Oral Cancer
Pathology:Oral cancer accounts for less than 3% of all cancers. It is the eleventh most common cancer worldwide. Squamous cell carcinoma (SCC) is the predominant form of oral cancer and accounts for greater than 90% of malignant pathology. Other forms include salivary gland tumors, mesenchymal tumors, lymphoma, and melanoma.Oral cancer is predominantly a disease of older age. More than 92% of oral and pharyngeal cancers occur in individuals older than 40 years, with the average age being 63. Oral cancer is predominantly male disease, but females have experienced a steady rise in the incidence of oral cancer since the increase in female smokers began in the 1950s.
The natural history of oral SCC
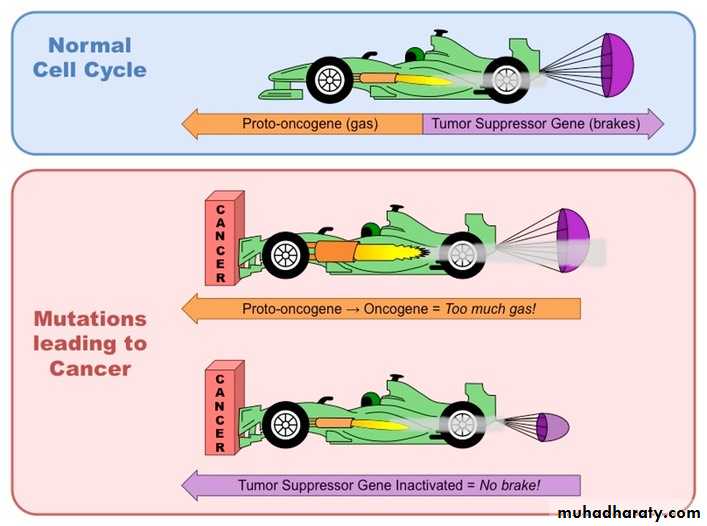
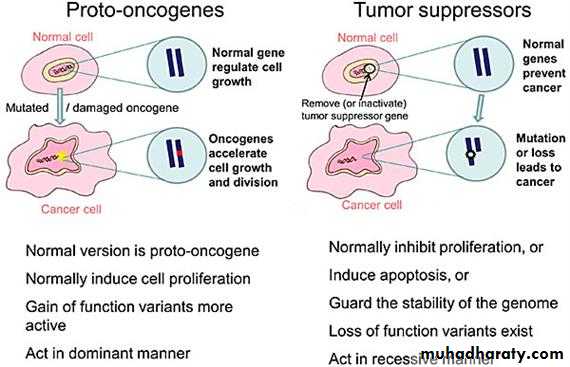
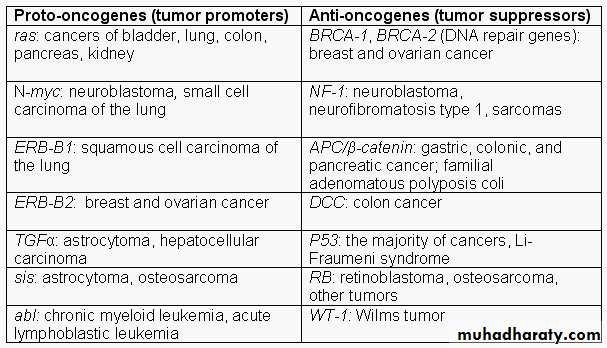
Oral carcinogenesis appears to evolve through a complex, multistage process involving bio molecular changes that precede premalignant lesions, which in turn precede invasive cancer. The genetic changes caused by exposure to carcinogens like tobacco and alcohol tend to accumulate over time in the entire mucosa exposed to this insult. The fundamental regulatory mechanism in carcinogenesis is thought to be the cellular balance between oncogenes and tumour suppressor genes. The proto-oncogenes stimulate cell growth and proliferation and are under negative control of the tumour suppressor genes, which prevent Over growth.A cancer may therefore arise either from activation of a proto-o or due to loss of a tumour suppressor gene. Numerous genetic events are required to cause a cancer, but the most frequently observed molecular abnormality is mutation of the 'p53 tumour suppressor gene' which is seen in 40-70% of malignant lesions and 20% of premalignant lesions. Several other oncogenes and tumour suppressor genes have been studied, but no clear relationship has been demonstrated with phenotypic behaviour or survival.
Aetiology:
The cause of oral SCC is multifactorial. No single causative agent orfactor (carcinogen) has been clearly defined or accepted, but both
extrinsic and intrinsic factors may be at work.
• Tobacco smoking & Smokeless tobacco use:
Studies revealed that the proportion of smokers among patients with oral carcinoma is 2-3 times greater than the general population. Also pipe and Cigar smoking carries a greater oral cancer risk than does cigarette smoking. The risk of oral SCC is dose and time dependent. The practice of reverse smoking is popular in India and South America considerably elevates one's risk for oral cancer. Chronic Smokeless tobacco use increases the risk of oral SCC 2-26 times. Approximately 50% of all oral cancers in smokeless tobacco users occur at the site where the tobacco is habitually placed.2.betel quid:
is a compound of natural substances chewed for their psychostimulating effects. Among betel quid users in Asia, the lifetime risk of developing oral cancer is a remarkable 8%.3. Alcohol:
It is uncertain whether excessive alcohol consumption alone can initiate carcinogenesis, although it is well established that alcohol in combination with tobacco is a significant risk factor for oral cancer development (the risk increases 15 times).
4. Chronic irritation:
including poor oral hygiene, il1-fitting prostheses, chronic use of mouth washes or Marijuana smoking.
5. Phenolic agents:
there is increased risk of oral cancer for workers in the wood products industry chronically exposed to certain chemicals, such as phenoxy acetic acids.
6. Radiation:
this include ultraviolet radiation and X-irradiation, which reduces immune reactivity and produces chromosomal abnormalities.7. Iron deficiency:
especially severe chronic form known as Plummer- Vinson syndrome. People who are deficient in iron tend to have impaired cell-mediated immunity, and iron is essential to the normal functioning of epithelial cells of the upper digestive tract. In deficiency states, these epithelial cells turn over more rapidly and produce an atrophic or immature mucosa.
8. Vitamin A deficiency:
producing excessive keratinization of the skin and mucous membrane.9. Syphilis :
(tertiary stage has long been accepted as having a strong association with the development of dorsal tongue carcinoma. Also the arsenical agents and heavy metals that were used to treat syphilis before the advent of modern antibiotic therapy have carcinogenic properties themselves and may have been responsible for some of the earlier cancer development in this disease. Today syphilis associated oral malignancies are rare because the infection is typically diagnosed and treated before the onset of the tertiary stage.
10. Candida infection:
hyperplastic candidiasis also called candida leukoplakia is considered a cancerous condition. Some strains of candida albicans produce certain chemicals that are implicated in carcinogenesis. But the role of candida infection in oral cancer development is debated.• Oncogenic viruses :
human papilloma virus is implicated in oral cancer development especially subtypes 16, 18, 31 and 33. The mechanism involves 2 virally encoded proteins; E6 which promotes degradation of p53 tumor suppressor gene products and E7 which promote degradation of pRb gene products.12. Immunosuppression:
13. Oncogenes and Tumor suppressor genes: which are chromosomal components capable of being acted on by a variety of causative agents.
Site distribution ;
The importance of the "cancer-prone crescent" and its significance is related to the postulate that most oral cancers should occur in mucosa where saliva pools due to gravity exposing it to salivary carcinogens. The site distribution of oral SCC is varied but the general trend is as follows:
- Tongue 35% (31% lateral border, 2% tip and 2% dorsum).
- Floor of mouth 30% (25% anterior and 5% posterior).
- Lower alveolus 15%.
- Buccal mucosa- 10%.
- Upper alveolus 5%.
- Hard palate 3%.
- Retromolar trigon 2%.
The distribution of oral cancer in developing countries is, however, very different and may be explained by certain habits peculiar to that population, for example, betel quid chewing that contributes to the high incidence of buccal cancer in the Indian subcontinent.
Clinical presentation:
Despite the fact that the oral cavity is an easily accessible site for the patient and the clinician, a surprisingly large number of oral tumors present late because of the painless and rather vague nature of the symptoms.The clinical manifestation of oral cancer is varied including:
Exophytic or mass forming lesion:which typically has a surface that is irregular, fungating, papillary, or verruciform, and its color may vary from normal to red to white, depending on the amount of keratin and vascularity. The surface is often ulcerated, and the tumor is indurated on palpation.
-Endophytic
growth pattern which has a depressed, irregularly shaped, ulcerated, central area with a surrounding rolled border of normal, red or white mucosa. The rolled border results from invasion of the tumor downward and laterally under adjacent epithelium with induration of the underlying tissues.Leukoplakic, Erythroplakic or combined Erythroleukoplakic
lesions (speckled leukoplakia) which has a high incidence of malignant transformation. A thorough examination of the upper aerodigestive tract mucosa should be performed in every case since synchronous multiple primary cancer occur in approximately in 4% of patients with oral cancers.Symptoms:
Lesions in the floor of mouth or tongue may be painful, infiltrative lesions of the floor of mouth also may extend to invade bone anteriorly, muscles of the floor of mouth deeply, or tongue posteriorly. Patients may complain of difficulty in swallowing or speaking, which becomes even more pronounced when the tumor spreads to the floor of the mouth.
Early spread to the alveolus and periosteum of the mandible is common ; clinical fixation of the tumor to the mandible indicates periosteal involvement, and direct bone invasion may be present in a high number of cases. Patients may report pain while chewing, intermittent bleeding, loose teeth or ill-fitting dentures in gingival or alveolar ridge lesions. Some symptoms like trismus or altered sensation or anesthesia of the lower lip may signify locally advanced disease.
Clinical staging:
The purpose of staging is to group patients into statistical classificationsthat:
1. Provide useful information on treatment (appropriate therapy for a
given tumor can be selected) and prognosis
2. This standardized format facilitates research, assessment Outcomes, and communication among clinicians by establishing uniform reporting parameter
As a general rule, more advanced stage implies a worse prognosis
Initial staging is performed by using all available clinical and radiographic data (cTNM). Final staging incorporates histopathologic data if surgery is performed (pTNM),
The TNM system stages cancer purely on the anatomic extent of disease and does not account for the many biologic, molecular, or host characteristics that are known to influence prognosis.
One of the major limitations of the previous editions of the TNM system was that it failed to take into consideration the prognostic implications of the third dimension or depth of invasion of the primary tumor. With the increase in tumor depth there is an increase in the incidence of the nodal metastasis and a decrease in the overall survival rate.
TNM system (Previous edition)
T- Two-dimensional tumor size.
N-Nodal status in the cervical region.
M-Metastatic disease beyond the cervical lymph nodes
Primary Tumor (T)
TX: Primary tumor cannot be assessed
TO: No evidence of primary tumor
Tis: Carcinoma in situ
T1: Tumor no larger than 2 cm in greatest dimension
T2: Tumor larger than 2 cm but no larger than 4 cm in greatest dimension
T3: Tumor larger than 4 cm in greatest dimension
T4a: Moderately advanced local disease:
(Lip) Tumor invades through cortical bone, inferior alveolar nerve floor of mouth, or skin of face, that is, chin or nose.
(Oral cavity) Tumor invades adjacent structures only (e.g through cortical bone (mandible or maxilla) into deep extrinsic muscle of tongue [genioglossus, hyoglossus, palatoglossus, and styloglossus), maxillary sinus skin of face).
T4b: Very advanced local disease. Tumor invades masticator space, pterygoid plates, or skull base and/or encases internal carotid artery.
Regional Lymph Nodes (N)
NX: Regional lymph nodes cannot be assessedNO: No regional lymph node metastasis
N1: Metastasis in a single ipsilateral lymph node, no larger than 3 cm in greatest dimension
N2a: Metastasis in a single ipsilateral lymph node larger than 3 cm but no larger than 6 cm in dimension
N2b: Metastasis in multiple ipsilateral lymph nodes, none larger than
6 cm in greatest dimension
N2c: Metastasis in bilateral or contralateral lymph nodes, no larger
than 6 cm in greatest dimension
N3: Metastasis in a lymph node larger than 6 cm in greatest dimension.
Distant Metastasis (M)
MX: Distant metastasis cannot be assessed
MO: No distant metastasis
M1: Distant metastasis
In 2017 the 8th Edition of the TNM system introduced major changes:
- For the T category of oral SCC the depth of invasion (DOT) is acknowledged. Pathologically, DOI is measured from the level of the basement membrane of the closest adjacent normal mucosa to the deepest point of tumor invasion. The other change from prior editions of the TNM system is the elimination of the T0 category.- For the N category extra nodal extension (ENE) has been added as a prognostic variable for regional lymph node metastases in addition to the size of metastatic lymph nodes.
• T CRITERIA
• T CATEGORY• TX
• Primary tumor cannot be assessed
• Tis
• Carcinoma in situ
• T1
• Tumors ≤2 cm,≤5 mm depth of invasion (DOI)
• T2
• Tumor ≤2 cm, DOI >5 cm, and ≤10 mm or tumor >2 cm but ≤4 cm and ≤10 mm DOI
• T3
• Tumor >4 cm or any tumor 10 mm DOI
• T4a
• Moderately advanced local disease Lip; tumor invades through cortical bone or involves the inferior alveolar nerve, floor of mouth, or nose)Oral cavity; tumor invades adjacent structures only (eg, through cortical bone of the mandible or maxilla, or involves the maxillary sinus or skin of the face); note that superficial erosion of bone/tooth socket (alone) by a gingival primary is not sufficient to classify a tumor as T4
• T4b
• Very advanced local disease; tumor invades masticator space pterygoid plates, or skull base and/or encases the internal carotid artery
Stage Grouping
Grading:
Histopathologic grading of SCC is based upon the degree of differentiation and resemblance to normal squamous epithelium and the amount of keratin production. It consists of 3 grades:Grade 1 (well differentiated)
Grade 2 (moderately differentiated)
Grade 3 (poorly differentiated)
The histopathologic grade of a tumor is related to its biologic behavior;
grade 1 (well differentiated) tumor is a low-grade tumor and it grows at a slightly slower pace and metastasizes later in its course whereas high-grade tumor (poorly differentiated) enlarges rapidly and metastasizes
early. A tumor with a microscopic appearance somewhere between these two extremes is called moderately differentiated.
Physical examination
During examination the following points should be considered:• Tumor's location, s Size, and relationship to adjacent anatomic
structures.
• Fixation to the mandible,
• Proximity to the midline often guides the decision for unilateral
versus bilateral neck dissection when indicated.
• Trismus or decreased tongue mobility may be an indication of Cranial nerve deficits suggest tumor involvement, which may invasion into deeper structures increase suspicion for peri-neural spread.
• The status of the dentition should be assessed in patients in whom radiation therapy may be indicated because of the risk for xerostomia-related caries and osteoradionecrosis. Plans should be made for non-viable teeth to be removed at the time of surgery or before radiation therapy.
• Biopsy of the primary tumor is required for histologic diagnosis and treatment planning.
• Lymph nodes in the neck must be palpated carefully to assess for cervical metastasis or other abnormalities. Palpable nodes should be evaluated for size, location, and fixation to skin or deeper structures.
• Identify distant sites that may be used for reconstructive purposes.
Radiographic assessment
Pretreatment imaging is important to evaluate:• The tumor size and extent.
• Involvement of adjacent anatomic structures.
• Staging the cervical lymph nodes.
• Tumor invasion for the bone especially the mandible.
The modalities used include:
I. Conventional RadiographsII. Computed Tomography
The most common imaging modality used. The main advantages are: 1. excellent bone detail,
2. adequate soft tissue enhancement,
3. and relatively low cost and availability.
While the main disadvantages include;
• ionizing radiation,• artifacts created by metallic dental restorations and irregular teeth sockets and periapical lesions that may be confused as bony invasion
III. Magnetic Resonance Imaging
Advantages are:
1. superior soft tissue details .
• lack of ionizing radiation.
• MRI is superior to CT when there is suspicion of perineural invasion, skull base invasion or intracranial involvement.
The main disadvantages are;
• more sensitive to motion artifacts,
• expensive,
• difficult for patients who suffer from claustrophobia,
• and it is contraindicated in case of presence of ferromagnetic implants.
IV. Ultrasound
Advantages:• quick,
• inexpensive,
• non-invasive,
• lymph nodes can be sampled under ultrasound guidance.
The main disadvantages: include;
• limited utility in the oral cavity.
• Bone does not transmit sound, it is highly technique sensitive, and operator dependent with steep learning curve.
Positron Emission Tomography (PET)
Functional imaging with 18F-fluorodeoxyglucose PET has been shown to be an effective tool in the diagnosis of head and neck cancer. PET has shown promise in the evaluation of metastatic disease, tumor recurrence, and treatment response after chemotherapy or radiation therapy. The integration of PET and CT technology is more accurate than either modality alone in the depiction of head and neck malignancies.
Treatment
The goals of the treatment of cancer of the oral cavity are:1. Cure of the cancer.
2. Preservation or restoration of speech, mastication, swallowing, and external appearance.
3. Minimization of the sequelae of treatment such as dental decay, osteonecrosis of the mandible, and trismus.
4. Awareness of the risk of subsequent primary tumors and their management.
The main modalities of treatment are surgery, radiotherapy and chemotherapy (others: immunotherapy, photodynamic therapy, an laser). in general. small and superficial tumors of the oral cavity are equaly amenable to being cured by surgical resection or radiotherapy.
Therefore use of a single modality is preferred as the definitive treatment in early stage (T1 and T2) tumors of the oral cavity. When the end point of treatment, that is, cure of cancer, is comparable, other factors must play a role in the selection of initial treatment. These factors include complications, cost, convenience, compliance, and long-term sequelae of treatment. Considering these factors, surgery is the preferred treatment for T1 and T2 tumors of the oral cavity.
In advanced stage (T3 and T4) oral cancer combining surgery with adjuvant postoperative radiotherapy offers improved loco regional control but does not improve survival.
The most important high-risk features for combining surgery and radiotherapy are:
Positive margins.
Extranodal spread.
Multiple positive nodes.
Perineural or vascular invasion.
Metastasis to lymph node levels IV and V.
Surgical treatment
Surgical excision is one of the two mainstays of loco-regional treatment of oral cancer. It allows histopathological assessment of the clearance margins of the tumor together with further information regarding tumor spread and dynamics
Factors that influence the choice of surgical treatment for a primary tumor of the oral cavity are:
Tumor Factors
- Site.
- Size.
- Location (anterior versus posterior.
- Proximity to bone.
- Previous treatment.
- Depth of invasion.
- The histological characteristics of the primary tumor (i.e., type and
grade).
- Status of cervical lymph nodes.