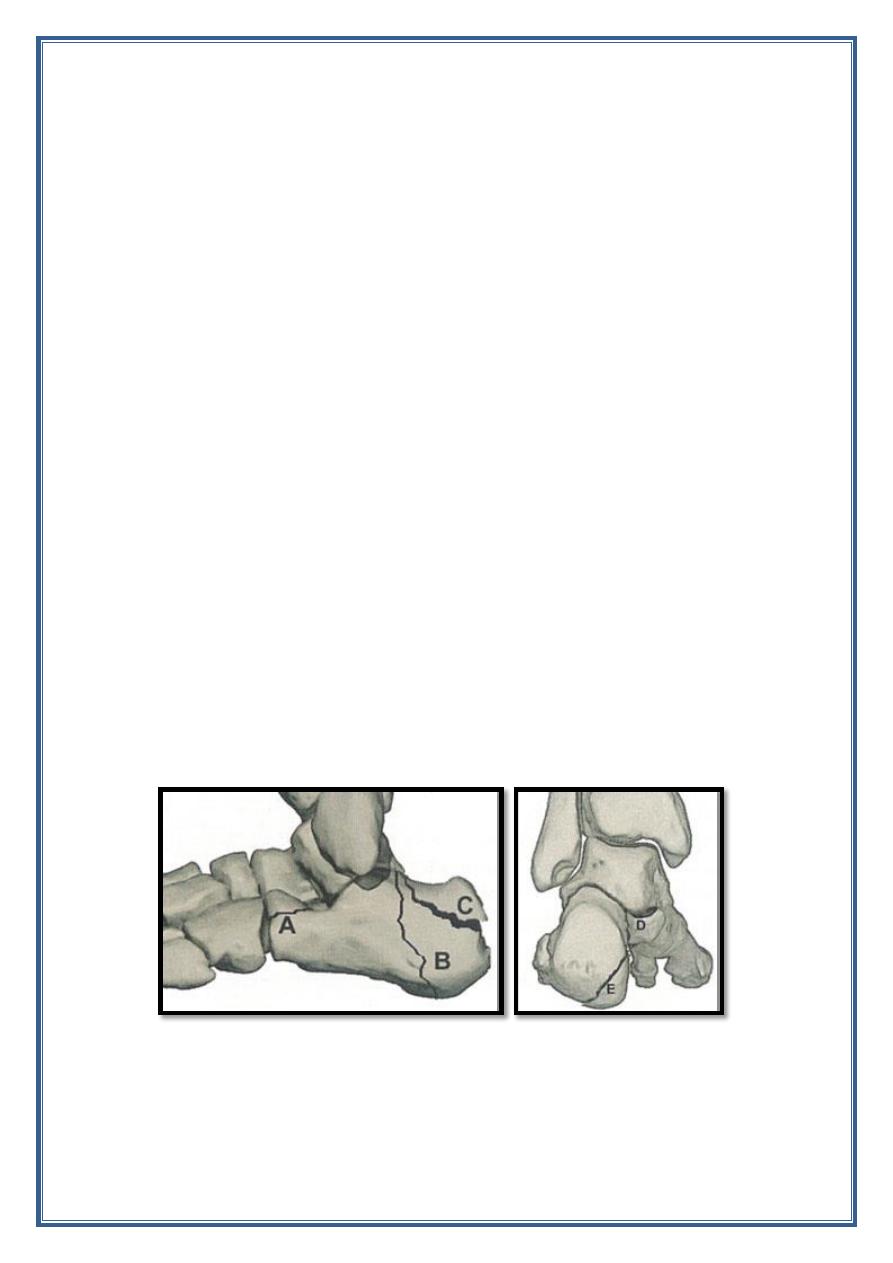
Classification:
Calcaneal fracture divided into:
i.
Extra articular fracture( account for 25 %) of calcaneal fracture,
and this include:
A. Anterior procces.
B. The body.
C. The tuberosity.
D. The sustentaculum tali.
E. The medial tubercle.
ii.
Intra articular fracture: these injuries are much more complex and
unpredictable in their outcome, and include:
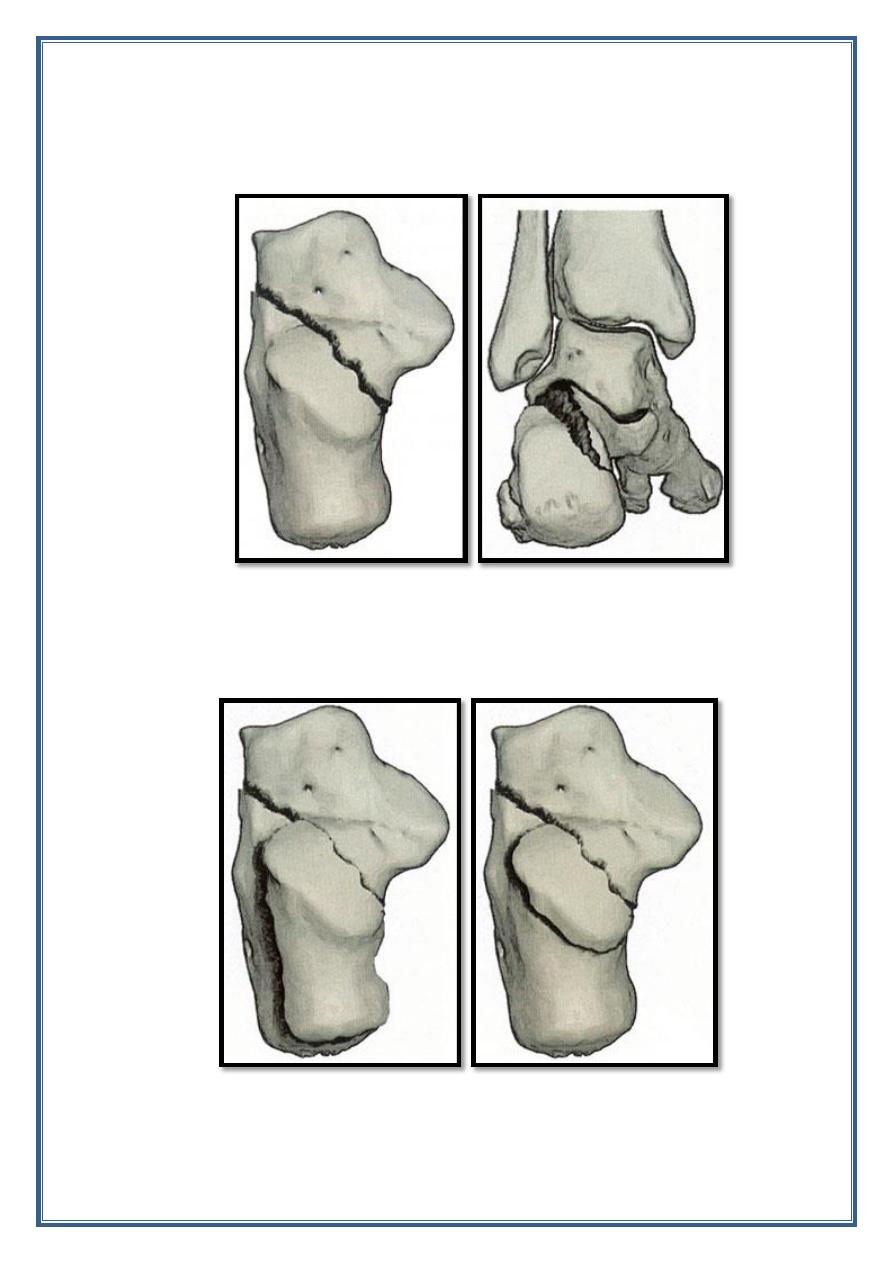
22
A. Primary fracture line is created by the impact of the talus on the
calcaneum. It run from obliquely posterior- medial to anterio-
lateral.
B. Secondary fracture line may create tongue or joint depression
fracture .
23
Presentation:
Symptoms.
o Pain.
Physical examination:
o Diffuse tenderness to palpation.
o Echemosis and swelling.
o Shortened, widened , heel with a varus deformity.
Imaging :
Radiographic view: AP, lateral, oblique.
- Extra articular fracture are usually fairly obvious.
- Intra articular fracture can also identified in plane film.
- If there is displacement of the fragment the lateral view may
show flattening of the tuber- joint angle ( Bohler' s angle).
CT scan : for accurate definition of intra articular fractures.
Treatment:
a. Extra articular fracture : the vast majority are treated closed :
1. Compression bandaging, ice packs, and elevation until the
swelling subside.
2. Exercise as soon as pain permits.
3. No weight bearing for 4 weeks and partial weight bearing for
another 4 week.
b. Intra articular fracture:
1. Undisplaced fracture are treated in the same way as extra
articular fracture.
2. Displaced fracture treated by ORIF as soon as the swelling
subside.
24
Complications:
Early:
1. Swelling and blistering .
2. Compartment syndrome.
Late:
1. Malunion.
2. Peronio tendon impingement.
3. insufficiency of the tendo- achillis.
4. Talo-calcaneal stiffness and osteoarthritis.
Injury of metatarsal bones
:
Metatarsal fractures are relatively common and are four types:
1. Crush fracture due to direct blow.
2. Spiral fracture of the shaft due to twisting injury.
3. Avulsion fracture due to ligament strain.
4. Insufficiency fracture (stress fracture). Due to repetitive stress.
Clinical features:
Pain, swelling, and bruising of the foot.
- With stress fracture the symptoms and signs are more insidious.
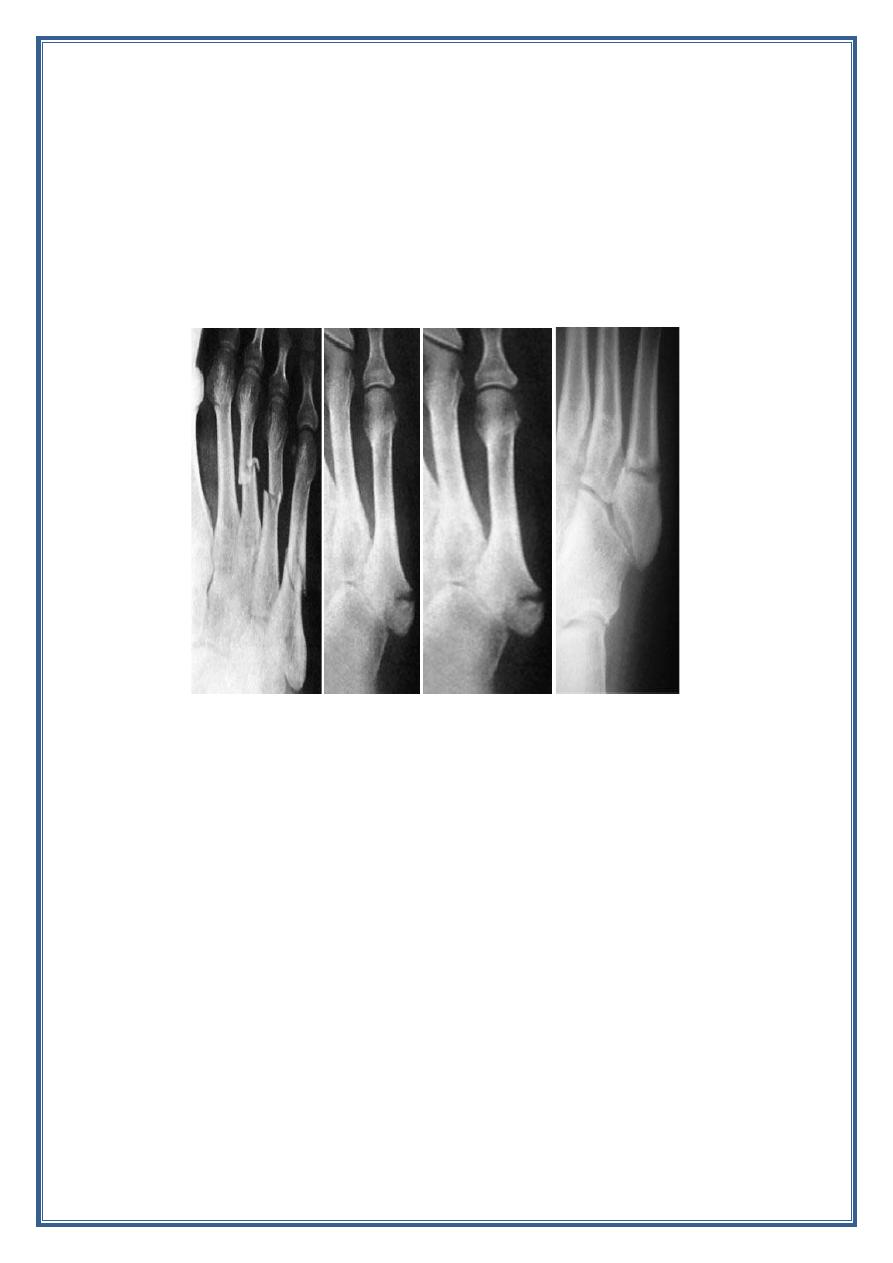
Imaging:
Ap , lateral , and oblique view .
Treatment:
a. Undisplaced and minimally displaced fractures can be treated
conservatively by:
1. The foot is elevated until swelling subside.
2. Leg immobilized in cast.
3. Non weight bearing for 4 weeks.
4. At the end of that period exercise start and the patient is
encouraged to resume normal activity.
25
b. Displaced fracture :
1. Displaced fracture from the 2
nd
-5
th
metatarsal in the coronal
plain can be treated conservatively.
2. Fracture of the 1
st
metatarsal and displaced fracture from 2
nd
–
5
th
in the sagittal plain ( i.e. depression or elevation of displaced
fragment) treated by ORIF with K wires or plates and screw.
