thyroid gland
By
Dr.Salah Aljanaby
Ass. Prof
General and Laparoscopic Surgeon

SURGICAL ANATOMY
•
The normal thyroid gland weighs 20
–25 g.
•
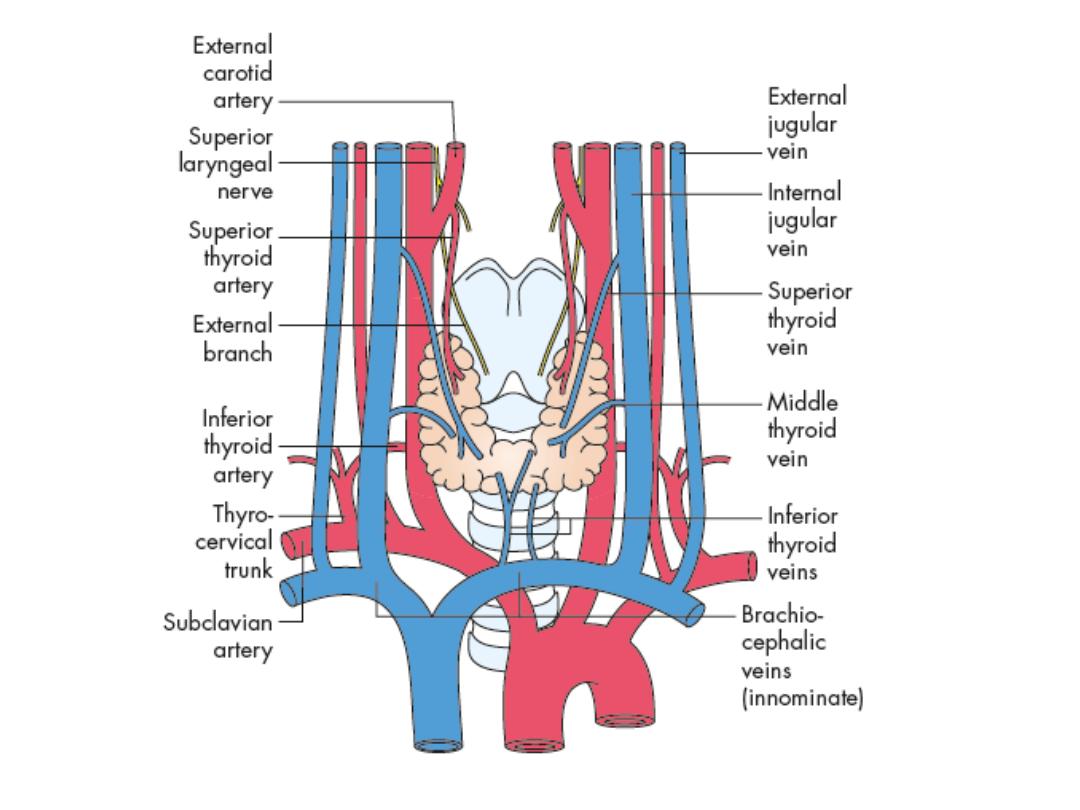
The arterial supply is rich, and extensive anastomoses occur between the
main thyroid arteries and branches of the tracheal and esophageal arteries
•
There is an extensive lymphatic network within the gland. Although some
lymph channels pass directly to the deep cervical nodes, the subcapsular
plexus drains principally to the central compartment juxtathyroid
–
‘Delphian’– and paratracheal nodes and nodes on the superior and inferior
thyroid veins (level VI), and from there to the deep cervical (levels II, III, IV and V)
and mediastinal groups of nodes (level VII)
•
The normal parathyroid gland weighs up to 50 mg
•
orange/brown colour
•
Most adults have four parathyroid glands

• PHYSIOLOGY
•
Thyroxine
• The hormones tri-iodothyronine (T3) and l-thyroxine (T4) are bound to
thyroglobulin within the colloid. Synthesis within the thyroglobulin
complexis controlled by several enzymes, in distinct steps:
• • trapping of inorganic iodide from the blood;
• • oxidation of iodide to iodine;
• • binding of iodine with tyrosine to form iodotyrosines;
• • coupling of monoiodotyrosines and di-iodotyrosines to form T3 and T4.
• When hormones are required, the complex is resorbed into the cell and
thyroglobulin is broken down. T3 and T4 are liberated and enter the blood,
where they are bound to serum proteins: albumin, thyroxine-binding
globulin (TBG) and thyroxinebinding prealbumin (TBPA). The small amount
of hormone that remains free in the serum is biologically active.
• The metabolic effects of the thyroid hormones are due to unbound free T4
and T3 (0.03 and 0.3 per cent of the total circulating hormones,
respectively). T3 is the more important physiological hormone and is also
produced in the periphery by conversion from T4. T3 is quick acting (within
a few hours),
• whereas T4 acts more slowly (4–14 days).

• Parathormone
• The parathyroid glands secrete the 84-amino acid
peptide parathyroid
• hormone (PTH), which controls the level of serum
calcium in extracellular fluid
• PTH is released in response to a low serum calcium
or high serum magnesium level. PTH activates
osteoclasts to resorb bone, and increases calcium
reabsorption from urine and renal activation of
vitamin D with subsequent increased gut absorption
of calcium. Renal excretion of phosphate is also
increased.

• Calcitonin
• The parafollicular C cells of the thyroid are of
neuroendocrine origin and arrive in the
thyroid via the ultimobranchial body
• They produce calcitonin which is a serum
marker for recurrence of medullary thyroid
cancer.

• The pituitary–thyroid axis
• Synthesis and liberation of thyroid hormones from the thyroid
is controlled by thyroid-stimulating hormone (TSH) from the
anterior pituitary.
• Secretion of TSH depends upon the level of circulating thyroid
hormones and is modified in a classic negative feedback
manner.
• In hyperthyroidism, when hormone levels in the blood are
high, TSH production is suppressed whereas in
hypothyroidism it is stimulated. Regulation of TSH secretion
• also results from the action of thyrotrophin-releasing
hormone (TRH) produced in the hypothalamus.

• Thyroid-stimulating antibodies
• A family of IgG immunoglobulins bind with TSH receptor
sites (TRAbs) and activate TSH receptors on the follicular
cell membrane.
• They have a more protracted action than TSH (16–24
versus 1.5–3 hours) and are responsible for virtually all
cases of thyrotoxicosis not due to autonomous toxic
nodules. Serum concentrations are very low but their
measurement is not essential
• to make the diagnosis

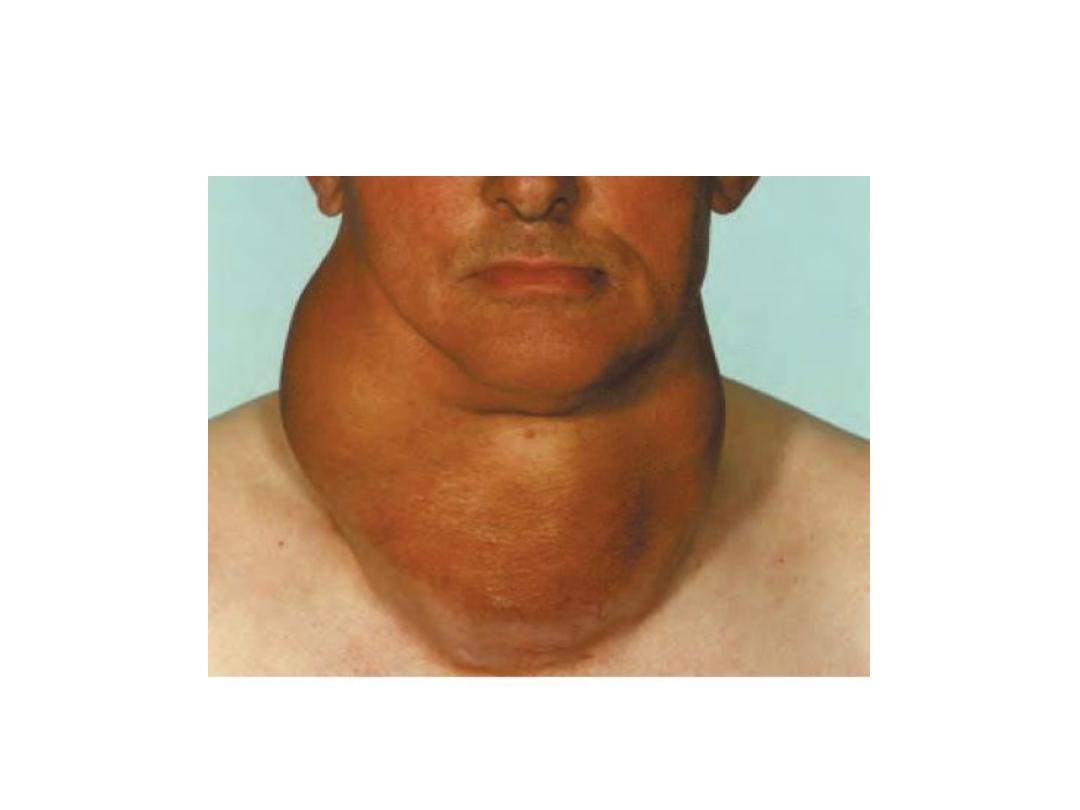
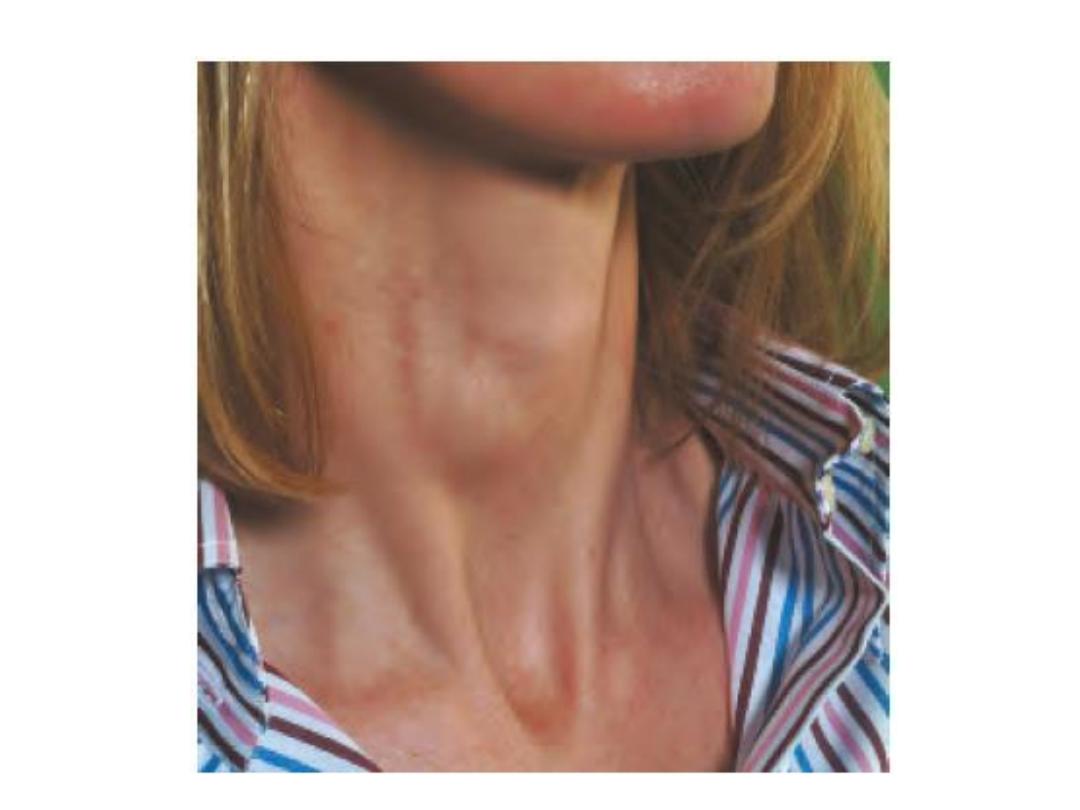
• THYROID ENLARGEMENT
• The normal thyroid gland is impalpable.
• Goitre is generalised enlargement of the thyroid
gland
• Isolated (solitary )swelling is discrete swelling (nodule)
in one lobe with no palpable abnormality elsewhere
• Dominant swelling is discrete swellings with evidence
of abnormality elsewhere in the gland
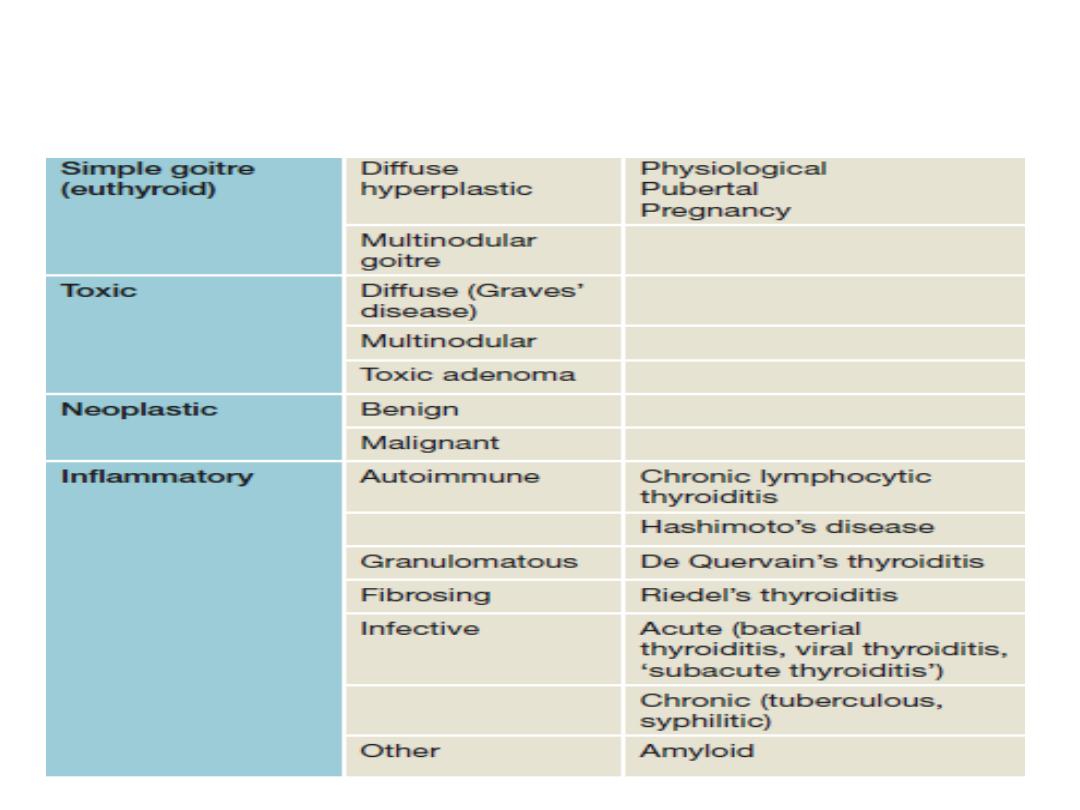
Classification of thyroid swellings
• Simple goitre
•
Aetiology
• stimulation of the thyroid gland by TSH,
• inappropriate secretion from a microadenoma in the
anterior pituitary (which is rare),
• chronically low level of circulating thyroid hormones.
• The most important factor in endemic goitre is dietary
deficiency of iodine
• defective hormone synthesis probably accounts for many
sporadic goitres

•
The natural history of simple goitre
• Stages in goitre formation are:
1) ●● Persistent growth stimulation causes diffuse hyperplasia; all
lobules are composed of active follicles and iodine uptake is
uniform. This is a diffuse hyperplastic goitre, which may persist for
a long time but is reversible if stimulation ceases.
2) ●● Later, as a result of fluctuating stimulation, a mixed pattern
develops with areas of active lobules and areas of inactive lobules.
3) ●● Active lobules become more vascular and hyperplastic until
haemorrhage occurs, causing central necrosis and leaving only a
surrounding rind of active follicles.
4) ●● Necrotic lobules coalesce to form nodules filled either with
iodine-free colloid or a mass of new but inactive follicles.
5) ●● Continual repetition of this process results in a nodular goitre.
Most nodules are inactive, and active follicles are present only in
the internodular tissue.

•
Diagnosis
The patient is euthyroid,
The nodules are palpable and often visible; they are
smooth, usually firm and not hard
Goitre is painless and moves freely on swallowing.
Hardness and irregularity, due to calcification, may
simulate carcinoma.
A painful nodule, sudden appearance or rapid
enlargement of a nodule raises suspicion of carcinoma
but is usually due to haemorrhage into a simple nodule.
Differential diagnosis from autoimmune thyroiditis may
be difficult and the two conditions frequently coexist.

•
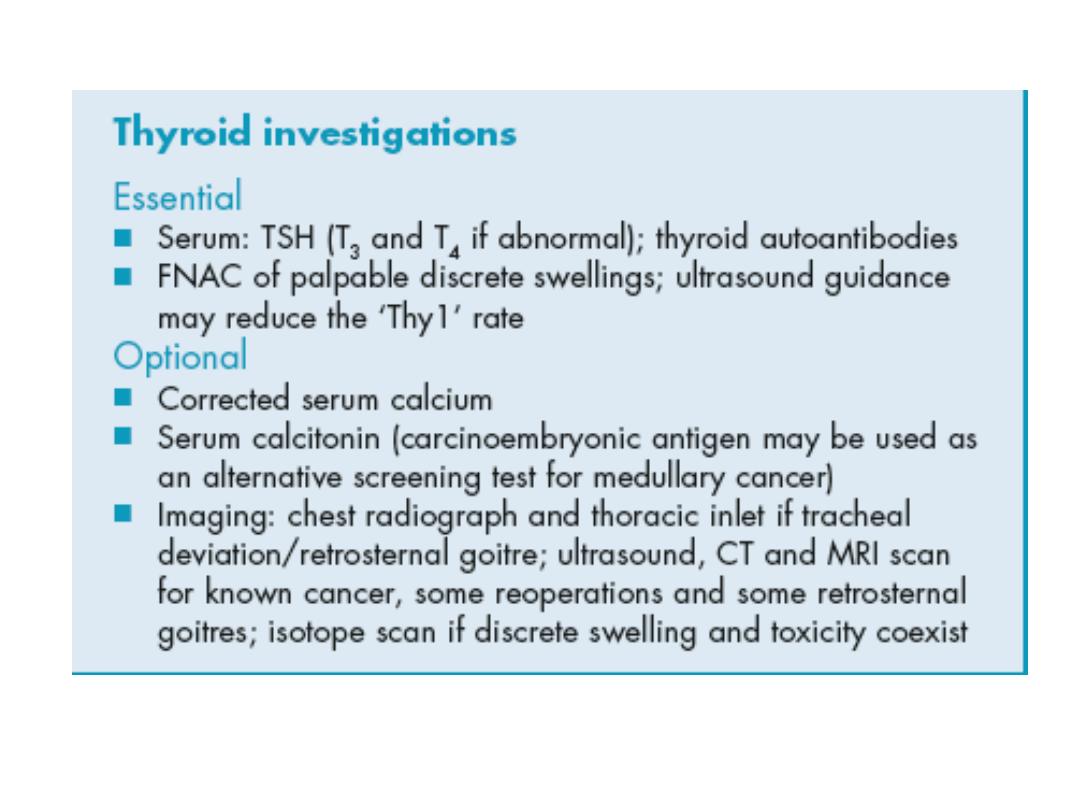
Investigations
1) Thyroid function should be assessed to exclude mild
hyperthyroidism,
2) Thyroid antibodies tested to differentiate from
autoimmune thyroiditis.
3) Ultrasound is the gold standard assessment
4) FNAC is only required for a nodule within the goitre that
demonstrates ultrasonic features of concern. The biopsy
should be performed under ultrasonic guidance to
ensure the correct nodule is sampled.
5) CT scan of the thoracic inlet is the best modality to
assess tracheal or oesophageal compression.
•
Complications
o Tracheal obstruction
may be due to gross lateral displacement or compression in a lateral
or anteroposterior plane by retrosternal extension of the goitre
o SECONDARY THYROTOXICOSIS
Transient episodes of mild hyperthyroidism are common, occurring in
up to 30% of patients.
o CARCINOMA
An increased incidence of cancer (usually follicular) has been
reported from endemic areas.
•
Prevention and treatment of simple goitre
• In endemic areas the incidence of goitre has been
strikingly reduced by the introduction of iodised salt.
• In the early stages, a hyperplastic goitre may regress if
thyroxine is given in a dose of 0.15–0.2 mg daily for a few
months.
• Although the nodular stage of simple goitre is irreversible,
more than half of benign nodules will regress in size over
10 years.
• Most patients with multinodular goitre are asymptomatic
and do not require operation.
• Surgery is indicated for nodular goitres
• 1. features of underlying malignancy
• 2. swallowing symptoms i
• 3. cosmetic reasons i
• 4. tracheal compression
• There is a choice of surgical treatment
in multinodular goitre
:
•
Total thyroidectomy
• with immediate and lifelong replacement of
thyroxine
• .
Subtotal thyroidectomy
• partial resection of each lobe removing the bulk
of the gland, leaving up to 8 g of relatively
normal tissue in each remnant.
Colloid goitre
Multinodular goitre

• Clinically discrete swellings
• common
• palpable in 3–4% of the adult population
• three to four times more frequent in women
than men.

•
Diagnosis
• . About 70% of discrete thyroid swellings are
clinically isolated and about 30% are dominant.
• The importance of discrete swellings lies in the
risk of neoplasia compared with other thyroid
swellings.
• 15% of isolated swellings prove to be malignant
and an additional 30–40% are follicular
adenomas.
• The remainder are non-neoplastic, largely
consisting of areas of colloid degeneration,
thyroiditis or cysts.
•
Investigation
• THYROID FUNCTION
• If hyperthyroidism ‘toxic adenoma’ or toxic multinodular goitre.
• The combination of toxicity and nodularity is indication for isotope scanning
to localise the area(s) of hyperfunction.
• AUTOANTIBODY TITRES
• chronic lymphocytic thyroiditis.
• ISOTOPE SCAN
• except when toxicity is associated with nodularity.
• ULTRASONOGRAPHY
• ultrasonic features in a thyroid swelling associated with thyroid neoplasia,
including microcalcification and increased vascularity, but only macroscopic
capsular breach and nodal involvement are diagnostic of malignancy.
• FINE-NEEDLE ASPIRATION CYTOLOGY
• FNAC should be used, ideally under ultrasound guidance, . FNAC is reliable in
identifying papillary thyroid cancer but cannot distinguish between a benign
follicular adenoma and follicular carcinoma, as this distinction is dependent
not on cytology but on histological criteria, which include capsular and
vascular invasion. FNAC is both highly specific and sensitive.
• RADIOLOGY
• Plain films have previously been used to assess tracheal
compression and deviation
• CT scanning is also useful if ultrasound has identified
metastatic disease in the neck as it can assist surgical
planning and also assess the superior mediastinum and
lungs
• LARYNGOSCOPY
• Flexible laryngoscopy has rendered indirect laryngoscopy
obsolete and is widely used preoperatively to determine
the mobility of the vocal cords. The presence of a
unilateral cord palsy coexisting with an ipsilateral thyroid
nodule of concern is usually diagnostic of malignant
disease.
• CORE BIOPSY
rarely indicated in thyroid masses
useful in the rapid diagnosis of widely invasive
malignant disease, for example anaplastic
carcinoma, or in the diagnosis of
lymphadenopathy.

• The main indication for operation is the risk of neoplasia, which
includes follicular adenoma as well as malignant swellings.
• 50% of isolated swellings and 25% of dominant swellings should
be removed on the grounds of neoplasia.
• the age and sex of the patient and the size of the swelling may be
relative indications for surgery
• clinical criteria to assist in selection for operation according to the
risk of neoplasia and malignancy…. hard, irregular swelling
…..RLN paralysis……Deep cervical ymphadenopathy The
incidence of thyroid carcinoma in women is about three times
that in men, but a discrete swelling in a male is much more likely
to be malignant than in a female
• The risk of carcinoma is increased at either end of the age range
and a discrete swelling in a teenager of either sex must be
provisionally diagnosed as carcinoma. The risk
• increases as age advances beyond 50 years, more so in males.
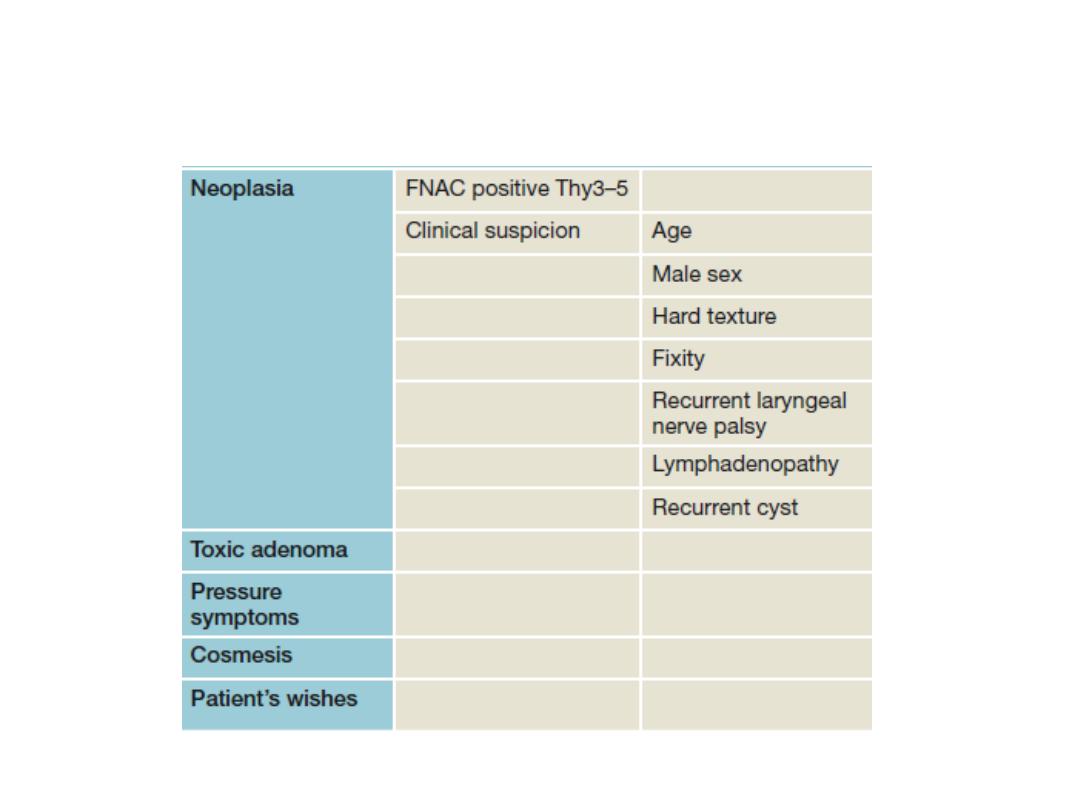
Indications for operation in thyroid swellings
.

•
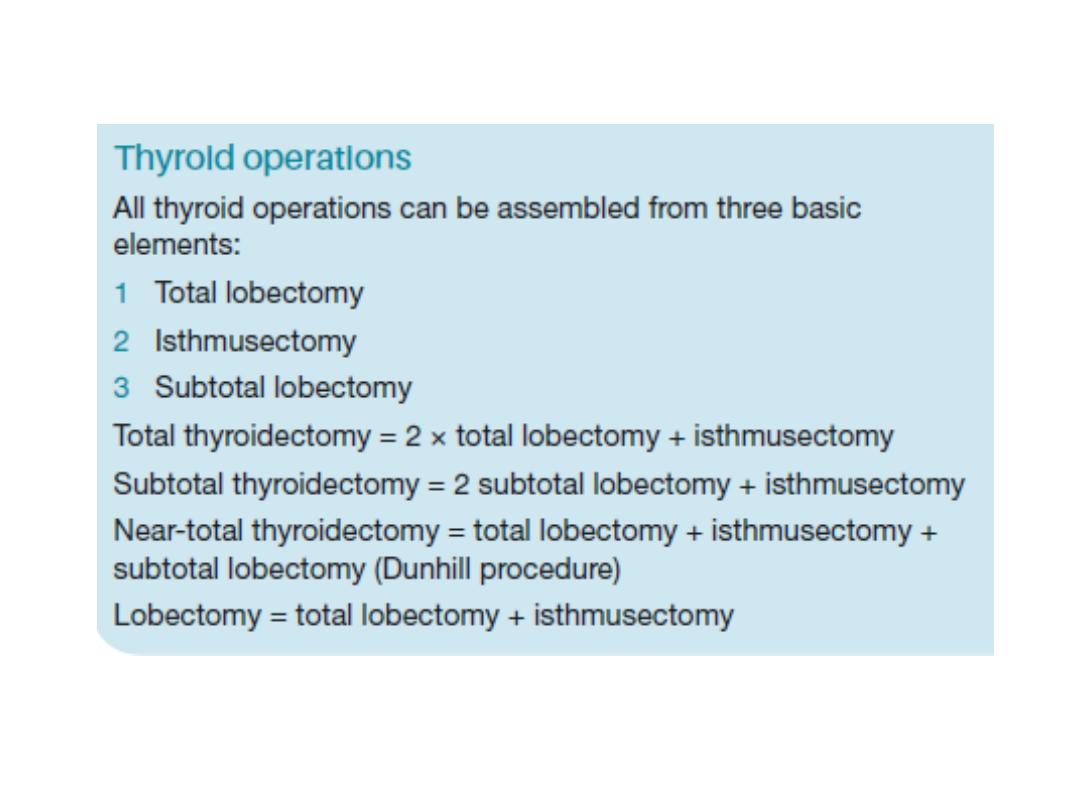
Selection of thyroid procedure
• The choice of thyroid operation depends on:
• ●● diagnosis (if known preoperatively);
• ●● risk of thyroid failure;
• ●● risk of RLN injury;
• ●● risk of recurrence;
• ●● Graves’ disease;
• ●● multinodular goitre;
• ●● differentiated thyroid cancer;
• ●● risk of hypoparathyroidism
.

•
Retrosternal goitre
Arise from the slow growth of a multinodular gland down
in to the mediastinum.
As the gland enlarges within the thoracic inlet, pressure
may lead to dysphagia, tracheal compression and
eventually airway
symptoms.
Patient should be considered for surgery if there is
significant airway compression


• HYPERTHYROIDISM
• Thyrotoxicosis
•
symptoms due to a raised level of circulating thyroid
hormones, is not responsible for all manifestations of
the disease.
• Clinical types
are:
• ●● diffuse toxic goitre (Graves’ disease);
• ●● toxic nodular goitre;
• ●● toxic nodule;
• ●● hyperthyroidism due to rarer causes.
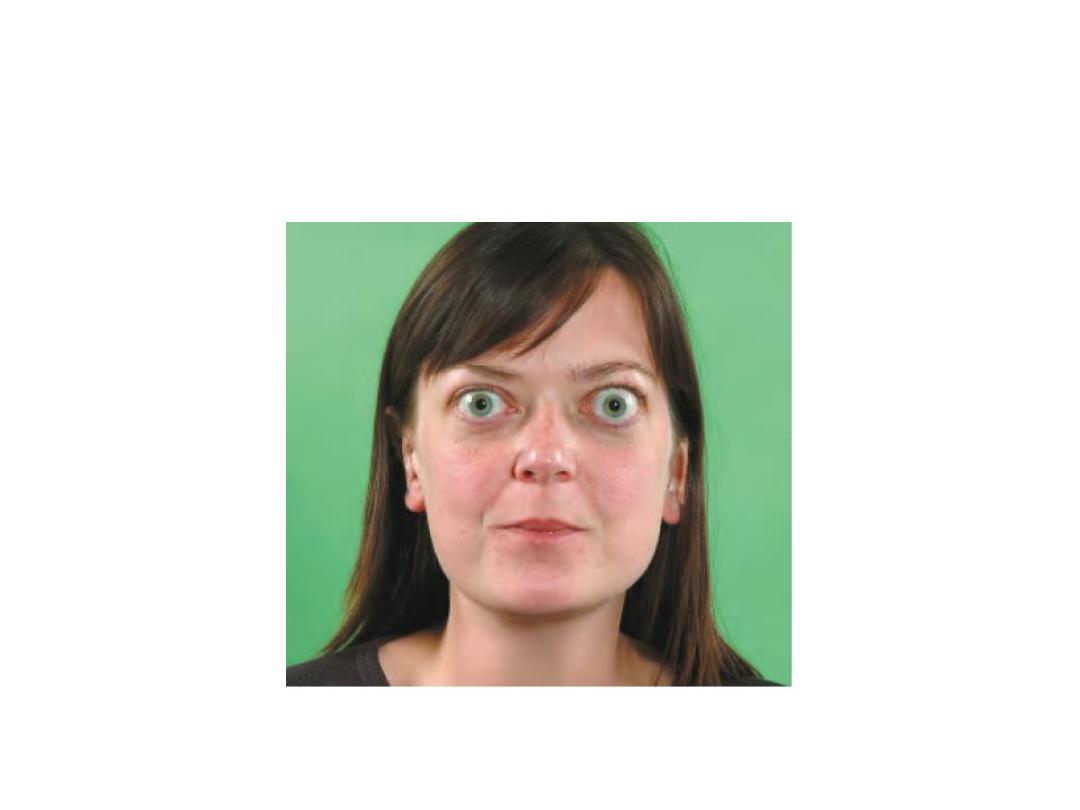
• Clinical features
• The symptoms are:
• • tiredness
• • emotional lability
• • heat intolerance
• • weight loss
• • excessive appetite
• • palpitations.
• The signs of thyrotoxicosis are:
• • tachycardia
• • hot, moist palms
• • exophthalmos
• • eyelid lag/retraction
• • agitation
• • thyroid goitre and bruit.

•
Diffuse toxic goitre
• diffuse vascular goitre appearing at the same
time as hyperthyroidism,
• usually occurs in younger women
• frequently associated with eye signs.
• The syndrome is that of primary thyrotoxicosis
• 50% of patients have a family history of
autoimmune endocrine diseases.

•
Toxic nodular goitre
• A simple nodular goitre is present for a long time
before the hyperthyroidism
• usually in the middle-aged or elderly
• very infrequently is associated with eye signs.
• The syndrome is that of secondary
thyrotoxicosis.

•
Toxic nodule
• solitary overactive nodule, which may be part of a
generalised nodularity or a true toxic adenoma.
• It is autonomous and its hypertrophy and
hyperplasia are not due to TSH-RAb.
• TSH secretion is suppressed by the high level of
circulating thyroid hormones and the normal
thyroid tissue surrounding the nodule is itself
suppressed and inactive.
Graves’ disease.

•
Principles of treatment of thyrotoxicosis
• Non-specific measures are rest and sedation
• specific measures, i.e. the use of antithyroid
drugs, surgery and radioiodine.
• ANTITHYROID DRUGS
• Those in common use are carbimazole and propylthiouracil.
• used to restore the patient to a euthyroid state and to maintain this for
a prolonged period in the hope that a permanent remission will occur,
i.e. that production of thyroid-stimulating antibodies (TSH-RAb) will
diminish or cease.
• Antithyroid drugs cannot cure a toxic nodule.
• ●● Advantages.
• No surgery
• no use of radioactive materials.
• ●● Disadvantages.
• Treatment is prolonged
• failure rate is at least 50%.
• The duration of treatment may be tailored to the severity of the toxicity,
with milder cases
being treated for only 6 months and severe cases for 2 years before
stopping therapy.

• SURGERY
• In diffuse toxic goitre and toxic nodular goitre with overactive
internodular tissue, surgery cures by reducing the mass of overactive
tissue by reducing the thyroid below a critical
• mass.
• Advantages.
• The goitre is removed
• the cure is rapid and the cure rate is high if surgery has been adequate.
• Disadvantages.
• Recurrence of thyrotoxicosis occurs in at least 5% of cases when
subtotal thyroidectomy is carried out.
• There is a risk of permanent hypoparathyroidism and nerve injury.
• Young women tend to have a poorer cosmetic result from the scar.
• Every operation carries a risk, but with suitable preparation and an
experienced surgeon the mortality is negligible and the morbidity low.
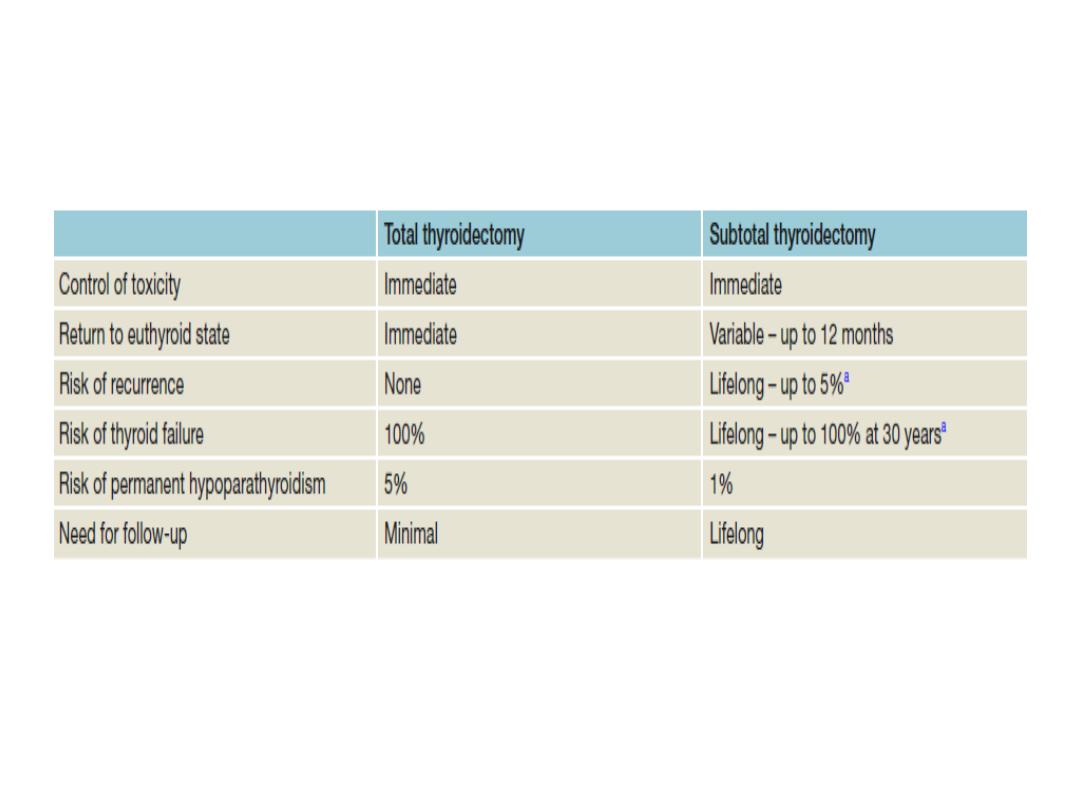
Comparison of surgical options for Graves’ disease
.

• RADIOIODINE
• Radioiodine destroys thyroid cells and, as in thyroidectomy,
reduces the mass of functioning thyroid tissue to below a critical
level.
• ●● Advantages.
• No surgery
• no prolonged drug therapy.
• ●● Disadvantages.
• Isotope facilities must be available.
• The patient must be quarantined while radiation levels are high
and avoid pregnancy and close physical contact, particularly with
children.
• Eye signs may be aggravated.
•
Choice of therapy
• Each case must be considered individually.
• guiding principles on the most satisfactory treatment for
a particular toxic goitre at a particular age be modified
according to the facilities available and the personality
and wishes of the individual patient, business or family
commitments and any other coexistent medical or
surgical condition. Access to post-treatment care and
availability of replacement thyroxine can be important
considerations in resource-poor countries.
• In advising treatment, compliance, influenced by social
and intellectual factors, is important; many patients
cannot be trusted to take drugs regularly if they feel well,
and indefinite follow-up, which is essential after
radioiodine or subtotal thyroidectomy is a burden for all.
• DIFFUSE TOXIC GOITRE
• Most patients have an initial course of antithyroid drugs with radioiodine
for relapse. Exceptions are those who refuse radiation, have large
goitres, progressive eye signs or are pregnant.
• TOXIC NODULAR GOITRE
• Toxic nodular goitre is often large and uncomfortable and enlarges still
further with antithyroid drugs. A large goitre should be treated surgically
because it does not respond as well or as rapidly to radioiodine or
antithyroid drugs as does a diffuse toxic goitre.
• TOXIC NODULE
• Surgery or radioiodine treatment is appropriate.
• Radioiodine is a good alternative for patients over the age of 45 years
because the suppressed thyroid tissue does not take up iodine and thus
there is minimal risk of delayed thyroid insufficiency.
• FAILURE OF PREVIOUS TREATMENT WITH ANTITHYROID DRUGS OR
RADIOIODINE
• In this case, surgery or thyroid ablation with 123I is appropriate.

• Surgery for thyrotoxicosis
•
Preoperative preparation
• aims to make the patient biochemically
euthyroid at operation.
• Preparation is as an out-patient and only rarely
is admission to hospital necessary on account of
severe symptoms at presentation, failure to
control the hyperthyroidism or non-compliance
with medication.

• Carbimazole 30–40 mg per day is the drug of choice for
• preparation.
• When euthyroid (after 8–12 weeks), the dose may be
reduced to 5 mg 8-hourly or a ‘block and replace’ regime
used. In this case, the high dose of carbimazole is
continued to inhibit T3 and T4 production and a
maintenance dose of 0.1–0.15 mg of thyroxine is given
daily. The last dose of carbimazole may be given on the
evening before surgery.
• Iodides are not used alone because, if the patient needs
preoperative treatment, a more effective drug should be
given.

• An alternative method of preparation is to abolish the clinical
manifestations of the toxic state, using β-adrenergic blocking
drugs.
• These act on the target organs and not on the gland itself.
Propranolol also inhibits the peripheral conversion of T4 to T3.
• The appropriate dosages are propranolol 40 mg t.d.s. or the
longer acting nadolol 160 mg once daily.
• Clinical response to β-blockade is rapid and the patient may be
rendered clinically euthyroid and operation arranged in a few days
rather than weeks.
• β-adrenergic blocking drugs do not interfere with synthesis of
thyroid hormones, and hormone levels remain high during
treatment and for some days after thyroidectomy. It is, therefore,
important to continue treatment for 7 days postoperatively.

• Iodine may be given with carbimazole or a β-adrenergic
blocking drug for 10 days before operation.
• Iodide alone produces a transient remission and may
reduce vascularity.
POSTOPERATIVE COMPLICATIONS
1) Haemorrhage
• is the most frequent life-threatening complication of thyroidectomy
• Around 1 in 50 patients will develop a haematoma, and in almost all
cases this will develop in the first 24 hours. If an arterial bleed
occurs, the tension in the central compartment pressure can rise
until it exceeds venous pressure. Venous oedema of the larynx can
then develop and cause airway obstruction leading to death.
• If a haematoma develops, clinical staff should know to remove skin
sutures in order to release some pressure and seek senior advice
immediately.
• Endotracheal intubation should be used to secure the airway while
the haematoma is evacuated and the bleeding point controlled.
•
• 2. Recurrent laryngeal nerve paralysis and voice change
• RLN injury may be unilateral or bilateral, transient or
permanent.
• Injury to the external branch of the superior laryngeal
nerve is more common because of its proximity to the
superior thyroid artery. This leads to loss of tension in
the vocal cord with diminished power and range in the
voice. Patients, particularly those who use their voice
professionally, must be advised that any thyroid
operation will result in change to the voice even in the
absence of nerve trauma.
3.Thyroid insufficiency
Following total thyroidectomy, clearly thyroxine replacement will be
required.
Around one in three patients who has a lobectomy will require
supplementation; rates are higher in those with thyroid autoantibodies.
Subtotal thyroidectomy was at one time performed with the aim of leaving
sufficient tissue to maintain thyroid function.
4.Parathyroid insufficiency
This is due to removal of the parathyroid glands or infarction through
damage to the parathyroid end arteries; The incidence of permanent
hypoparathyroidism should be less than 1% and most cases present
dramatically
2–5 days after operation but, very rarely, the onset is delayed for 2–3
weeks or a patient with marked hypocalcaemia may be asymptomatic. The
complication is limited to total thyroidectomy,
as when lobectomy is performed the contralateral parathyroid glands are
sufficient to maintain calcium levels.
5,Thyrotoxic crisis (storm)
. acute exacerbation of hyperthyroidism.
. occurs if a thyrotoxic patient has been inadequately prepared for
thyroidectomy and is now extremely rare.
Very rarely, a thyrotoxic patient presents in a crisis and this may
follow an unrelated operation.
Symptomatic and supportive treatment is for dehydration,
hyperpyrexia and restlessness. This requires the administration of
intravenous fluids, cooling the patient with ice packs,
administration of oxygen, diuretics for cardiac failure, digoxin for
uncontrolled atrial fibrillation, sedation and intravenous
hydrocortisone.
Specific treatment is by carbimazole 10–20 mg 6-hourly, Lugol’s
iodine 10 drops 8-hourly by mouth or sodium iodide 1g i.v.
Propranolol intravenously (1–2 mg) or orally (40 mg 6-hourly) will
block β-adrenergic effects.
6.Wound infection
Cellulitis requiring prescription of antibiotics
A significant subcutaneous or deep cervical abscess is
exceptionally rare and should be drained.
7.Hypertrophic or keloid scar
This is more likely to form if the incision overlies the sternum
and in dark skinned individuals.
Intradermal injections of corticosteroid should be given at
once and repeated monthly if necessary. Scar revision rarely
results in significant long-term improvement.
8.Stitch granuloma
• This may occur with or without sinus formation and is
seen after the use of non-absorbable, particularly silk,
suture material. Absorbable ligatures and sutures should
be used throughout thyroid surgery. Some surgeons use a
subcuticular absorbable skin suture rather than the
traditional skin clips or staples.
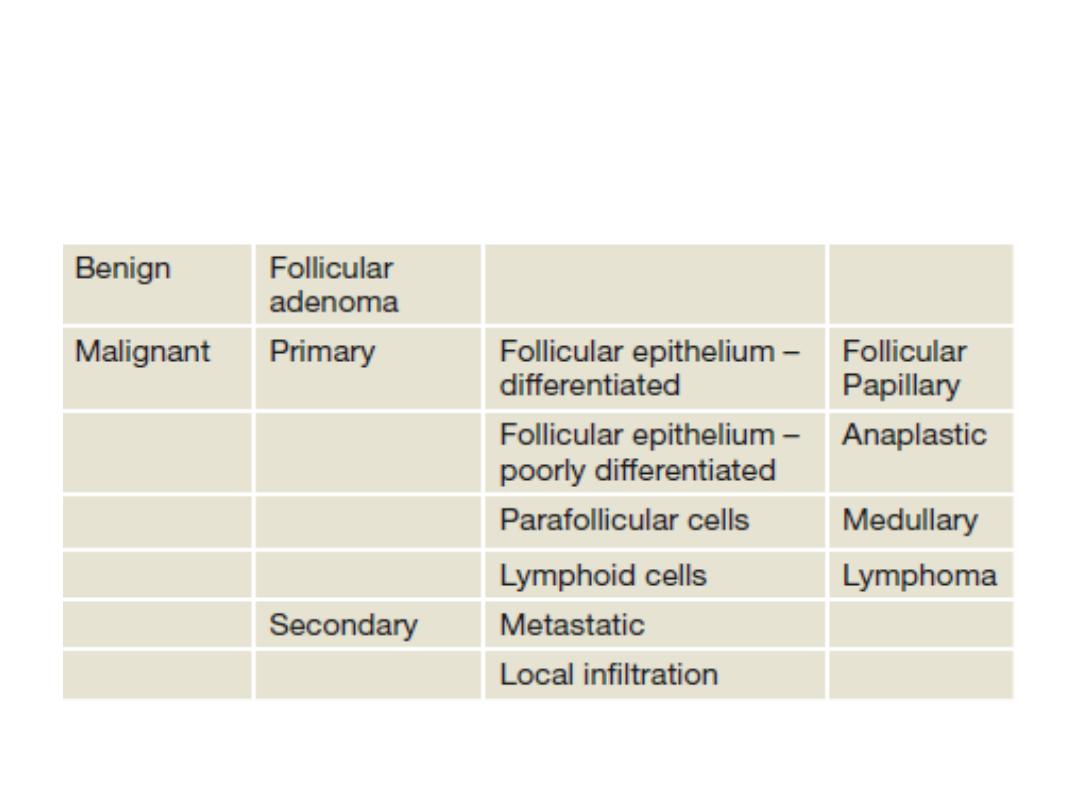
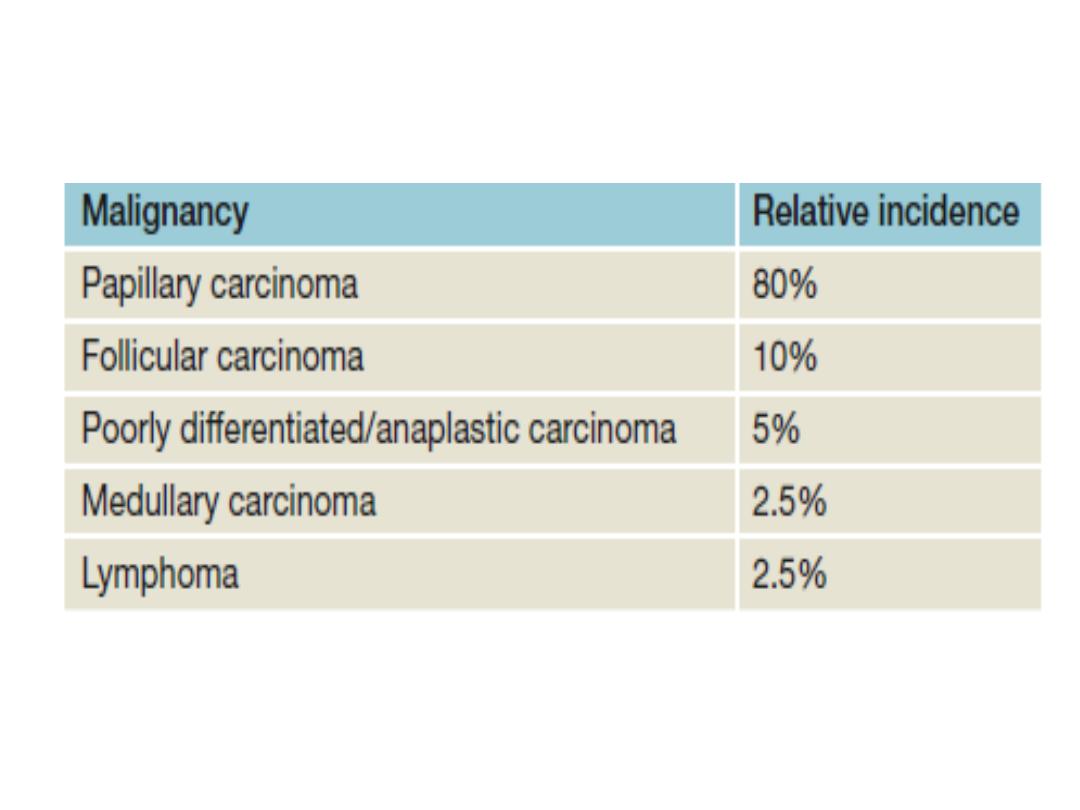
• NEOPLASMS OF THE THYROID
Classification of thyroid neoplasims
• Benign tumours
• Follicular adenomas present as clinically solitary
nodules
• distinction between a follicular carcinoma and an
adenoma can only be made by histological
examination; in the adenoma there is no invasion of
the capsule or of pericapsular blood vessels. For this
reason, FNA, which provides cytologic detail but not
tissue architecture, cannot differentiate between
benign and malignant follicular lesions
• . Diagnosis and treatment is therefore, by wide
excision, i.e. total lobectomy.
• The remaining thyroid tissue is normal so that
prolonged follow-up is unnecessary.

• Malignant tumours
The vast majority of primary malignancies are carcinomas derived
from the follicular cells
Such tumors were thought of as differentiated (papillary, follicular
and Hürthle cell) and undifferentiated (anaplastic).
The parafollicular C cells can undergo malignant transformation
into medullary carcinoma, and thyroid lymphoma is another
primary thyroid malignancy.
the thyroid can be involved by direct spread from surrounding
structures (larynx and oesophagus) or metastases (most
commonly from renal cell carcinoma).
Lymph node and blood-borne metastases of thyroid cancer occur
primarily to bone and lung and may be the mode of presentation


•
Aetiology of malignant thyroid
tumours
• The great majority of thyroid cancers have no known
aetiological factor.
• The most important identifiable aetiological factor in
differentiated thyroid carcinoma (particularly papillary) is
irradiation of the thyroid under 5 years of age.
• Short latency aggressive papillary cancer is associated
with the ret/PTC3 oncogene and later developing,
possibly less aggressive, cancers with ret/PTC1.
• The incidence of follicular carcinoma is high in endemic
goitrous areas, possibly due to TSH stimulation.
• Malignant lymphomas sometimes develop in
autoimmune thyroiditis

• Clinical features of thyroid cancers
• The annual incidence is about 0.6 per million of the population
• The sex ratio is three females to one male.
• The mortality rates remain static at over 80% 5-year survival for all
groups.
• anaplastic carcinoma predicts poor outcome
• differentiated carcinomas generally having excellent outcomes.
• The most common presenting symptom is a thyroid swelling
• Enlarged cervical lymph nodes may be the presentation of papillary
carcinoma (PTC).
• RLN paralysis is very suggestive of locally advanced disease.
• Anaplastic growths are usually hard, irregular and infiltrating.
• A differentiated carcinoma may be suspiciously firm and irregular, but is
often indistinguishable from a benign swelling.
• Small papillary tumours may be impalpable, even when lymphatic
metastases are present.
• Pain, often referred to the ear, is suggestive of nerve involvement from
infiltrating
• tumours.

• Diagnosis of thyroid neoplasms
• Clinical history and examination continue to be the cornerstone of
diagnosis of thyroid neoplasms.
• radiation exposure and family history
• Examination of the central neck and regional lymphatics should
be combined with assessment of vocal cord function.
• Biochemical assessment of thyroid function
• Following initial assessment, the next step is ultrasound.
• This non-invasive investigation is most accurate at assessing
thyroid swellings. Not only can a judgement be made on the
presence, size and number of thyroid nodules present, but an
estimate of risk of malignancy can be made depending on these
findings.
• Following ultrasound, lesions can be categorised as benign,
indeterminate or malignant. Benign lesions require no further
assessment unless surgery is considered for compressive
symptoms.
• Indeterminate or malignant lesions should be investigated with
FNAC
.
• Occasionally, the surgeon will encounter a thyrotoxic
patient. Such cases are one of the few indications for a
radioiodine uptake scan. This allows assessment of the
function of a nodule. Hot nodules are very rarely
malignant. Cold nodules will require assessment as for all
other thyroid neoplasms.
• Following clinical, ultrasound and cytological
assessment, the vast majority of lesions will be
characterised as benign, malignant or indeterminate.
Further treatment will be planned accordingly.

• Papillary carcinoma
• is the most common thyroid malignancy.
• its propensity for lymph node metastases.
• more common in younger patients
• Distant metastases are uncommon in PTC.
• ‘papillary microcarcinoma’. This term is used to
describe PTC that is <10 mm in size. These lesions are
common (detected in about 10% of benign thyroid
resections) and not associated with adverse outcomes,
including recurrence or non-survival.

• Follicular carcinoma
• Follicular carcinoma can normally only be differentiated
from follicular adenoma by the architecture on histology.
For this reason, follicular lesions on FNA are unable to be
diagnosed as malignant in the absence of clinical features
such as metastases
• Multiple foci of follicular carcinoma are seldom seen and
lymph node involvement is much less common than in
papillary carcinoma.
• Blood-borne metastases are more common and the
eventual mortality rate, although still low, is twice that of
papillary cancer
• Hürthle cell tumours are a rare variant of follicular
neoplasm in which oxyphil (Hürthle, Askanazy) cells
predominate histologically. Hürthle cell cancers are
associated with a poorer prognosis.

• Prognosis in differentiated thyroid carcinoma
• The prognosis in differentiated thyroid carcinoma
compared to most cancers is excellent.
• prognosis is much more dependent on age at
diagnosis, size of the tumour, metastatic disease and
the presence of either extrathyroidal spread (in
papillary cancer) or major capsular transgression (in
follicular carcinoma).
• scoring systems all of which identify the group of
patients at high (40 per cent at 20 years) or low (1
per cent at 20 years) risk of death
• All patients should be TNM staged and this
classification acknowledges the low risk of patients
aged less than 45 years at presentation

Surgical treatment
• Total thyroidectomy is recommended for
tumours greater than 2 cm and those with
nodal involvement or metastases and
lobectomy for the remainder.

Additional measures
•
Thyroxine
• thyroxine in a dose of 0.1– 0.2 mg daily, to suppress
endogenous TSH production, for all patients after
operation for differentiated thyroid carcinoma on the
basis that most tumours are TSH dependent.
•
Radioiodine
• The indications for scanning after operations for
differentiated carcinoma are also disputed, but
radioiodine is indicated in patients with unresectable
disease, local recurrence or metastatic disease, high-
risk patients, and in those with a rising serum
thyroglobulin level.
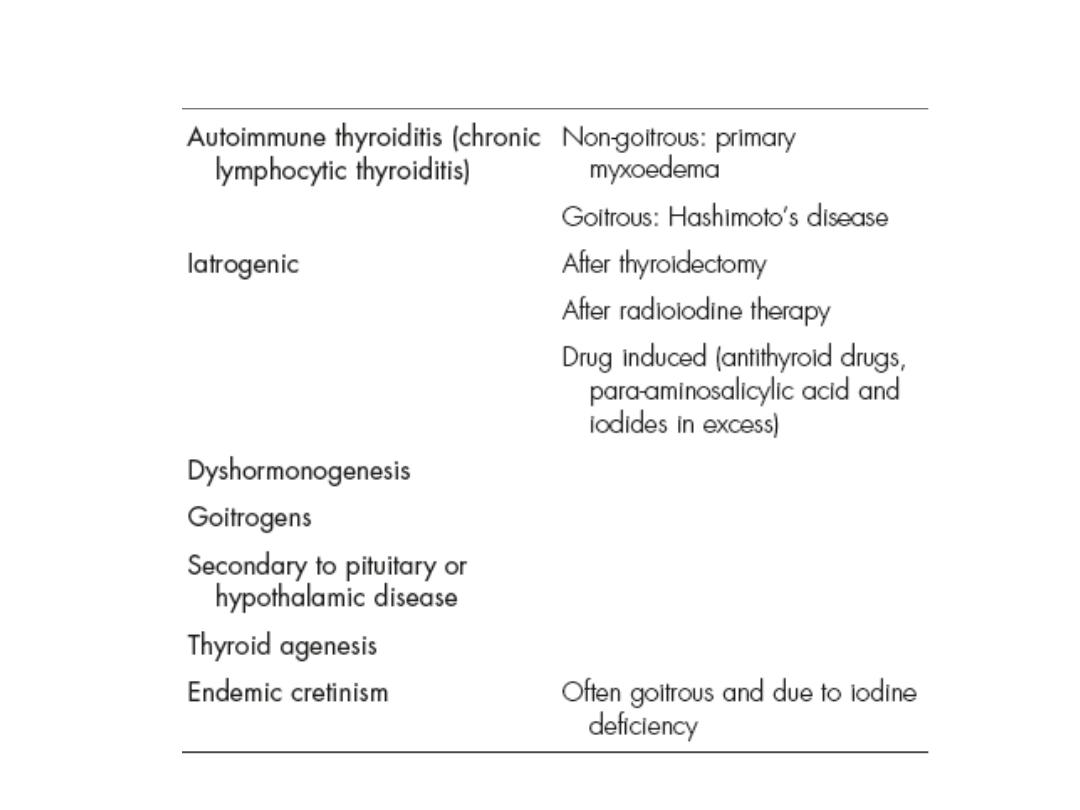
HYPOTHYROIDISM

• Adult hypothyroidism
• The term myxoedema should be reserved for severe thyroid
failure and not applied to the much more ommon mild thyroid
deficiency.
• The signs of thyroid deficiency are:
• • bradycardia • cold extremities • dry skin and hair •
periorbital puffiness • hoarse voice • bradykinesis, slow
movements • delayed relaxation phase of ankle jerks.
• The symptoms are:
• • tiredness • mental lethargy • cold intolerance • weight
gain • constipation • menstrual disturbance • carpal tunnel
syndrome.

•
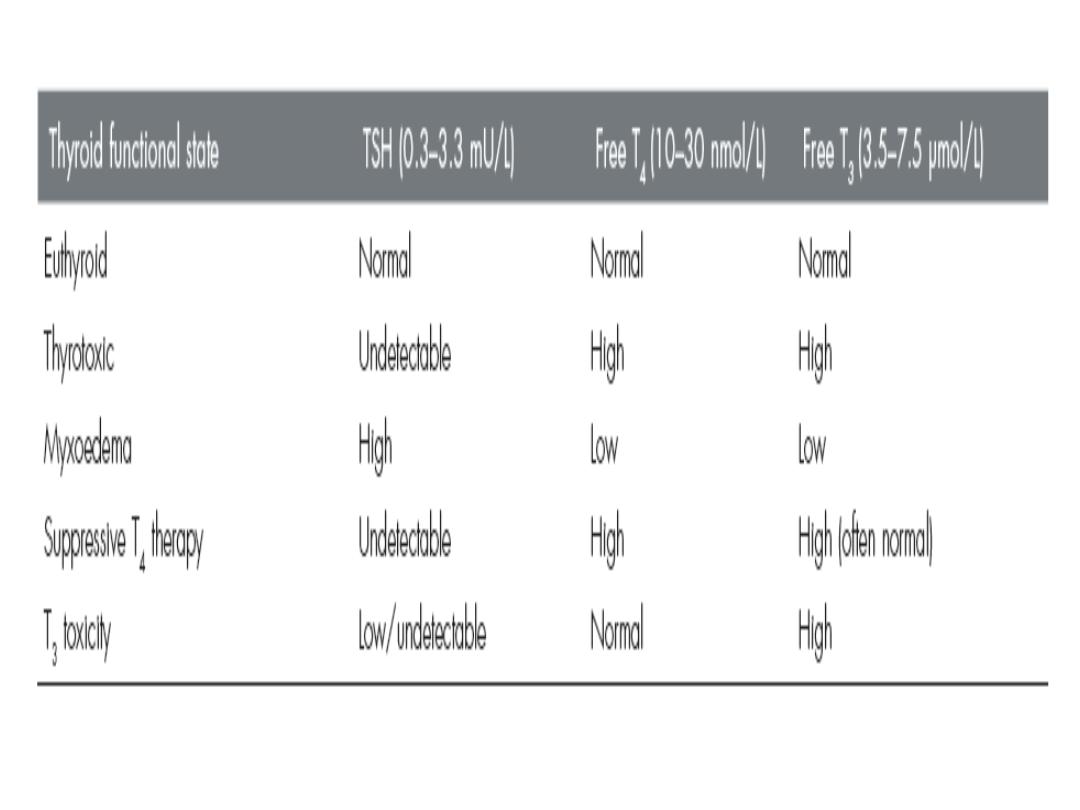
Thyroid function tests
• These show low T4 and T3 levels with a high
TSH (except in the
• rare event of pituitary failure)
• High serum levels of TPO antibodies are
characteristic of autoimmune disease.
•
Treatment
• Oral thyroxine (0.10–0.20 mg) as a single daily
dose is curative.

•
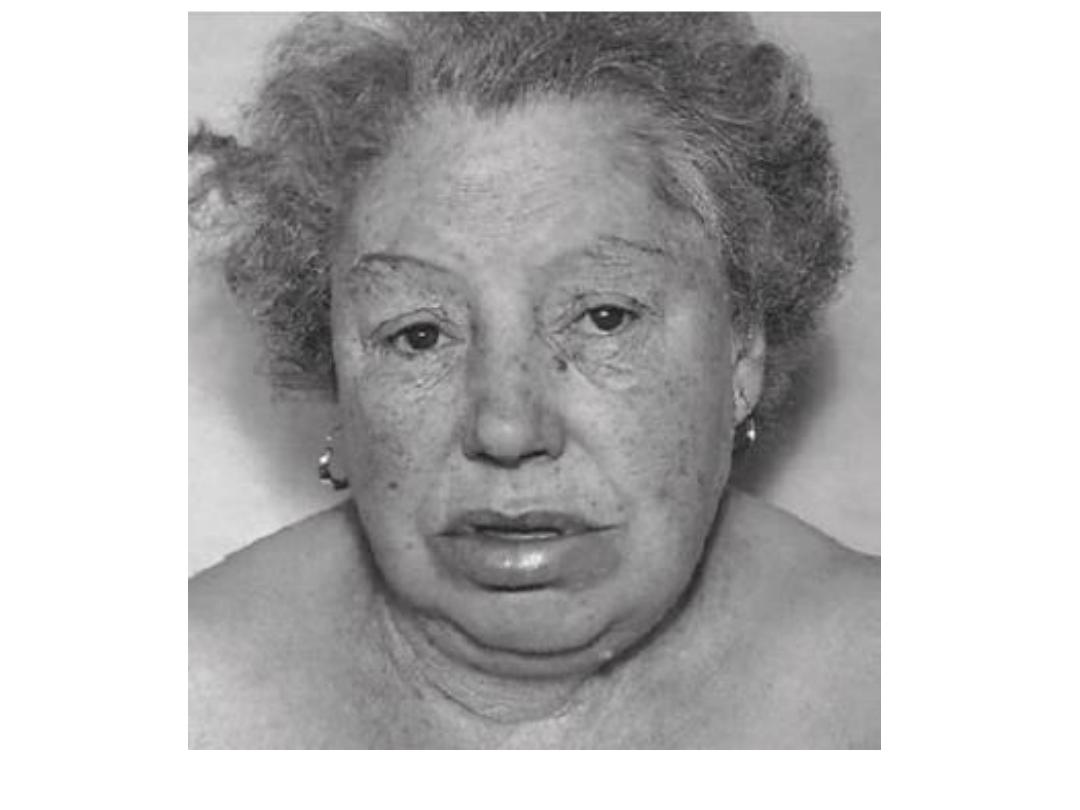
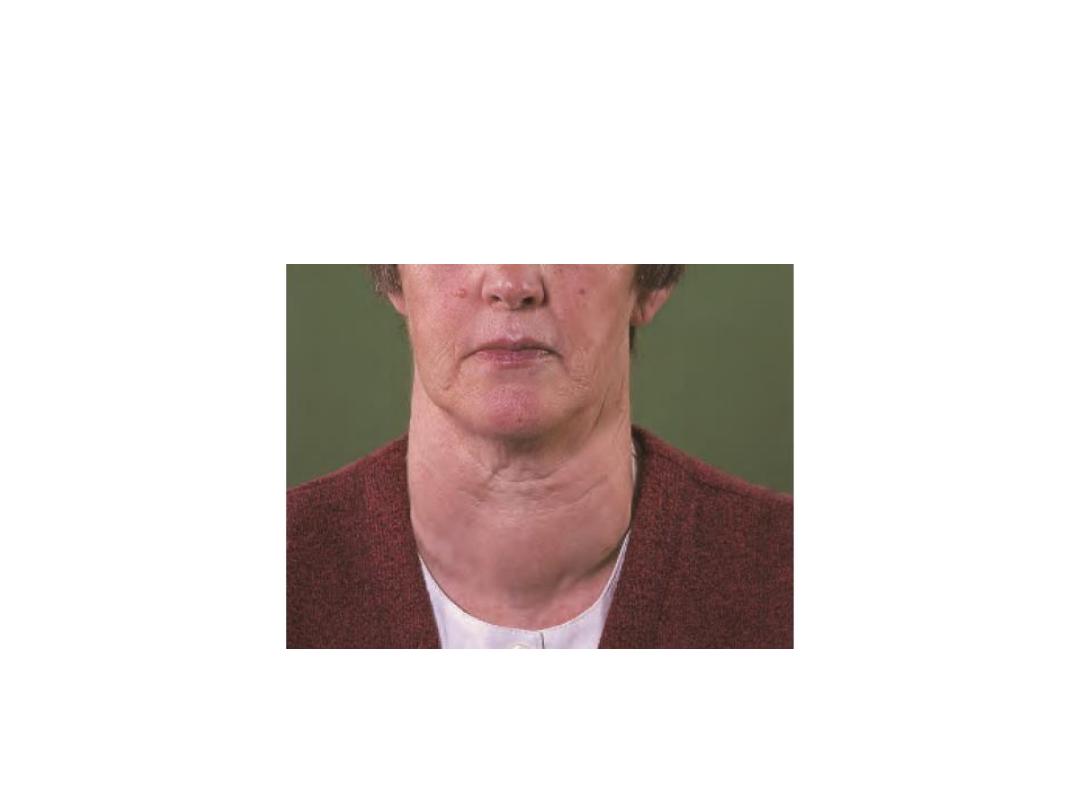
Myxoedema
• The signs and symptoms of hypothyroidism are accentuated. The
facial appearance is typical, and there is often supraclavicular
puffiness, a malar flush and a yellow tinge to the skin .
• Myxoedema coma, characterised by altered mental state,
hypothermia and a precipitating medical condition, for example
cardiac failure or infection, carries a high mortality.
• Treatment
• thyroid replacement, either a bolus of 0.50 mg of T4 or 10 μg of
T3 either i.v. or orally every 4–6 hours. If the body temperature is
less than 30°C, the patient must be warmed slowly.
• Intravenous broad-spectrum antibiotics and hydrocortisone (in
divided doses) are recommended.
• Primary or atrophic myxoedema is considered to be an
autoimmune disease similar to chronic lymphocytic (Hashimoto’s)
thyroiditis but without goitre formation.
• Delay in diagnosis is common and the degree of hypothyroidism is
usually more severe than in goitrous autoimmune thyroiditis
.