1
GASTROINTESTINAL TRACT Lec 5-6 TUCOM-DEP. OF PATHOLOGY
Disorders of the Stomach
CONGENITAL ANOMALIES:
1- Diaphragmatic Hernia.
2- pyloric stenosis.
3- Pancreatic and gastric heteretopia.
Diaphragmatic Hernia.
Weakness or partial to total absence of a region of a diaphragm,
usually on the left may permit the abdominal content to herniate into
the thorax. (away from hiatal orifice).
In utero, neonatal, adult presentation.
Differ from the hiatal hernia in that the defect in the diaphragm does
not involve the hiatal orifice.
Hernial wall composed of peritoneum and pleura.
Usually the stomach or small bowel and even part of liver accompany
it, lethal respiratory embarrassment in the newborn.
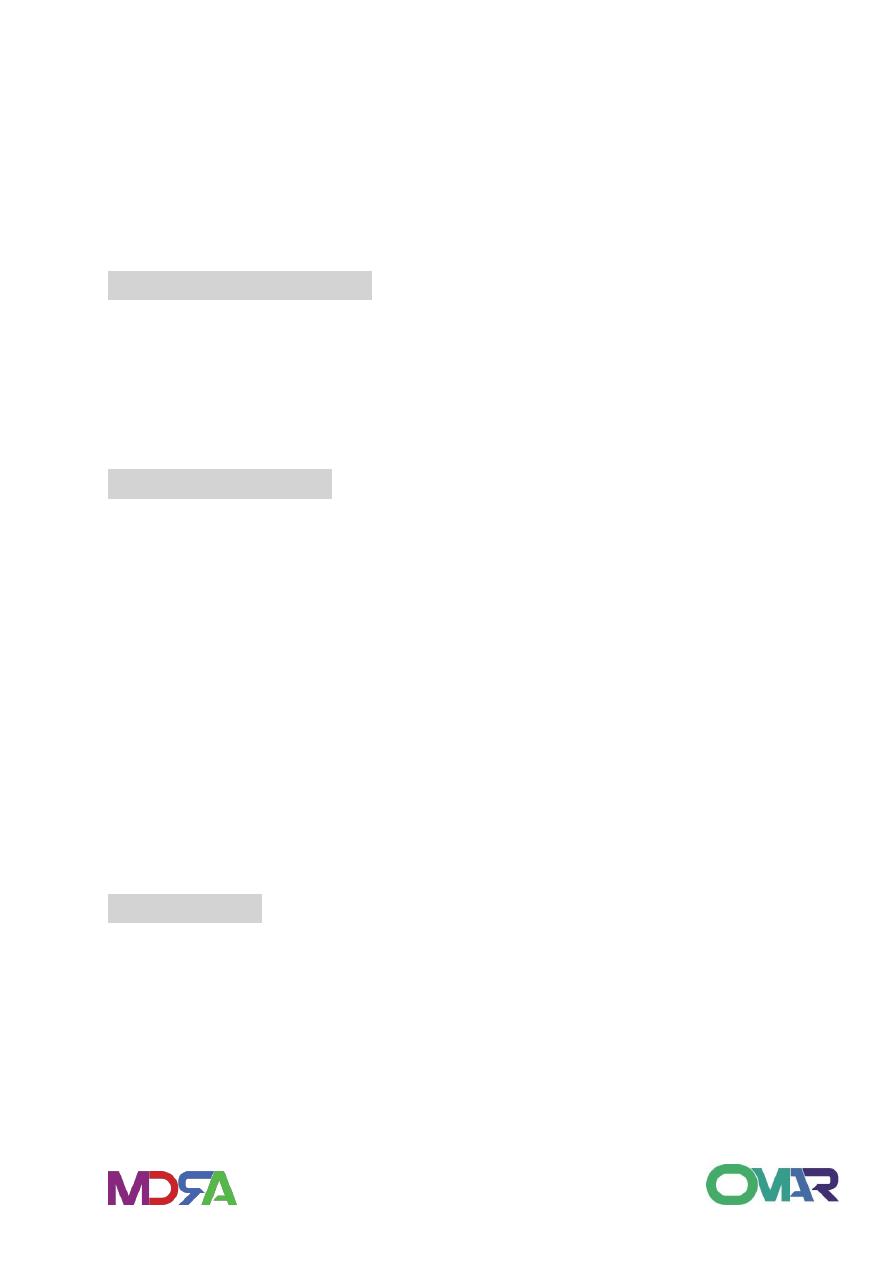
Pyloric stenosis
Called as congenital hypertrophic pyloric stenosis.
Affects male three to four times more often than females.
2
Congenital Hypertrophic Pyloric Stenosis:
• Clinical manifestations
Symptoms develop during third and
fourth week of life or in second week.
Non bilious vomiting
Vomiting increases in frequency and
becomes projectile
• Diagnosis
History
Palpated firm, ovoid palpable mass in the epigastrium with visible
peristalsis.
Occur due to hypertrophy and possibly hyperplasia of the muscularis
properia of pylorus.
GASTRITIS
DEF: inflammation of gastric mucosa.
ACUTE G:
.transient.
.hemorrhage into mucosa.
.asymptomatic, may cause nausea, vomiting and epigastric pain or
bleeding in severe cases.
.Micro. Neutrophilic infiltration, erosion, and purulent exudate.
3
PATHOGENESIS:
• .Heavy use of NSAIDs especially aspirin.
• .Excessive alcohol consumption.
• .heavy smoking.
• .Chemotherapy, uremia, systemic infections.
• .Severe stress, (trauma, burn, surgery).
• .Ischemia, suicidal, (acid and alkali).
• .Irradiation.
• .intubation.
• (increase acid sec, decrease bicarbonate, direct damage to mucus
layer, damage to epithelium).
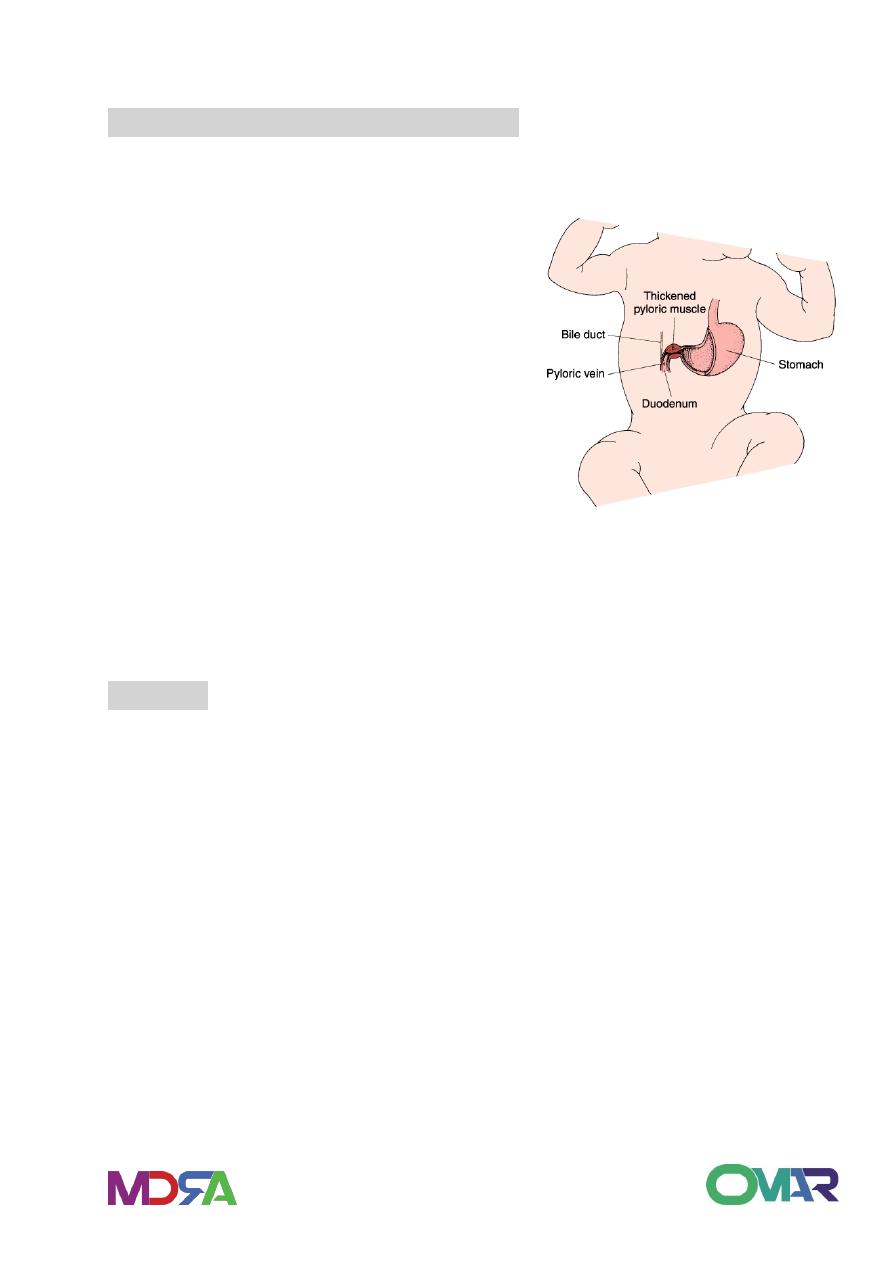
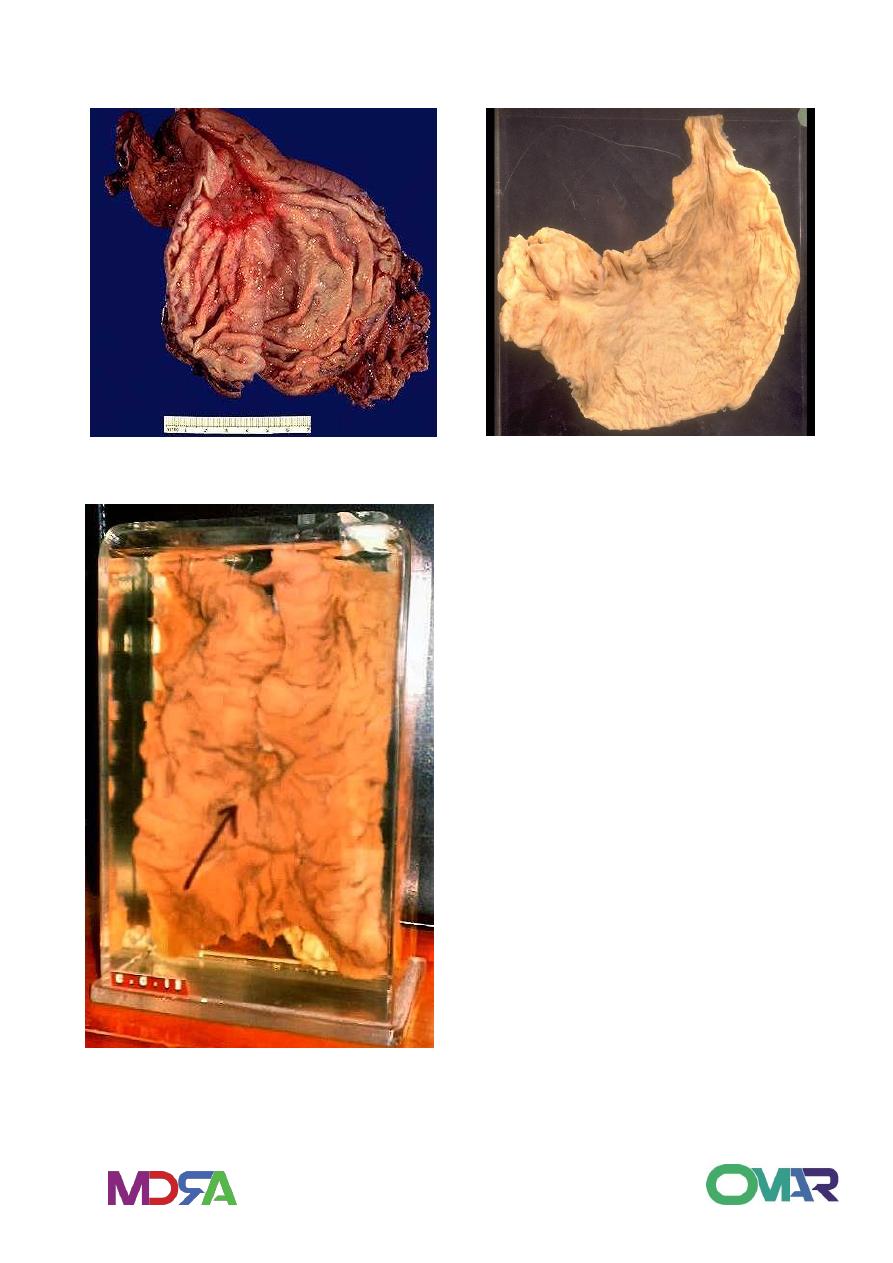
Acute Esophagitis & Gastritis
CHRONIC GASTRITIS
Is the presence of chronic mucosal inflammatory changes leading
eventually to mucosal atrophy and epithelial metaplasia, usually in the
absence of erosions.
Pathogenesis:
.The major etiologic associations are:
1- pernicious anemia. (immunologic)
2- chronic infection (H. pylori).

4
3- Toxic. (alcohol, cigarette).
4- post surgical ( antrectcomy and gastro enterostomy)
5- motor and mechanical.
6- radiation.
7- granulomatous conditions.
8- Miscellaneous ( graft VHD , amyloidosis, uremia).
AUTOIMMUNE GASTRITIS:
CALLED AS DIFFUSE CORPORAL ATROPHIC GASTRITIS:
Auto antibodies = parietal cells and intrinsic factor.
result in gland destruction and atrophy and loss of acid production.
IF Ab == PA.
Associated with other autoimmune diseases.
CHRONIC INFECTION:
S- shaped G- ve.
antrum and corpus.
increase with age, with 50% of asymptomatic adults over 50 Y.
mechanism in gastritis unclear but may be H. pylori colonization of
mucosa may be damaged by other events leads to retarded healing
and inflammation.
also role of metabolic cellular alterations due to infection, bacterial
toxins, and host inflammatory response.
RESPONSE TO ANTIMICROBIALS.
risk of ulcer and cancer.

5
MORPHOLOGY
GROSS:
reddened, coarser texture than normal. May be flattening of the
mucosa. Sometimes, there is thick folds.
differ according to type or cause or severity of the disease.
Microscopy:
In early stages there is lymphocytes and plasma cell infiltration in
lamina properia, if limited to upper third = chronic superficial gastritis.
In severe cases there is inflammatory cell infiltration in all mucosa
thickness with lymphoid aggregates.
Additional features include:
1- activity: if neutrophils, active gastritis.
2- regenerative changes: enlarged hyperchromatic cells with mitotic
activity in mucosal cells.
3- metaplasia: columnar absorptive cells, goblet intestinal cells.
4- atrophy: loss in glandular structure .
5- H pylori found on mucosal cells seen by different stains in antrum
of 95% of active cases, but absent in areas of intestinal metaplasia.
6- dysplasia cytologic changes with atypia in severe cases.
Clinical features
Nausea, vomiting and upper abdominal discomfort.
With severe parietal loss in autoimmune gastritis hypochlorhydria and
achlorhydria.
Circulating gastric autoantibodies.
Pernicious anemia in 10%.
Relation with peptic ulcer.
Long term risk of carcinoma in gastric atrophy in
about 2-4%.
6
Gastric ulceration
Definition:
Ulceration (breach in mucosa) due to acid & pepsin attack – peptic
ulcer.
Esophagus & Stomach Normal Normal Stomach
1-Peptic ulcer
Is a chronic, most often
solitary, lesions that
occur in any portion of
the
gastrointestinal
tract exposed to the
aggressive action of
acid-
Etiology of PUD
Normal
Increased Attack
Hyperacidity
Weak defense
Helicobacter
pylori*
Stress, drugs,
smoking
7
Imbalance between gastroduodenal mucosal defense mechanisms and
the damaging forces.
Etiology:
Helicobacter pylori infection.
Hyperacidity - eg. Zollinger Ellison. (increased gastrin and acid
secretion).
Drugs - anti-inflammatory (NSAIDs) & impaired defense cause
suppression of prostaglandin synthesis, and direct irritative.
Corticosteroids promote ulcer.
Cigarette smoking impairs healing and favors recurrence.
Rapid gastric emptying
Personality and stress
Alcohol in cirrhotic patients.
Pathogenesis:
1-Helicobacter pylori infection
Colonization of gastric mucous
Urease ammonia neutralization of acid Rebound acid
production.
Protease – Mucous and glycoprotein break down.
Weak mucosal resistance
Acid & Pepsin digestion of mucosa
Deeper than just mucosa
Single, punched out, clean base.
Chronic Ulceration
Most common infection in the world (20%)
8
10% of men, 4% women develop PUD *
Positive in 70-100% of PUD patients.
H.pylori related disorders:
Chronic gastritis – 90%
Peptic ulcer disease – 95-100%
Gastric carcinoma – 70%
Gastric lymphoma
Reflux Oesophagitis.
Non ulcer dyspepsia
Gram negative, Spiral bacilli
Spirochetes
Do not invade cells – only mucous
Breakdown urea - ammonia
Break down mucosal defense
Chronic Superficial inflammation
2- Gastric acid and pepsin

9
Peptic Ulcer Morphology:
90% ulcers in first portion of duodenum or lesser curvature of
stomach(4:1).
80 to 90% cases single ulcer. Round Small ulcers with sharply
punched out edges* It has a smooth clean base with puckering of
surrounding mucosa and the mucosal folds are radiating from the
crater in a spoke like fashion.
Small <2cm, clean base*.
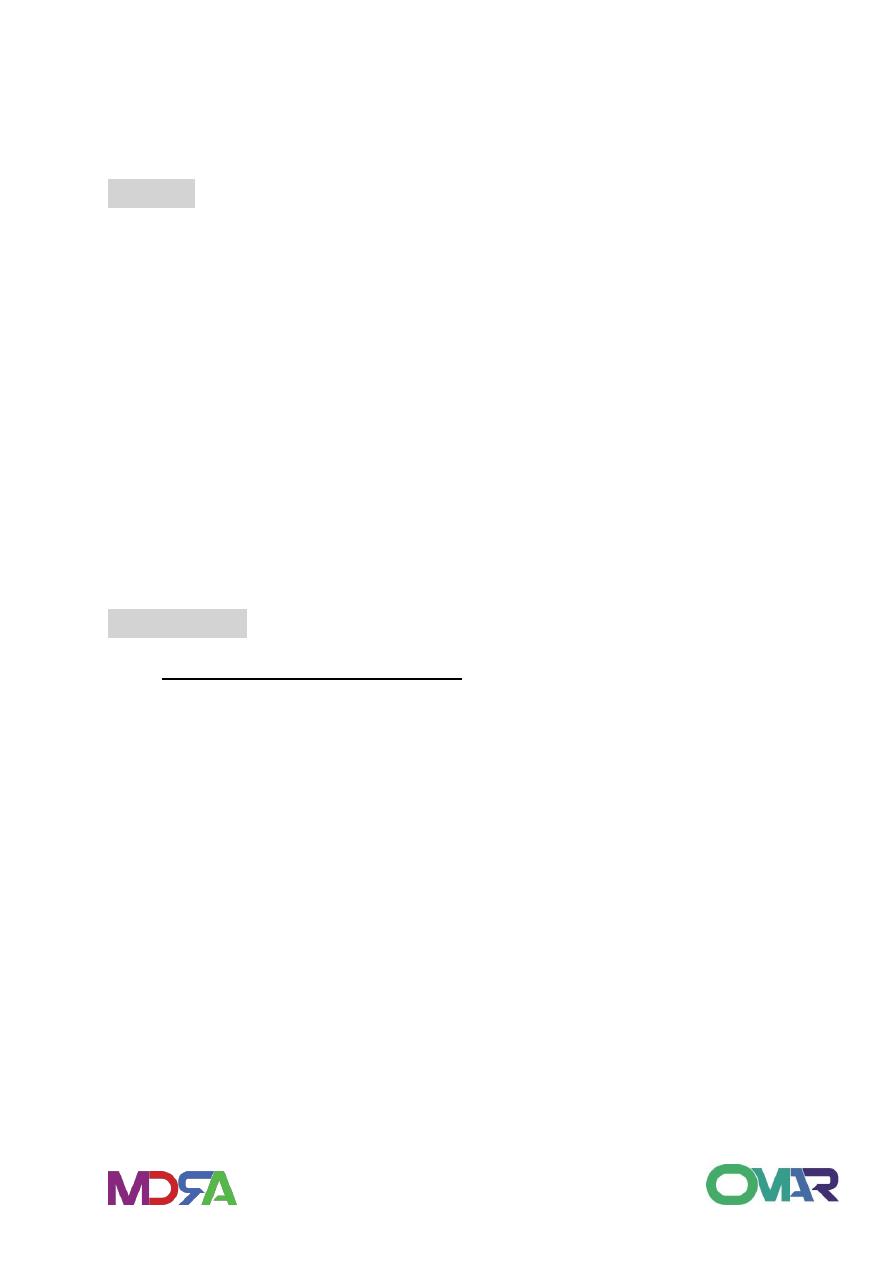
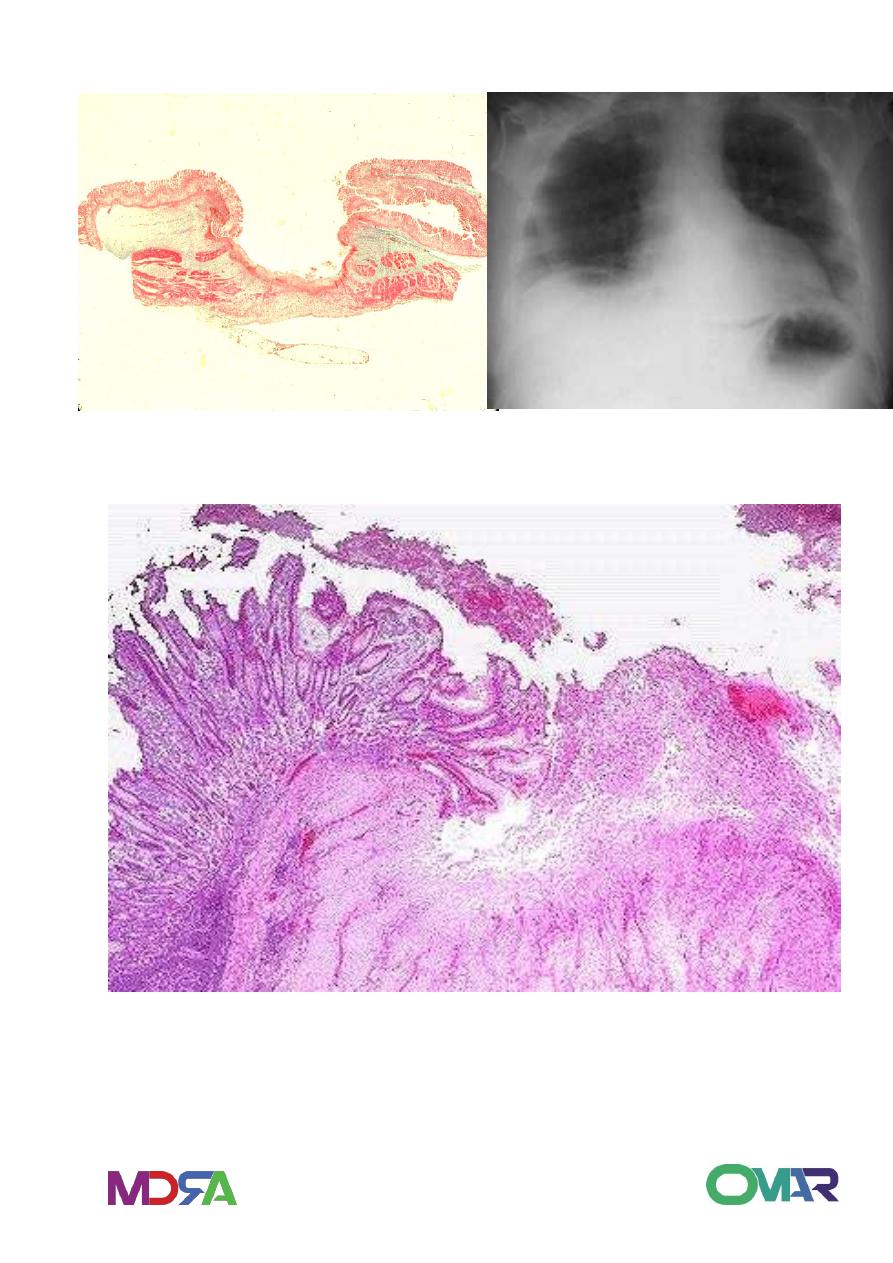
Microscopy: 4 zones.
Superficial necrotic layer.
Inflammatory cells zone.
Granulation tissue zone
Collagenous scar layer.
Complications:
Bleeding – Chronic-IDA, Acute, Massive
Fibrosis, Stricture obstruction – pyloric stenosis.
Perforation – Peritonitis- emergency.
Gastric carcinoma. (not duodenal ca)
11
Base of Ulcer Eroded artery
Active granulation tissue
proliferating small blood Base of Ulcer – Rt.Side of image
vessels fibroblasts,
Inflammatory cells
Normal
gastric
mucosa
Gastric mucosa
demonstrating S-
shaped bacilli
Helicobacter pylori
In addition to
lymphocytes
And plasma cells in the
lamina properia,
neutrophils
are visible within the
epithelium above the
basement membrane
11
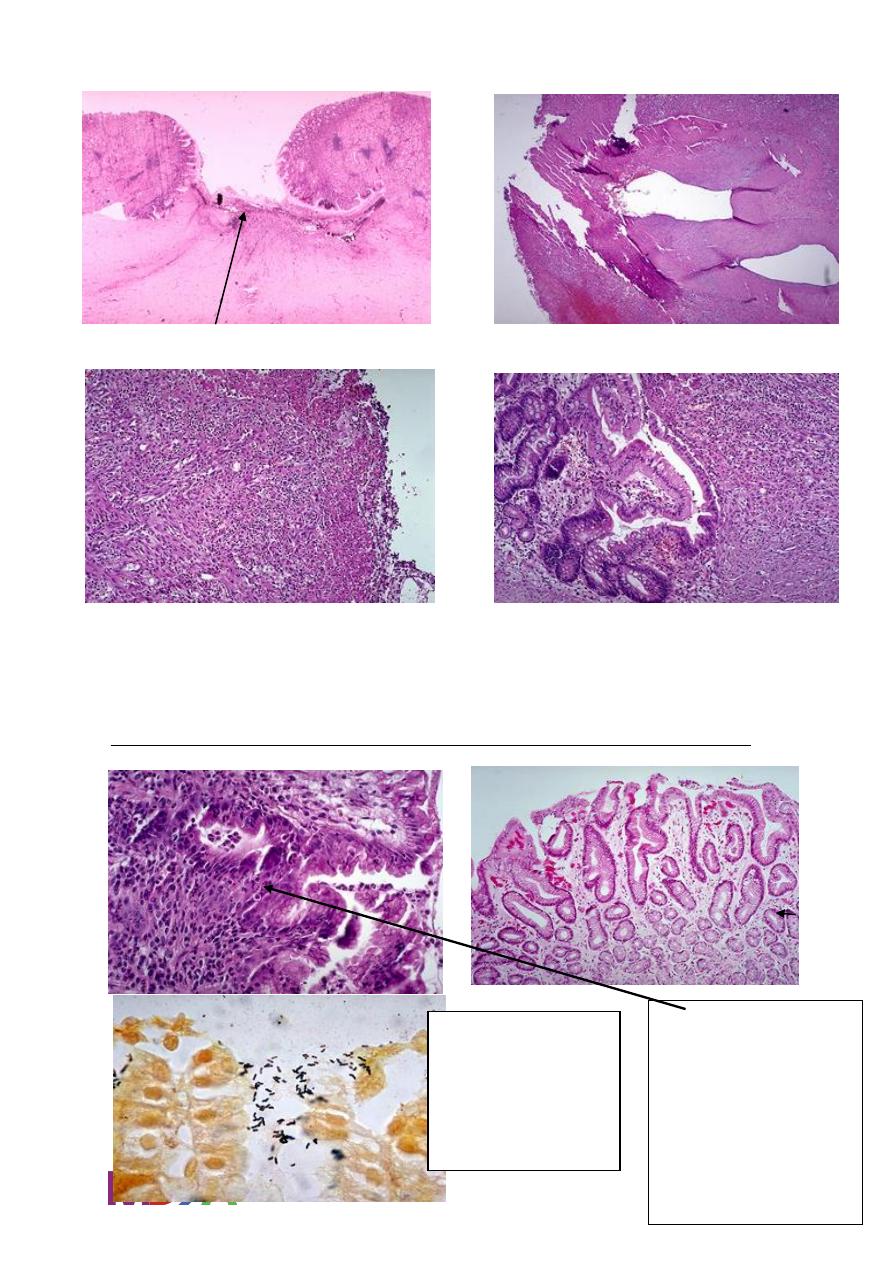
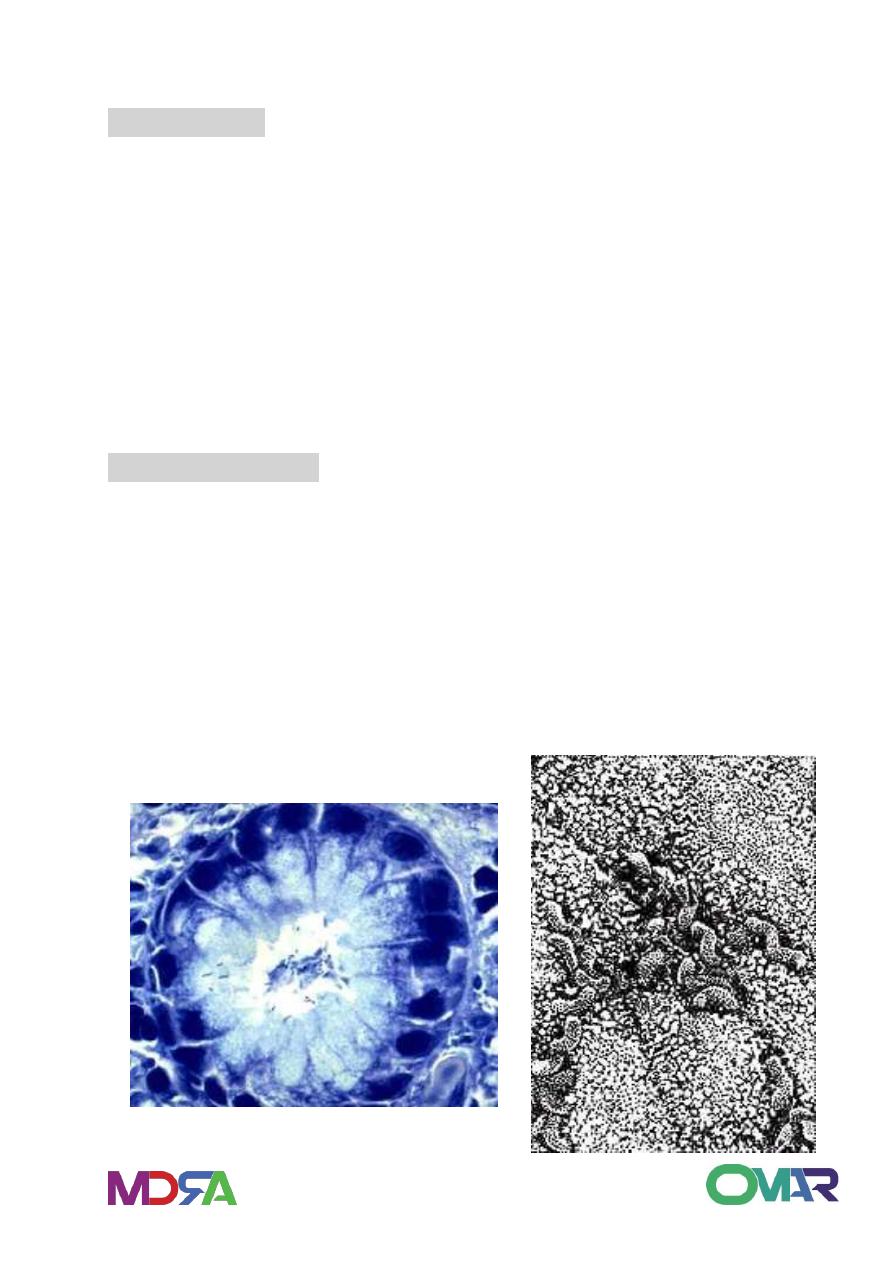
Gastric peptic ulcer
Peptic ulcer – Endoscopy Duodenal Peptic Ulcer
12
Gastric Ulcer Gastric Ulcer
Gastric Ulcer
Punched out ulcer
Clean base
Small single
Radiating mucosal
folds.
Benign ulcer.
No tumor.
13
Peptic Ulcer Microscopy Perforation
Peptic Ulcer
14
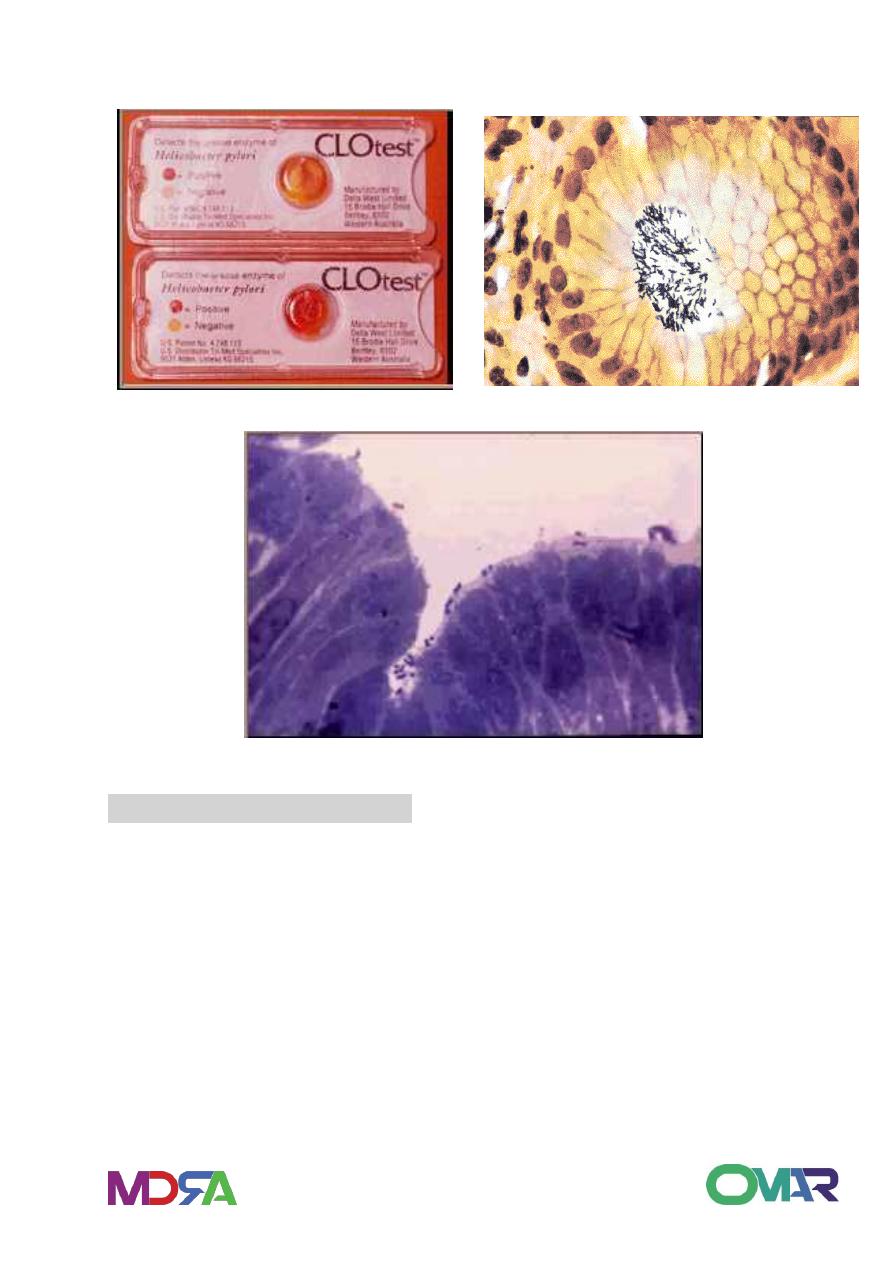
PUD - Diagnosis
Endoscopy
Barium meal – contrast x-ray
Biopsy – bacteria & malignancy
H.Pylori:
Endoscopy cytology
Biopsy – Special stains
Culture - difficult
Urease Breath test.
Points to Remember:
A peptic ulcer is a sore in the lining of the stomach or duodenum due
to attack by acid & Pepsin.
The major cause - H. pylori bacterium. Others are NSAIDs. spicy food,
stress are risk factors.
H. pylori can be transmitted from person to person through close
contact
A combination of antibiotics and H pump inhibitors is the most
effective treatment.
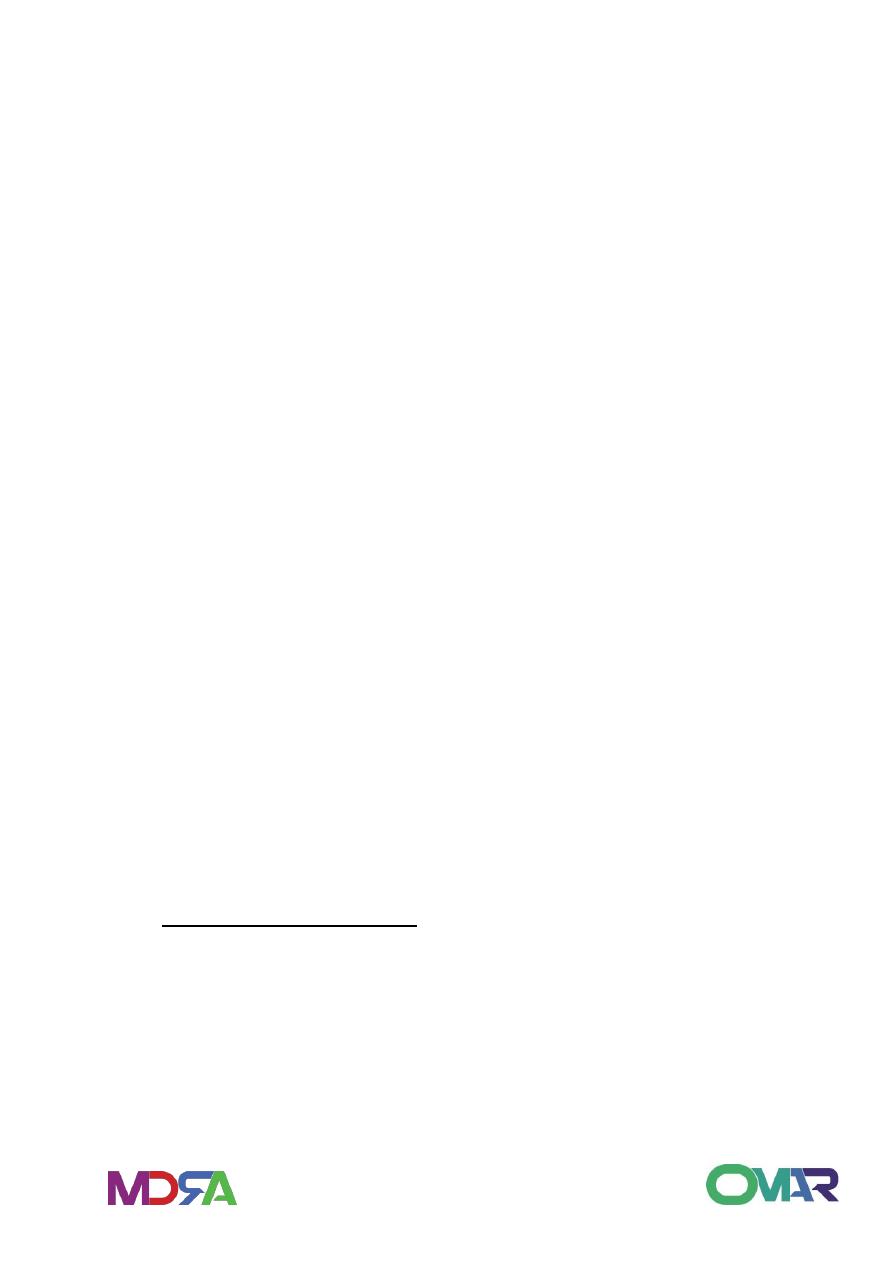
Helicobacter pylori
15
Urease production test H. Pylori organisms- silver st.
Toludine Blue stain – H pylori
ACUTE GASTRIC ULCERATYION
Focal, acutely developing gastric mucosal defects may appear
following severe stress so called as: stress ulcer.
Usually multiple, mainly in the stomach.
From erosion to deep ulcer.
Seen in : shock, extensive burns (Curling’s ulcer in proximal
duodenum), sever trauma, head injury (Cushing’s ulcer), drugs (
NSAIDs).
Intracranial lesions associated with vagal stimulation and increased
gastric secretions.

16
Morphology
Gross:
usually less than 1 cm, circular and small. Rarely deep.
anywhere in the stomach.
rugae normal, margins and base not indurated.
Micro:
Abrupt lesions.
suffusion of blood into mucosa and sub mucosa, no scar.
heal by complete re epitheialization.
Clinical course
In 5-10% of patients admitted to intensive care unit.
May be asymptomatic or may create an emergency due to bleeding.
1- ability to correct underlying condition.
2- antacid.
3- blood transfusion.
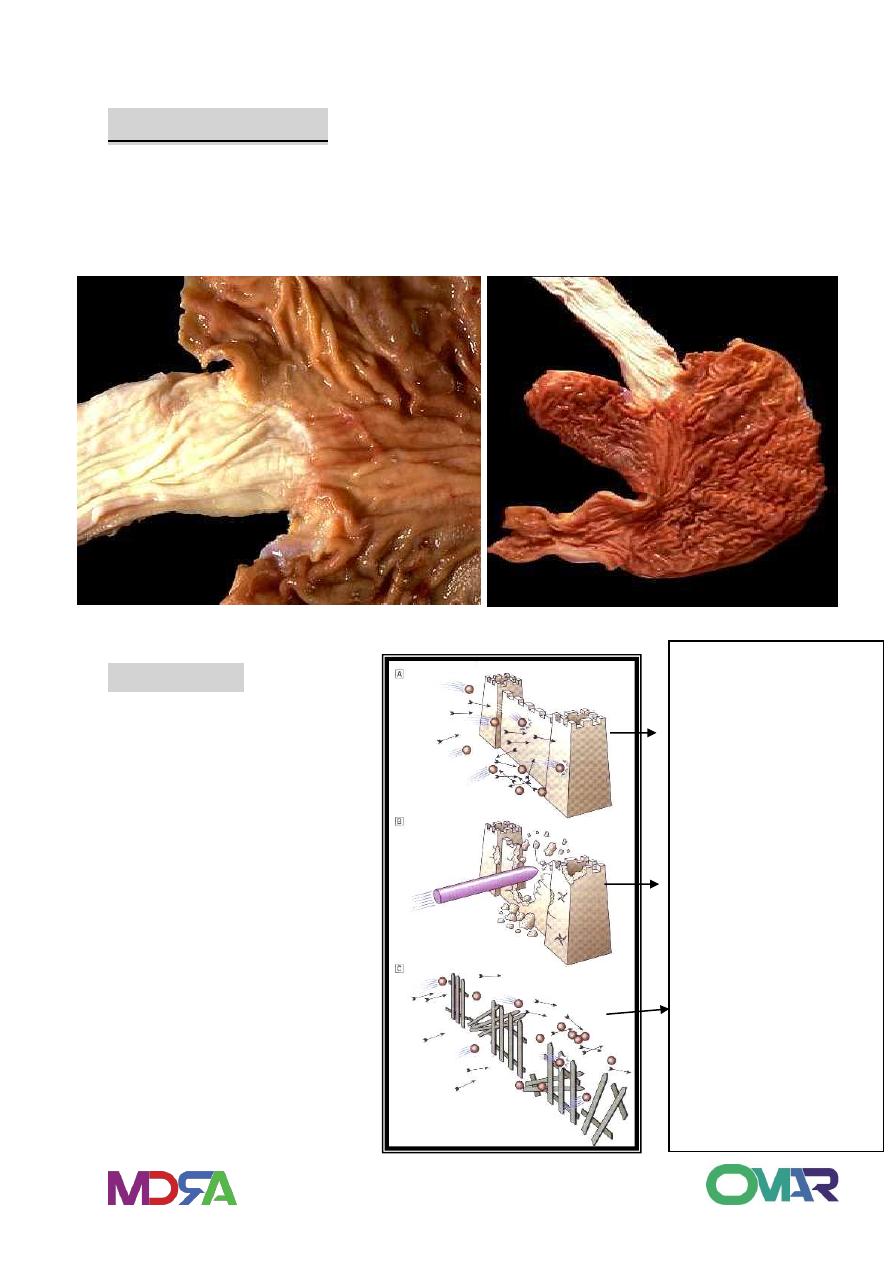
HYPERTROPHIC GASTROPATHY
a group of uncommon conditions with enlarged and giant rugae,
caused not by inflammation, but by hyperplasia of the mucosal
epithelial cells.
1- Menetrier’s disease : hyperplasia of surface mucous cells with
glandular atrophy.
2- hypertrophic hypersecretory gastropathy: hyperplasia of parietal
cells and chief cells within the glands.
3- Zollinger-Ellison syndrome: gastric gland hyperplasia secondary to
excessive gastrin secretions in gastrinoma.
CLINICAL IMPROTANCE:
1- mimic infiltrative carcinoma or lymphoma on radiology.
2- peptic ulcer risk.
17
old age , male 3:1 , present with epigastric discomfort, diarrhea,
weight loss, and sometimes bleeding.
protein loss, hypoalbuminemia.
Prone to metaplasia and carcinoma.
Tumours of the stomach and duodenum
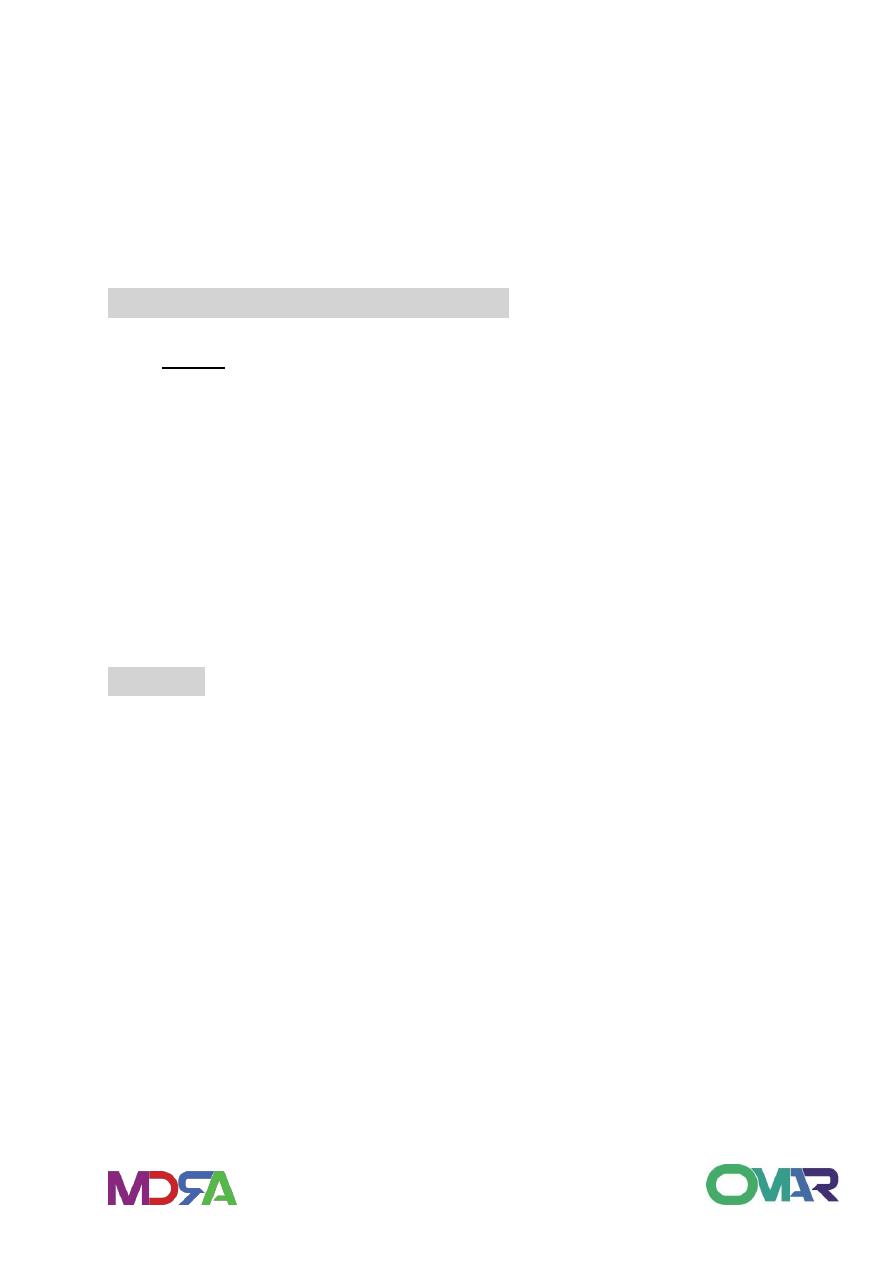
Polyp
: is any nodule or mass that projects above the level of the
surrounding mucosa.
Any lesion in the wall may project to lumen but the term is restricted
to mucosal lesions.
Most (90%), are non neoplastic, small, sessile and multiple in 25%.
Usually in setting of chronic gastritis and has no malignant potential.
Tumors of mucosal origin benign or malignant may present as
polypoid lesions.
Adenoma
Benign called as adenoma, that has malignant potential and has
proliferative dysplastic cells.
5-10% of polyps of stomach.
Gastric adenomas called also as adenomatous polyps present as
sessile or pedunculated (with stalk) mostly in distal portion of the
stomach.
Up to 40% of gastric adenomas contain a focus of carcinoma at the
time of diagnosis, and the risk of cancer is 30% in near mucosa.
Usually arise in chronic gastritis with prominent intestinal
metaplasia.
18
INTRODUCTION
Benign
Polyps
Non neoplastic
Hyperplastic
Fundic gland
Neoplastic
Adenomas
Tumors
Adenomas
Leiomyomas
Lipomas
Malignant
Tumors
Carcinoma 90-
95%
Lymphoma 4%
Carcinoid 3%
Sarcoma 2%

19
Gastric carcinoma
Epidemiology:
World wide, incidence vary, high in Japan, Chile, Costa Rica,
Colombia, China, Portugal, Iceland, Finland, Scotland.
Lower in UK, US, Canada, Australia, New Zealand, Greece, Honduras
and Sweden.
3
rd
most common GI malignancy (after colorectal and pancreatic)
14
th
cause of cancer related death in U.S.
85-95% are caused by adenocarcinoma
15% are caused by Non-Hodgkin’s lymphoma & leiomyosarcomas
H. pylori: 80 percent of gastric carcinomas result from H. pylori due
to the result of free radicals
Dietary nitrates (bacteria in stomach breaks down nitrites to
compounds that are carcinogenic in animals)
Hypochlorhydria: occurs in gastric atrophy and promotes bacterial
growth in stomach
Foods such as starch, pickled vegetables, salted fish and meat,
smoked foods and salt
People who smoke cigarettes or use alcohol are 3-5 times more likely
Epstein-Barr virus is now implicated as a cause
Pernicious anemia
Chronic atrophic gastritis
Gastric polyp
Achlorhydria
Barrett’s esophagus
Having had a Billroth 2 procedure

21
Genetic factors include:
First degree relatives
Type A blood
Anatomy of the stomach
location
37% in the proximal third of the stomach
30% in the distal stomach
20% in the midsection
Remaining 13% in the entire stomach
Pylorus and antrum= 50-60%.
Cardia= 25%.
Body and fundus= 40%.
Greater curvature=12%.

21
Clinical features: Onset
Insidious (slowly developing)
Usually discovered in advanced stages
Men>Women
Occurs between the ages of 50-70
Increased mortality in
Japanese
Costa Ricans
Chileans
Native Americans
African Americans
Scandinavians
Assessment
History:
High risk foods
Alcohol/tobacco use
Treated for H. Pylori infection
Gastritis, pernicious anemia, gastric surgery, polyps
Immediate family dx gastric cancer
Blood type
Physical Assessment
Early gastric cancer
Indigestion
Abdominal discomfort initially relieved with antacids

22
Feeling of fullness
Epigastric, back, or retrosternal pain
NOTE: most people will show no clinical manifestations
Advanced stage:
Nausea/vomiting
Obstructive symptoms
Iron deficiency/anemia
Palpable epigastric mass
Enlarged lymph nodes
Weakness/fatigue
Progressive weight loss
Evidence of metastatic cancer
Abdominal mass, ascites or jaundice
Enlarged Virchow’s node ( supraclavicular n.)
Sister Mary Joseph’s node (infiltration of the umbilicus)
Blumer’s shelf( a mass in pelvic cul-de-sac)
Krukenberg’s tumor( enlarged ovaries on PE)
Diagnosis: Labs
Decreased hematocrit and hemoglobin
Macrocytic or microcytic anemia (decreased vit.B12 and iron
absorption)
Stool positive for occult blood

23
In Advanced stages:
Hypoalbuminemia
Bilirubin and alkaline phosphate will be abnormal
Increased level of carcinoembryonic antigen
Radiographic assessment
Double contrast upper GI series
C.T.
Esophago -gastroduodenoscopy (EGD)
Endoscopic ultrasound (EUS)
Other findings include
Polypoid mass
Ulcer crater
Thickened fibrotic gastric wall
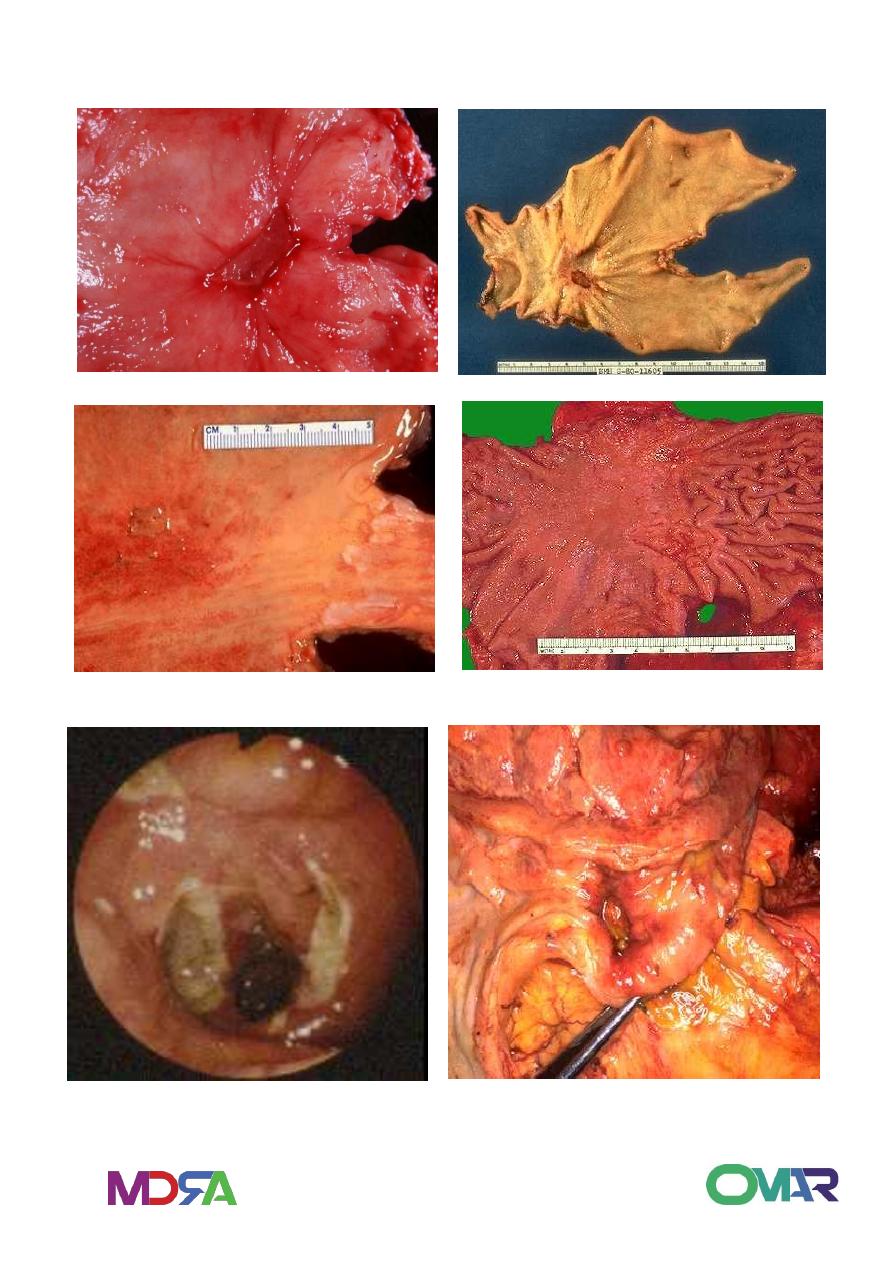
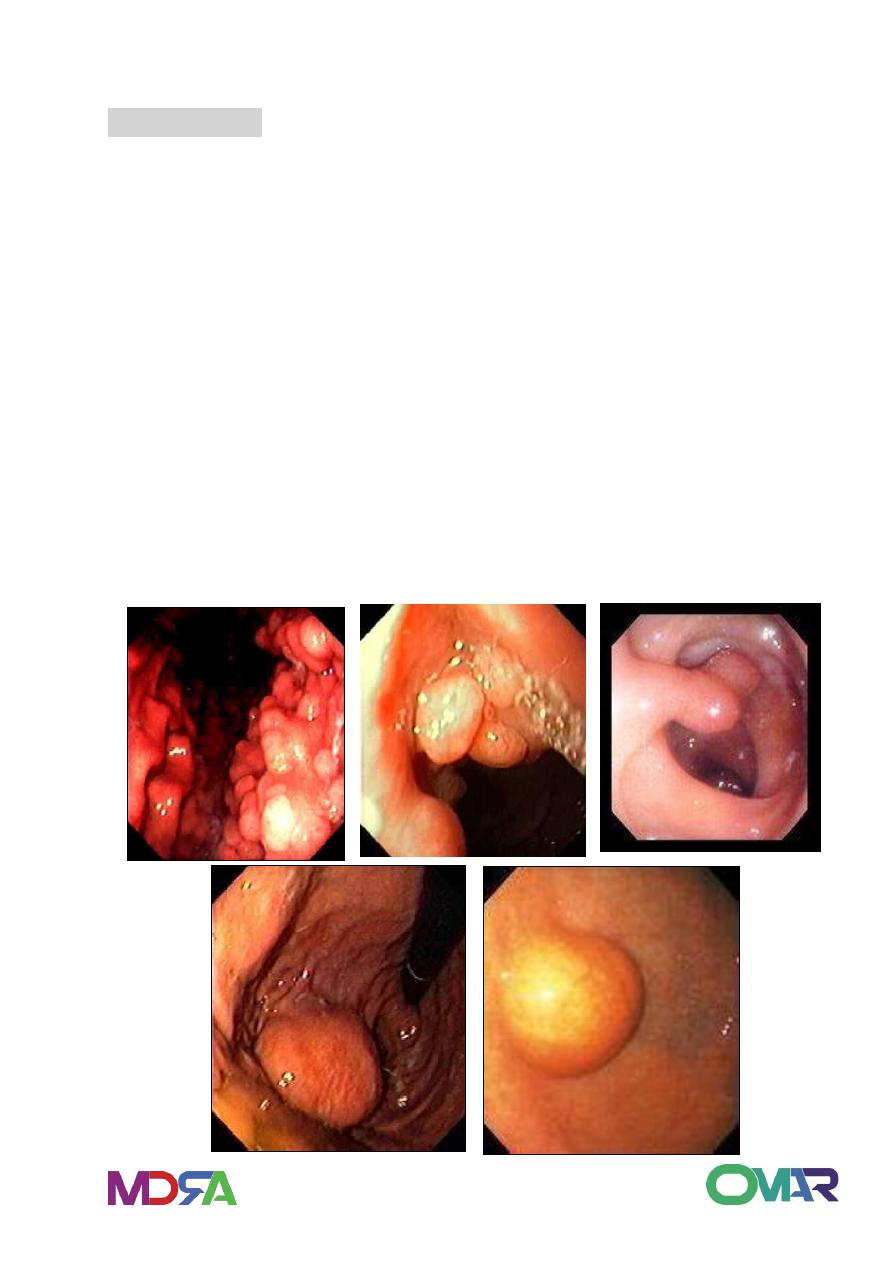
Morphology: Gross:
1. polypoid/ fungating carcinoma
2. Ulcerating/ penetrating carcinoma( 70% )
3. Infiltrating / scirrhous carcinoma = linitis plastica( 5~15% )
4. Superficial spreading carcinoma = confined to mucosa / submucosa;
5-year survival of 90%
5. Advanced carcinoma
24
GASTRIC CARCINOMA
Gastric tumors - 2 to 4 per cent of
upper GI bleeds
Gastric lymphoma usually located in
the corpus. Prognosis better.
Helicobacter pylori
has
been
associated to the development of
mucosa-associated lymphoid tissue
(MALT). Major role of H. pylori in the
development of MALT lymphoma
Benign
Ulcer
Gastric
carcinoma
Gastric
Lymphoma
25
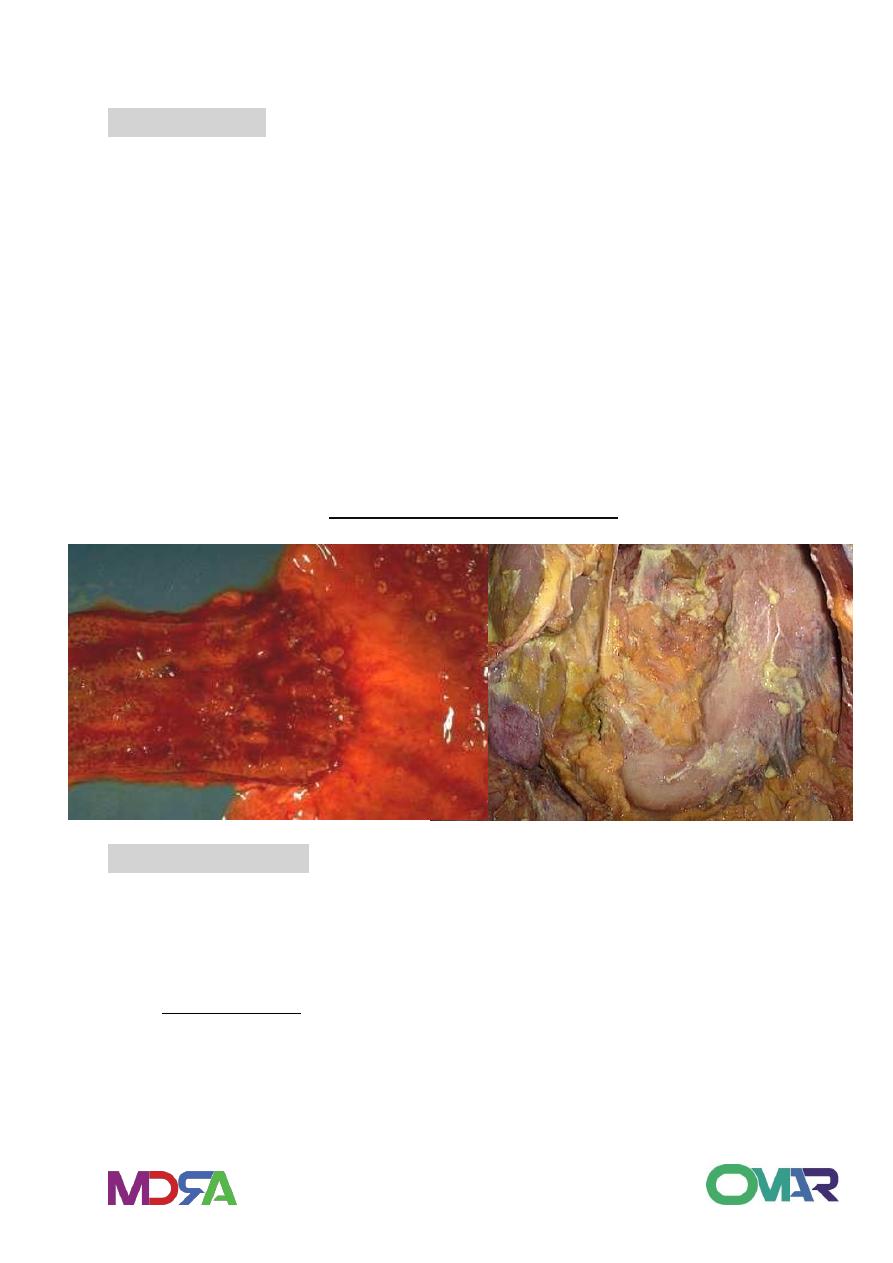
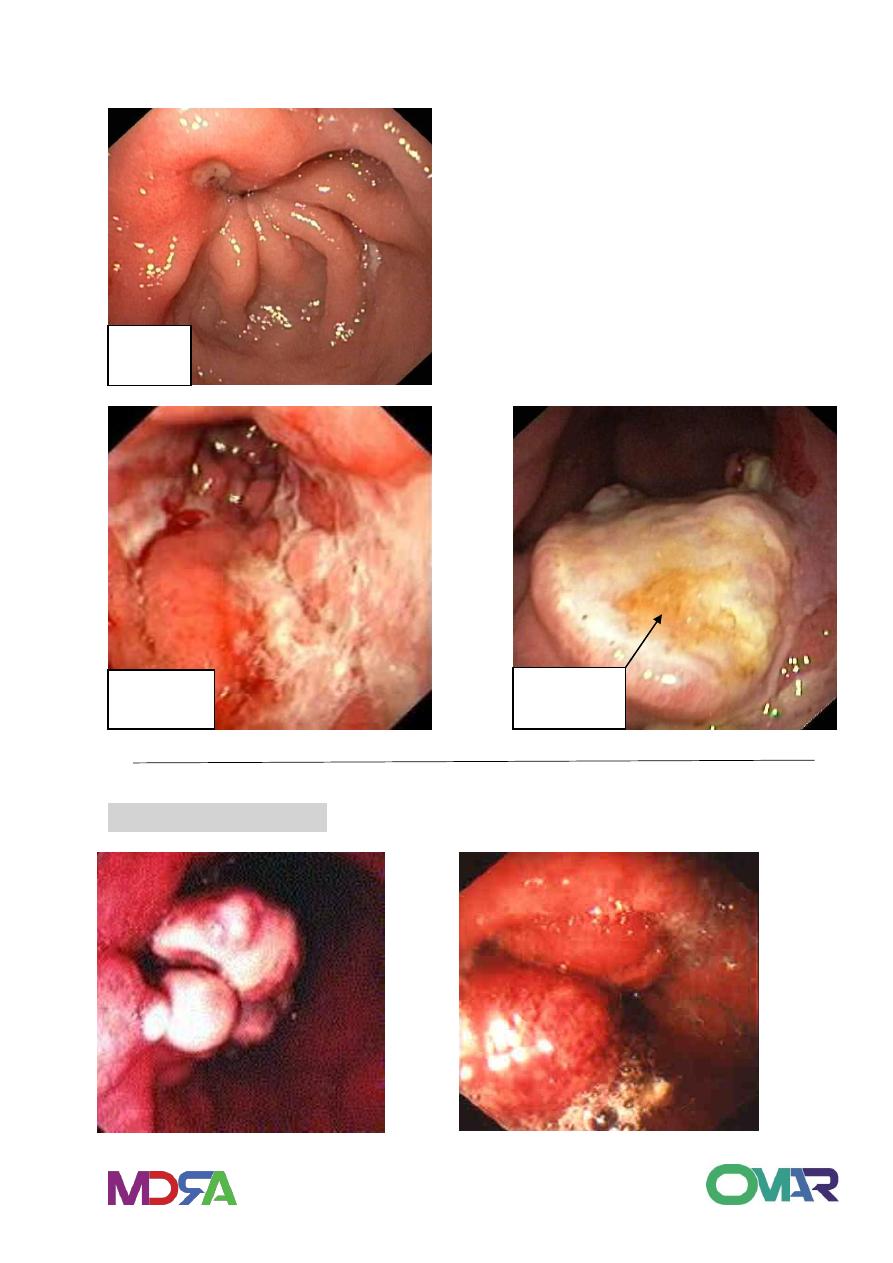
Linitis Plastica – Schirrhous Carcinoma
.
Fungating Carcinoma
Gastric Carcinoma
linitis plastica
1. histo: frequently signet ring cell type+ increase fibrous tissue
2. Firmness, rigidity, reduced capacity of stomach, a peristalsis in
involved area
3. Granular/ polypoid fold with encircling growth
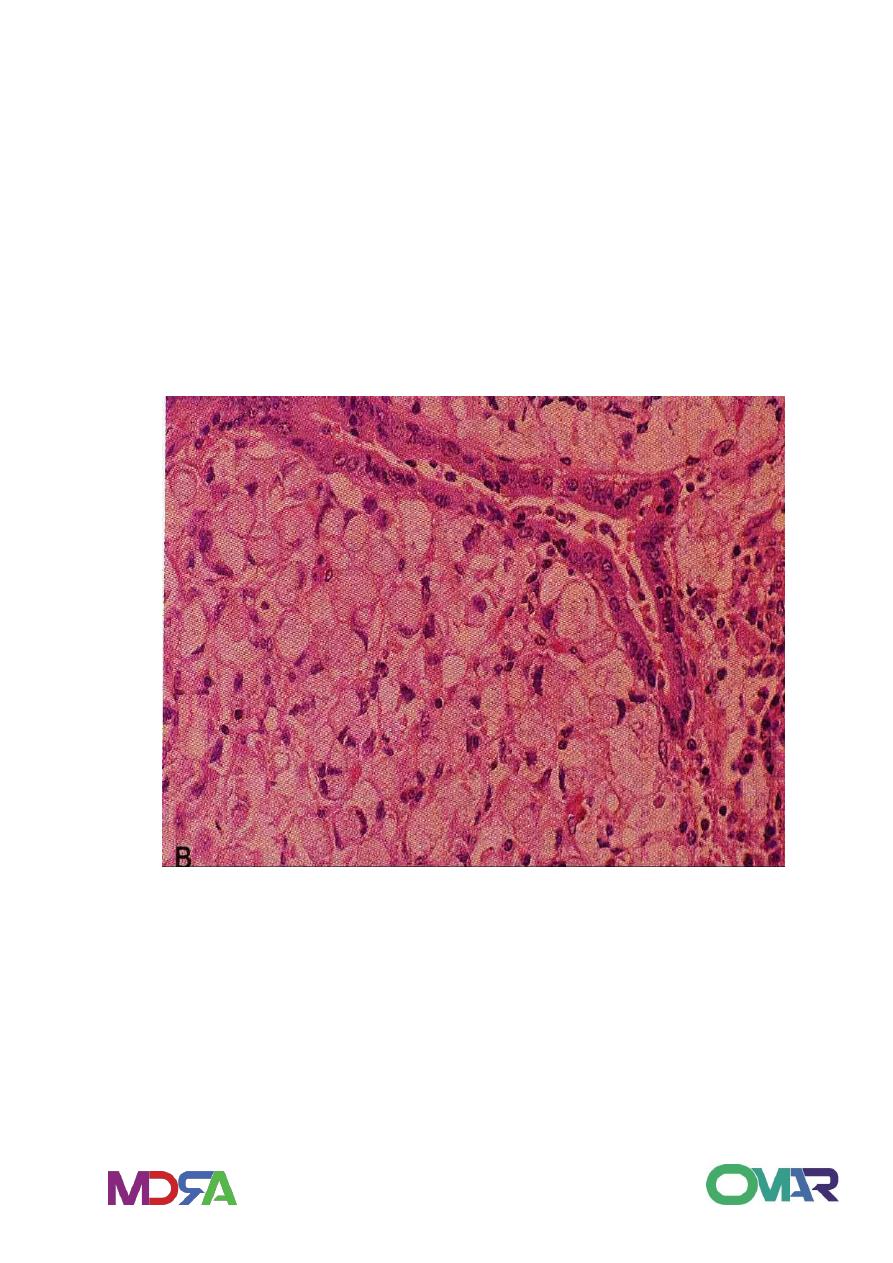
Microscopy:
It has two histologic subtypes, intestinal and diffuse, according to
Laurens classification.
26
Intestinal composed of neoplastic intestinal glands as colonic
adenocarcinoma, with expanding growth pattern.
Diffuse composed of gastric type mucous cells not forming glands
but permeate in mucosa and arrange as scattered cells or small
clusters in infiltrative growth pattern. The mucin expand the cells
and push nucleus to periphery creating signet-ring cells. Associated
fibrosis and rigidity occur due to mucin causing desmoplastic
reaction.
Gastric adenocarcinoma
