
THE PARATHYROID
GLANDS

PRIMARY
HYPERPARATHYROIDISM
is commonly a sporadic rather than familial
condition
associated with hypercalcaemia and
inappropriately raised serum PTH levels due
to enlargement of one or more glands and
hypersecretion of PTH.
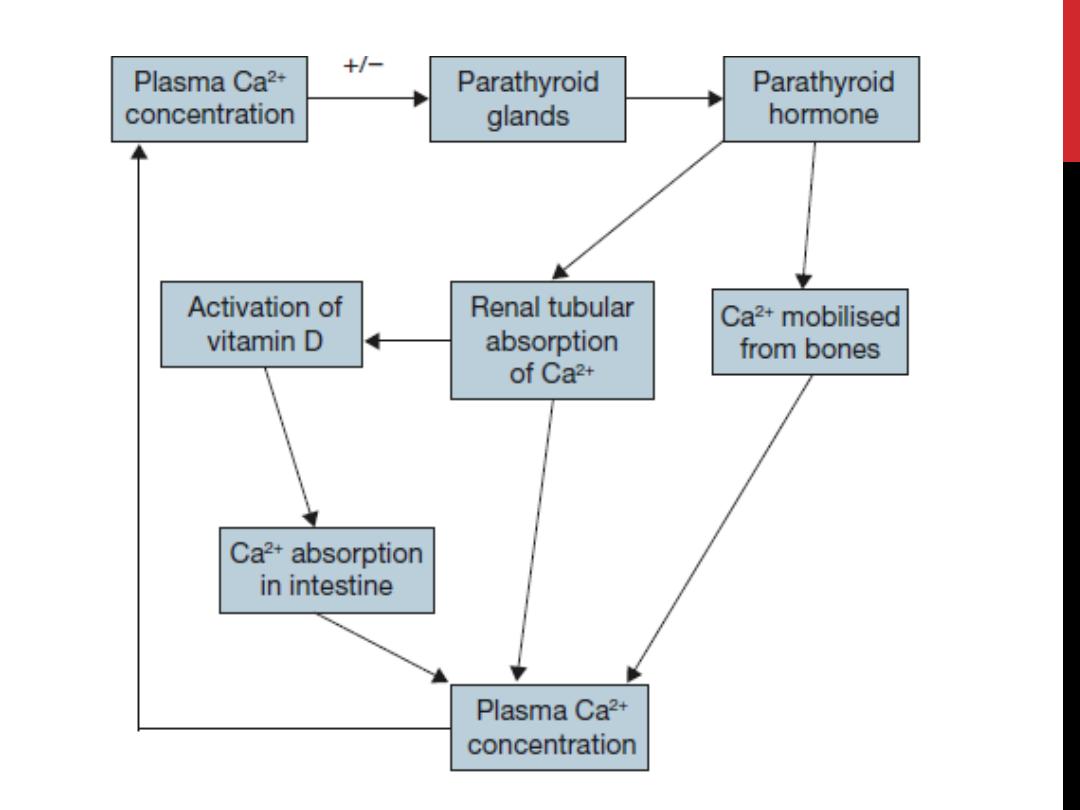
The normal response to hypercalcaemia is
PTH suppression.

Epidemiology
The prevalence of sporadic primary
hyperparathyroidism increases with age and affects
women more than men.
Approximately 1 per cent of adults are
hypercalcaemic on biochemical screening.
Familial hyperparathyroidism occurs as part of the
following genetically determined conditions:
• MEN1 (multiple endocrine neoplasia type 1:
Werner’s syndrome);
• MEN2A (Sipple syndrome), rarely in MEN2B;
• Familial hyperparathyroidism
.

Pathology
In sporadic disease …….85 per cent have a
single adenoma,
………………………………13 per cent have
hyperplasia affecting all four glands
……………………………. 1 per cent will have
more than one adenoma or a carcinoma.
In familial disease, multiple gland
enlargement is usual.

Clinical presentation
The classic quartet of ‘stones, bones, abdominal groans and psychic
moans’
Patients are typically identified incidentally with an elevated total calcium or
following routine assessment of bone densitometry (DEXA scan).
Most patients will have some vague constitutional symptoms, such as
fatigue, muscle weakness, depression or some mild memory impairment on
questioning.
The presence of kidney stones remains the most common clinical
manifestation of symptomatic PHPT. Between 15% and 20% of patients will
have nephrolithiasis and over 40% of patients will have hypercalciuria.
postmenopausal women present with significant osteopenia or
osteoporosis in the distal one-third of the radius with a minimal reduction in
the lumbar spine
PHPT may present with pancreatitis, although it is rarely seen in patients
with milder forms of the disease.
Common epidemiologically linked disorders, such as hypertension and
peptic ulcer disease, are often encountered.
Clinical examination is usually normal. Band keratopathy, pathognomonic
of
the disease and due to deposition of calcium phosphate crystals in the
cornea, is now rarely identified.
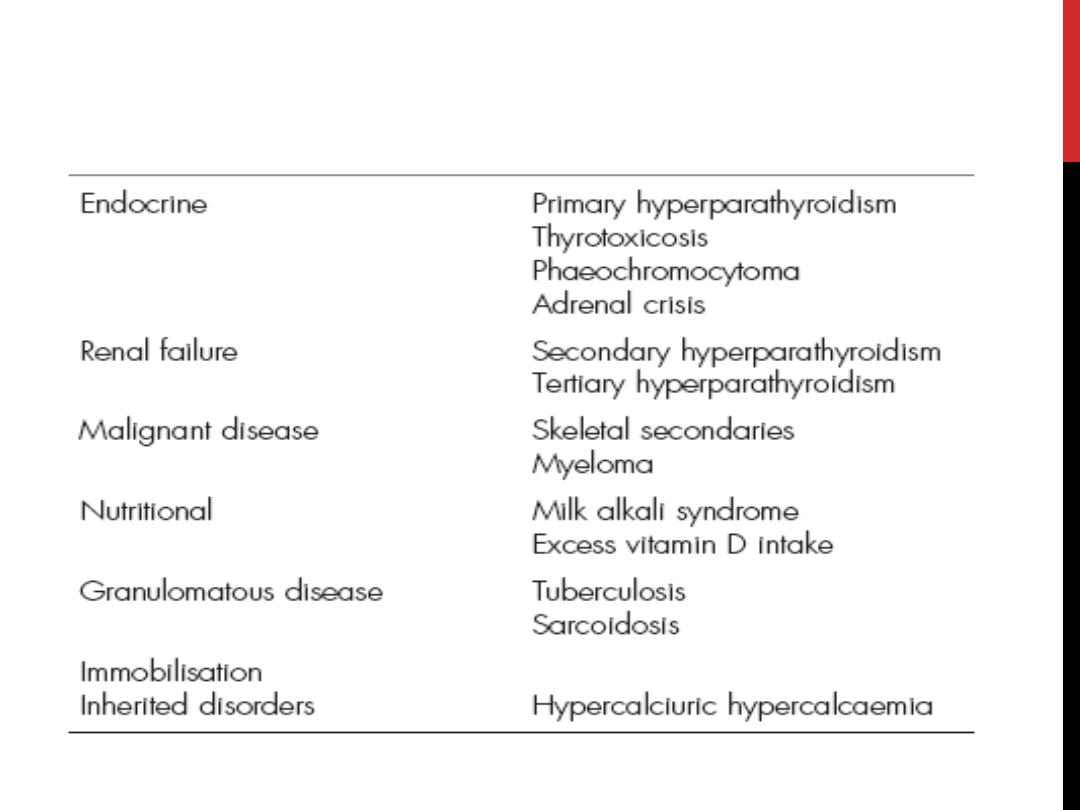
THE DIFFERENTIAL DIAGNOSIS OF PHPT
INCLUDES OTHER CAUSES
OF HYPERCALCAEMIA

Diagnosis
PHPT is a biochemical diagnosis.
Only when the disease has been confirmed biochemically should
localisation studies be
undertaken.
elevated total, or more specifically ionised, calcium,
elevated PTH.
It is associated with a low serum phosphate in the setting of normal
creatinine and vitamin D levels;
24-hour urinary excretion of calcium may be normal or elevated. It is
important to perform a 24-hour urinary collection to rule out the
presence of the rare familial hypocalciuric
hypercalcaemia.
Alkaline phosphatase may be elevated in patients in whom there is
concomitant bone disease. This is important to recognise
preoperatively, as the surgeon should anticipate significant
postoperative hypocalcaemia due to the development of hungry
bone syndrome.

Treatment of primary
hyperparathyroidism
surgery is the only curative option
medical strategies and therapies, particularly in mild
hyperparathyroidism,
which include simple expectant treatment until the calcium
level or symptoms reach a level at which surgery becomes
more attractive, low calcium diet, withdrawal of drugs
(diuretics and lithium) which aggravate hypercalcaemia and,
more recently, calcium reducing agents such as
bisphosphanates and the calcium receptor agonist cinacalcet.
Occasionally, patients present with a parathyroid crisis and
severe hypercalcaemia (serum calcium greater than 3.5
mmol/L). This results in confusion, nausea, abdominal pain,
cardiac arrhythmias and hypotension with acute renal failure.
Intravenous saline and bisphosphonate therapy (pamidronate)
are required to correct the dehydration and hypercalcaemia.

Indications for operation
1)Urinary tract calculi
2)Reduced bone density
3)High serum calciuma
4)? All in younger age group
<50 years
5)Deteriorating renal function
6)Symptomatic hypercalcaemia

Consent for surgery
Preoperative discussion must include the
possibilities of:
1)
• persistent hyperparathyroidism (5
per cent);
2)
• recurrent laryngeal nerve injury (1
per cent);
3)
• postoperative haemorrhage (1 per
cent);
4)
• permanent hypoparathyroidism;
5)
• recurrent hyperparathyroidism

Preoperative localisation
1)
High frequency neck ultrasound is non-
invasive and should identify 75 per cent of
enlarged glands.
2)
Technetium-99m (99mTc)-labelled sestamibi
(MIBI) isotope scans also identify 75 per
cent of abnormal parathyroid glands.
3)
Single-photon emission computed
tomography (SPECT) gives a three-
dimensional image which may influence the
surgical approach.
4)
CT, PET and MRI imaging are not indicated
prior to first-time neck exploration
.

Secondary hyperparathyroidism
Chronic renal failure results in secondary
hyperparathyroidism.
The kidney cannot convert vitamin D into the physiologically
active 1,25-cholecalciferol. Reduced intestinal absorption of
calcium resulting in a low serum calcium and elevated
phosphate due to renal failure to excrete phosphate increases
secretion of parathyroid hormone.
Prolonged stimulation results in parathyroid hyperplasia.
Initially this is reversible following renal transplantation but
when autonomous hyperfunction progresses after
transplantation this is termed tertiary hyperparathyroidism.
Secondary hyperparathyroidism also occurs in vitamin D-
deficient rickets, malabsorption and
pseudohypoparathyroidism.

Clinical and biochemical
features
These include bone pain, pruritus, muscle
weakness, renal osteodystrophy and soft-
tissue calcification
Calciphylaxis (calcific uremic arteriolopathy)
is the end stage of this condition with
arteriolar occlusion resulting in cutaneous
ulceration and gangrene.
The systemic effects of these changes
results in a high mortality and urgent
parathyroidectomy may be required if the
PTH is excessively high.

Treatment
Medical treatment of secondary hyperparathyroidism
includes
dietary phosphate restriction, calcium and vitamin D
supplementation.
Cinacalcet is not recommended except in patients
unfit for surgery.
Surgery is indicated when there is an excessive rise
in the calcium/phosphate product and serum PTH.
Patients are prepared with high-dose vitamin D
(calcitriol) to reduce the severity of the profound
hypocalcaemia which would otherwise follow
parathyroidectomy.
Preoperative dialysis is obligatory.
