NEOPLASIA
Dr Mustafa Salah Fadhil MSc, FIBMS pathBenign VS Malignant
•Feature
BenignMalignant
Growth rate
Slow
Relatively rapid
Mitoses
Infrequent
Frequent & often atypical
Histological resemblance to normal tissue
Good
Variable, from well differentiated to completely undifferentiated (anaplastic).
Nuclear morphology
Near normal
Usually enlarged, hyperchromatic , irregular outlines, multiple nucleoli & pleomorphic ( variable sizes & shapes
Invasion
No
Yes
Metastasis
Never
Frequent
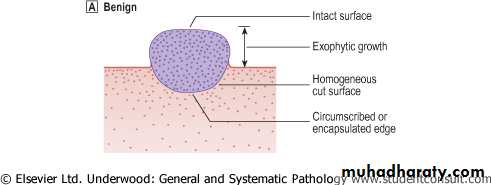
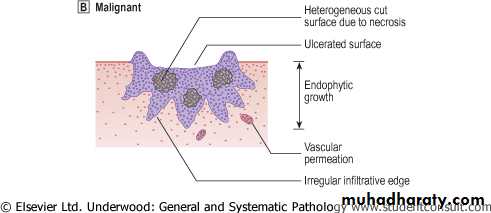
Border
Often circumscribed or encapsulated
Often poorly defined or irregular
Necrosis
rare
Common
ulceration
Rare
Common on skin or mucosal surface.
Direction of growth on skin or mucosal surface
Often exophytic
Often endophytic
Certain terms
• Dysplasia
• Carcinoma in situ• Anaplasia
• Metastasis
Dysplasia
Disordered growth in epithelial membranes (e.g. the squamous epithelium of the cervix, skin, and bronchial mucosa) characterized by1. Pleomorphism
2. Loss of polarity
3. Nuclear Changes
a. hyperchromasia
b. ↑N/C
c. ↑Mitotic figures
Some dysplastic lesions are almost certainly reversible
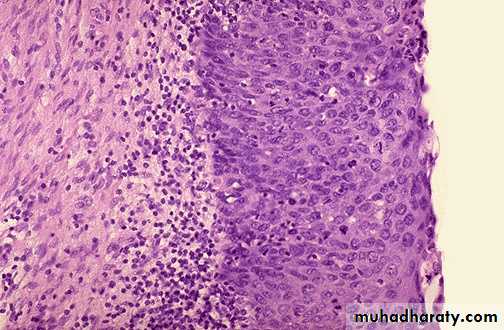
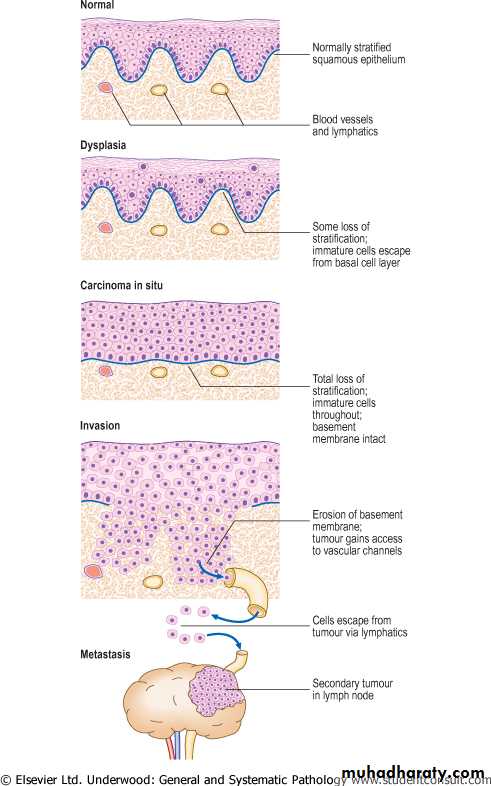
Carcinoma in situWhen dysplastic changes involve the full thickness of the epithelium, but does not penetrate the basement membrane, it is called carcinoma in situ (CIN).
• Only in epithelia. Not in mesenchymal tissues
• Complete excision at this very early stage will guarantee a cure.
• Once the tumor cells breach the basement membrane, the tumor is said to be invasive
• The phase of in situ growth may last for several years before invasion commences.
• The term ‘intraepithelial neoplasia’, as in cervical intraepithelial neoplasia (CIN), is used increasingly to encompass both carcinoma in situ and dysplasia
Cervix: part of stratified squamous epithelium shows disorderly arranged cells, hyperchromatic nuclei with mitosis . The basement membrane is intact, and there is no tumor cells in the subepithelial stromaDiagnosis: Carcinoma In Situ
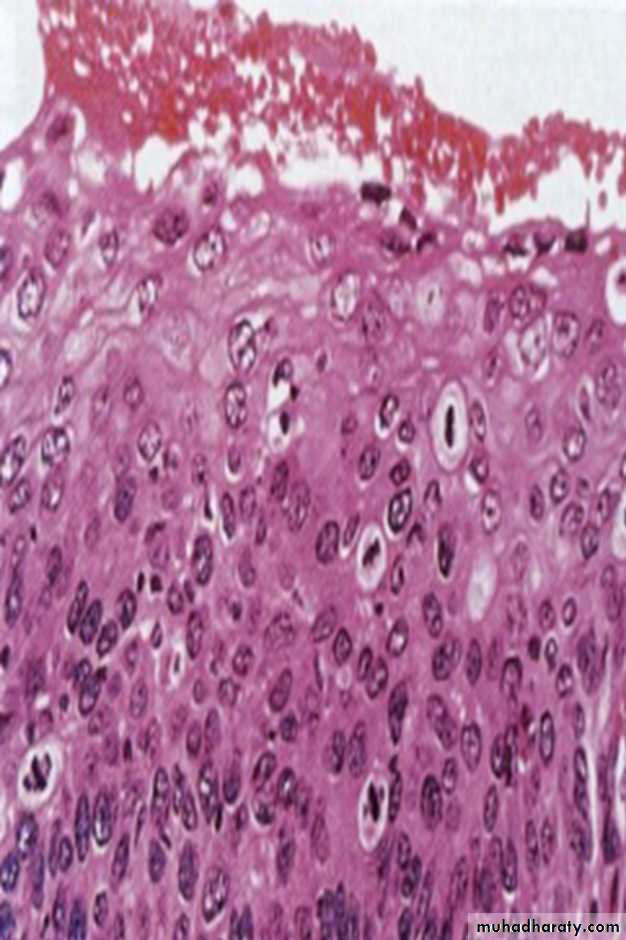
Squamous cell carcinoma following in situ carcinoma
Evolution of an invasive squamous cell carcinoma from the precursor lesions of dysplasia and carcinoma in situ (usually grouped together as intraepithelial neoplasia). Note that the tumor cells cannot reach routes of metastasis such as blood vessels and lymphatics until the basement membrane has been breached
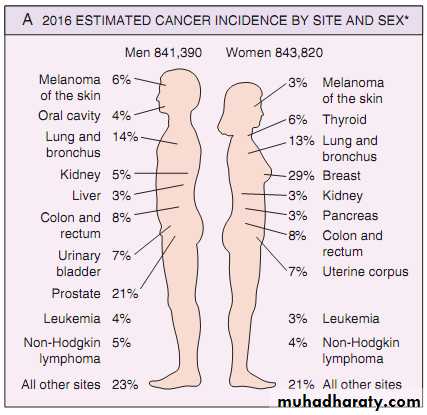
Cancer incidence
Spread of Malignant Tumors:
Malignant tumors can spread in several ways:
• Local spread
• Lymphatic spread
• Blood (haematogenous) spread
• Transcoelomic spread
• Intraepithelial spread
1- Local Spread
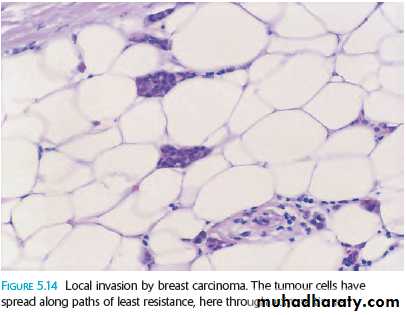
-Malignant cells have the ability to invade the surrounding tissues .-Tumor cells follow the paths of least resistance and spread easily through loose fibrous and adipose tissue.
-For epithelial tumors the first step should break the basement membrane.
Local invasion by breast carcinoma. The tumor cells have spread along paths of least resistance, here through adipose tissue
2- Lymphatic Spread
This is the principal mode by which carcinomas spread.
The very thin walls of lymphatics are readily penetrated by tumor cell , which is carried along in the lymph to Sentinel lymph node (the first node in a regional lymphatic basin that receives lymph flow from the primary tumor).
The enlargement of the regional nodes may be caused by either:
1. The spread of cancer cells (metastasis) or
2. Reactive hyperplasia to tumor cell antigens (no cells) (Nodal enlargement near a cancer does not necessarily mean dissemination).
• Ultimately the malignant cells may reach the thoracic duct and enter the superior vena cava from which further dissemination through the blood stream may occur (Haematogenous Spread).
Microscopically, metastatic adenocarcinoma in a lymph node It is common for carcinomas to metastasize to lymph nodes
3- Blood (Haematogenous) Spread
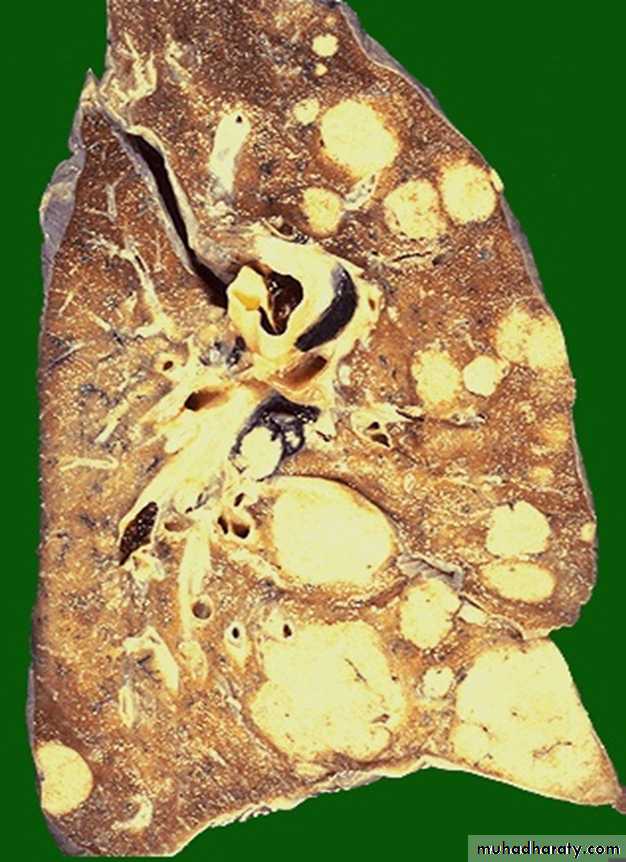
It is typical of sarcomas but is also seen with carcinomas (in the later stages).Tumor cells are able to invade thin walled veins and grow along the venous system or embolize into the blood stream.
The site of initial metastasis depends on the venous flow draining the tumor site.
• Lungs & Liver are the most frequently involved by metastases in haematogenous spread.
Metastatic adenocarcinoma lung
Pulmonary metastases(Cannonball appearance)
Liver metastasis by
adenocarcinomaLiver metastases
(Cannonball appearance)
4- Transcoelomic Spread:
It means spread of tumor across body cavities, (the peritoneal, pleural and pericardial spaces). This is best seen in intra-abdominal tumors, especially ovarian carcinoma and gastric carcinoma.Example: Gastric carcinoma can spread in this way to involve the peritoneal cavity, often seeding in the ovaries (bilateral). known as Krukenberg’s tumors
Transcoelomic spread (peritoneal cavity)
Metastatic breast carcinoma-pleura: Neoplasms can spread by seeding along body cavities. Here is a focus of metastatic breast carcinoma seen along the pleura overlying the lung.5-Intraepithelial Spread
This is the process by which tumor cells can infiltrate between the cells of a normal epithelium, without invading the underlying stroma.
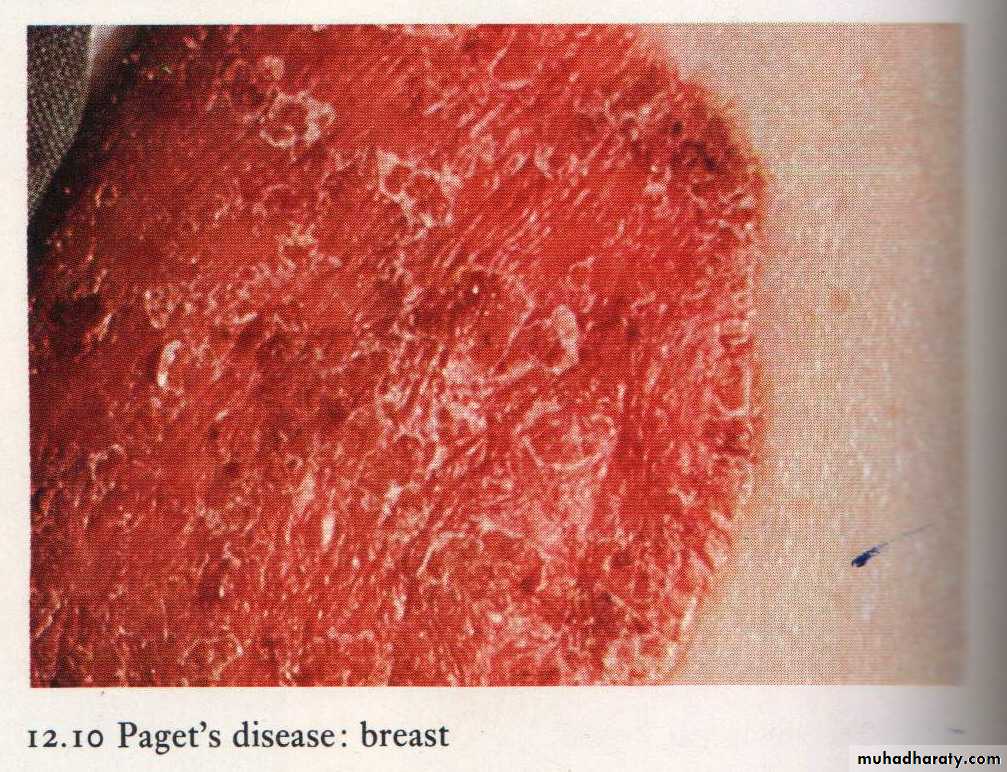
It is best seen in Paget’s disease of the nipple in which the cells of ductal carcinoma (in situ or invasive carcinoma) of breast grow through the duct into the nipple skin giving an appearance resembling eczema
Pagetˈs disease of the nipple
Paget's disease of the breast : intraepithelial extension of an underlying ductal carcinoma in situ or invasive ductal carcinoma.
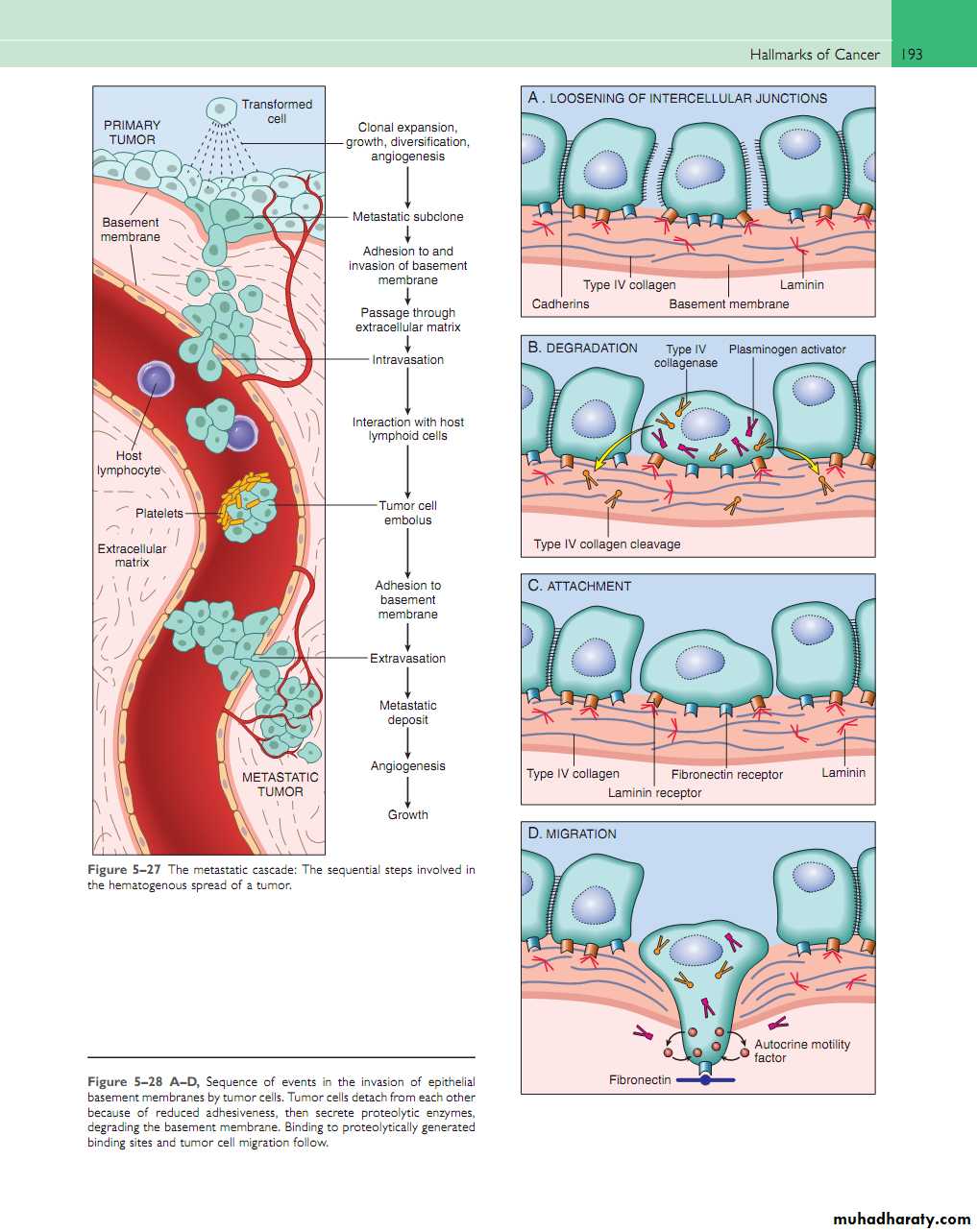
Mechanism of tumor spread
I/ Direct Spread and Invasiveness1-Reduction in Cell- Cell Adhesion
reduced expression of E-cadherin (adhesion molecule)
2-Invasion of Basement Membrane and Stroma
1. cancer cells attach to the basement membrane (integrin molecule)
2. production of proteolytic enzymes by cancer
3-Tumor Cell Motility
The cells extrude pseudopodia at the front and attach to stromal proteins (growth factors, stromal components and cytokines)II/ Angiogenesis:
(New blood vessels formation)It is important step in tumor growth and metastasis
The stimulus for angiogenesis is the increased production of angiogenic factors by the tumor cells, especially vascular endothelial growth factor (VEGF), fibroblast growth factors.
The steps involved in angiogenesis include:
Proteolytic digestion of basement membrane by plasminogen activators and matrix metalloproteinases
Migration of endothelial cells, initially as a solid cord
Proliferation of endothelial cellsOrganization of the cords of endothelial cells into new blood vessels with lumens.
III/vascular InvasionThe thin walls and poorly formed basement membranes of newly formed blood vessels allow the tumor cells to penetrate.
Once tumor cells are free within the lumen of the blood vessel, they are carried into the circulation (tumor embolus) and lodge in a capillary bed.
IV/ Establishment of a New Colony
This involves tumor embolus extravasation with formation of new deposits, associated with development of a tumor blood supply by stimulation of angiogenesis as previously described.Mechanism of tumor spread
The site at which circulating tumor cells leave the capillaries to form secondary deposits is related to:1- The anatomic location of primary tumor
2- Vascular drainage of the primary tumor. Many tumors arrest in the first capillary bed they encounter (lung and liver, most commonly)
3- Tropism of particular tumors for specific tissues, e.g. prostatic carcinoma preferentially spreads to bone, this due to chemokines and tumor cells may have adhesion molecules whose ligands are expressed preferentially on the endothelial cells of the target organ.
Benign tumor
Large painless palpable lump (feeling of discomfort)Hormonal Effects when benign tumor arising in endocrine gland
e.g. thyroid adenoma leads to hyperthyroidism
Local effect (pressure effects) due to tumor expansion e.g.
Pituitary adenoma may cause hypo-pitutarisim
Benign meningeal tumor causing epilepsy)
Clinical effects of tumors
Transformation into a malignant neoplasm (e.g. adenomatous polyp progressing to an adenocarcinoma)
Obstruction to the flow of fluid (e.g. benign epithelial tumor blocking a duct)
Effects of Malignant tumors
1-local Effects (direct effect):
-Pain due to compress the adjacent structures such as nerves by the mass of malignant tumor .-Hemorrhage from an ulcerated carcinoma may be acute or chronic, thus leading to iron deficiency anemia.
-Narrowing (stenosis) or complete obstruction of a hollow viscus (also can be seen in big benign tumors).
-Hormonal effect, cancers arising within or metastatic to an endocrine gland may cause an endocrine insufficiency by destroying the gland.
2-Metastatic Effects:
Metastases can cause similar mass effects to primary tumors, but because they are usually multiple consequences tend to be more severe.• Effects of Malignant tumors
3-Non-metastatic Effects:
This is a heterogeneous group of disorders, many due to release of cytokines such as interleukin 1 (IL-1) and tumor necrosis factor α (TNFα) from tumor cells.Patients with advanced cancer are often wasted (cachectic) with weight loss, anorexia and
Immunosuppression
Abnormalities of coagulation
Neurological disorders, for example neuropathy, cerebellar degeneration.
4-Paraneoplastic Syndromes:
Symptoms complexes in individuals with cancer that cannot be explained by presence of primary cancer or its metastases, this due to the tumors produce hormones or hormone like substances not normally produced by their tissue of origin.Occur in about 10% of persons with cancer.
They are important for the following reasons:
They may represent the earliest manifestation of an occult neoplasm.
May cause significant clinical problems and may even be lethal.
May clinically mimic metastatic disease thus confuse management .
Causal mechanism
Underlying cancerClinical syndromes
• ACTH or
• ACTH-like substance
Small-cell carcinoma of lung
Cushing Syndrome
Pancreatic carcinomaNeural tumors
Parathyroid hormone–related protein (PTHRP), TGF-α, TNF, IL-1
Squamous cell carcinoma of the lungHypercalcaemia
Breast cancerRenal carcinoma
Adult T-cell leukemia /lymphomaCausal mechanism
Underlying carcinomaClinical Syndromes
Insulin or insulin-like substance
Ovarian carcinomaHypoglycaemia
Fibrosarcoma
Other mesenchymal sarcomas
ErythropoietinGastric carcinoma
Polycythemia
Renal carcinoma
Cerebellar hemangiomaHepatocellular carcinoma
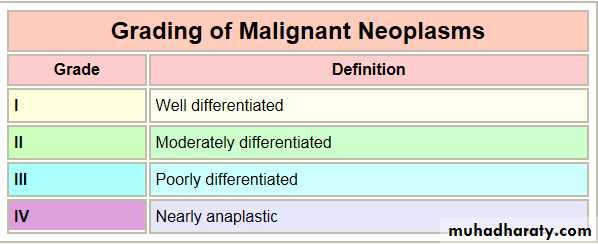
Grading and Staging of Tumors:Methods are used to asses the aggressiveness of malignant tumors and the spread of them.
necessary for prognosis of the malignant tumor and choice the proper treatmentGrading of malignant tumors
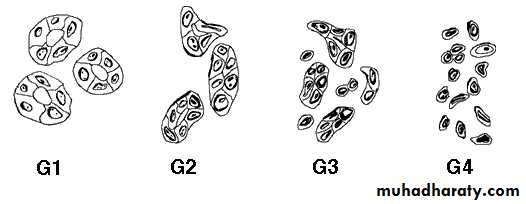
It is based on the degree of differentiation (the resemblance (degree of similarity) of cancer cells to tissue of origin).
The main parameters that look for :
Mitotic activity
Nuclear pleomorphism
Degree of differentiation
Extent of necrosis.
Degrees of differentiation adenocarcinoma
Normalwell
moderate
poor
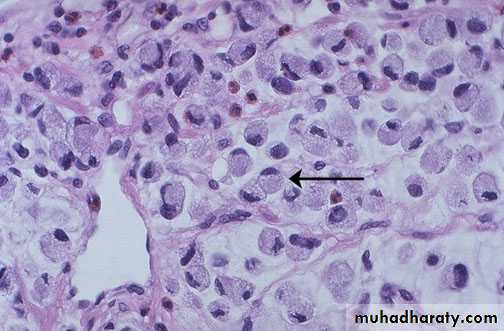
slide shows the cell nest composed of malignant squamous cells ( pleomorphic, hyperchromatic nuclei & high N/C ratio) with keratin peardiagnosis: well differentiated squamous cell carcinoma
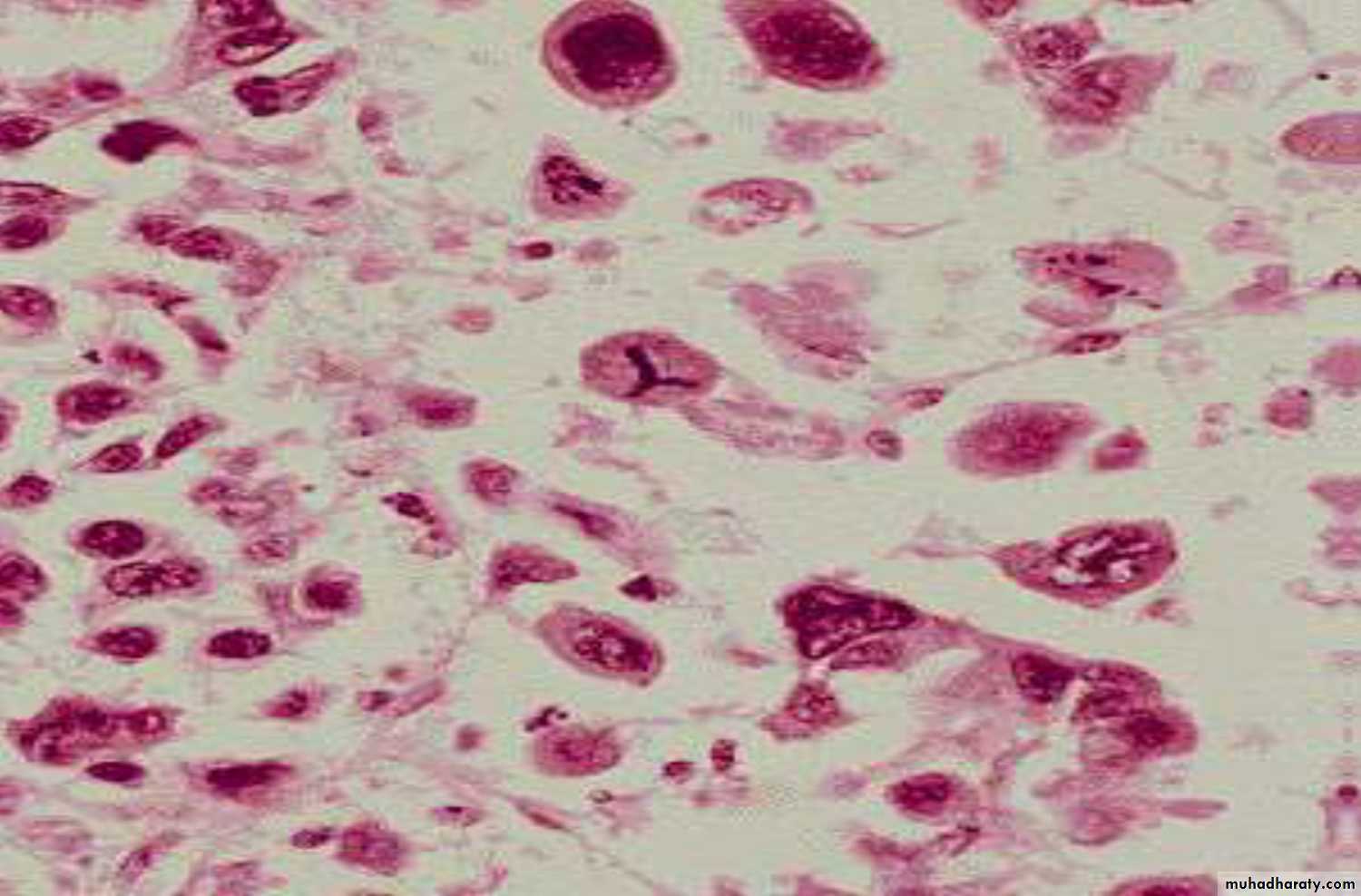
Rhabdomyosarcoma, marked cellular and nuclear pleomorphism, hyperchromatic nuclei, and tumor giant cells.
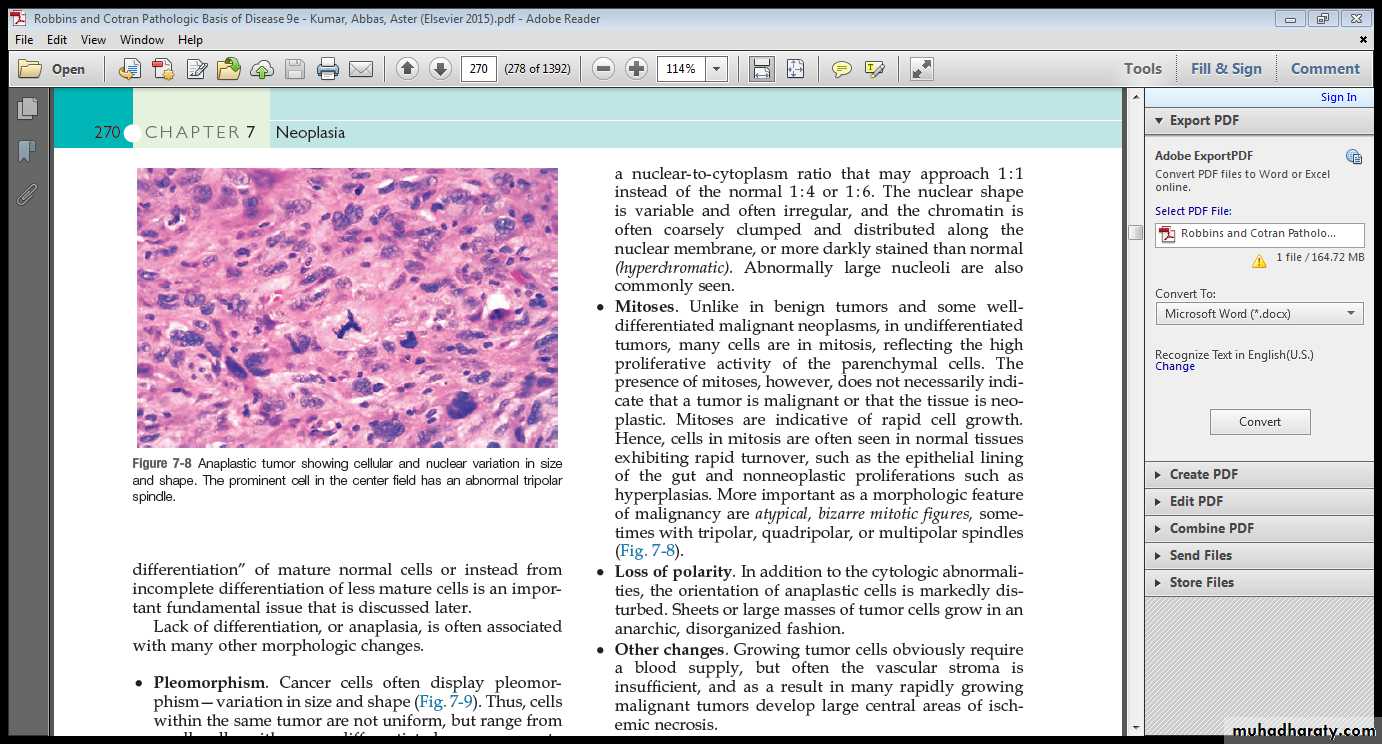
Anaplastic tumor showing cellular and nuclear variation in size
and shape. The prominent cell in the center field has an abnormal tripolar spindle.Signet ring carcinoma of stomach( Poorly differentiated Adeno-carcinoma) The tumor cells have eccentric nuclei, pushed to the side by a central globule of mucus.
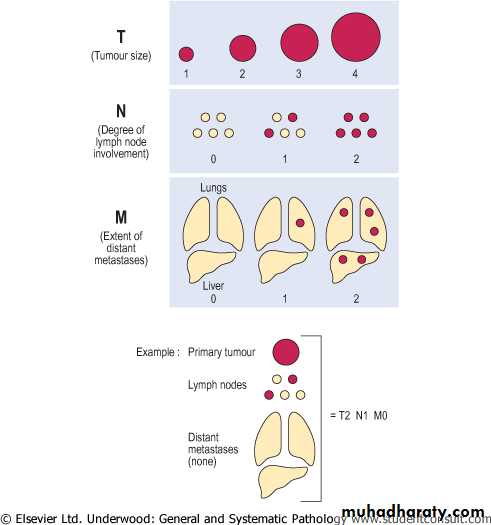
The staging of cancers
Tumor stage : assess the extent of tumor clinically & pathological.
-The major staging system currently in use is the American Joint Committee(AJC) on Cancer Staging. This system uses a classification called the TNM System.
-Other systems include the Dukes’ staging system for colonic carcinoma, Clarks & Breslow for Melanoma
General principles of TNM staging system:
T for size of primary tumorTis (in situ) is referred to carcinoma limited to mucosa
T1-T4 : ↑size of tumor OR depth of invasion
N for lymph node involvement
-N0: no nodal involvement
-N1 to N3: involvement of an ↑number and range of nodes
M for distant metastases
-M0: no distant metastases.
-M1 presence of blood-borne metastases.
Staging is of greater clinical value than grading.