INTERTROCHANTERIC FRACTURES
Dr. Jamal Al-Saidy
M.B.Ch.B. .F.I.C.M.S
Intertrochanteric fractures are, by definition, extracapsular.
They are common in elderly, osteoporotic people; most of the patients are women in the
8th decade. However, in contrast to intracapsular fractures, extracapsular trochanteric
unite quite easily and seldom cause avascular necrosis.
Mechanism of injury
The fracture is caused either by a fall directly onto the greater trochanter or by an indirect
twisting injury.
The crack runs up between the lesser and greater trochanter and the proximal fragment
tends to displace in varus.
Pathological anatomy
& classification : -
Generally the
intertrochanteric fractures are divided
into stable and unstable varieties (Evans). The unstable one is that when
>
2 pieces, Reverse
oblique and Subtrochanteric extension.
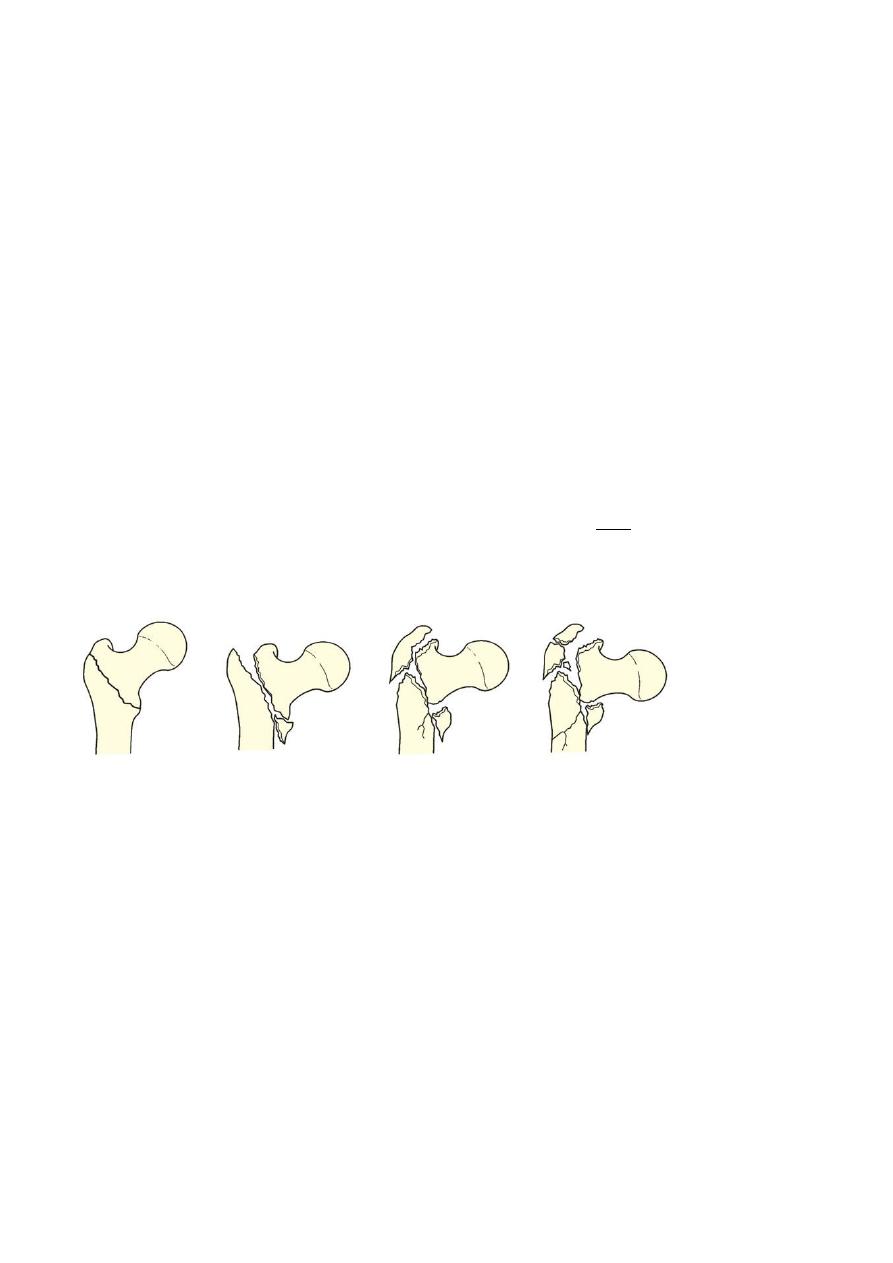
The importance of fracture pattern is detailed in the classification by Kyle (1994) which
distinguishes four basic patterns that reflect increasing the degree of the instability and
complexity and also increasing difficulty at reduction and fixation. Types 1 and 2 account for the
majority (nearly 60 per cent).
TYPE 1
TYPE 2
TYPE 3
TYPE 4
Type 1 :- Undisplaced, uncomminuted
Type 2 :- Displaced minimal comminuted lesser trochanter fracture varus
Type 3 :- Displaced greater trochanter fracture varus
Type 4 :- Severely comminuted subtrochanterec extension( reverse oblique)
Clinical features
The patient is usually old and is unable to stand.
The leg is shorter and more externally rotated than with a transcervical fracture (because
the fracture is extracapsular) and the patient cannot lift his or her leg.
X-ray
--
Undisplaced, stable fractures may show no more than a thin crack along the
intertrochanteric line; the diagnosis may have to be confirmed by scintigraphy or MRI.

--
More often the fracture is displaced and there may be considerable comminution.
Treatment
Intertrochanteric fractures are almost always treated by early internal fixation – not
because they fail to unite with conservative treatment (they unite quite readily), but (a) to
obtain the best possible position and (b) to get the patient up and walking as soon as
possible and thereby reduce the complications associated with prolonged recumbency.
Non-operative treatment may be appropriate for a small group who are too ill to undergo
anaesthesia; traction in bed until there is sufficient reduction of pain to allow mobilization
which much depends on the quality of nursing care and physical therapy.
Fracture reduction at surgery is performed on a fracture table that provides slight traction
and internal rotation; the position is checked by x-ray and the fracture is fixed with an
angled device – preferably a sliding screw in conjunction with a plate or intramedullary
nail. The side plate should be long enough to accommodate at least 4 screws below the
fracture line.
If closed reduction fails to achieve a satisfactory position, open reduction and
manipulation of the fragments will be necessary.
The addition of bone grafts may hasten union of the medial cortex.
Postoperatively, exercises are started on the day after operation and the patient allowed
up and partial weightbearing as soon as possible.
Complications
most of these
ctures,
fra
as with femoral neck
Early complications are the same
-
:
EARLY
patients
are in poor health.
LATE
Failed fixation
Malunion Varus and external rotation deformities are common.
Non-union: Intertrochanteric fractures seldom fail to unite.
Pathological fractures :
Intertrochanteric fractures may be due to metastatic disease or myeloma, In addition to
internal fixation, methylmethacrylate cement may be packed in the defect to improve
stability.
If there is involvement of the femoral neck, replacement with a cemented prosthesis may
be preferable.
THANK YOU
Dr. Jamal Al-Saidy
M.B.Ch.B. .F.I.C.M.S
