
Cervical cancer
Ass.Prof. Dr. Alaa AL.Naser
Objectives:
1.revise the anatomy of the cervix, blood supply,
lymphatic's.
2. understand epidemiology and pathology of disease.
3. know optimum pre-treatment assessment, how to
manage surgically and non-surgically.
4. recognize suspicious cervical lesions, and take
appropriate biopsies.
5. Be able to counsel patients with regard to Dx., Mx.,
Prognosis.
Cervix (2.5 cm long, internal os connects to uterus,
external os connect to vagina.
Cervix have 2 parts: supra vaginal part(anteriorly is
bladder, post. Is the rctouterine pouch). Other part is
vaginal part.
Blood supply(uterine arteries branches of internal
iliac arteries, vaginal arteries which is branches of
uterine arteries anastomosis with pudendal arteries)
Venous( via uterine venous plexus to internal iliac
veins)

Lymphatic's(external iliac node, internal iliac, sacral
node &superficial inguinal node)
Epidemiology
cervical cancer is one of the most common cancers in
women worldwide. It is the third most common cancer in
women, nearly all invasive squamous cell carcinoma are
preceded by persistent HPV infection & CIN and vast
improvement in screening dramatically lowered the
incidence of invasive disease in developed countries, yet
in developing countries remain the most lethal
malignancy in women
.
It tends to occur in middle life. Most cases in woman younger
than 50. It rarely in women younger than 20. 15% of cases of
cervical cancer are fond in women over 65.
Risk
1. Demographic risk, high in Hispanic followed by
African-American group, Asians and Pacific Islanders.
2. HPV infection is the primary etiologic infectious agent
99%. High risk type cancer of cervix, vulva, vulva and
vagina. 2/3 cause by HPV 16,18.
3. Lower socioeconomic predictor's low education, women
do not have easy access to adequate health services
including pap smear.
4. Being younger than 17 at first full term pregnancy 2
times more than who wait for 25.

5. Cigarette smoking, chemicals and harmful substance are
absorbed through blood stream, smoker twice risk than
nonsmoker. Tobacco by-products found in the cervical
mucus of women who smoke damage the DNA of cervix
cells and also makes the immune system less effective in
frightening HPV infections(genotoxicity secondary to the
presence of tobacco-derived carcinogen in cervical
mucus).
5. Reproductive behavior parity women who had 3 or
more full term pregnancies have increased risk =
unprotected coitus, low immunity, secondary to trauma.
6. COC long term use of birth control pills increased risk
for cervical cancer and risk return back after stopping and
to normal risk after 10 year sopping.
7. Being overweight more likely to develop
adenocarcinoma.
8. Diet low in fruits and vegetables increased risk.
9. Chlamydial infection increases risk persistent HPV
infection& invasive disease.
10. Having a weakened immune system either diseases
HIV that weakened the immunity correlate with level of
CD4 lymphocyte. And immune suppressive drugs.
11. DES (hormonal medication used in the past to prevent
miscarriage, women of the mothers receive DES develop
clear cell adenocarcinoma of cervix and vagina. And
squamous cell carcinoma of cervix.
12. Having family history of cervical cancer if mother or
sister have cervical cancer chance 2-3 times higher than if
no one in family, may be familial tendency (but not
genetically inheritance)
13. Sexual activity increase no. of sexual partner, early age
of sexual intercourse.

Pathophysiology
The malignant transformation of cervical cells is
intimately related to HPV infection, which infects basal
keratinocytes and replicates during keratinocytes
differentiation.(DNA virus), have regulatory early E and
late L genomic regions. E protein required for replication
and or cellular transformation, these include E6,E7.
E6 bind to E6-AP which associate with tumor suppressor
protein P53 cause rapid degradation. Loss of P53 result in
failure of growth arrest and loss of apoptotic signal in
response to cell damage.
E7 interacts with retinoblastoma tumor suppressor gene
pRb, E7-pRb initiate cell growth. Both E6, E7 result in
aggressive cervical cancer.
Tumor spread
1.The most common mothed for spread is via direct
extension to adjacent tissue include parametria ,vagina
,pelvic side wall and bladder and rectum. Less common
metastasise to ovaries.
2. Lymph node spread Para cervical, parametrial, ureteric,
obturator, internal, external, common iliac L.N.
2. Lymph vascular space involvement as ca. invade deeper
into stromal, it enters blood capillaries and lymphatic
channels, so less commonly by hematogenous spread lung,
bone, liver, mediastinum, spleen, adrenal and brain.
3. Blood borne spread is unusual.

Histological types
Squamous cell carcinoma: majority of cervical cancer, it
develop after an interval of preinvasive disease, it k.k by
increased N/C ratio, prominent mitotic figure CIN
progress to CIS with subsequent invasive disease after
penetration to basement membrane.
Grossly: range from small nodular lesion to large friable
easily to bled. It spread by direct extension.
Adenocarcinoma (most other cervical cancer which
develop from mucous secreting gland of endocervix)
Grossly the ectocervix appear normal, but cervix expand
(barrel-shaped cervix).
Mixed cervical carcinomas (adenosquamous carcinoma
Diagnosis
Symptoms
A large portion of women dx. With cervical ca. may be
asymptomatic. Diagnosed after evaluation of abnormal pap
smear.
For those with symptom early stage ca.create watery
vaginal discharge, may contain blood ,between period and
after menopause. with tumor growth and necrosis
malodorous vaginal discharge.
intermittent vaginal bleeding that follow coitus or
douching, as tumor enlarge patient may present with
uncontrolled bleeding.
Pain during sex.
Extension to pelvic side wall, compress adjacent organs to
produce symptom like lower extremities edema, low
backache radiating to posterior leg, often radiating sciatic
nerve root, lymphatic's, veins or ureter, ureteral

obstruction , hydronephrosis and uremia, occasionally ca.
invade bladder and rectum presented with vesico vaginal
or rectovaginal fistula. Hematuria , bleeding per rectum.
Physical examination
Most women with cervical cancer finding is cervical lesion
which should be biopsied.
Cervical cancer clinically staged and examination is
critical for treatment planning. For this reason exam
include detailed description of size (depth, width),
rectovaginal exam to detect paramerium and pelvic side
wall extension.
With advance disease enlarge supraclavicular L.N or
inguinal L.N, lower extremities edema, ascites, decrease
breath sound indicate lung metastases.
External genital and vaginal examination looking for
concomitant lesions, HPV is risk for vulvar, vaginal,
cervical cancer. Superfacial groin and femoral L.N
examination.
Cervix may appear grossly normal if micro invasive
disease, or visible lesion entophytic, exophtic, polyploidy
lesion or barrel-shaped cervix, cervical ulceration or
granular mass.
Watery, purulent or bloody discharge.
Bimanual exam. Enlarge uterus, advance may have vaginal
involvement.
Rectovaginal examination find rectovaginal septum thick
irregular.
Per-rectum exam also required.
Test for women with symptoms of cervical
cancer or abnormal pap smear results.
Diagnostic testing
1. Medical history and physical exam this include
information related to risk factors and symptoms of
cervical cancer.
PAP SMEAR screen test not diagnostic but may be done
an abnormal pap test may mean more testing need.
2. Colposcopy symptoms suggestive cervical cancer or if
abnormal pap test an instrument that stay outside the body
with magnifying lenses. It help the doctors see the surface
of the cervix closely and clearly, it can done safely even in
pregnancy like pap test , not do during menstrual cycle,
use acetic acid solution on cervix if abnormal area seen so
biopsy taken.
3.Biobsy
colposcopy biopsy=abnormal area biopsy forceps small
1/8 inch section result mild cramping brief pain slight
bleeding under local anaesthetic agent.
Endocervical curettage (TZ when cannot be seen by
colposcopy by narrow instrument into cervical canal to
scrape the inside tissue and send for lab exam.
Cone biopsy, removed a cone shaped piece of tissue from
cervix including TZ. Cone biopsy not only diagnostic also

treatment it completely remove precancerous lesion. It can
done LEEP, LLETZ (local anaesthesia in doctor's office)
Cold knife cone biopsy in hospital surgical scalpel or laser
is used, general anaesthesia or spinal or epidural.
4. Imaging has a vital role in determining correct
management at initial staging, recurrent disease and
complication.
Chest X-ray
Pelvic MRI(soft tissue parts of the body)= most sensitive
for detecting locally advance disease.
imaging determined (tumor volume, parametrical extension,
confirming that tumor is confined to the cervix, nodal status.
CT scans are usually done if the tumor larger or if there is
concern about cancer spread.
Intra venous urography (rarely used if any abnormal area from
cervical cancer obstructing ureters)
PET this test helpful if cancer spread to L.N using special
glucose contain radioactive atom, cancer cells in the body
absorbed this sugar and used special camera can detect
radioactivity.
5.Cystoscopy, proctoscopy and EUA most often done in women
who have large tumors.
STAGING
Tests used during cervical cancer staging
A-Lab test (CBC, urine analysis, LFT, RFT)
B-Radiological (CXR, IVP, CT scan, MRI)
C-Procedural (cystoscopy, proctoscopy, EUA
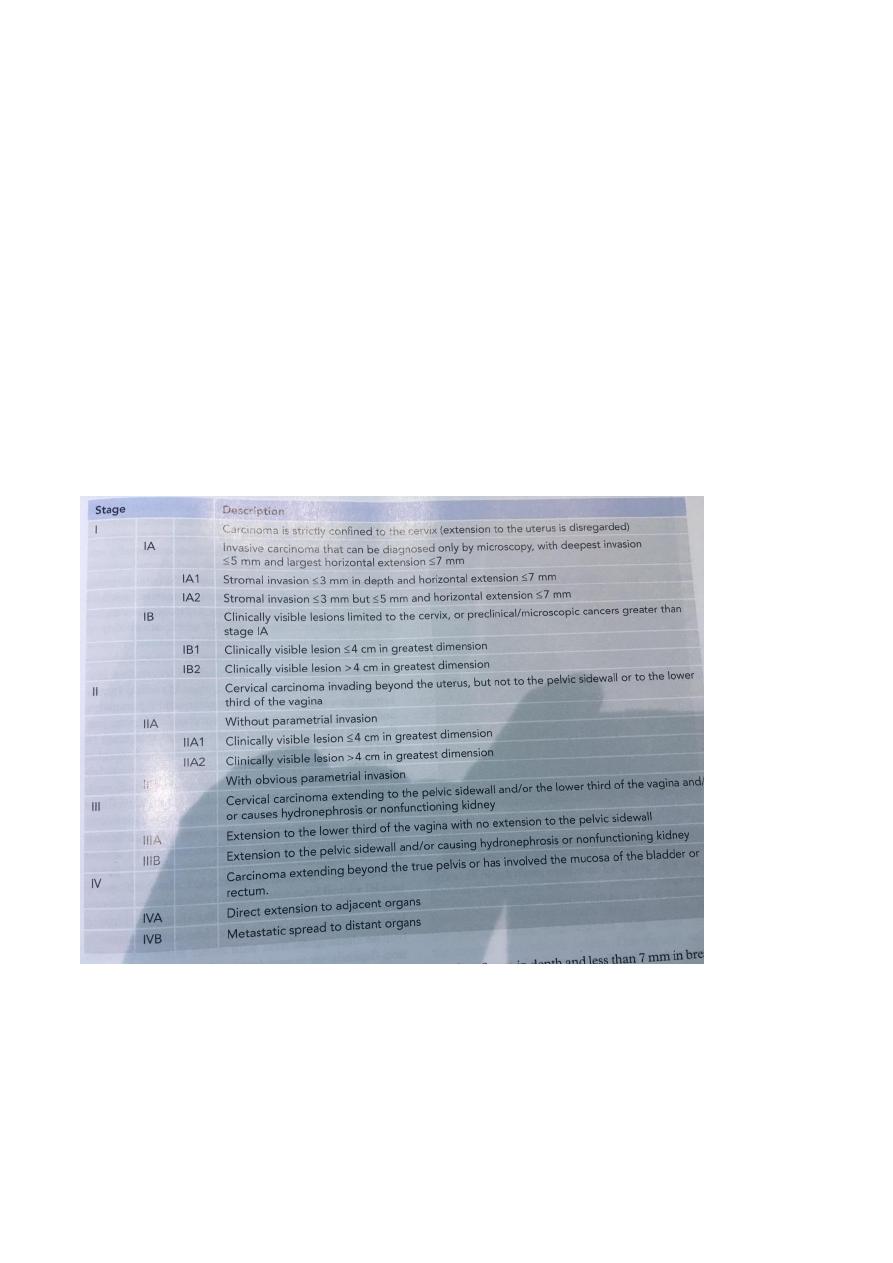
Cervical cancer staging
FICO staging
based on physical exam with or without
anesthesia and limited imaging study CXR, IVP and
barium enema. C-T , MRI, PET may be used to assist in
case of clinical suspsion of parametrial and pelvic side
wall metastasis. few other tests in some cases, cystoscopy
and proctoscopy. It is not based on what find during
surgery.
Surgical staging
Lymph node dissection of pelvic and
Para-aortic lymph node.
Prognosis
FIGO stage, size, surgical staging.
Cervical cancer survival

Stage 5-years survival
1A 100%
1B 88%
11A 68%
11B 44%
111 18-39%
1VA 18-34%
Treatment
Early stage disease (stage I-IIA)
Advance stage IIB and higher.
Primary disease stage 1A type one hysterectomy
1A2 radical hysterectomy
Trachelectomy (uterine preservation treatment) in women
wish to conserve fertility. MRI is performed preop. To
assess tumour size and location. Exclude tumour greater
than 2cm and involvement of uterine isthmus.
Stage 1B-11A either surgery or radiotherapy
Radical hysterectomy selected for young patient with low
BMI, wish to preserve ovarian function, and have concern
about sexual function.
Stages 11B through 1VA
Advanced stage cervical cancers, treatment for these
tumors must be individualized to maximize patient
outcome, it have poor prognosis, radiation therapy by
external beam pelvic radiation, brachytherapy(intracavity
radiation), currently chemo radiation use for advance
cancer, pelvic exenteration by removal of
bladder,rectum,uterus (if present) and surrounding tissues.
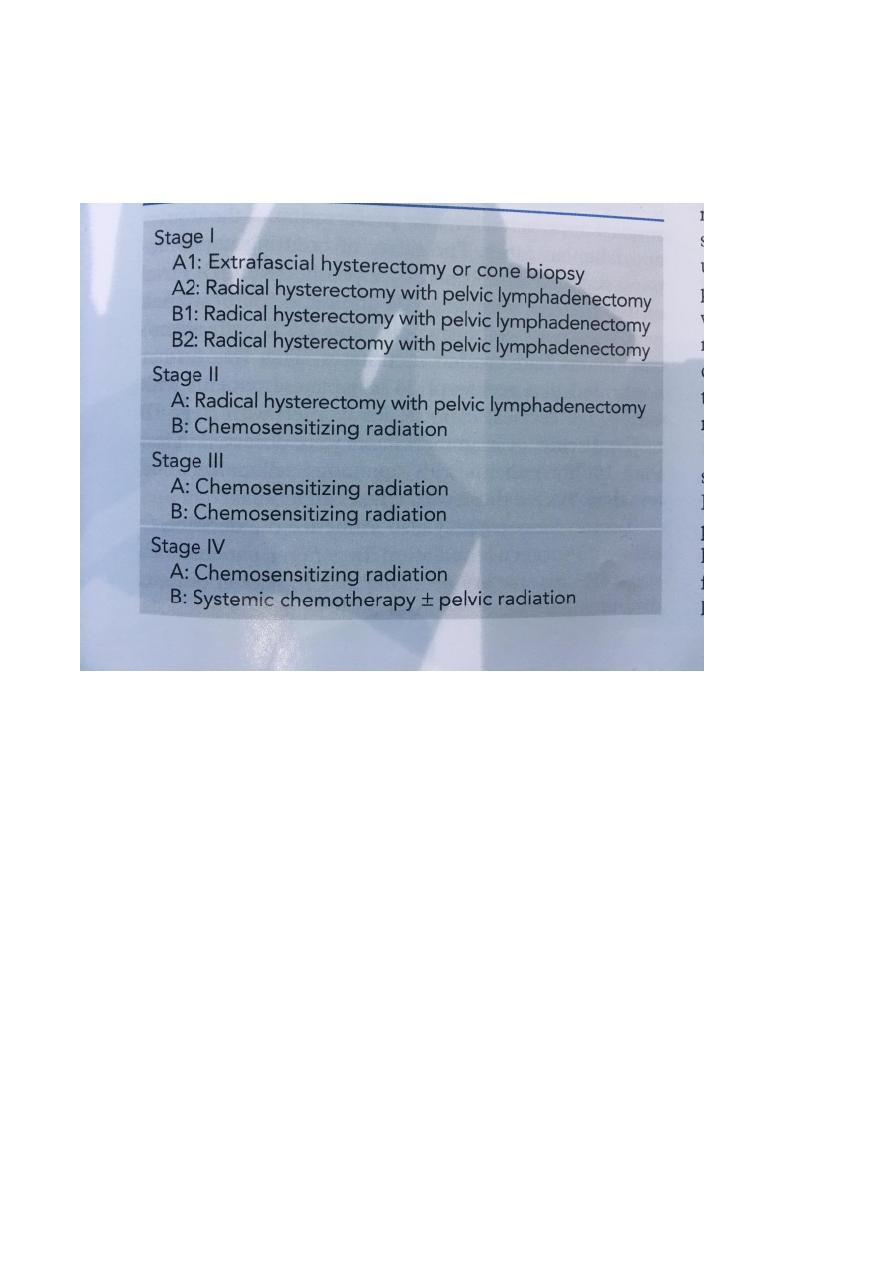
Stage 1VB
Poor prognosis treated with goal of palliation.
