1
NEONATOLOGY
By dr. Adnan Al-Rikabi
Definition of terms :
1. The normal human gestational period is 280 days or 40 weeks , calculated
from the first day of the mother last menstrual cycle .
a- Preterm gestation refers to delivery at less than 37 wks gestation .
b- Term gestation refers to delivery at 38 to less than 42 wks gestation .
c- Post term gestation refers to delivery at or after 42 wks gestation .
2. The neonatal period is defined as the first 28 days ( 4 wks) of life for term
infant , although , from a practical standpoint it is extended in the case of
prematurely delivered infant.
3. Fetal and neonatal growth :
a- Fetal growth, the fetal growth rate is 5 g /day at 14-15 wks gestation, 10
g/day at 20 wks and 30 g/day at 32-34 wks. The growth rate slows after 36
wks gestation.
b- Neonatal growth :
(1)- after birth , there is a loss of weight due to a loss of extracellular
water and suboptimal caloric intake . term infant lose 5% of their birth
weight , preterm infants lose up to 15% of their birth weight .
(2)- term infant regain their birth weight by the end of the first week of life
and thereafter gain 20-30 g/ day .
Delivery room management of the newborn
A- Goals .the goals of delivery room management are to assess and promptly
attend the immediate needs (e.g oxygenations, ventilations ) and potential
problems (e.g serious anomalies ) of the newborn .
B- Physical layout and equipment . the newborn resuscitation are should be in
immediate proximity to the delivery room . it should have adequate lighting
and space for personal and equipment for resuscitation, including a bed with
a radiant warmer .
C- Preparation for delivery .
1- Obtaining perinatal information .the pediatrician must have specific
information concerning the mother and the fetus to prepare for routine care
of the mother and newborn as well as treatment of specific problems
related to a particular delivery ,
a- Obstetric history should include all information that may be pertinent
to the immediate fetal conditions .the information is best obtained from
the obstetrician and the medical chart and by direct communication
2
with parents .important issues are ( maternal age , medical and
previous obstetric history , length of gestations , blood group
incompatibilities , maternal infections , maternal drug use , ultrasound
evaluations of fetal growth and amniotic fluid volume or congenital
anomalies , signs of chorioamnionitis including prolonged rupture of
fetal membrane ,maternal fever , and leukocytosis .
b- Labor history should include ( fetal heart tracing , duration of fetal
membrane rupture , evaluation of amniotic fluid (color and quantity ),
progress of labor and fetal blood PH.
2- Composition of the resuscitation team .personnel and their tasks vary with
type of delivery that is anticipated .high risk deliveries include (maternal
diabetic , RH and ABO incompatibility , preterm delivery at less than 38
wks ,post term delivery at more than 42 wks , multiple gestations ,maternal
bleeding , severe pre eclampsia ,IUGR, fetal anomalies , breech
presentations , cesarean delivery , fetal distress .So high –risk team include
a- Team leader to direct resuscitation and direct and institute airway
management .
b- One to assess heart rate and to initiate cardiac compression if needed .
c- One to assess with drying , suctioning , ventilation ,and prepare drugs
for injection .
d- One to gain intravenous access and to administer drugs .
3- Equipment for resuscitation include :
a- Airway management (suction pump with regulator ,DeLee suction
catheter , oral airway with deferent sizes ,endotracheal tubes ,
laryngoscope , suction catheter .
b- Ventilations and oxygenations ( oxygen source , mask of deferent sizes
, bag with oxygen reservoir ) .
c- Intravenous access ( umbilical catheter 3.5 F and 5 F ,instruments for
umbilical cut down , saline solution 0.9% .
d- Drugs like (epinephrine , plasma volume expander , sodium
bicarbonate or naloxone ) .
D- Assessment of the newborn and the APGAR score . The goal of the
initial assessment is to determined the newborn state of oxygenation and
ventilation. this is usually done by performing an abbreviated APGAR
evaluation.
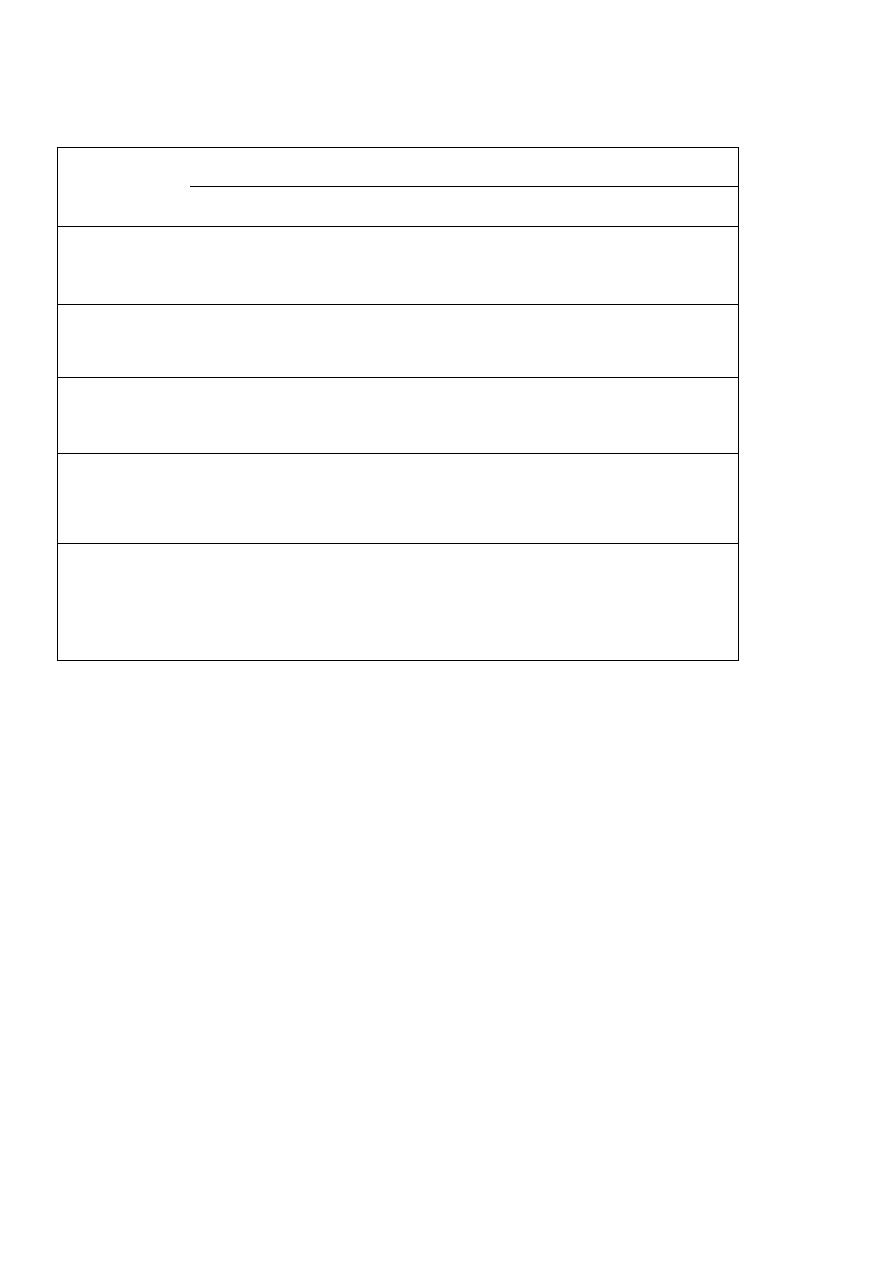
3
TABLE . APGAR evaluation of the newborn
Sign
Score
0 1 2
Heart rate
Absent <100 beats/min >100 beats/min
Respiratory
effort
Absent weak, irregular
strong , regular
Muscle tone
Flaccid
some flexion
well flexed
Response to
catheter in
nostril
No response grimace
cough or sneeze
Skin color
Blue ,pale body pink
entire body pink
Extremities blue
1- The degree score was devised as a means of assessing the oxygenation ,
ventilation, and degree of asphyxia in a uniform manner that quickly
communicates information to all people involved in the resuscitation of the
newborn .
The APGAR evaluation is performed at one and five minutes after birth .
Five signs – heart rate ,respiratory effort ,muscle tone ,reflex irritability
and skin color __are examined and assigned a score of 0, 1, 2. The
APGAR score is obtained by adding all individual scores .
a- A score of 8-10 reflect good oxygenation and ventilation and indicates
no need for vigorous resuscitation .
b- A score 5-7 indicate a need for stimulation and supplemental oxygen .
c- A score lees than 5 indicates a need for assisted ventilation and
possible cardiac support .
1- The apgar score is a useful method of communicating the well-being of
the newborn .however urgently needed resuscitation should not be delayed
while a full examination Is performed . bradycardia or poor respiratory
effort alone indicate a need for immediate resuscitation .
4
2- The apgar score at five minute reflects the adequacy of resuscitation and
the degree of perinatal asphyxia .
E- Resuscitation . the purpose of resuscitation is to re-oxygenate the CNS of
the newborn by providing oxygen , establishing ventilation , and ensuring an
adequate cardiac output . although it may be difficult to differentiate
primary apnea from secondary apnea , a quick assessment of the newborn
skin color , respiratory activity , and heart rate should allow prompt
institution of appropriate resuscitation .
1-Routine procedures .the evaluation and procedures that constitute the
resuscitation of the newborn are listed in the order in which they should be
initiated .
a- Maintenance of body heat . the infant should be dried and provided
with radiant heat to maintain body temperature . it is important to
avoid hypothermia , which will increase the newborn oxygen
consumption .
b- Establishment of an airway . immediately after delivery , the infant
head should be placed in a neutral or slightly extended position and an
airway established by clearing the mouth , nose and pharynx of thick
secretion or meconium . deep and frequent oropharyngeal suctioning
should be avoided because it will increase the vagal output causing
apnea and bradycardia .
c- Ventilation . the adequacy of air exchange in the newborn must be
assessed . in the most cases , drying off, suctioning and tactile
stimulation ( e. g. gentle flicking of the feet or rubbing of the back ) are
adequate to induce effective spontaneous ventilation .
(1) If ventilation is adequate , supplemental oxygen may be given to
improve heart rate or skin color .
(2) If supplemental oxygen does not improve heart rate or skin color ,
or if ventilation is inadequate , mechanical ventilation should be
initiated , using mask and bag ventilation .
(a) If spontaneous ventilation improves ,mechanical ventilation
should be stopped and supplemental oxygen resumed .
(b) If the response is poor or if airway obstruction occurs ,an
endotracheal tube should be inserted and mechanical
ventilation continued .
5
d- Circulation . If mechanical ventilation does not improve the heart rate
or skin color one of the following steps taken .
(1)- If heart rate is less than 60beats b/min or between 60 and 80
beats / min and not improving cardiac compression is initiated
over the lower third of the sternum at a rate of 90 compression /min ,
the ratio of compression to ventilation is 3:1(90 compression , 30
breath ) if heart rate not improve , epinephrine is administered via an
umbilical venous catheter or endotracheal tube .
(2)- If heart rate is 80 beats /min or greater but there is poor perfusion
or weak pulse , a plasma volume –expanding agent is administered at a
dose of 15 ml / kg .
d- Drug support . the following drugs may be useful during resuscitation .
(1) Sodium bicarbonate (2 mEq/kg ) should be reserved until it is
clear that a metabolic acidosis exists .
(2) Naloxone (0.1mg/kg) may be helpful for poor spontaneous
respiratory effort secondary to maternal narcotic use during labor .
Naloxone is contraindicated in an infant born to mother who is
addicted to narcotics .
(3) Dopamine (5-20 ug/kg/min) improve myocardial function .
2-Special proplems requiring resuscitation:
a- Meconium aspiration syndrome . thick meconium is a serious
concern because it may be aspirated and result in aspiration pneumonia
, it imperative that the meconium be removed from the airway before
any attempt is made to ventilate the infant .
b- Choanal atresia is a membrane or bony obstruction of the posterior
nasal passage .
c- Progressive respiratory distress or cyanosis that occur in an infant
despite appropriate resuscitation usually suggests an underlying
disorder of the cardiopulmonary system , which require immediate
investigation ( cyanotic heart disease , congenital or acquired disorders
of the lung like diaphragmatic hernia or pneumothorax) .
6
Neonatal examination
Goals of neonatal examination :
1- Assess wellness of the newborn , screening for general abnormalities , birth
trauma or acquired medical problems .
2- Assess the newborn for gestational age and appropriateness of size for
gestational age .
3- When appropriate confirm infants normality to parents .
4- When appropriate demystify and reassure parents about common , benign
variation in newborn physical examination or behavior .
5- Foster early infants –parent bonding and parental self-confidence .
Physical examination :
1- general appearance .important observation include body proportion , activity
, quality of cry ,skin color , gross abnormalities ,unusual features and signs of
respiratory distress , weight , length and head circumference measurement are
obtained and recorded .
2- skin color may suggest cyanosis , pallor or jaundice .
a- normal peripheral vascular instability presentation include skin
mottling . peri-oral cyanosis and cyanosis of the hand sand feet , with lips ,
mucous membrane , nail beds and tongue remaining pink .
b- cracking or desquamation of the skin is normal in the term and
postmature infants . in the term infant fine downy hair known as lanugo
covers the skin , particularly the shoulder and upper back .
c- jaundice in the neonate is first visible on the face and as the serum
bilirubin level rises it progress caudally to include the rest of the body and
the sclera .natural sunlight should be used to inspect the skin for the extent
of jaundice .
d- birth marks are common and visible at birth include flat vascular nevi
(e.g.salmon patch nevus and port wine stains ) and Mongolian spots .raised
vascular nevi usually become apparent several wks after birth ( e.g.
capillary or strawberry hemangioma , cavernous hemangioma ) .
e- benign rashes are common :
1- comerythema toxi has a flea-bite appearance with scattered
erythematous macules that may contain papulopustular centers filled
with eosinophils . this rash typically changes distribution from day to
day .
2- milia are transient fin , pinpoint, yellow-white papules caused by retain
sebum that typically cover the bridge of the nose, chin,and cheeks .
7
3- neonatal pustular melanosis consists of small vesiculopustules that
are present at birth and rupture within a few days , leaving transient
pigmented macules with scaly borders .
3-head and neck .the head and face frequently exhibit sequelae of the birth
process including bruises and asymmetries . most resolve spontaneously
.facial features should be carefully inspected for size , placement and symmetry .
a- .palpation of skull determines contour , extent of separation or over riding of
sutures and the size of the fontanelles .
1- molding of the head shape into elongated or asymmetric contour occurs
secondary to intrauterine pressure or forces during labor .
2- cephalhematoma and caput succedaneum .
b- eyes : dimming the room light cradling the occiput in the examiner hand to left
the baby head off the mattress may stimulate the baby to open her or his eyes .
1- conjunctival or sclera hemorrhage resolve with time and usually benign .
2- the presence of a red reflex exclude the presence of lens opacities .
3- up to 3 months the eyes normally may appear to cross intermittently.
c- Ears patency of the canal should be determined . malformed or low set ears
may be associated with auditory or renal abnormalities .
d- Nose newborns are nose breathers obstruction of the nasal passage reslt in
respiratory distress .
e- Mouth . should be examined by inspection and palpation . common minor
abnormalities include small, white epithelial pearls along the gum margins .
small white cyst termed epistein pearls along the median raphe of the hard
palate . palpation may reveal a submucosal bony cleft of palate .
f- Neck must be hyperextended to inspect adequately for masses . congenital
masses include goiter ,cystic hgroma , brachial cleft cysts and thyroglossal
cysts . a webbing of the neck is seen in turner syndrome .
4-chest :
a- Clavicles are palpated for signs of fractures
b- Respiratory rate and pattern and the presence of chest asymmetry ,
retraction granting and nasal flaring must be determined in some healthy
infants , transient crackles may be auscultated during the first few hrs after birth
, unaccompanied by signs of respiratory distress . a normal pattern of periodic
breathing with pauses up to 10-15 seconds unaccompanied by bradycardia or
change in the color and tone may be observed .
c- Cardiac location is screened by determined that the heart sound s are loudest in
the left chest . soft systolic murmurs are commonly heard in the first 24 hours of
life , probably because of closing ductus arteriosus or normal changes in the
pulmonary vascular resistance . these murmur usually disappear within 48 hrs
after birth.
8
5-abdomen is convex and moves prominently with respiration .
a- A normal liver edge may be palpated 1-2 cm below the right costal margin ,
and the tip of the normal spleen may be palpated ate the left costal margin .
b- Because the most common abdominal masses in the newborn involve the
genitourinary tract , palpation of the kidneys is important . the kidney may
be palpated in the fingertips pressing deeply onto the lower lateral aspect of
the abdomen with opposite hand rested under the baby back at a level just
superior th the iliac crest .
6 - inguinal region and genitalia :
a- Femoral pulses must always be palpated because diminished pulse suggest
coaractation of aorta .
b- Male genitalia examination should include location of the urethral meatus ,
palpation of the testes and a for bulge in the groin or scrotum suggesting
hernia or hydrocele .
c- Female genitalia examination should a certain the presence of urethral and
vaginal opening as well as a normal sized clitoris to exclude ambiguous
genitalia , imperforated hymen and vaginal atresia . in normal infants a
transient swelling of the labia minora or a vaginal discharge that is mucoid or
bloody results from the influence of maternal hormones .
d- Anus is inspected for patency and placement .
7- Extremities temporary flexion contractures at the elbow , hips and knees are
seen in the term newborn as a result of intrauterine pressure effects
.approximately 5% of all newborn have more significant limb deformities
either deformities caused by positional abnormalities and intrauterine posture
or true malformation .
a- Developmental dysplasia of the hip (DDH) .occurs in 1 in 1000 live birth
and is much more common in girls and breech delivery .. asymmetry in
lower limb length , placement of the medial thigh and gluteal folds or
degree of hip flexion should raise suspicion for unilateral hip dislocation .
when the hips are flexed to 90 degrees the legs normally can be abducted
fully to touch the examining table " telescoping " of the femoral head with
subluxation ( barlow ) maneuver or a palpable " thump " with ortalani
maneuver suggest dislocation .
b- Erbs and klumpke palsy as a result of trauma to the brachial plexus result
in asymmetric or diminished arm movements .
8- Back .the spine is inspected and palpated for sinus tract or overlying lesions
such as lipomas , hairy tufts , or hemangiomas ,any of which may be signs of a
covert neural tube defect .
9- Neurological examination . overall state of consciousness and the ease with
which the infant makes transition from waking to sleeping or fussing to
calming as well as strength of cry should be noted .primitive primary reflexes ,
cranial nerves .

9
10- Gestational age . and appropriateness of size for gestational age .
a- Gestational age may be determined by assessing certain physical and
neurological characteristic that evolve in a predictable and progressive
fashion during the later part of gestation . finding are assigned numerical
values when compared to standard rating scales and summed totals are
correlated to specific gestational ages .
b- After determining gestational age , weight ,length , and head
circumference values are plotted on graphs that classified newborns
according to appropriateness of size for gestational age .
CARE OF THE NEWBORN .
A- Fluid and electrolyte requirements .
Water represents 94% of the fetal weight at three months of gestation. At term
,water content has decline to 80% of the birth weight of the newborn.
1- Fluid loss and replacement :
a- Fluid loss.
(1) During the first week of life , the extracellular fluid space contracts
,resulting in large reduction in body water . This water loos is
responsible for 5% of the weight loss observed in term infants .the
preterm infant may loss up to 10-15% of his birth weight .
(2) Water loss through evaporation from the skin and from expired air
is referred to as insensible water loss. Water loss through the urine
and stool is referred as sensible water loss .stool accounts for a
very small amount of sensible water loss .
b- Fluid replacement , is based on fluid loss and calculated as the sum of
insensible and sensible water loss. Initial parenteral fluid replacement
should be accomplished with a 10% of dextrose solution .
Fluid intake in term infants is usually begun at 60-70 ml/kg on day one
and increased to 100-120 ml/kg by days 2-3.smaller , more premature
infants may need to start with 70-80 ml /kg on day one and advance
gradually to 150 ml/kg .day .
c- Fluid balance is monitored by examining :
(1)- urine output .
(2)- change in body weight .
(3)- serum sodium concentration .
(4)- urine specific gravity .

10
2- Electrolyte loss and replacement :
a- Sodium , potassium and chloride , are the principle salts that are lost
through the urine and should be replaced accordingly .assuming an
adequate urine output , replacement is begun 24 hrs after birth at the
following rates:
(1)- sodium 1-3 mEq/kg/day .
(2)- potassium 1-2 mEq /kg/day .
(3)- chloride 1-3 mEq /kg /day .
b- Calcium .a decrease in serum calcium concentration frequently occurs
during the first week of life . serum calcium concentration below 7
mg/dl or below 3-3.5 mg/dl(ionized )bare considered hypocalcemia .
(1)- early neonatal hypocalemia . nearly all infants experience small
decline in tatal serum calcium during the first few days of life owing to intrauterine
parathyroid hormone suppression . early neonatal hypocalcemia rarely requires
treatment except in preterm , infant of diabetic mother and asphyxiated infants .
(2)- late neonatal hypocalcemia (non physiological )is seen at the end of
the first week of life , may be due to :
(a)- increased phosphate ingestion , as occur in infant whon are fed
cows milk .
(b)- hypomagnesemia .
( c)- hypoparathyroidisim .
(3)- therapy usually consists of calcium replacement with calcium
gluconate and treatment of underling cause of hypocalcemia .
( c )- other required mineral as phosphorus , magnesium , iron and trace
Metals .
b- Nutritional consideration . the composition of the nutritional solution
and the route of delivery depend on the gestational age , general
medical condition and possible special nutritional need of the newborn
a- Enteric nutrition .
(1)- Route of feeding :
(a)-the term infant can be breast- fed or bottle fed on demand
as long as attention is paid to intake and fluid balance .

11
(b)- the otherwise healthy preterm infant who is between 34-
38-wks should be fed every 3 hrs by breast bottle or gavage depend
on the infant strength and alertness .
( c)- the preterm infant who is less than34 wks does not have a
well coordinated suck and swallow reflex , and therefore should be
fed via a feeding tube . the feeding may be gastric bolus every 2-3
hrs except in infant weighting less than 1000 g .
(d)- continuous gastric or transpyloric feeding is employed in
the infant who weight less than 1000 g , because this infant has a
limited gastric volume and may experience intermittent
hypoglycemia and hypoxia when given bolus feedings .so trophic
feeding can be given at 10-20 ml/kg/day and the volume increased
accordingly .intravenous fluid are needed until feeding provide
approximately 120/kg/day .
(e)- continuous transpyloric feeding should be considered for
the infant who require an endotracheal tube and mechanical
ventilation to prevent gastric reflex and aspiration .
(2)- feeding solution .
The composition of the feeding solution depends on the
presence or absence of special protein , carbohydrate , or fat
requirements or intolerance which in turn depend on gestational
age , gastrointestinal motility status , and the possibility of
intestinal enzyme deficiencies or other metabolic disorders .
(a)- term infant who do not have complicating metabolic problem :
All of the water calorie , protein , and vitamin requirement of
the normal term infant are met by human milk or 20 kcal/oz cows
milk based formula .
The specific nutritional need of these infant for normal growth are
as follow:
(!) the normal term infant needs 100- 120 kcal/kg /day to meet
basal and growth requirement .
(!!) the infant also needs 2-3g/kg/day of protein for cellular growth
which represent approximately 10% of total daily calorie intake .
(!!!) in addition ,40% of the daily calorie requirement should be
derived from carbohydrates with remainder provided by dietary fat.
(b)- preterm infant :have decreased gastric motility and intestinal
lactase activity as well as increased calcium and phosphorus
requirement ,among other nutritional problems. The initial feeding
solution should be a dilute whey –based formula or human milk as
positive nitrogen balance is achieved , the infant may be advanced
to a formula that is high in calcium ,phosphorus and protein , or to
supplemented human milk .a 24kcal/oz formula is reserved for
infants whose water intake must be restricted and infants who can
not tolerate adequate feeding volumes .
12
( c)- infant with special metabolic needs . special formula solutions
are available for infant with selected intestinal enzyme deficiencies
( sucrase – isomaltase deficiencies ) or metabolic diseases (PKU) .
(3)- Vitamins and mineral . commercially available formula now are
fortified with vitamins ,minerals, and trace elements .therefore formula
fed term infants do not routinely require vitamins or mineral addition .
(a)- special vitamins need .
(i) infants who are fed human milk may receive a multiple –
vitamins supplement containing vit. A,D and C .
(ii) Owing to small body store and inadequate feeding
volumes , preterm infants should routinely receive a multiple –vitamin
supplement containing a the fat soluble vitamins ( A and D ) and the
water –soluble vitamins (B and C ). In addition , the preterm infant
who is less than 36 wks and should receive vitamin E to prevent
hemolytic anemia .
(b)- special mineral and trace element needs :
(i) Iron .all infant require iron supplementation ,which may be
obtained via iron –fortified formula or through a separate supplement .
iron supplement may be delayed in the preterm infant until enteric
feeding are tolerated . because of the increased bioavailability of iron
in human milk ,iron supplementation in term breast –fed infants may
wait the introduction of iron –fortified cereal at 4-6 months of age .
Folic acid also needed to be added for DNA and produce new cells .
( ii) fluoride .supplementation probably should not be given to
infant younger than 6 months of age , even when otherwise indicated ,
because the danger of fluorosis .
( iii) calcium and phosphorus . the needs of the growing term
infant are met by either commercial formula or human milk . owing to
rapid bone growth , the calcium and of phosphorus requirements of
the preterm infants are greater and necessitate special fortified formula
or supplementation if fed human milk .
b. Total parenteral nutrition .
preterm and other sick infants may required total parenteral nutrition
because of gastrointestinal disorders ( e.g. neonatal necrotizing enterocolitis ) as well
as nongastrointestinal disorders ( e.g.respiratory diseases , sepsis ) an intravenous
solution of dextrose , aminoacid , fat , vitamins ,and mineral can be administered by
either peripheral or central venous access . appropriately used ,total parentral nutrition
can provide adequate calories and protein to support the basal need and growth of the
sick infants .
13
C - Principles of drug therapy in neonate .
The administration and dosing of drug a are different in neonates
.disregarding this fact may result in toxicity or nontherapeutic use of drugs
.after administration of a drug , the effect and disposition depend on a number
of the following factors :
1- Route of administration, determines the peak drug level , how quickly the
peak level is reached ,and how long the peak drug level is sustained .
2- Solubility and PH determine the compatibility of drugs, tissue penetration
and excretion rate .
3- Protein binding .the plasma total protein and albumin level of the new born
are lower than the adult levels .
a- At similar total drug concentration , there will be , a larger unbound
drugs fraction for drugs with strong protein binding in the newborn
compared to the adult .because unbound fractionis the active ftaction in
the blood , lower total drug concentrations are needed to achieve a
therapeutic effect in the newborn .
b- Drug competition for albumin binding sites in the infant with
hyperbilirubinemia also poses a problem . if all the albumin binding
sites are occupied with bilirubin , there will be a larger free fraction of
drug in the blood . conversely , if the drug displaces bilirubin or is
already occupying the binding site, the increase in free bilirubin may
increase the risk of kernicterus .
4- Metabolism of the drugs by the liver : often is suboptimal because of low
levels of glucuronyl transferase . this often result in increase in plasma
drug level and excretion of unchanged drug compared to the adult.
5- Excretion of drugs by the kidney : often is impaired owing to low renal
blood flow , low glomerular filtiration rate ,and immature tubular function
Gestational age assessment :
Estimation of gestational age can be based on :
Menstrual period .
Date of conception .
Fetal ultrasonography .
Physical and neuromuscular criteria after birth ( ballard score ).
The ballard score is based on the neonate physical and
neuromuscular maturity and can be used up to 4 days after
birth .the neuromuscular component are more consistent over
time because the physical component mature quickly after
birth . however , the neuromuscular component can be affected
by illness and drugs.

14
The physical and neuromuscular score are added to calculate
gestational age .
Physical criteria include ( increasing firmness of the pina of the
ear ,size of the breast tissue , lanugo hair , creases of planter
surface and genitalia ) .
Neurological criteria include ( posture , squire window , arm
recoil ,popliteal angle , scarf signs and heal to ear ) .
Birth trauma
Birth injury refers to avoidable and unavoidable injury to the fetus during the birth .
Caput succedaneum
is a diffuse edematous often dark swelling of the soft tissue of
the scalp that extended across the midline and suture line ,and seen after prolong labor
in fullterm and premature infants .
Cephalhematoma
is a subperiosteal hemorrhage that does not cross the suture lines
and may associated with skull fractures . with time may organized and calcified , also
may cause jaundice , both caput and cephalhematoma not need treatment .
Retinal and subconjuctiveal hemorrhage
are common and not need treatment .
Brachial plexus
may result from excessive traction on the neck producing paresis or
complete paralysis .the simplest one Erb- duchenne paralysis involve the fifth and
sixth cervical nerves .the usual picture is is painless adduction , internal rotation of the
arm and moro reflex absent on affected side and the hand grasp is intact . Klumpke
paralysis is caused by injury to the seventh and eight cervical nerve and the first
thoracic nerve , if the sympathetic nerve are injured an epsilateral Horner syndrome (
ptosis ,miosis ) treatment of brachial injury is supportive and include positioning to
avoid contracture , active and passive exercise may be needed and nerve graft in
persist defect .
Facial nerve injury may be the result of compression of the seventh between the
facial bone and the mother pelvic bone or the physician forceps .this peripheral injury
is characterized by asymmetric crying face and the affected side is flaccid , the eye
does not close , the nasolabial fold is absent and the side of the mouth is dropped at
rest . if there is a central injury to the facial nerve , only the lower two third of the face
( not the forehead ) are involved .
skull fractures are rare are usually linear and require no treatment other than
observation for very rare delayed complications like leptomeningeal cyst .depressed
fractures may need elevation .
clavicle fracture is the most common fractures and usually is unilateral of course in
macrosomic infants after shoulder dystocia .decreased the movement and moro reflex
15
on the affected side . the prognosis is excellent and many infants require no
treatment.
Extremity fractures are less commonly than clavicle and involve humerus more than
the femur .the treatment involve immobilization and triangular splint pandage for the
humerus and traction suspension for the legs for femoral fractures .
Visceral trauma to the liver and spleen or adrenal gland occurs in macrosomoc
infants and in extremely premature infants with or without breech or vaginal
delivery.rupture of the liver with subcapsular hematoma formation may lead to
anemia and shock and DIC . infants with anemia and shock who are suspected to have
intraventricular hemorrhage but with normal head ultrasound examination should be
evaluated for hepatic or splenic rupture .infants with severe adrenal gland
hemorrhage may exhibit a flank mass , jaundice and hematuria with or without shock .
Certain procedures that can be done to the newborn :
1- Metabolic screen . before discharge a blood sample should be obtained from
every neonate for presence of congenital hypothyroidismand phenylketonuria.
In certain states screening also performed for other inborn error of metabolism
like ( galactosemia , cystic fibrosis . sickle cell anemia , maple syrup urine
disease homocystinuria , histidinemia ) .
2- Every newborn should receive a single dose of 0.5 -1 mg of natural vitamin K
within one hour of birth .
3- Prophylaxis of gonococcal ophthalmia either a 1% silver nitrate or 0,5
erythromycin .
4- Newborn circumcision has potential medical benefits and advantage with
disadvantage . benefit and risk should be carefully explained to the parents
a- Benefits :
Prevent inflammation of glans and prepuce .
Decrease the incidence of penile cancer at adult .
Reduce urinary tract infection .
b- Risk :
Local infection .
Bleeding .
Pain .
5- All newborn should be vaccinated with first dose of hepatitis vaccine .and if
the mother is hepatitis B surface antigen –positive should also receive a dose
of hepatitis B immunoglobulin as soon as possible after birth .
16
Problems in bonding between the sick infant and his parents :
Bonding :the process of psychological attachment of the parents to the newborn .the
following procedures are recommended to minimized the physical separation of the
infant from the parents and to encourage the formation of a strong bond .
1- Whenever possible , the mother should be transported to a tertiary care center
before delivery .
2- When the infant is transported to another hospital , the father should travel
immediately to the referral center so that he may keep close contact with the
infant and bring photographs and information back to the mother .
3- Visitation should be available 24 hrs a day .
4- A strong line of communication be established between the medical staff
( i.e .physician, nurse , social workers ) and the parents .
5- The parents should encourage to keep in contact by telephone when visitation
is difficult .
6- The parents suold be prepared regarding what to expect during their first visit
to the nursery ,and they should be made aware of any sudden change in the
infant condition .
7- Information should conveyed in a positive and truthful manner .
8- Psychological evaluation and support should be made available to parents who
are having a particularly difficult time coping with their sick infant or the
intensive care unit setting . parents groups often are helpful .
9- Plans for discharge should be made in advance and should include the parents
.having the parent stay overnight in the hospital before discharge can
significantly help them adapt to new roles that they will perform after they
leave the hospital . any current or future medical problems and follow-up
plans should be explained to the parents .

17
Prematurity :
Live infants delivered before 37 wks from the last day of the last menstrual period .
Low birth weight ( weight 2.5 kg or less ) due to prematurity or to poor intrauterine
growth or both .
Prematurity and IUGR are associated with increased neonatal morbidity and mortality
Very low birth weight infants weigh less than 1.5 kg .and predominantly premature .
Causes of prematurity
Fetal like ( multiple gestation , fetal distress , ).
Placental ( placenta previa , placental dysfunction ).
Uterine ( bicornuate uterus ) .
Maternal ( heart diseases , D .M . ,renal disease , maternal infection ).
Others like premature rupture of membrane ,trauma , polyhydramios .
A premature infant may show these signs soon after birth :
Trouble breathing .
Low weight .
Low body fat .
Inability to maintain a constant body temperature .
Less activity than normal .
Movement and coordination problems .
Complication of prematurity :
Brain hemorrhage .
Pulmonary hemorrhage .
Hypoglycemia .
Infection .
Anemia .
Patent ductus arteriosus .
Respiratory distress syndrome .
Long term outlook for premature infants include :
Hearing and speech problems .
Vision loss or blindness .
Learning disability .
Physical disability .
Delayed growth and poor coordination .
that interfere with the circulation and efficiency of the placenta , with
the development or growth of the fetus or with the general health and
nutrition of the mother .
18
Intrauterine growth restriction and small for gestational age :
IUGR represent a deviation from expected growth pattern . the decreased fetal growth
associated withIUGR is adaptation to unfavorable intrauterine conditions that result in
permanent alteration in metabolism , growth and development .
SGA describes an infant who birth weight is statistically less than 10
th
percentile or
two standard deviation below the mean birth weight for gestational age .
Causes of IUGR and SGA :
1- Maternal causes ( genetic short stature, infections , young age ,
smoking , poor nutrition black race , chronic diseases like diabetes)
2- Fetal congenital infection , defect in metabolism , multiple
gestation , chromosomal abnormalities ) .
3- Maternal medication ( antimetabollites , lead mercury , narcotics
steroid , warfarin ).
4- Placental and uterine ( abruption placentae , abnormal implantation
At birth infants who are mildly to moderately SGA appear smaller than normal with
decreased subcutaneous fat .
More severely affected may present with a wasted appearance with asymmetrical
findings including larger head for size of the body (central nervous system sparing )
widened anterior fontanelles , small abdomen thin arms and legs decreased
subcutaneous fat dry skin and meconium stained umbilical cord .
Physical examination should detail the presence of dysmorphic features like
abnormal extremities and hepatosplenomegaly . jaundice , skin rash and cataract that
may suggest the presence of congenital infection or metabolic defect .
Infants with severe IUGR or SGA may have problems at birth include respiratory
acidosis ,metabolic acidosis , asphyxia , hypotension , hypoglycemia , polycythemia ,
meconium aspiration syndrome .
Management of IUGR and SGA infants is usually symptomatic and supportive . the
diagnosis evaluation at birth should be directed the cause if possible . the mortality
rate are 5-20 times those of infants who are appropriate for gestational age . postnatal
growth and development depend on part on the etiology , the postnatal nutritional
intake and the social environment .infants who have IUGR and SGA secondary to
congenital infection , chromosomal abnormalities or constitutional syndromes remain
small throughout life . infants who have growth inhibited late in gestation because of
uterine constraints , placental insufficiency , or poor nutrition have cutch up growth
and approach their inherited growth and development potential under optimal
environmental conditions .
19
Post –term infants :
Post term infants are those born after 42 completed weeks of gestation regardless the
birth weight .
Clinical features may involve skin desquamation , long nail abundant hair ,pale skin
alert face , and loose skin meconium stained nails and umbilical cord .
Complication include ( perinatal depression . meconium aspiration . persistent
pulmonary hypertension , hypoglycemia , hypocalcemia , and polycythemia .
Large –for- gestational – age infants:
Infants with birth weight >the 90
th
percentile for gestational age are called large for
gestational age . neonatal mortality rate decrease with increasing birth weight until
approximately 4kg after which they increased . maternal diabetes , obesity and large
parental size are predisposing factors .infant have a higher incidence of birth trauma
like ( brachial plexus injuries, fractured clavicle cephalhematoma )
Increased risk of hypoglycemia and polycythemia , congenital anomalies ,
Multiple gestation :
Multiple gestation always should be seen as a high risk event owing to its increased
association with intra uterine accidents , growth abnormalities , prematurity and
problems at the time of delivery like abnormal position and asphyxia .
1-Incidence . approximately 1-1.3% of all live birth are the result of twin gestation .
the true incidence of twin gestation is probably is slightly higher . the monozygotic
twining rate is 3.5-4 in live births or 35-40 %of all twin who are born .
1- Etiology :
a-monozygotic twin : maybe viewed as a teratogenic event because
it occurs more frequently with increasing maternal age
.isassociated with more congenital malformation and can be caused
by teratogen . a problem of a symmetry in the developing embryo
20
may result in conjoined twins .the incidence of monozygotic twins
is unaffected by racial and familial factors .
b-dizygotic twinning :is caused by double ovulation , which may
be related to elevated gonadotropin .twin not of the same sex are
dizygotic . in twin of the same sex , zygosity should be determined and
recorded at birth through carefull examination of placenta .
c. incidence increase due to treatment of infertility with overian
stimulant and in vitro fertilization .
2- Prenatal problems :
a- Death : may be occur because of cord accidents and twin to
twin transfusion , which may lead to the death of one fetus ,
with thromboplastin release and subsequent DIC in the second
twin .
b- Growth disturbances are the rule :
(1)- IUGR there is a decrease potential for growth in twin
fetus compared to a single fetus ., probably owing to the
limitation of placental area for nutrient transfer .
(2)- twin to twin transfusion , resulting in a large polycythemic
twin and a small anemic twin .
c- the incidence of congenital malformation is doubled .
c- Increased spontaneous apportion .
d- Preterm delivery is the most common complication of multiple
gestation it occurs in up to 50% of twin pregnancies , the
incidence is even higher in triplet and quadruplet pregnancy .
e- Maternal complications include
Pregnancy induced hypertension .
Polyhydramnios .
Hyperemesis and nausea .
Anemia .
3- Postnatal problems include :
1. Prematurity and its complications.
2. Growth retardation.
3. Perinatal asphyxia .especially of the second twin because the
placenta may be separated after birthof the first twin . and in
instances of malpresentation or vasa previa may result in long
term morbidity and mortality .
4- Management is aimed at :
a- Identifying multiple gestation as early as possible .
b- Managing other medical problems .
c- Controlling preterm labor .
d- Identifying ideal route of delivery .
e- Avoiding asphyxia in the second twin
21
Maternal diseases affecting the newborn
1- Idiopathic thrombocytopenia ITP : ITP is immune process in which
antibodies are directed against platelets that cross the placenta and cause
thrombocytopenia in the fetus and newborn , that increase the risk of
intracranial hemorrhage .close maternal and fetal management is vital . infants
with hemorrhage may need platelets transfusion or intravenous
immunoglobulin .the condition usually resolve within 4-6 wks .
2- Systemic lupus erythematosus SLE : immune abnormalities in SLE can lead
to the production of antibodies that can cross the placenta and injure fetal
tissues and the most serious problems in fetus is damage to the cardiac
conducting system which result in congenital heart block . neonatal lupus may
occur and is characterized by skin lesion thrombocyropenia , autoimmune
hemolysis and hepatic involvement . the mortality rate is about 2o% and most
surviving infants require pacing .
3- Neonatal hyperthyroidism : is due to the transplacental passage of thyroid –
stimulating antibodies , hyperthyroidism can appear rapidly within the 12 to
48 hrs . symptoms may include IUGR prematurity , goiter exophthalmos ,
stare , craniosynostosis . flushing, congestive heart failure tachycardia
,arrhythmia , hypertension , hypoglycemia , thrombocytopenia and
hepatosplenomegaly .treatment include propylthiouracil , iodine drops and
propranolol .the condition usually resolve in 2-4 months .
4- Antiphospholipid syndrome: is associated with throbophilia and recurrent
pregnancy loss . antiphspholipid antibodies are found in 2-5% of the general
healthy population . obstetric complications arise from the prothrombotic
effects of theantiphospholipid antibodies on the placental function .
vasculopathy ,infarction, and thrombosis have been identified in the mothers
with antiphospholipid syndrome that manifested by fetal growth impairment ,
placental insufficiency , maternal preeclampsia and premature birth .
5- Diabetes mellitus :
22
RESPIRATORY TRACT DISORDERS
Respiratory disorders are the most frequent cause of admission for neonatal intensive
care in both term and preterm infants . signs and symptoms of respiratory distress
include cyanosis , grunting , nasal flaring retraction, tachypnea , decreased breath
sounds with or without rales and pallor .
The first breath :
Initiation of the first breath is caused by a decline in Pao2 and PH and a rise in Paco2
as a result of interruption of the placental circulation , a redistribution of cardiac
output , a decrease in body temperature and various tactile and sensory inputs .
Hyaline membrane disease (respiratory distress syndrome of newborn )
Is a respiratory disorder that primarily affects preterm infants who are born before the
biochemical maturation of their lungs .
Biochemical development : the most important prenatalevent is the production of
surfactant by type II alveolar cells .
The major function of surfactant is to decrease alveolar surface tension and
increasing lung compliance . surfactant prevent alveolar collapse at the end of
expiration and allows for opening of the alveoli at a low intra-thoracic pressure . the
ratio of lecithin to sphingomyelin in the aminiotic fluid is areflection of the amount of
intrapulmonary surfactant and lung maturity .an L/S ratio of 2:1 or greater usually
indicates biochemical lung maturity .
Surfactant increase by ( steroid administration , prolonged membrane rupture
,preeclampsia , placental insufficiency , thyroide hormone , theophyline ).
Surfactant decreased by ( maternal diabetes , acute asphyxia ) .
1- Pathophysiology . the lungs are poorly compliant owing to deficiency of
surfactant resulting in classic complex of progressive atelectasis ,
intrapulmonary shunting , hypoxemia ,and cyanosis .the hyaline membrane
that forms and lines the alevioli is composed of protein and sloughed
23
epithelium – the result of oxygen exposure , alveolar capillary leakage and the
forces generated by the mechanical ventilation of these infants .
2- Clinical features: affected infants characteristically present with tachypnea ,
grunting , nasal flaring , chest retraction ,and cyanosis , in first three hours of
life . there is decrease air entry on auscultation .apnea and irregular respiration
are ominous sign requiring immediate action .respiratory failure may occur in
severe course
3- Clinical course : the natural course is a progressive worsening over the first
48- 72 hrs of life .
(a) After the initial insult to the airway lining , the epithelium is repopulated
with type II alveolar cells .
(b) Subsequently , there is increase production and release of surfactant , so
that there are sufficient quantities in the air spaces by 72 hrs of life .this
result in improvement in lung compliance and resolution of the respiratory
distress .
4- Diagnosis :is confirmed by a chest radiograph that reveals a uniform ground-
glass pattern and an air bronchogram that is consistent with a deffuse
atelectasis , clinical manifestation and gas analysis .
RDS should be differentiated from ( early onset sepsis , pneumonia , cyanotic
heart diseases , aspiration syndromes , spontaneous pneumothorax , transient
tachypenia of newborn .) .
5- Therapy and prognosis :
a- Conventional therapy for the affected premature infant include supportive
care as well as the administration of oxygen . it also necessary to increase
the main airway pressure by use of continuous positive airway pressure ,
intermittent assisted ventilation , or a high frequency oscillation . outcome
with conventional therapy is good .
b- Exogenous surfactant replacement therapy with artificial or bovine
surfactant has become an important intervention for those infants with
severe surfactant deficiency . alveolar opening and improvement in
oxygenation and ventilation occur almost immediately .
6- Prevention . when amniotic fluid assessment reveals fetal lung immaturity
and preterm delivery can not be prevented , administration of corticosteroid to
the mother 48 hrs before delivery can induce or accelerate the production of
fetal lung surfactant .
7- Complications :common complications and associated findings include
pneumothorax , patent ductus arteriosus , intraventricular hemorrhage ,
necrotizing enterocolitis , bronchopulmonary dysplasia and retinopathy of
prematurity .
24
Transient tachypnea of newborn :
Is thought to result from decreased lymphatic absorption of fetal lung fluid
It most commonly occurs in the infant born near term by cesarean section
,without preceding labor ( the catecholamine surge associated with labor and
delivery which is thought to enhance pulmonary lymphatic drainage does not
occur in this setting )
(1)-
clinical features
. the tachypnea is quiet or mild and usually not associated
with retraction . the infant appears comfortable and rarely cyanotic .
(2
)- diagnosis :
is based on the delivery and chest radiograph ,which
characterized by fluid in the major fissure , prominent vascular marking ,
increased interstitial markings and hyperinflation . auscultation may
reveal rales .
(3)-
therapy
is supportive . the tachypnea resolves in a few days .low doses of
supplemental oxygen may be required .
persistent of the fetal circulation( persistent pulmonary hypertension ).
Usually a disease of term infants who are experience acute or chronic in utero
hypoxia .it is seen frequently in infant with meconium aspiration syndrome .
(1) Pathophysiology . the primary abnormality is a failure of the pulmonary
vascular resistance to fall with postnatal lung expansion and oxygenation .
(a) Normally at birth the systemic vascular resistance rises as a result of
cessation of blood flow through the placenta , and pulmonary vascular
resistance falls with the first breath .
(b) With persistence of the fetal circulation , the pulmonary vascular
resistant continues to be high and may in fact be higher than the
systemic resistance .this result in shunting of the deoxygenated blood
which is returning to the right side of the heart away from the lungs.
The right to left shunt can occur at both the atrial level(foramen of
ovale ) and through the ductus arteriosus .because the lung are
bypassed the blood is not oxygenated and hypoxemia ensues.
(2) Clinical features . these infants have rapidly progressive cyanosis
associated with mild to severe respiratory distress . there is a varied
response to oxygen administration depending on the size of the shunt .
(3) Diagnosis :
(a) The diagnosis is suggested by a history of perinatal asphyxia and
clinical cyanosis at birth combined with a negative cardiovascular
examination and negative chest radiograph , although parenchymal
disease may coexist ( MAS,RDS ) .
(b) Echocardiography should be used to establish the diagnosis and should
demonstrate :
(!) the absence of cyanotic heart disease .
(!!) an increased pulmonary vascular resistance .
25
(!!!) the presence of right to left shunt at the foramen of ovale ductus
arteriosus , or both .
(4) Therapy : include supplemental oxygen , mechanical ventilation ,
hyperventilation ,support of systemic blood pressure and administration of
sodium bicarbonate and pulmonary vasodilators .
(5) Prognosis : the overall mortality rate associated with this disease is high
.extra-corporeal membrane oxygenation may improve the outcome .
Apnea
Apnea is cessation of breathing for longer than 20 seconds . apnea often occurs in
preterm infants ( apnea of prematurity ) and reflect immaturity of the respiratory
control mechanism in the brain stem .
(1)- clinical features ,bradycardia ( HR less than 80beats/min ) often associated with
apnea .apnea of prematurity is characterized by periodic breathing and intermittent
hypoxia , which further diminish respiratory derive .
(2)- diagnosis . of apnea of prematurity is made after excluding other reason for the
apnea like :
Respiratory ( pneumonia , airway obstruction, hypoxia , pneumothorax ).
CNS ( intracranial hemorrhage , seizure , drugs ,hypoxic injury ).
Infections ( sepsis , meningitis ).
Metabolic ( hypoglycemia , hypocalcemia , decrease or increase sodium ,
hypothermia ).
Cardiovascular ( heart failure , hypotension , ).
Gasrtointestinal ( necrotizing enterocolitis , ).
(3)- therapy : therapy of apnea of prematurity include one of ht efollowing :
a- tactile stimulation
b--maintain body temperature .
c- supplemental oxygen .
d- administration of respiratory stimulant ( theophyline , caffeine )
e- use continuous positive air way or intermittent assisted ventilation ) .
f- treatment of underling cause .
prognosis : apnea of prematurity dose not alter prognosis unlees it severe ,
recurrent and refractory to therapy ).
26
Choanal atresia
: is a unilateral or bilateral obstructionof the posterior
nasal airway by a membrane or bony septum .this life threatening anomaly
result from failure of the bucconasal mucosa to rupture .
Clinical features : because most newborn are obligate nose breathers ,
bilateral atresia usually presents in the delivery room as airway obstruction ,
apnea and cyanosis .distressed neonate then cry which relieve the cyanosis .
unilateral obstruction may be asymptomatic .
Diagnosis : is confirmed either by inability to pass a suction catheter through
the nostril into the oropharynx or by radiography using radioopaque dye to
show the area of nasal obstruction .
Therapy : emergency management consists of establishing an airway either
with an oral airway or by endotracheal intubation . definitive therapy is
surgical reconstruction performing in neonatal period .
Diaphragmatic hernia :
Diaphragmatic hernia is a displacement of the abdominal content into the
thoracic cavity through a defect in the diaphragm .
Types :
(a) hernias through the foramen of bochdalek are by far the most commonly
seen diaphragmatic hernia . the defect , which almost always is on the left
occurs in the posteriolateral portion of the diaphragm . it results from
failure of the pleuroperitoneal canal to close , which normally occurs
between 6-8 wks gestation.
(b) Herians through the foramen of morgagni are somewhat rare , the hernia
usually on the right .frequently the hernia contain only omentum and the
affected newborn is asymptomatic .
Pathophysiology : ipsilateral pulmonary hypoplasia results from
compression of the affected lung by the displaced gastrointestinal organs
a shift of the mediastinal structures resulting in compression of the
contralateral lung may cause hypoplasia of the lung to a lesser degree .
Diagnosis : is confirmed by a chest radiograph demonstrating air-filled
bowel in the hemithorax .
Therapy : includes intubation , vigorous oxygenation and mechanical
ventilation , decompression of the intestinal tract with a nasogastric tube ,
27
correction of metabolic acidosis , and surgical removal of the abdominal
contents from the thorax with repair of the hernia .
(a) Mask and bag ventilation should be avoided or minimized because it
results in distension of the bowel and further compromises the
pulmonary function of the affected newborn .
(b) Pulmonary hypertension frequently complicates the preoperative and
postoperative course .
(c) Extracorporeal membrane oxygenation may be helpful in selected
infants .
Prognosis : survival rates depend on the degree of the lung hypoplasia
and the presence of other anomalies ,symptoms before 24 hrs of age ,
herniation to the contralateral lung and need for ECMO . with
conventional therapy , survival rates are approximately 67% , however
the use of extracorporeal membrane oxygenation may improve
survival .
Meconium aspiration syndrome (MAS)
MAS is a multiorgan disorder with perinatal asphyxia as the
underlying cause . it is most commonly occurs in post term infants and
in infants who are small for gestational age due to intrauterine growth
retardation . both have placental insufficiency as a common for fetal
hypoxia .
(1) Pathophysiology . the fetal hypoxia triggers via a vagal reflex ,
the passage of thick meconium into the amniotic fluid .the
contaminated amniotic fluid is swallowed into the oropharynx and
aspirated at birth with the initiation of breathing . with severe fetal
asphyxia and acidosis , the meconium may be aspirated prenatally
because of fetal gasping .other organ affected by the perinatal
hypoxia include the brain ,heart gastrointestinal tract and kidneys .
(2) Diagnosis : is established by the presence of mecomium in the
tracheal or amniotic fluid combined with symptoms of respiratory
distress and a chest radiograph that reveals a pattern of diffuse
infiltrate with hyperinflation .
(3) Therapy : because most episodes of aspiration occur with the
initiation of respiration , the most effective therapy is prevention .
this consist of removal of the meconium before the initiation of
ventilation . the meconium is removed from the infant airway as
follows:
The oropharynx is suctioned before both delivery of the thorax
and initiation of breathing ,and again when the infant is on the
warmer bed .
28
The vocal cords are visualized using a laryngoscope , and a
large endotracheal tube or DeLee catheter is inserted .
Direct wall-unit suction is applied to the tube or catheter as it is
removed . this procedure is repeated if significant meconium is
removed . only after the trachea is cleared of any meconium
should spontaneous or artificial ventilation be initiated .
If aspiration has occurred and the infant is in distress , therapy
consists of administration of oxygen and mechanical
ventilation .
Persistent pulmonary hypertension also may coexist and should
be vigorously treated .
Pneumothorax :
Pneumothorax is presence of free air in the pleural space . the air often is under
pressure and in this setting is referred to as tension pneumothorax .
(1) Incidence and etiology . asymptomatic , spontaneous pneumothorax occurs in
1-2% of otherwise healthy newborn at birth . symptomatic pneumothorax
more commonly occurs in the infant who is receiving mechanical ventilation
or who has underling lung disease ( RDS, MAS) .
(2) Clinical manifestations . symptoms and signs include cyanosis , tachypnea
,and elevation of the affected hemithorax . auscultation reveals diminished
breath sounds on the affected side .
(3) Diagnosis :
(a) The diagnosis made by a chest radiograph that demonstrate a dense
partially collapsed lung surrounded by a large area of radiolucent air
within the hemithotax . depending on the degree of tension and lung
compliance , the mediastinal structures are shifted toward the opposite side
of the chest .
(b) Transillumination of the thorax may aid in the diagnosis of the
pneumothrax in the emergencies , positive evidence is the transmission of
light through the affected side .
(4) Therapy :varies with the severity of the symptoms .
(a) If no other lung disease exists and there is minimal respiratory distress ,
supplemental 100% oxygen ( nitrogen wash out technique ) for several
hours usually is sufficient .
(b) If a significant degree of tension , respiratory distress ,or some other lung
disease exist the air should be evacuated by aspiration with a syringe and
needle or by a chest tube if a continuous air leak exists .

29
Digestive system disorders
Neonatal necrotizing enterocolitis ( NEC ) : refers to a spectrum of varying degrees of
acute intestinal necrosis usually following injury of the bowel with secondary
invasion and devitalization of the bowel wall .
1- Incidence . this is a serious and common problem affecting 1-5% of all
newborn admitted to the intensive care units . affected infants most commonly
are premature near 90% , asphyxiated and suffering from other medical
problems . necrotizing enterocolitis rarely observed in a healthy term infants
and less common in in infants fed human milk .
2- Etiology and pathogenesis :
(a) Bowel ischemia secondary to preceding perinatal asphyxia generally is
regarded as the cause of bowel wall injury . the introduction of formula or
human milk then provides the substrate for bacterial overgrowth . bacterial
invasion of thr bowel wall often with gas production ( pneumatosis
intestinalis ), leads to tissues necrosis and perforation .
(b) Other predisposing factors includes :
(1) Systemic hypotension .
(2) Patent ductus arteriosus .
(3) Placement of au umbilical artery catheter .
(4) Exchange transfusion .
(5) Previous treatment with systemic antibiotics .
(6) Use of hyperosmolar formula .
(7) Rapid advancement of the feeding volume .
3- Clinical features and diagnosis : signs and symptoms are usually are noted
during the first 2 wks of life , shortly after enteric feeding has begun :
Gastric residuum which often is bile stain .
Abdominal distension .
Blood in stool .
Lethargy and apnea .
Poor perfusion with hypotension or shock .
Abdominal wall discoloration .
Unstable temperature and metabolic acidosis .
4- Laboratory findings :
(1) Suggestive on blood film leukocytosis , neutropenia or thrombocytopenia.
(2) Suggestive findings on abdominal radiography include :
(a) Dilated thickened bowel loops .
(b) Pneumatosis intestinalis which usually starts in the right lower part .
(c) Perforation , with free abdominal air and portal vein air .
30
5--Clinical course :two distinct clinical patters are noted :
a- Most infants follow a course characterized by feeding intolerance ,
abdominal distension occult blood in the stool , and dilated bpwel loops on
radiography . these finding improve rapidly with therapy .
b- The other group of infants has severe progressive symptoms including
groos blood in the stool , extreme abdominal tenderness , hypotension
disseminated intravascular coagulation and sepsis . peumatosis intestinalis
and perforation frequently occur in this setting .
6- Therapy :
a- Treatment should begin with discontinuation of enteric feeding , gastric
drainage and administration of intravenous fluid .
b- Once culture have been taken ,systemic antibiotics ( e.g. ampicillin
,gentamicin ) shloud be given .also any accompanying disorders (e.g. DIC)
should be treated .
c- Surgical resection of the necrotic bowel segment is indicated for infants
who have a progressive downhill course and for those in whom intestinal
perforation has occurred .
7- Prognosis : the mortality rate associated with necrotizing enterocolitis which
is highest in the most premature infants is approximately 30% .later
complications may include intestinal strictures and short bowel syndrome ..
Anemia of the newborn
Neonatal hemoglobin concentration at birth about 16.5-18 g/dl. After birth
hemoglobin decline to 11-12 g/dl at 3-6 months at term . premature infant has
a lower hemoglobin concentration to achieves a nadir at 1-2 months after birth
.fetal hemoglobin represent 60- 90 %of hemoglobin at term birth and the level
decline to adult level by 4 months of age . for term infant blood volume is 70-
90 ml/kg and a preterm infant ,blood volume is 90-100 ml/kg .
The physiological anemia noted at 2-3 months of age in term infant and at 1-2
months of age in preterm infants , is a normal process that does not result in
signs of illness and does not require any treatment . it is a physiological
condition believed to be related to several factors including increased tissue
oxygenation experience at birth , shortened RBC life span and low
erythropoietin levels .
Etiology : symptomatic anemia in the newborn period may be caused by
decreased RBC production ,increased RBC destruction or blood loss ..

31
Hemolytic disease of the newborn ( erythroblastosis fetalis ) .
Result from blood group incompatibility between the mother and the fetus .
hemolysis occurs when maternal antibodies to a particular blood group antigen
cross the placenta and bind to fetal red blood cells , which are then destroyed
in the spleen .
ABO blood group incompatibility : with neonatal hemolysis develops only if
the mother has IgG antibodies from a previous exposure to A or B antigens
.these IgG antibodies cross the placenta by active transport and affect the
fetus or newborn . sensitization of the mother to fetal antigens may have
occurred by previous transfusion or by condition of pregnancy that result in
transfer of fetal erythrocyte into maternal circulation such as first trimester
abortion , ectobic pregnancy amniocentesis , or normal pregnancy .
ABO incompatibility with sensitization usually does not cause fetal disease
other than mild anemia . it may produce hemolytic disease of newborn ,
however which is manifested as significant anemia and jaundice . because
many mother who have blood group O have antibodies to A and B before
pregnancy , the first born infant of A or B type may be affected . in contrast to
RH disease , ABO hemolytic disease dose not become mre severe with
subsequent pregnancies .hemolysis with ABO incompatibility is a less severe
than hemolysis in RH-sensitized pregnancy , either because the anti A or anti
B antibody may bind to non erythrocytic cells that contain A or B antigen or
because fetal erythrocyte have a fewer A or B antigenic determinants than they
have RH sites . with declining incidence of RH hemolytic disease , ABO
incompatibility has become the most common cause of neonatal jaundice
requiring therapy .
Erythroblastosis fetalis :
Erythroblastosis fetalis classically is caused by Rh blood groip
incompatibility . most RH negative mother have no anti-Rh antibodies at the
time of their first pregnancy . in most Rh-sensitized cases ,the D antigen of the
fetus sensitized the Rh negative mother resulting in IgG antibody production
during the first pregnancy . because most mothers are not sensitized to Rh
antigen at the start of pregnancy . Rh erythroblastosis fetalis is uaually a
disease of second and subsequent pregnancies .the first affected pregnancy
results in an antibody response in the mother which may be detected during
antenatal screening with coombs test and determined to be ant-D antibody .
The first affected newborn may show no serious fetal disease and may
manifest hemolytic disease of the newborn only by development of anemia
and jaundice . subsequent pregnancies result in an increasing severity of
response because of an earlier onset of hemolysis in utero . fetal anemia , heart
failure elevated venous pressure , portal vein obstruction and

32
hypoalbuminemia result in fetal hydrops, which is characterized by ascites ,
pleural and pericardial effusion and anasarca .the risk of fetal death is high .
If the fetus near term can be delivered and treated in neonatal intensive care
unit . if the fetus less than 33 wks and immature lung intrauterine transfusion
O-negative blood into the umbilical vein is indicated and may have to be
repeated until pulmonary maturity is reached
Prevention : of sensitization of the mother carrying an Rh –positive fetus is
possible by treating the mother during gestation ( more than 28 wks
gestational age and within 72 hrs after birth with anti-Rh-positive immune
globulin . the dose (300ug) is base on the ability of this amount ao antiRh-
positive antibody to bind all the possible fetal Rh positive erythrocytes
entering the maternal circulation during the fetal –to-maternal transfusion at
birth ( approximately 30 ml).
Diagnosis and management :
Hemolysis in utero result in hydrops with ( ansarca ,heart failure,and
pulmonary odema that result in asphyxia , hepatosplenomegaly ,pallor and
become jaundice within 24 hrs after birth . patients with ABO incompatibility
often are asymptomatic and show no physical signs at birth , mild anemia with
jaundice develops during the first 24-72 hrs of life .
Newborn with acute blood loss due to( feto-maternal hemorrhage , placenta
previa ,or internal hemorrhage ) is characterized by pallor , diminished
peripheral pulses ,and shock but no hepatosplenomegaly .
Newborn with chronic blood loss caused by ( chronic fetal-maternal
hemorrhage , twin to twin transfusion ) present with marked pallor , heart
failure hepatosplenomegaly with or without hydrops with low HB at birth and
decreased serum iron store . shock is more typical in patient with internal
hemorrhage whereas in hemolytic diseases heart failure may br seen with
severe anemia .
Laboratory evaluation :
A complete blood count , blood smear , reticulocyte count , blood type and
direct coombs test (to determined the presence of antibody coated RBCs)
should be performed in the initial evaluation of all infants with hemolysis .
RBC enzymes , hemoglobin electrophoresis and RBC membrane tests .
The diagnosis of fetal- maternal hemorrhage is confirmed by the Kleihauer –
Betke acid elusion test .
Internal hemorrhage or when nonimmune hemolysis is suspected ,ultrasound
of liver brain spleen or adrenal gland may be indicated .
The treatment of symptomatic neonatal anemia is transfusion of cross
matched packed RBCs .if immune hemolysis is present ,the cells to be
transfused must be cross matched against maternal and neonatal plasma .
Acute volume loss may need non blood products such as saline if blood not
available .
To correct anemia 10-15 ml/kg of packed RBCs can be given

33
Neonatal hyperbilirubinemia
Neonatal hyperbilirubinemia is a condition characterized by an excessive
concentration of bilirubin in the blood .there are two types of neonatal
hyperbilirubinemia ( unconjugated ) which can be physiological or pathologic
in origin and (conjugated ) which always stems from pathologic cause . both
types may lead to jaundice . neurotoxic concentration of unconjugated
bilirubin can cause kernicterus .
1- Normal bilirubin metabolism : bilirubin is a bile pigment formed from the
degradation of heme that is mainly derived from red blood cell destruction
75% but also from ineffective red blood cell production 25% .
Bilirubin is poroduced by the catabolism of hemoglobin in the reticuloendotheelial
system . the tetrapyrole ring of the heme is cleaved by heme oxygenase to form
equivalent quantities of biliverdin and carbine monoxide . biliverdin is converted to
bilirubin by bilivedin reductase . one gram of hemoglobin produce 35 mg of bilirubin
compared with adult newborn have two to three fold greater rate of bilirubin
production (6-10 mg/kg/day vs.3mg/kg/day ) this increased production is caused in
part by increased RBC mass and short half life of erythrocyte 70-90 days compared to
120 days in adult .Bilirubin produced after hemoglobin catabolism is lipid soluble and
unconjugated and react as un indirect reagent in the van den bergh test .indirect –
reacting unconjugated bilirubin is toxic to the central nervous system and is insoluble
in water ,limiting its excretion . unconjugated bilirubin binds to albumin on specific
bilirubin binding sites , one gram of albumin binds 8.5 mg of bilirubin in the newborn
.if the binding sites become saturated or if a competitive compound binds at the site
displacing bound protein , free bilirubin becomes available to enter the central
nervous system .organic acids and and drugs like sulfisoxazole can displace bilirubin
from its binding sites on albumin .Bilirubin dissociates from albumin at the
hepatocyte and become bound to a cytoplamic liver protein Y ligandin . hepatic
conjugation result in the production of bilirubin diglucuronide , which is water suloble
and capable of biliary and renal excretion . the enzyme glucuronosyl transferase
represents the rate – limiting step off bilirubin conjugation . the concentration of
ligandin and glucuronosyl transferase are lower in newborn particularly in premature
than in older children .Conjugated bilirubin gives a direct reaction in the van den
bergh test . most conjugated bilirubin is excreted through the bile into the small bowel
and eliminated in the stool .some bilirubin may undergo hydrolysis back to the
unconjugated fraction by intestinal glucuronidase , however and may be reabsorbed
(enterohepatic recirculation ) . in addition , bacteria in the neonatal intestine covert
bilirubin to urobilinogen and stercobilinogen which are excreted in urine and stool
and usually limit bilirubin reabsorbtion . delayed passage of meconium which contain
bilirubin , also may contribute to the enterohepatic recirculation of bilirubin .maternal
indirect hyperbiliruninemia also may increase fetal bilirubin level .
34
Physiological jaundice :
Physiological jaundice is a common cause of hyperbilirubinemia among newborn it
is a diagnosis of exclusion made after careful evaluation has ruled out more serious
causes of jaundice such as hemolysis , infection and metabolic diseases .
Physiological jaundice as opposed to pathological jaundice is characterized by :
(1) Clinical jaundice appearing after first day .
(2) An increase in the total serum bilirubin concentration of less than 5mg/dl/day
(3) A total serm bilirubin concentration of less than 13 mg/dl in term and less than
15mg/dl in preterm and direct bilirubin of less than 1.5-2 mg/dl .
(4) Persistence of clinical jaundice for less than one week .
Pathological jaundice :
Jaundice and underling hyperbilirubinemia are considered pathological if the time of
appearance ,duration ,or pattern varies rom that of physiological jaundice .the greatest
risk associated with indirect hyperbilirubinemia is the development of bilirubin
induced neurological toxicity which typically occurs with high indirect bilirubin
levels , the development of kernicterus depends on :
1- Level of indirect bilirubin .
2- Duration of exposure to bilirubin elevation .
3- The cause of jaundice .
The infants well-being .
specific causes of nonphysiological indirect hyperbilirubinemia include :
(i) – hemolytic diseases of immune etiology .(fetomaternal blood group
incompatibilities RH and ABO as well as non immune like spherocytosis ,
hemoglobenopathies red blood cell enzyme deficiency .
(ii)- extravascular blood loss and accumulation ( cephalhematoma ) .
(iii)- increased enterohepatic circulation due to intestinal obstruction .
(iv)- breast feeding associated with poor intake .
( v)- disorder of bilirubin metabolism like Gilpert syndrome and Crigler-Najjar
syndrome.
(vi) – metabolic disorder like hypothyroidism .
35
Jaundice associated with breast –feeding :
Significant elevation in indirect bilirubin (breast milk jaundice ) develops in term
infants after the seven day with maximum concentration as high as 10-30 mg/dl
reached during the 2
nd
-3
rd
wk .and may persist for 3-10 wk at a lower level if the
breast feeding discontinued for one or two days the serum level fall rapidly. although
uncommon kernicterus can occur .the cause of breast milk jaundice is unclear but may
be due to glucuronidase in some breast milk .
The late jaundice associated with breast feeding should be distinguished from early
onset known as breast feeding jaundice which occur in the 1
st
wk and may be a result
of decreased milk intake or dehydration .
Crigler –najjar syndrome :
Is a serious rare autosomal recessive , permanent deficiency of
glucuronosyltransferase that result in severe indirect jaundice . type ll respond to
enzyme induction by Phenobarbital producing elevted enzyme and reduce bilirubin
.type l does not respond to Phenobarbital and manifest as persist indirect jaundice
often leeding to kirnicterus in absence of hemolysis .
Gilbert disease : is caused by a mutation of the promoter region of
glucuronosyltransferase and result in mild indirect jaundice and usually occur after
puberty and not need treatment .
Causes of jaundice in the first wks ( physiological jaundice , ABO and Rh –
incompatibility , concealed hemorrhage , congenital infection , sepsis ,breast feeding
jaundice , Crigler –Najjar syndrome ,urinary tract infection , polycythemia ) .
Causes of jaundice after first wks ( beast milk jaundice , septicemia , bile duct atresia ,
hepatitis , galactosemia , hypothyroidisim , CF ,inborn error of metabolism ) .

36
Kernicterus ;
Kernicterus is a severe neurological condition associated with very high levels of
unconjucated bilirubin in the blood . kernicterus is characterized by yellow staining of
the basal ganglia and hippocampus ,which is accompanied by wide spread of cerebral
dysfunction .
(a) Causes . kernicterus occurs when free bilirubin crosses the blood brain barrier
and enter the brain cell .
(i)- normally unconjugated bilirubin is bound tightly to albumin which prevent
bilirubin from crossing the blood brain barrier .free bilirubin exists when ths
amount of unconjugated bilirubin exeeds the binding capacity of albumin.
(ii)- bilirubin also may enter the brain at a low concentration owing toe
displacement from the albumin binding site by another compound ( e.g. sulfa
drugs). Which lead to increased free bilirubin concentration or because of
disruption of the blood brain barrier by sepsis , asphyxia , acidosis , or
infusion of hyperosmolar solutions .
(b) Kernicterus causes a complex of neurologic symptoms including the earliest
clinical manifestation as lethargy ,hypotonia , irritability poor moro response
and poor feeding . later signs include bulging fontanelle , opisthotonic
posturing , pulmonary hemorrhage ,fever and seizure .
Infants with severe cases of kernicterus die in the neonatal period , survived
infants may developed nerve deafness . choreosthetoid cerebral palsy , mental
retardation and discoloration of the teeth .
Kernicterus can be prevented by avoiding high indirect bilirubin levels and
avoiding condition and drugs that may displace bilirubin from albumin .
Early signs occasionally may be reversed by immediately exchange
transfusion .
Treatment of jaundice :
Regardless the cause the goal of therapy is to prevent neurotoxicity related to indirect
–reacting bilirubin .
(1)--Phototherapy : is an effective and safe method for reducing indirect bilirubin
particularly when initiated before serum bilirubin increased to levels associated with
kernicterus . in term infants phototherapy is begun when indirect levels are between
16- 18 mg/dl . in premature infants when bilirubin is at lower levels . blue and white
lights are effective in reducing bilirubin levels .
Phototherapy causes a photochemical reaction producing the reversible , more water
soluble isomers of indirect bilirubin this isomr can be excreted bypassing the liver
conjugation system or excreted in urine .

37
Because phototherapy may require 6-12 hrs to have a measurable effect it must be
started at bilirubin level below those indicated for exchange transfusion . the
therapeutic effect of phototherapy depend on :
Light energy and effective wavelength 425-to475 nm wavelength .
The distance between the light and infant 15-20 cm .
The surface area of exposed skin .
Rate of hemolysis and metabolisim and excretion of bilirubin .
Complications of phototherapy include :
Increased insensible water loss and dehydration .
Macular –papular skin rash .
Lethargy and masking of cyanosis .
Nasal obstruction by eye pads and potential retinal damage .
Loose stool .
Bronze baby syndrome in infants with direct jaundice .
(2)- intravenous immunoglobulin in jaundice caused by isoimmune hemolyric disease
and can be used if phototherapy not effective and bilirubin approaching exchange
level .
(3)- metalloporphyrins a single i.m dose on the first day of life may reduce the need
for subsequent phototherapy . the proposed mechanism is competitive enzymatic
inhibition of the rate – limiting conversion of heme protein to biliverdin .
(4)- exchange transfusion : is used principally in hemolytic disease or when the
bilirubin concentration is very high . this procedure directly remove the bilirubin from
the intravascular space . unbound antibodies that initiate the hemolytic process and
affected red blood cell also are removed beside correction of anemia .
Exchange transfusion usually is performed when the serum bilirubin concentration is
20 mg/dl or more . the specific bilirubin concentration that requires treatment varies
with gestational age , the cause of jaundice and the presence of medical complications
(e.g. sepsis , acidosis ).
As the rule of thumb alevel of 20 mg/dl for bilirubinnis te exchange number for
infantwith hemolysis who weigh more than 2000g .asymptomatic infant with
physiological or breast milk jaundice may not require exchange transfusion unless
indirect bilirubin level exceed 25 mg/dl .the exchangeable level of bilirubin for other
infants may be estimated by calculating 10% of birth weight in grams , so the level in
an infants weighing 1500g would be 15mgdl .

38
The exchange transfusion is usually performed umbilical catheter in vein to a distance
no greater than 7 cm in a full term .the exchange should be carried out over 45-60
min.with aspiration of 20 ml of infant blood alternating with infusion of 20 ml of
donor blood , 5-10 ml may be indicated in sick or premature infants .
1- Rh hemolytic disease of the newborn need O Rh negative RBCs do not have
major blood group antigen so they are not memolysed by maternal antibodies
that may still be present in the infants circulation .if RBC are made available
before delivery of the sensitized infant the RBCs must be O Rh negative and
cross matched against the mother . if the RBCs are sourced after delivery the
RBCs must be cross matched against infant .
2- ABO incompatibility : use group O , Rh specific RBCs . these RBCs
contained low levels of antibodies and lack antigens that could trigger any
circulating maternal antibodies in th newborn .
Estimated double volume to be exchange :
Term/preterm=85ml x 2 x weight(kg)= 170 ml x weight (kg) .
The infants stomach should be emptied before transfusion to prevent aspiration and
body temperature should be maintained and vital signs monitored .
After exchange transfusion the bilirubin level must be determined at frequent intervals
every 4-8 hrs because bilirubin may rebound within hrs as a result of continued
hemolysis and redistribution of bilirubin from tissue store .
Acute complications include ( transient bradicardia , cyanosis ., transient vasospasim ,
thrombosis , apnea , infections necrotizing enterocolitis , vessel perforation or
hemorrhage , metabolic instability ).
Late complications ( late anemia GVH reaction , inspissated bile syndrome , portal
vein thrombosis ) .
39
Conjugated or direct hyperbilirubinemia
Direct jaundice defined as direct bilirubin level > 2mgdl or > 20% of the total
bilirubin is never physiological . direct bilirubin is not neurotoxic to the infant but
signifies a serious underling disorder involving cholestasis or hepatocellular injury .
Causes of direct jaundice :
1- TORCH infection ( toxoplasmosis ,rubella,cytomegalovirus ,herpes simplex)
2- Metabolic disorders ( e.g. galactosemia ).
3- Bacterial sepsis .
4- Obstructive jaundice ( e.g. biliary atresia ) .
5- Prolonged administration of intravenous protein solution .
6- Neonatal hepatitis , alpha one antitrypsin deficiency , cystic fibrosis .
7- Inspissated bile from prolonged hemolysis .
diagnosis : is based on conjugated fraction of the bilirubin level and ( liver enzymes
,bacterial and viral culture , metabolic screen , hepatic ultrasound sweet chloride and
possible liver biopsy ) .
therapy : is directed to the underlying cause of direct jaundice .
Hydrops fetalis :
I s a condition that develops I utero , usually as a result of chronic anemia due to
hemolytic disease ,although many etiologies exist and its chief features include
anemia or anasarca and hypoptoteinemia with heart failure .
1- Etiology :
a- Severe chronic anemia due to ( isoimmunizationdue to Rh and ABO
incompatibility ) ,homozygous alph thalasemia , twin to twin transfusion .
b- Cardiac ( structural defect , paroxysmal aterial tachycardia ) .
c- Hypoproteinnemia .
d- Intrauterine infection including syphilis , toxoplasmosis and CMV ) .
e- Chromosomal disorders ( e.g. turner syndrome ) .
2- Pathophysiology :
The exact pathophysiology is unknown , but the central factor in the
development of the hydrops fetalis appears to be severe chronic anemia with
loss of oxygen-carrying capacity , leading to hypoxia and acidosis . a
controlling factor is hypoproteinemia , which together with anemia causes the
development of congestive heart failure , edema , pleural effusion and ascites
.all of these problems contribute to the respiratory distress seen at birth .
3- Clinical features :
a- Signs and symptoms include ( congestive heart failre,pallor, pleural
effusion.periphral edema and hepatosplenomegaly ).
b- Laboratory findings include ( anemia,hypoprotenemia,hypoxia.acodosis ) .
40
4- Therapy : is aimed at correcting the anemia and treating the cogntive heart
failure and respiratory distress .in addition appropriate treatment should be
provided for associated etiologies .idiopathic causes of hydrops are associated
with a high mortality rate .
Polycythemia :
Polycythemia occurs in 2-5% of all newborn and is defined as a hematocrit
of 65% or greater when a freely following blood sample is taken from a large
vein . hyperviscosity of the blood almost always exists in associated with
polycythemia .
a- Etiology. Polycythemia has been associated with the following conditions
:
1- Fetoplacental transfusion associated with birth asphyxia or delayed
cord clamping .
2- Twin to twin transfusion .
3- Chronic intrauterine hypoxia secondary to placental insufficiency (e.g.
pregnancy induced hypertension with fetal growth retardation or
increased fetal metabolism ( e.g. with maternal diabetes ) .
4- Endocrine disorder ( e.g. hyperthyroidism ) .
5- Genetic disorder ( e.g. down syndrome , Beckwith –Wiedeman syn.) .
b- Pathophysiology :
1- Many of the problems associated with polycythemia were originally
thought to be caused by organ ischemia and hypoxia secondary to an
increase in blood viscosity . it is now known that most of the blood
flow reduction is the result of an increased oxygen content in the
arterial blood .this reciprocal relationship of decreased blood flow and
increased arterial oxygen content result in a normal or increased
delivery of oxygen to most organs .
2- Therefore , most of the problems associated with polycythemia are
more likely the result of the perinatal events ( i.e. acute or chronic
hypoxia ) that also are responsible for the development of the
polycythemia , rather than any flow disturbance attributable to the
polycythemia itself .
c- Clinical features :
1- Symptoms and signs include :
a- Tachypnea and cyanosis and feeding intolerance .
b- Jitterness and seizure .
c- Renal dysfunction .
d- Hypoglycemia ,thrombocythemia .
e- Necrotizing enterocolitis .
2- Complications .polycythemia is associated with an abnormal long term
neurologic outcome .
41
d- Therapy : generally is supportive .reduction of the hematocrit by partial
exchange transfusion may be helpful in alleviating distress , renal
dysfunction and hypoglycemia , but may increase the risk of necrotizing
enterocolitis .
The equation used in partial exchange is :
Volume of exchange (ml) = blood volume x ( observed – desired
hematocrit ) /observed hematocrit .
The desired hematocrit is 50% and the blood .
Hemorrhagic disease of the newborn
Have the most profound deficiency of vitamin K-dependent factors ( VII,X,V and
II ) and these factors decline further after birth , because breast milk is a poor source
of vit. K , breastfed infants are at increased risk for hemorrhage that usually occurs
between day three and seven of life . bleeding usually ensues from the umbilical cord
, circumcision site ,intestine , scalp , mucosa , and skin but internal hemorrhage places
the infant at risk for fatal complications such as intracranial hemorrhage .
Hemorrhage on the first day of life resulting from the deficiency of the vitamin K
dependent factors often is associated with administration to the mother of drugs that
affect vitamin K metabolism in the infant . this early pattern of hemorrhage has been
seen withmaternal warfarin and antibiotics ( e.g.isoniazid or rifampicin ) therapy and
in infants of mothers receiving Phenobarbital and phenytoin . bleeding also may occur
1to 3 months after birth particularly among breastfed infant .vitaminK deficiency in
breastfed infant also should raise suspicion about the possibility of vitamin K
malabsorption resulting from cystic fibrosis , biliary atresia , hepatitis or antibiotics
suppression of the colonic bacteria that produce vitamin K .
Levels of PIVKA ( protein induced by vitamin K absence ) increased in vitamin K
deficiency and are helpful diagnostic marker, vitamin K administration rapidly
correct the coagulation defects ( normalizes prothrombin time which is depend on
vitamin K ) and reducing PIVKA to undetectable levels .the bleeding time which
reflect platelet function and number is a normal during newborn period .
Prevention and treatment :
Bleeding associated with vitamin K deficiency may be prevented by administration
of vitamin K to all infants at birth . before routine administration of vtamin K 1-2% of
all newborn have hemorrhagic disease of newborn .
One intramuscular dose ( 1 mg) of vitamin K prevents bleeding .
Treatment of bleeding resulting from vitamin K deficiency involves intravenous
administration of 1-5 mg of vitamin K . if severe life threatening hemorrhage is
present fresh frozen plasma also should be given . unusually high doses of vitamin K
may be needed for hepatic disease and for maternal warfarin or anticovulsant therapy .
42
Neurological disorders
Hypoxic –ischemic encephalopathy (HIE ) :
Condition known to reduced uteroplacental blood flow or to interfere with
spontaneous active respiration after complete birth lead to perinatal hypoxia , to lactic
acidosis and if severe enough to reduce cardiac output or cause cardiac arrest to
ischemia . the combination of the reduced availability of oxygen for the brain
resulting from hypoxia and the diminished or absent blood flow to the brain resulting
from ischemia leads to reduced glucose for metabolism and to accumulation of lactate
that produces local tissue acidosis . after reperfusion hypoxic-ischemic injury also
may be complicated by cell necrosis and vascular endothelial edema , reducing blood
flow distal to the involved vessels .typically hypoxic –ischemic encephalopathy in the
term infant is characterized by cerebral edema , cortical necrosis , and involvement of
basal ganglia , whereas in the preterm it characterized by periventricular
leukomalacia . both lesions may result in cortical atrophy , mental retardation and
spastic quadriplegia or diplegia .
Perinatal risk factors and conditions associated with birth asphyxia : ( extremes in
maternal age i.e.<20 yrs or > 35 yrs , placental abruption or previa , preeclampsia ,
preterm gestation , meconium stain ameniotic fluid feat bradycardia , malpresentation
, multiple gestation and maternal diabetes ).
Postnatal symptoms of asphyxia :
a- Brain :
1- Mild asphyxia .the infants initially well be depressed . this followed by a
period of hyperalertness which resolves within 1 or 2 days . there are no
focal signs and the prognosis is excellent for a normal outcome .
2- Moderate asphyxia . the infants will be very depressed . this is followed by
a prolonged period of hyperalertness and hyperreflexia . generalized
seizure often occur hours after the episode of asphyxia but are controlled
easily , resolving in a few days regardless the therapy . the prognosis is
variable , negative result on EEG are predictive of normal outcome .
3- Severe asphyxia .is associated with coma , intractable seizure , cerebral
edema and intracranial hemorrhage . the infant becomes progressively
more depressed over the first 1-3 days , as rhe cerebral edema develops
and death may occurs during this period . survival usually is associated
with a poor long term outcome .also the prognosis depend on other organ
injury and low apgar score especially if the score remains low by 20 min .
b- Heart . severe or prolonged episodes of asphyxia may result in hypoxic –
cardiomyopathy . signs and symptoms include hypotension, poor myocardial
contractility , cardiomegaly and congestive heart failure .
43
c- Lung . respiratory distress and a need for oxygen can occur owing to a delay
fall in pulmonary vascular resistance .
d- Kidney . depressed renal blood flow during the aspyxial events causes acute
tubular necrosis . this is usually self limiting .
e- GIT is associated with poor GIT motility or ileus . the hypoxia also predispose
to secondary bacterial invasion and to the development NEC .
f- Blood . hypoxia depressed bone marrow function and initiates intravascular
coagulopathy which result in thrombocytopenia prolonged PT and PTT and
clinical evidence of bleeding .
Diagnosis : MRI is the preferred imaging modality in neonates with HIE . CT
scan are helpful in identified focal hemorrhage lesion ,diffuse cortical injury
later on and damage to basal ganglia .ultrasonography it is the initial preferred
modality in preterm infant not in term .EEG may help to determined which
infants are at highest risk for long term brain injury .
Therapy :
1- General principles . the primary objective in treating perinatal asphyxia is
to restore oxygen supply to the body tissues , especially the brain . this
require ventilation with oxygen and ensuring adequate cardiac output . the
secondary objective is to evaluate the degree of hypoxic injury and to plan
treatment . whole body hypothermia or selective reduce mortality or major
neurodevelopmental impairment in term infants with HIE .phenobarbital is
the drug of choice for seizure . phenytoin and lorazepam may be needed
for refractory seizures . monitoring of blood pressure, hemodynamic
status , acid –base balance , hypoglycemia and possible infection is vital .
2- Specific therapy . specific delivery room resuscitation procedures .
And anticipate the conditions associated with asphyxia and treat if present.
44
Intracranial hemorrhage :
1- Subarachnoid hemorrhage: may occur after a normal or traumatic
delivery . bleeding is self limited and symptoms like irritability and
seizure resolves in a few days .the infant may be asymptomatic .
2- Subdural hemorrhage: also is seen with birth trauma . a significant
amount of blood can accumulate and cause focal neurological deficits
owing to pressure exerted on the brain . however drainage is necessary
only if symptoms are severe or do not resolve .
3- Intraventricular hemorrhage : is seen almost exclusively in preterm
infant and is the result of bleeding of the germinal matrix , frequently
after asphyxial insult .the hemorrhage occur in the first three days of
life . the clinical manifestation of IVH include seizures, apnea ,
bradycardia , lethargy ,coma , hypotension , metabolic acidosis ,
anemia not corrected by blood transfusion , bulging fontanelle and
cutaneous mottling .
Infants with small hemorrhage (grade 1 or 2 ) are asymptomatic ,
infants with larger hemorrhage ( grade 4) often have catastrophic event
that rapidly progress to shock and coma .
The diagnosis of IVH is confirmed and the severity graded by
ultrasound or CT examination through the anterior fontanelle :
Grade 1 IVH is confined to the germinal matrix .
Grade 2 blood noted in ventricle without ventricular dilation .
Grade 3 extension of grade 2 with ventricular dilation .
Grade 4 blood in dilated ventricle and in cerebral cortex .
Grade 4 hemorrhage has a poor prognosis as does the development of
periventricular , small echolucent cystic lesion with or without porencephalic cysts
and posthemorrahgic hydrocephalus . the cysts may correspond to the development of
periventricular leukomalacia which may be a precursor to cerebral palsy .
Treatment : treatment of acute hemorrhage involves standard supportive care
including ventilation for apnea and blood transfusion for shock . post hemorrhagic
hydrocephalus may be managed with serial daily lumber puncture ,external
ventrculostomy tube or a permanent ventricular –peritoneal shunt .implantation of the
shunt often is delayed because of the high protein content of the hemorrhagic
ventricular fluid .

45
Neonatal seizures :
Are not uncommon in the neonatal period subtle seizures which manifest as rhythmic
eye deviation or blinking lip smacking tongue thrusting , fluctuation of vital signs or
apnea are the most common form followed by generalized tonic , multifocal clonic ,
focal clonic and myoclonic seizures .
Seizures may be difficult to differentiate from benign jitteriness or from
tremulousness in infants of diabetes mother , in infants with narcotic withdrawal .in
contrast to seizures , jitteriness and tremors are sensory dependent elicited by stimuli
and interrupted by holding the extremity . seizure activity becomes manifested as
coarse , fast and slow clonic activity , whereas jitteriness is characterized by fine rapid
movement . seizures may be associated with abnormal eye movement .
Etiology :
1- Asphyxia .
2- Brain anomalies .
3- Intracranial hemorrhage
4- Systemic metabolic disorders ( hypoglycemia , hyponatremia ,hypernatremia ,
hypocalcemia ,hyperammonemia ) and inborn error of amino acid and organic
acid metabolism .
5- Meningitis and encephalitis .
6- Pyridoxine deficiency .
Diagnosis : the following evaluation should be made in effort to pin point the cause of
the seizure activity :
1- Neurological examination .
2- EEG .
3- Ultrasound and CT scanning
4- Screening for metabolic disorders involving ( glucose , calcium , or sodium )
for inborn error of metabolism ( amino acid s or organic acid .
5- Lumbar puncture and evaluation of the SCF for sepsis .
Treatment :
The treatment of neonatal seizures may be specific such as treatment of meningitis
or the correction of hypoglycemia , hypocalcemia , hypomagnesemia , hyponatremia
or vitamin B6 deficiency or dependency . in the absence of identifiable cause , therapy
shloud involve anticonvulsant agent such as ( 20-40 mg/kg of phenobarbital ) (10-20
mg/kg of phenytion ) or ( 0.1-0.3 mg/kg of diazepam ) followed by one of the two
longer acting drugs . the long term outcome for neonatal seizure usually is related to
the underlying cause and to the primary pathology such as hypoxic- ischemic
encephalopathy , meningitis , drug withdrawal , stroke or hemorrhage .

46
Neonatal hypoglycemia :
Neonatal hypoglycemia is defined as a plasma glucose concentration less than 35
mg/dl during the first 24 hrs and lees than 45 mg/dl thereafter . hypoglycemia is very
common in infants of diabetes mother as well as in infants who are born after various
perinatal complication , including prematurity , IUGR , and asphyxia .
1- Pathogenesis . the pathogenesis varies depending on the clinical setting and
the associated conditions affecting the infants .
a- Maternal diabetes , the hypoglycemia in infants of diabetes is the result of
a hyperinsulinemia state that persist after the umbilical cord is cut and the
maternal supply of glucose is interrupted .
b- Prematurity . preterm infants become hypoglycemia owing to diminished
glycogen store and to immaturity of gluconeogenic enzymes .
c- Growth retardation . growth retarded infants frequently are depleted of
hepatic glycogen and quickly become hypoglycemic .
d- Perinatal asphyxia . forces the fetus to use anaerobic metabolism , which
quickly depletes stored glycogen and result in hypoglycemia.
e- Cold stress . increased oxygen consumption as well as glucose
consumption . it also may increase free acids and result in hypoglycemia .
f- Sepsis. May cause hypoglycemia , although hyperglycemia also is
observed which presumably is caused by insulin insensitivity .
g- Beckwith-Wiedmann syndrome . is characterized by hypoglycemia ,
visceromegaly , macroglossia and omphalocele . hyperinsulinemia
secondary to pancreatic islet cell hyperplasia is responsible for
hypoglycemia .
h- Nesidioblastosis and pancreatic islet cell adenoma are associated with
hyperinsulinemia and hypoglycemia .
i- Metabolic disorder such as galactosemia and panhypopituitarism .
Clinical features :
Infants with hypoglycemia are not always symptomatic . however the following
symptoms may occur ( hypotonia or jitteriness , apnea or tachypnea, cyanosis
,hypothermia , poor feeding and seizures .
Therapy :
a- Primary therapy is intravenous glucose . the glucose infusion may be required
for several days until the basal insulin secretion rate decreases , glycogen
stores are replenished or gluconeogenesis improves . bolus infusion of
hypertonic glucose should be avoided because they may result in a rebound
hypoglycemia .intravenous glucose should be administered as a constant
47
infusion begun at a rate of 6-8mg/kg/min .this may be increased to a rate of up
to 20mg/kg/min ( a central venous access should be used for infusion given at
a rate above 15 mg/kg/min .
A small ( 0.5-1.0 g/kg ) bolus may be used for extreme hypoglycemia or if
severe symptoms related to hypoglycemia . this shloud always be followed by
a constant infusion .
b- Hypoglycemia that is secondary to hyperinsulinemia and resistant to
intravenous glucose should be treated with corticosteroid or diazoxide . if drug
treatment fails partial pancreatectomy should be performed . these more
aggressive forms of therapy rarely are necessary except for hypoglycemia that
associated with Beckwith-Wiedmann syndrome , nesidioblastosis , or islet cell
adenoma .
Infant of diabetic mother
Women with diabetes in pregnancy are at increased risk for adverse pregnancy
outcome . adequate glycemic control before and during pregnancy is crucial to
improving outcome .
The effect of diabetes on the fetus depend in part on severity of the diabetes state , age
of onset of diabetes , duration of treatment with insulin and presence of vascular
disease .poorly control maternal diabetes leads to maternal and fetal hyperglycemia
that stimulates the fetal pancreas , resulting in hyperplasia of the islets of Langehans
.fetal hyperinsulinemia results in increased fat and protein synthesis and fetal
macrosomia except brain and ossification centers .
Hypoglycemia develops in about 25-50% of of infants of diabetic mother and 15-25%
of infants of mothers with gestational diabetes . infants should initiate feeding within
1 hour after birth and a screen glucose test should be performed within 30 mint. Of
the first fed. In asymptomatic infants treatment indicated if plasma glucose less than
30mg/dl . in symptomatic infants the treatment indicated if plasma glucose less than
40% . treatment of hypoglycemia as mention above .
Neonatal problems of diabetic mother :
1- Birth asphyxia and birth trauma due to macrosomia .
2- Hypoglycemia , hypocalcemia , hypomagnecia .
3- Polycythemia and indirect jaundice .
4- Congenital anomalies is increased 3-folds like congenital heart disease .
5- Neurological disorders like neural tube defect and holoprosencephaly .
6- Renal disorders likes renal agenesis ,double ureter , renal vein thrombosis .
48
7- Respiratory likes RDS due low surfactant synthesis and TTN .
8- Preterm labor is common and the result of fetal distress or a planed early
delivery .
Prognosis :
The neonatal mortality rate is > 5 times that of infants of non diabetic mother
.the subsequent incidence of diabetes mellitus in infants of diabetic mother is a
higher than that in general population .
The key to optimal outcome is consistent euglycemia in the mother .
Neonatal hypocalcemia :
Hypocalcemia is a common in sick and premature newborn . total serum
calcium levels less than 6 mg/dl and ionized calcium levels of lees than 3 to
3.5 mg/dl are considered hypocalcemia .
Early onset neonatal hypocalcemia occurs in the first 3 days of life and is
often asymptomatic and can result from transient hypoparathyroidism or
congenital absence of the parathyroid gland and DiGeorge syndrome .
Hypomagnesemia ( < 1.5 mg/dl ) may be seen with hypocacemia that may
need to treat both conditions .
Late onset neonatal hypocalcemia or neonatal tetany often is the result of
high phosphate containing milk or the inability to excrete the usual
phosphorus in commercial infant formula . vitamin D deficiency and
malabsorption also can be associated with late onset hypocalcemia .
The clinical manifestations of hypocalcemia include ( apnea , muscle
twitching seizures , laryngospasm .
Chevostek sign and Trousseau sign can be see more with late onset
hypocalcemia .
Neonatal hypocalcemia may be prevented by administration of IV or oral
supplement at a rate of 25 to 75 mg /kg /day .
Early asymptomatic hypocalcemai of preterm infants and infants of diabetic
mother often resolved spontaneously .
Symptomatic hypocalcemia should be treated with 2- 4 ml /kg of 10% calcium
gluconate given intravenously and slowely over 10 to 15 minutes followed by
a continous infusion of 75 mg/kg/day of elemental calcium .
If hypomagnesemia is associated with hypocalcemia , 50% magnesium sulfate
0.1 ml/kg should be given by IM and repeated every 8 to 12 hrs .
The treatment of late hypocalcemia include immediate management as in early
hypocalcemia plus the initiation of feeding with low phosphate formula .
49
Infection
Infection continues to be a major cause of neonatal mortality and morbidity despite
advance in therapy . although perinatally acquired bacterial infections are the most
common infections that are acquired in utero remain important source of long term
disability .
General consideration :
a- Predisposing factors . the newborn is particularly susceptible to infection
owing to immaturity of immune system mechanism including
Neutrophil chemotaxis .
Neurtophil phagocytosis .
Bacterial activity .
Humeral components.
b- Timing and route of infection . the causative organism and abnormalities
associated with neonatal infection vary with time and route of infection .
1- Organisim responsible for transplacental infections before birth are ( CMV
, HIV , Rubella virus , toxoplasma gondi , echovirus and listeria
monocytogenes ) .and can cause abnormalities associated with infection
acquired in the first trimester ( congenital malformation , IUGR ,
microcephaly , hydrocephalus and still birth ) and also can cause
abnormalities with infection acquired later in pregnancy ( microcephaly ,
hydropes fetalis , DIC , anemia , IVH , hepatosplenomegaly , jaundice ,
skin and eye lesions beside still birth ) .
2- Perinatal infection include infections acquired through the fetal membrane
ascending infections acquired after rupture of membrane and infection
acquired via the birth canal . common causative organisims are ( Group B
Beta-hemolytic streptococcus , E-coli . Klebsiella species , streptococcus
pneumoniae Herpes simplex virus, Chlamydia trochomatis , neisseria
gonorrhoeae , neisseria meningitidis ) .and can cause the following
abnormalities ( respiratory distress , temperature instability , septic shock ,
neuropenia , thrombocytopenia , meningitis ) .
3- Postnatal infections most often are required as a result of nosocomial or
community exposure . hospitalized newborns who are premature or require
instrumentation are particularly susceptible . common causative organisms
are ( staphylococcus aureus , staphylococcus epidermidis , pseudomonas
aeruginosa , candida albicans , E –coli , klebsiella,clostridia,
enterococcus)and associated abnormalities are ( respiratory distress ,
feeding intolerance , apnea, anemia shock , DIC , hypoglycemia and
temperature instability )

50
2- Bacterial infection and neonatal sepsis . bacterial infection most frequently
are acquired via the birth canal or nosocomialy . the infection almost always is
bacteremic and associated with systemic symptoms – a condition referred to as
neonatal infection .
a- Incidence . neonatal sepsis is common in premature infants . about 1-4%
of these infants have at least one episode of sepsis during their
hospitalization . sepsis in term infants are rare , occurring in less than 1% .
b- Risk factors for early neonatal sepsis include :
1- Premature labor .
2- Low birth weight .
3- Prolonged rupture of the fetal membrane .
4- Chorioamnionitis .
5- Maternal fever .
c- Etiology . . the most common causative organisims include :
1- Gram-positive cocci especially group B Beta –hemolytic streptococci ,
but also staphylococcus aureus and staphylococcus epidermidis .
2- Gram- negative rods especially E-coli and klebsiella pneumoniae .
3- Gram-positive rods like listeria monocytogenes .
d- features :
1- Signs and symptoms of bacterial infections include :
Unexplained respiratory distress .
Unexplained feeding intolerance .
Temperature instability .
Hypoglycemia and hyperglycemia .
Apnea , lethargy or irritability .
2- Laboratory findings include :
a- Abnormal white blood cell count ,including neutropenia or un
elevated ratio of immature to total neutrophil suggest sepsis .
b- Prolonged of PT and PTT .
c- Tracheal aspirate , gastric aspirate for neutrophil count , gram stain
and culture .
d- Blood culture .
e- A lumber puncture .
f- Urine for general exam and culture .
g- Chest radiograph ,
h- Arterial blood gas analysis .
51
Therapy :
1-Empiric antibiotics therapy should begin after the diagnostic work up and consist of
a broad –spectrum penicillin ( usually ampicillin ) and un aminoglycoside ( usually
gentamicin ) . once culture data available . therapy should be tailored to the specific
organism .
2-The initial choice of antibiotics for nosocomial infection depend on nursery .
community and individual patient exposure information.
3-The duration of therapy usually is 7-10 days except for invasive infections ( e.g.
meningitis , osteomyelitis ) which require longer course of antibiotics therapy
4-Other complication can be treated accordingly for example treatment of shock with
fluid and vasopressor .
1- Monitoring serum drug level .
Persistent signs of infections despite antibacterial treatment suggest
candidal or viral sepsis .
Best regard

52
