HEMODYNAMIC DISORDERS
Dr. Mustafa Salah MSc; FIBMS PathAims of the lectures
What is hemodynamics of the human bodyWhat are the disease related to disordered human hemodynamics
What is the phathophysiology of each of these disorders.
…
….
Hemodynamic disorders
The health of cells depends on an unbroken circulation to deliver oxygen and nutrients and to remove wastesThe well-being tissues also requires normal fluid balance (homeostasis), which encompasses:
-Maintenance of vessel wall integrity
-Intravascular pressure and osmolarity within certain physiologic rangesHemodynamic disorders
These includes:
Edema
Congestion / hyperaemniaHemorrhage
Thrombosis
Embolism
Infarction
Shock
EDEMA
Definition: increased fluid in the interstitial tissue spacesApproximately 60% of lean body weight is water, of which 2/3 is intracellular, 1/3 extracellular (mainly interstitial)
Fluid collection in the different body cavities are variously designated as :
- Hydrothorax: fluid collection in pleural space- Hydroperitoneum (ascites): fluid collection in peritoneal cavity- Hydropericardium: fluid collection in pericardial space
Anasarca is a severe and generalized edema
Exudate is a protein-rich edema with specific gravity of over1.020
Transudate is a protein-poor edema with specific gravity of 1.012
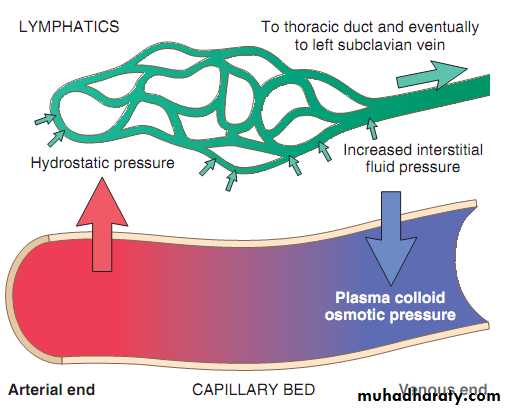
Factors influencing fluid movement across capillary wall
Pathophysiology of edema
• Increased hydrostatic pressure (HF)• Reduced plasma osmotic pressure (decreased albumin):
• Lymphatic obstruction ( inflammation or neoplasia)
• Sodium and water retention ( Renal failure)
• Increased vascular permeability ( inflammation)
Edema may be:
Morphology of edema- Most commonly seen in subcutaneous tissues, lungs, brain
- In congestive heart failure, edema occurs in dependent parts of the body
- In renal failure edema occur in eyelids causing periorbital edema
In both conditions, edema is pitting
Pulmonary edema, the lungs often are two to three times their normal weight, and contains edema fluid, and extravasated red cells.
HYPEREMIA AND CONGESTION
Both terms indicate a local increased volume of blood in a particular tissueHyperemia, is an active process resulting from arteriolar dilation and increased blood inflow, as occurs at sites of inflammation or in exercising skeletal muscle, (red color due to accumulation of oxygenated blood)
Congestion, passive process resulting from impaired outflow of venous blood from a tissue. It can occur systemically, as in cardiac failure, or locally as a consequence of an isolated venous obstruction, (red-blue tissue, cyanosis: due to accumulation of deoxygenated blood)
Long-standing congestion >chronic hypoxia> necrosis
HYPEREMIA AND CONGESTIONHYPEREMIA AND CONGESTION
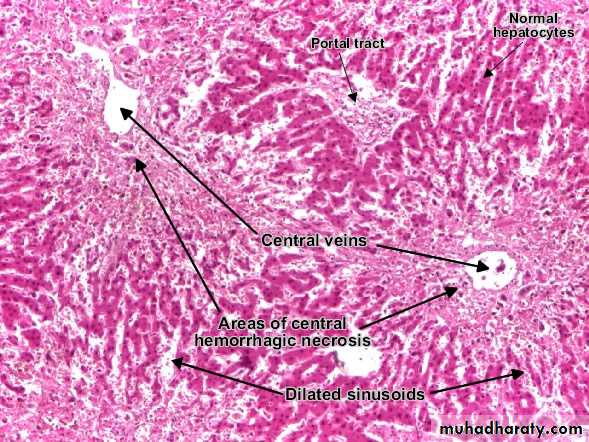
Morphology of hyperemia and congestion - Gross: cut surface is hemorrhagic and wet - Microscopy: engorgement of capillaries by bloodPulmonary congestion, (heart failure cells)
Aloveolar septa become thickened and fibrotic, and the alveolar spaces contain numerous macrophages laden with hemosiderin
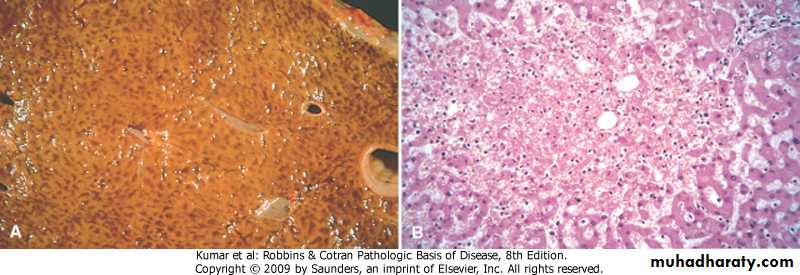
Hepatic congestion, (nutmeg liver)
The central regions of the hepatic lobules, viewed on gross examination, are red-brown and slightly depressed (owing to cell loss) and are accentuated against the surrounding zones of uncongested tan liver (nutmeg liver). Microscopic findings include centrilobular hepatocyte necrosis, hemorrhage, and hemosiderin-laden macrophages.
Local venous congestion: follows mechanical interference with the venous drainage from an organ
--- e.g. limbs in DVT caused by venous thrombosis .
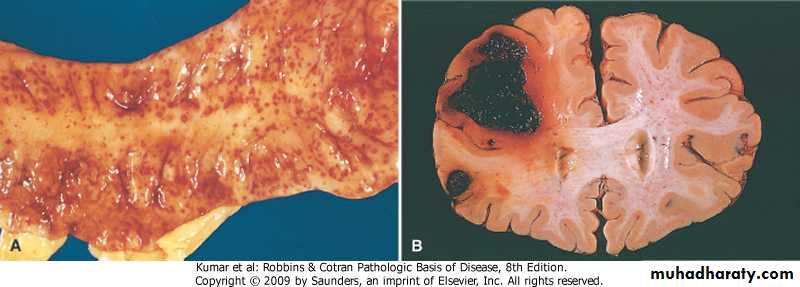
--- Compression of a vein by tumor or bandage.HEMORRHAGE
Extravasation of blood due to vessel ruptureCauses
- Chronic congestion- Hemorrhagic diatheses
- Vascular injury, (trauma, inflammation, atherosclerosis, neoplastic erosion)
HEMORRHAGE
patterns of hemorrhage -External bleeding -Internal bleeding .hematoma .hemothorax .hemoperitoneum.hemopericardium .hemarthrosis
- Petechiae (1- to 2-mm) - Purpura (>3mm) - Ecchymoses (>1 to 2cm)
HEMORRHAGE
HEMORRHAGE
Clinical significance of hemorrhage depends on:- Volume and rate of bleeding - Site involved - Duration (acute versus chronic or recurrent)
HEMOSTASIS AND THRMOBOSIS
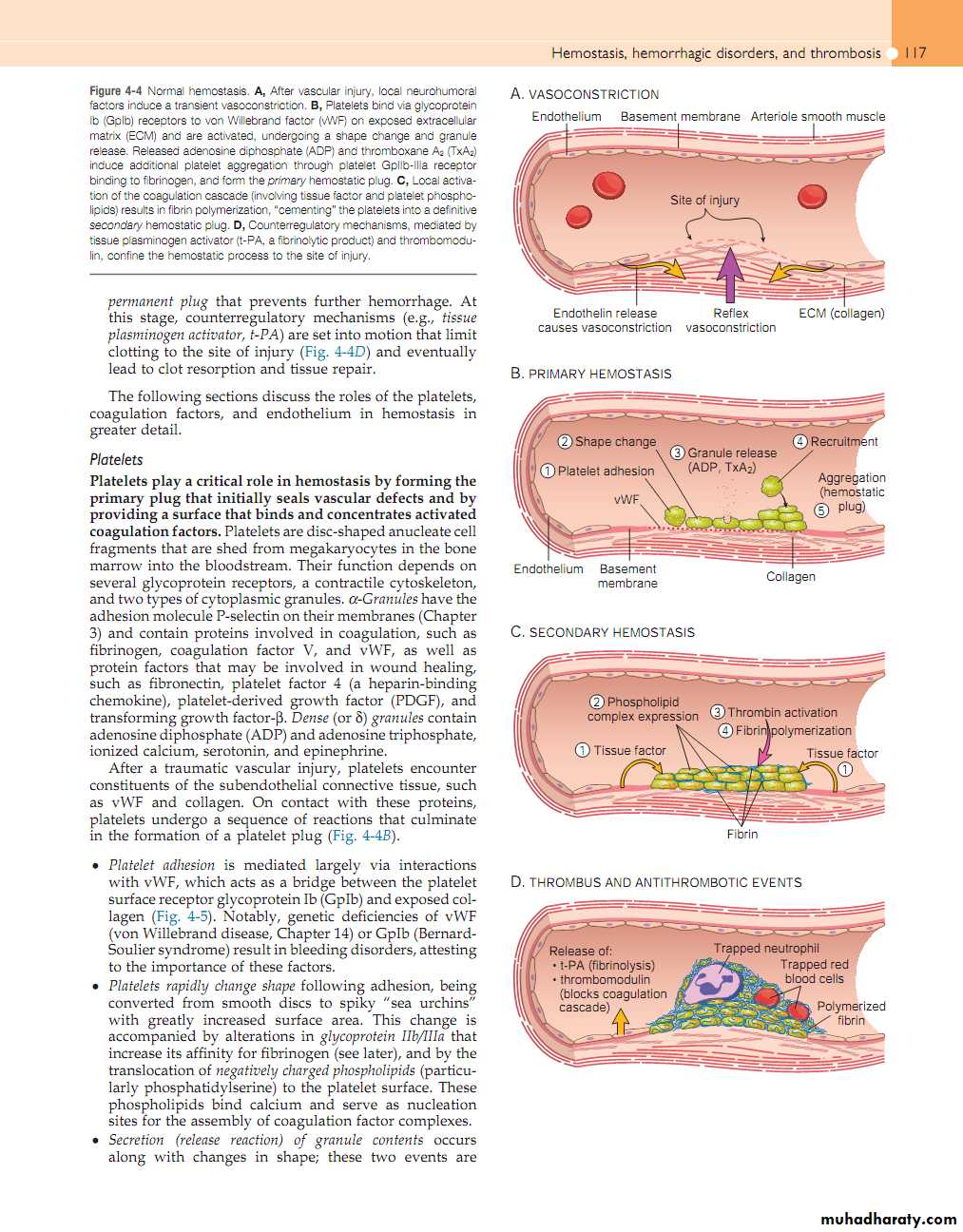
Both are regulated by: - Vascular wall - Platelets - Coagulation cascadeHemostasis
1. Maintaining blood in a fluid, clot-free state in normal vessels2. Rapid localized plug at a site of vascular injury
Sequence of events include; - Brief arteriolar vaso-constriction - Primary hemostasis (transient platelet plug) - Secondary hemostasis (activation of coagulation cascade) - Permanent plug
Hemostasis
1. Endothelial cells modulate several aspects of hemostasis, by having: - Anti-platelet, anticoagulant, and fibrinolytic properties - Pro-coagulant activities
2. Platelets play central role in hemostasis: - Adhesion - Secretion - Aggregation
Hemostasis
3. Coagulation Cascade- A series of enzymatic conversions, turning inactive pro-enzymes into active enzymes > thrombin formation
- Thrombin converts soluble fibrinogen into insoluble fibrin
- Activation of the clotting cascade also sets into motion a fibrinolytic cascade that limits the size of the final clot
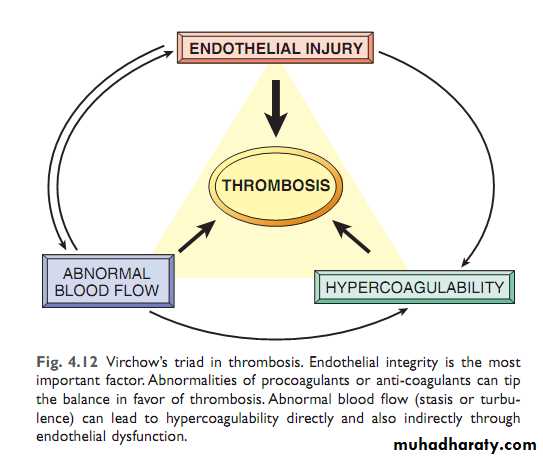
Thrombosis
Inappropriate activation of normal hemostatic processPredisposing factors (Virchow triad): 1- Endothelial injury 2- Stasis or turbulence of blood flow 3- Blood hypercoagulability
Thrombosis
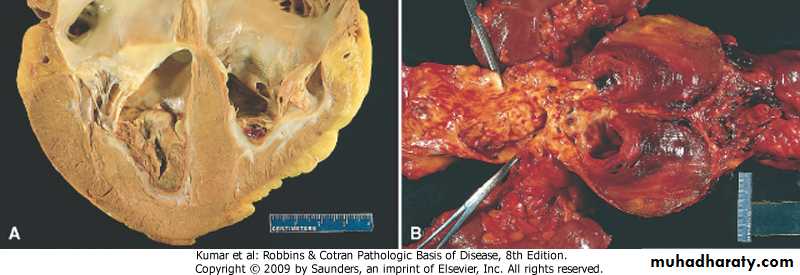
Morphology of thrombus- Thrombi may develop anywhere in the cardiovascular system
- Grossly and microscopically have laminations (lines of Zahn), produced by alternating pale layers of platelets admixed with some fibrin and darker layers containing more red cells
Thrombosis
Arterial thrombi are: - usually occlusive - firmly attached to the wall - gray-white and friable
Venous thrombi are: - almost invariably occlusive - less firmly attached to the wall - red
Mural thrombi are: - those attached to the wall of a spacious cavity
Vegetations are: - thrombi formed on heart valves
Thrombosis
These are "lines of Zahn" which are the alternating pale pink bands of platelets with fibrin and red bands of RBC's forming a true thrombus.
Thrombosis
Fate of the thrombus 1- Propagation 2- Embolization 3- Dissolution 4- Organization and re-canalizationClinical correlation - Cause obstruction of vessels - Are possible sources of emboli
DISSEMINATED INTRAVASCULAR COAGULATION (DIC)
Characterized by: - Sudden or insidious onset of widespread fibrin thrombi formation in the micro-circulation - Rapid consumption of platelets and coagulation proteins (consumption coagulopathy) - Activation of fibrinolytic mechanismsDISSEMINATED INTRAVASCULAR COAGULATION (DIC)
DIC is not a primary disease but a potential complication of many conditions have in common, the widespread activation of thrombin; - Obstetric complications - Infections - Neoplasms - Massive tissue injury