
Chronic obstructive pulmonary disease
Dr.Ahmed Hussein Jasim (F.I.B.M.S) (respiratory)

COPD) is a preventable and treatable disease characterised by persistent
airflow limitation that is usually progressive, and associated with an
enhanced chronic inflammatory response in the airways and the lung to
noxious particles or gases.
Related diagnoses include chronic bronchitis (cough and sputum on most
days for at least 3 months, in each of 2 consecutive years) and
emphysema (abnormal permanent enlargement of the airspaces distal to
the terminal bronchioles, accompanied by destruction of their walls and
without obvious fibrosis).
•
Extra-pulmonary effects include weight loss and skeletal muscle dysfunction.
Commonly associated comorbid conditions include
•
cardiovascular disease,
•
cerebrovascular disease,
•
the metabolic syndrome,
•
osteoporosis, depression and lung cancer.

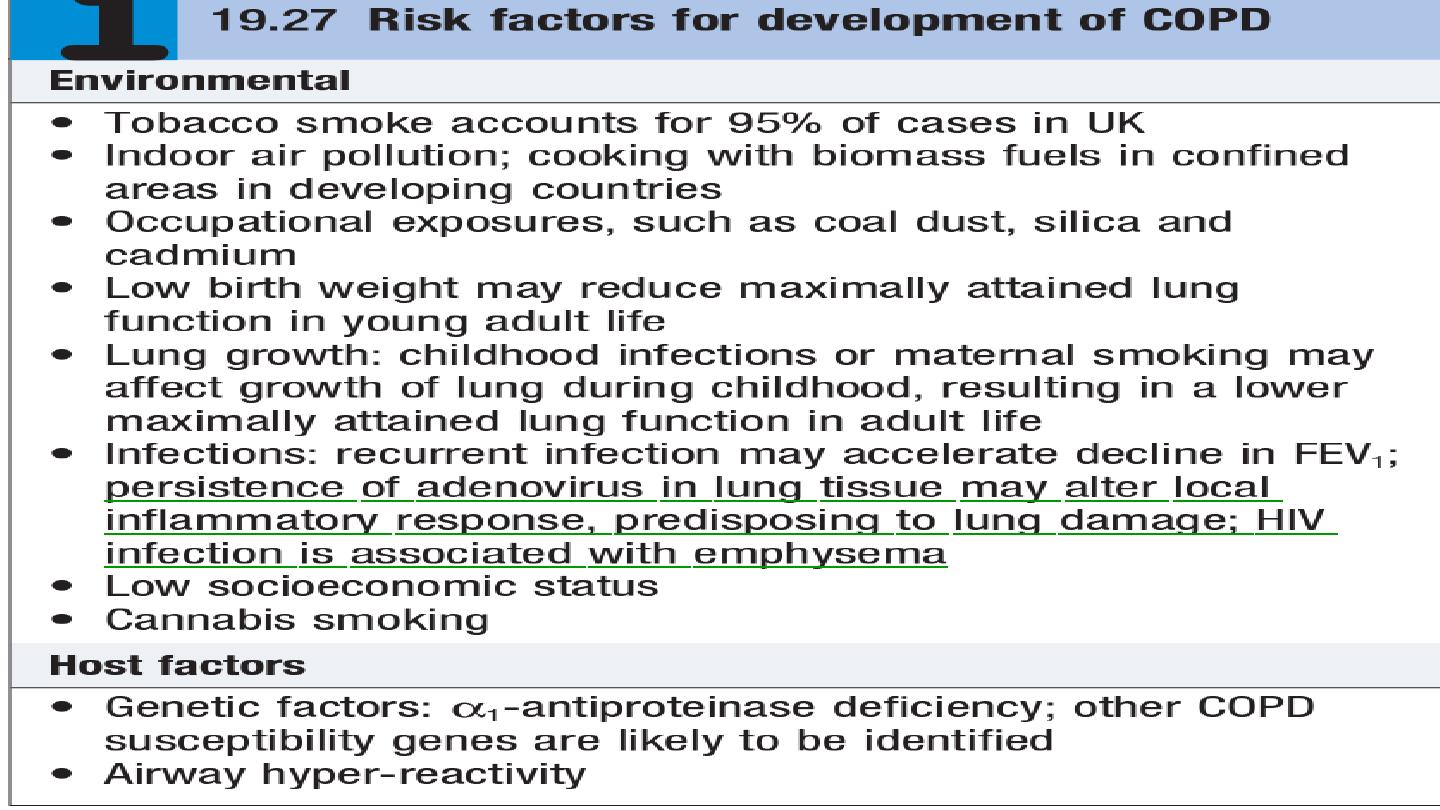
Epidemiology and aetiology
The prevalence of COPD is directly related to the prevalence of tobacco
smoking and, in low- and middle income countries and the use of biomass
fuels.
Cigarette smoking represents the most significant risk factor, and the risk
of developing COPD relates to both the amount and the duration of
smoking. It is unusual to develop COPD with less than 10 pack years (1
pack year = 20 cigarettes/day/year) and not all smokers develop the
condition, suggesting that individual susceptibility factors are important.

Pathophysiology
COPD has both pulmonary and systemic components .The presence of
airflow limitation, combined with premature airway closure, leads to gas
trapping and hyperinflation, reducing pulmonary and chest wall compliance.
Pulmonary hyperinflation also flattens the diaphragmatic muscles and leads
to an increasingly horizontal alignment of the intercostal muscles, placing
the respiratory muscles at a mechanical disadvantage.
Clinical features
COPD should be suspected in any patient over the age of 40 years who
presents with symptoms of chronic bronchitis and/or breathlessness.
Cough and associated sputum production are usually the first symptoms,
often referred to as a ‘smoker’s cough’.
Haemoptysis may complicate exacerbations of COPD but should not be
attributed to COPD without thorough investigation.

Breathlessness usually precipitates the presentation to health care. The
severity should be quantified by the modified MRC dyspnoea scale (Medical
Research Council).
Physical signs
•
Breath sounds are typically quiet.
•
Crackles may accompany infection but, if persistent, raise the possibility of
bronchiectasis.
•
Finger clubbing is not a feature of COPD and should trigger further
investigation for lung cancer or fibrosis.
•
Pitting oedema should be sought but the frequently used term ‘cor
pulmonale’ is actually a misnomer, as the right heart seldom ‘fails’ in
COPD and the occurrence of oedema usually relates to failure of salt and
water excretion by the hypoxic hypercapnic kidney.

Two classical phenotypes have been described: ‘pink puffers’ and ‘blue
bloaters’
The former are typically thin and breathless, and maintain a normal PaCO2
until the late stage of disease. The blue bloaters’ develop (or tolerate)
hypercapnia earlier and may develop oedema and secondary polycythaemia.
In practice, these phenotypes often overlap.
Investigations
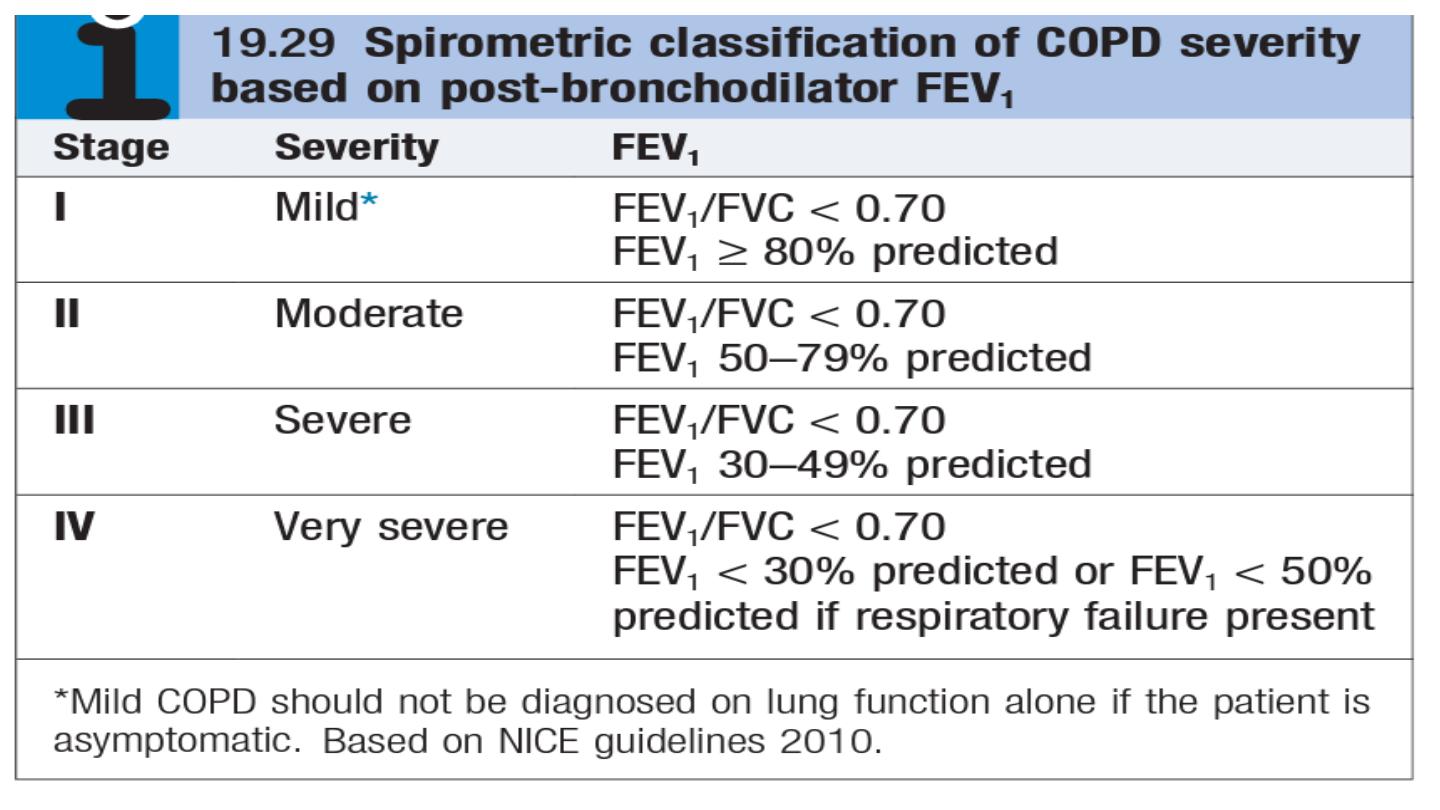
The diagnosis requires objective demonstration of airflow obstruction by
spirometry and is established when the post-bronchodilator FEV1/FVC is less
than 70%.
The severity of COPD may be defined in relation to the post-
bronchodilator FEV1 .

A low peak flow is consistent with COPD but is non-specific, does not
discriminate between obstructive and restrictive disorders, and may
underestimate the severity of airflow limitation.
Measurement of lung volumes provides an assessment of hyperinflation.
This is generally performed by using
the helium dilution techniques
. in
patients with severe COPD, and with large bullae in particular,
body
plethysmography
is preferred because the use of helium may underestimate
lung volumes. Emphysema is suggested by a low gas transfer value.
Exercise tests provide an objective assessment of exercise tolerance and a
baseline for judging response to bronchodilator therapy or rehabilitation
programmes; they may also be valuable when assessing prognosis.
Pulse oximetry of less than 93% may indicate the need for referral for a
domiciliary oxygen assessment.

chest X-ray is essential to identify alternative diagnoses, such as cardiac
failure, other complications of smoking such as lung cancer, and the
presence of bullae.
A blood count is useful to exclude anaemia or polycythaemia.
HRCT is likely to play an increasing role in the assessment of COPD, as it
allows the detection, characterization and quantification of emphysema and
is more sensitive than a chest X-ray for detecting bullae.
α1-antiproteinase should be assayed in younger patients with
predominantly basal emphysema.

Management
•
possible to help breathlessness
•
reduce the frequency and severity of exacerbations.
•
enhance the health status.
•
improve the prognosis.
•
Reducing exposure to noxious particles and gases, the role of smoking
in the development and progression of COPD, with advice and
assistance to help them stop. Reducing the number of cigarettes
smoked each day has little impact on the course and prognosis of
COPD, but complete cessation is accompanied by an improvement in
lung function and deceleration in the rate of FEV1 decline .

Bronchodilators
Bronchodilator therapy is central to the management of breathlessness.
The inhaled route is preferred and a number of different agents,
Short-acting bronchodilators, such as the β2-agonists salbutamol and
terbutaline, or the anticholinergic ipratropium bromide, may be used for
patients with mild disease.
Longer acting bronchodilators, such as the β2-agonists salmeterol,
formoterol and indacaterol, or the anticholinergic tiotropium bromide, are
more appropriate for patients with moderate to severe disease.
Theophylline preparations improve breathlessness and quality of life, but
their use is limited by side-effects, unpredictable metabolism and drug
interactions

Corticosteroids
Inhaled corticosteroids (ICS) reduce the frequency and severity of
exacerbations, and are currently re commended in patients with severe
disease (FEV1 < 50%) who report two or more exacerbations requiring
antibiotics or oral steroids per year. It is more usual to prescribe a fixed
combination of an ICS and a LABA.
Oral corticosteroids are useful during exacerbations but maintenance
therapy contributes to osteoporosis and impaired skeletal muscle function
and should be avoided.
Pulmonary rehabilitation
Exercise should be encouraged at all stages and patients reassured that
breathlessness, whilst distressing, is not dangerous. Most programmes
include 2–3 sessions per week for 6 and 12 weeks.
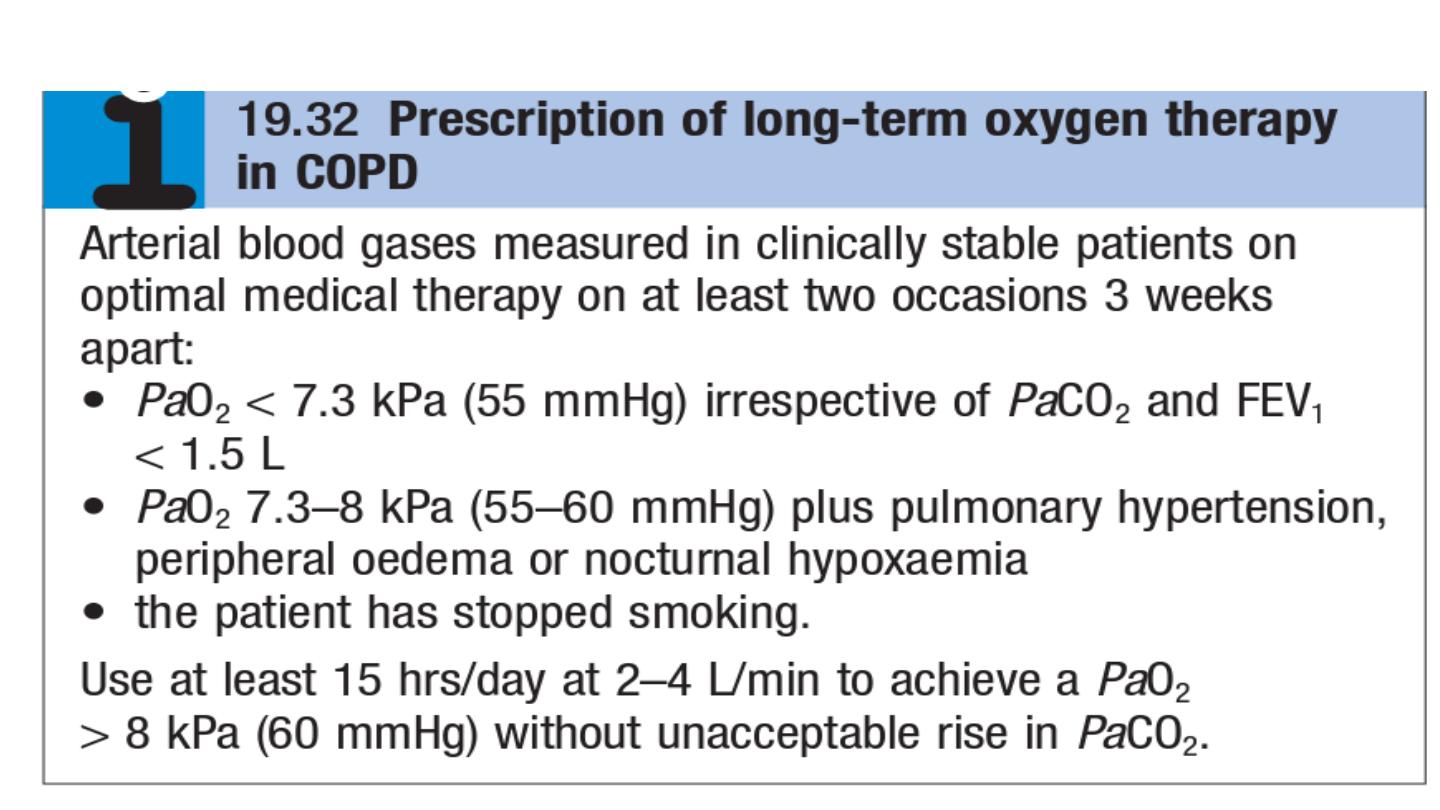
Oxygen therapy
Surgical intervention
Patients in whom large bullae compress surrounding normal lung tissue,
who otherwise have minimal airflow limitation and a lack of generalised
emphysema, may be considered for
bullectomy.
Patients with predominantly upper lobe emphysema, with preserved gas
transfer and no evidence of pulmonary hypertension, may benefit from
lung volume reduction surgery (LVRS).
Lung transplantation
may benefit carefully selected patients with advanced
disease .
Other measures
Patients with COPD should be offered an annual influenza vaccination
and, as appropriate, pneumococcal vaccination.

Prognosis
The prognosis is inversely related to age and directly related to the post-
bronchodilator FEV1
poor prognostic indicators include weight loss and pulmonary
hypertension
. A composite score comprising the body mass index (B), the
degree of airflow obstruction (O), a measurement of dyspnoea (D) and
exercise capacity (E) may assist in predicting death from respiratory and
other causes
Respiratory failure, cardiac disease and lung cancer represent common
modes of death.
Smoking cessation is the only intervention that is proven to
decrease the smoking-related decline in lung function

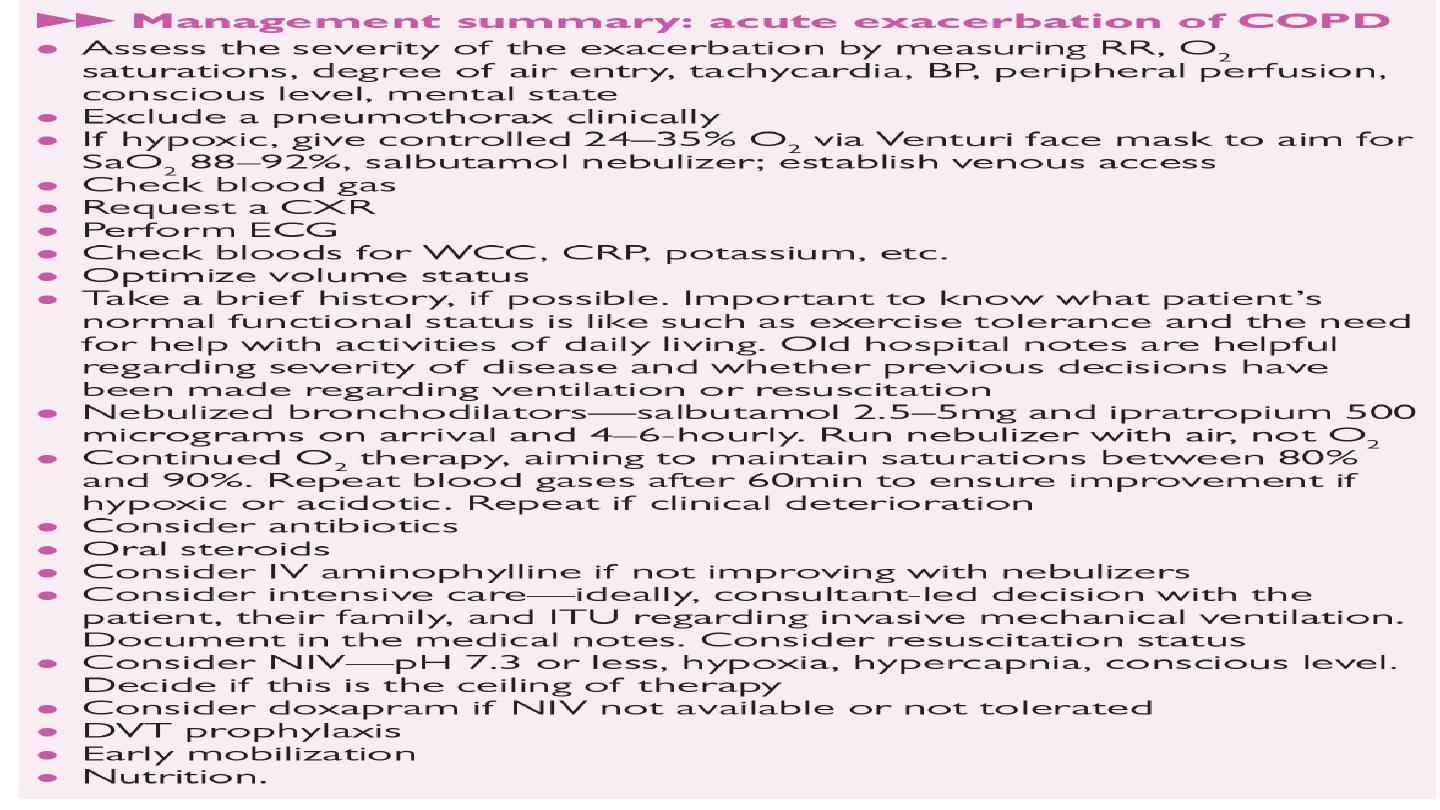
Acute exacerbations of COPD
Acute exacerbations of COPD are characterised by an increase in
symptoms and deterioration in lung function and health status.
They become more frequent as the disease progresses and are usually
triggered by bacteria, viruses or a change in air quality.
They may be accompanied by the development of respiratory failure and/
or fluid retention and are an important cause of death.
Many patients can be managed at home with the use of increased
bronchodilator therapy, a short course of oral corticosteroids and, if
appropriate, antibiotics.
The presence of cyanosis, peripheral oedema or an alteration in
consciousness indicates the need for referral to hospital.
Management
Controlled oxygen at 24% or 28% should be used with the aim of
maintaining a PaO2 above 8 kPa (60 mmHg) (or an SaO2 between 88%
and 92%) without worsening acidosis.
Nebulised short-acting β2-agonists, combined with an anticholinergic
agent (e.g. salbutamol and ipratropium), should be administered.

Oral prednisolone reduces symptoms and improves lung function. Currently,
doses of 30 mg for 10 days are recommended but shorter courses may be
acceptable.
the routine administration of antibiotics They are currently recommended,
however, for patients reporting an increase in sputum purulence, sputum
volume or breathlessness.
In most cases, simple regimens are advised, such
as an aminopenicillin or a macrolide. Co-amoxiclav is only required in
regions where β-lactamase-producing organisms are known to be common.
Exacerbations may be accompanied by the development of peripheral
oedema that usually responds to diuretics.
The use of the respiratory stimulant
doxapram
has been largely
superseded by the development of NIV, but it may be useful for a limited
period in selected patients with a low respiratory rate.

If the patient remains tachypnoeic, hypercapnic and acidotic (PaCO2 > 6 kPa,
H+
≥ 45 (pH < 7.35)), then NIV should be commenced.Its use is associated with
reduced requirements for mechanical ventilation and reduced mortality.
Mechanical ventilation may be considered in those with a reversible cause for
deterioration (e.g. pneumonia), or if PH <7.25.
Thromboprevention by subcutaneous given heparin or LMWH.

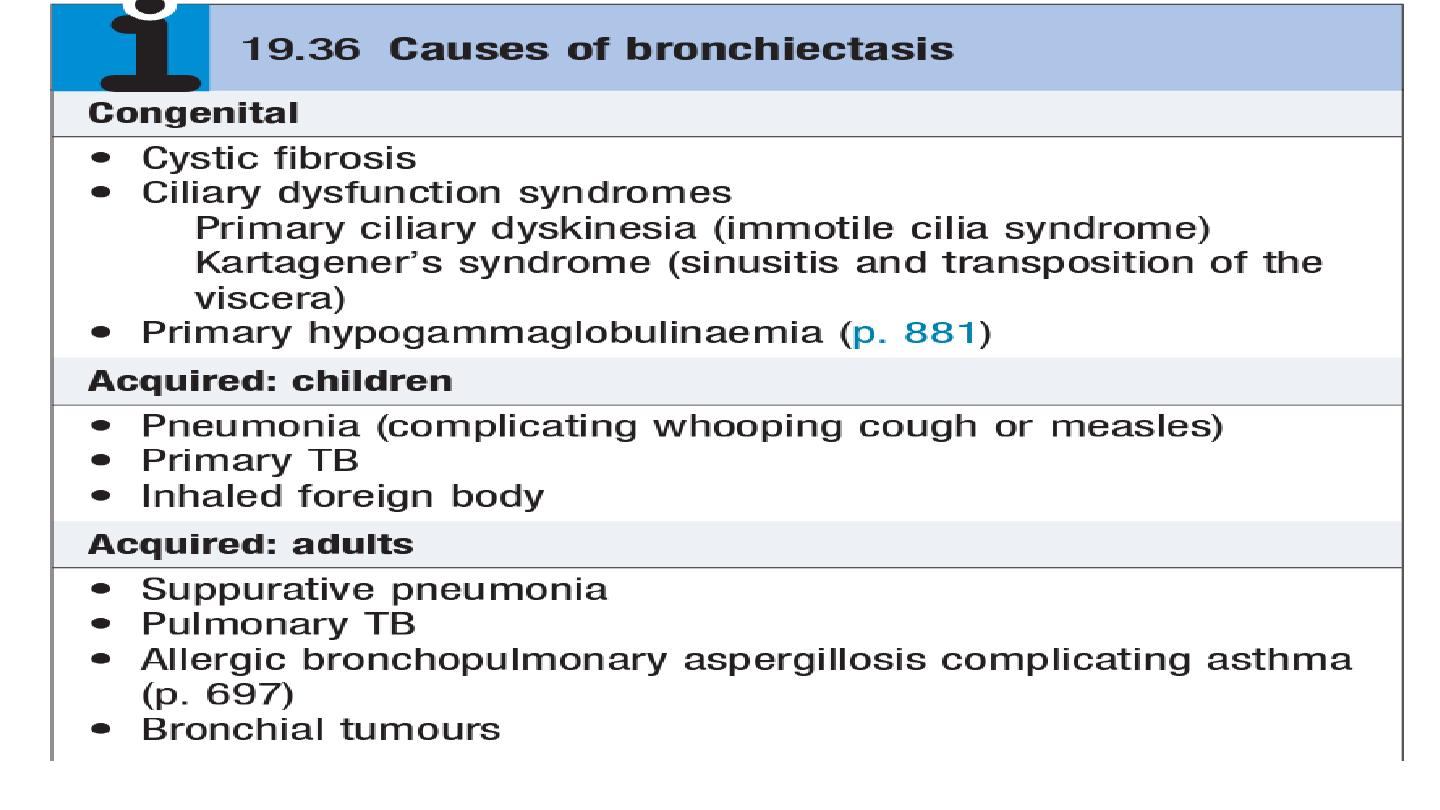
Bronchiectasis
Bronchiectasis means abnormal dilatation of the bronchi.
Chronic suppurative airway infection with sputum production, progressive
scarring and lung damage occur.
Aetiology and pathology
Tuberculosis is the most common worldwide.
Localized bronchiectasis may occur due to the accumulation of pus beyond an
obstructing bronchial lesion, such as enlarged tuberculous hilar lymph nodes, a
bronchial tumor or an inhaled foreign body (e.g. an aspirated peanut).
The bronchiectatic cavities may be lined by granulation tissue, squamous epithelium
or normal ciliated epithelium. There may also be inflammatory changes in the deeper
layers of the bronchial wall and hypertrophy of the bronchial arteries. Chronic
inflammatory and fibrotic changes are usually found in the surrounding lung tissue,
resulting in progressive destruction of the normal lung architecture in advanced cases.
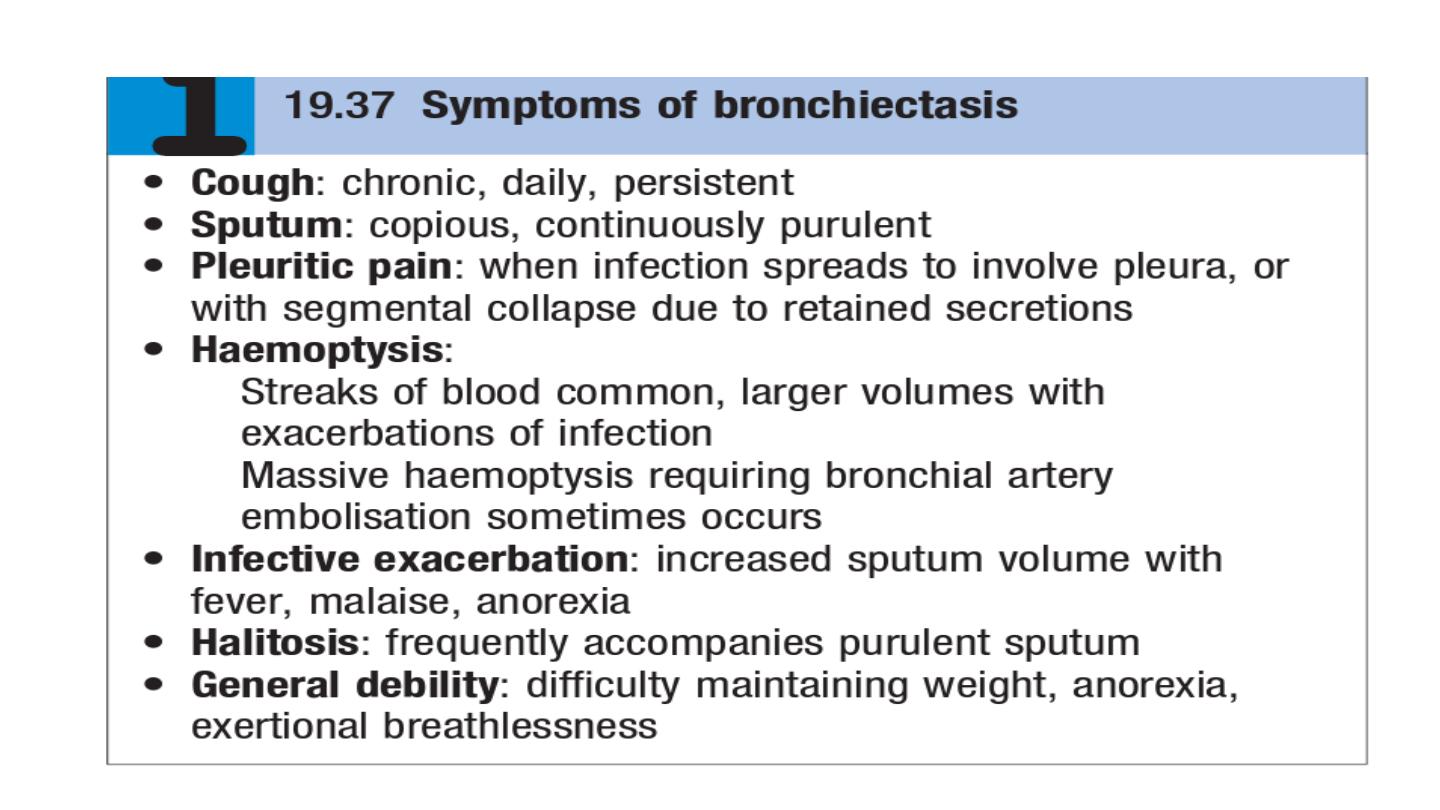
Clinical features
Investigations
common respiratory pathogens, sputum culture may reveal Pseudomonas
aeruginosa, fungi such as Aspergillus and various mycobacteria.
Frequent cultures are necessary to ensure appropriate treatment of
resistant organisms.
chest X-ray thickened airway walls, cystic bronchiectatic spaces, and
associated areas of pneumonic consolidation or collapse may be visible.
CT is much more sensitive, and shows thickened, dilated airways
A screening test can be performed in patients suspected of having a
ciliary dysfunction syndrome by measuring the time taken for a small
pellet of saccharin placed in the anterior chamber of the nose to reach
the pharynx, at which point the patient can taste it. This time should not
exceed 20 minutes but is greatly prolonged in patients with ciliary
dysfunction.

Ciliary beat frequency may also be assessed from biopsies taken from the nose.
Structural abnormalities of cilia can be detected by electron microscopy
Management
Physiotherapy
Deep breathing followed by forced expiratory manœuvres (the ‘active cycle of breathing’
technique) helps to move secretions in the dilated bronchi towards the trachea, from
which they can be cleared by vigorous coughing. Devices that increase airway pressure
either by a constant amount (positive expiratory pressure mask) or in an oscillatory
manner (flutter valve)
Antibiotic therapy
For most patients with bronchiectasis, the appropriate antibiotics are the same as those
used in COPD
Surgical treatment
Excision of bronchiectatic areas is only indicated in a small proportion of cases. These
are usually patients in whom the bronchiectasis is confined to a single lobe or segment
on CT.
