
Asthma 1
Assistant prof.Dr. Ahmed Hussein Jasim
FIBMS (resp),
FIBMS (med)
The chronic inflammation is associated with airway hyper-responsiveness that leads to
recurrent episodes of wheezing, breathlessness, chest tightness and coughing,
particularly at night and in the early morning.
These episodes are usually associated with widespread but variable airflow obstruction
within the lung that is often reversible, either spontaneously or with treatment.
PathophysiologyAirway hyper-reactivity (AHR) – the tendency for airways to narrow
excessively is integral to the diagnosis of asthma and appears to be related to
airway inflammation .The relationship between atopy (the propensity to produce
IgE) and asthma is well established, and in many individuals there is a clear
relationship between sensitisation and allergen exposure, as demonstrated by skin
prick reactivity or elevated serum specific IgE.
Common examples of allergens include house dust mites, pets such as cats and
dogs, pests such as cock-roaches, and fungi. Inhalation of an allergen into the
airway is followed by an early and late-phase broncho-constrictor response.
In cases of aspirin-sensitive asthma, the ingestion of salicylates results in
inhibition of the cyclo-oxygenase enzymes, preferentially shunting the
metabolism of arachidonic acid through the lipoxygenase pathway with
resultant production of the asthmogenic cysteinyl leukotrienes.

In exercise-induced asthma, hyperventilation results in water loss from the
pericellular lining fluid of the respiratory mucosa, which, in turn, triggers
mediator release.
In persistent asthma, is characterised by an influx of numerous inflammatory
cells,
asthma is predominantly characterised by airway eosinophilia, neutrophilic
inflammation predominates in some patients, while, in others, scant
inflammation is observed: so-called ‘pauci-granulocytic’ asthma.
With increasing severity and chronicity of the disease, remodelling of the
airway may occur, leading to fibrosis of the airway wall, fixed narrowing of
the airway and a reduced response to bronchodilator medication.

Clinical features
Typical symptoms include recurrent episodes of wheezing, chest tightness,
breathlessness and cough.
Classical precipitants include exercise, particularly in cold weather, exposure to
airborne allergens or pollutants, and viral upper respiratory tract infections.
Patients with mild intermittent asthma are usually asymptomatic between
exacerbations. Individuals with persistent asthma report ongoing breathlessness
and wheeze, but these are variable, with symptoms fluctuating over the course
of one day, or from day to day or month to month.
Some patients with asthma have a similar inflammatory response in the
upper airway. Careful enquiry should be made as to a history of sinusitis,
sinus headache, a blocked or runny nose, and loss of sense of smell.
In some circumstances, the appearance of asthma is triggered by medications.
Beta-blockers, even when administered topically as eye drops, may induce
broncho spasm, as may aspirin and other non-steroidal anti-inflammatory drugs
(NSAIDs).

The classical aspirin sensitive patient is female and presents in middle age
with asthma, rhinosinusitis and nasal polyps.
Other medications implicated include the oral contraceptive pill, cholinergic agents and
prostaglandin F2α. Betel nuts contain arecoline, which is structurally similar to methacholine and
can aggravate asthma.
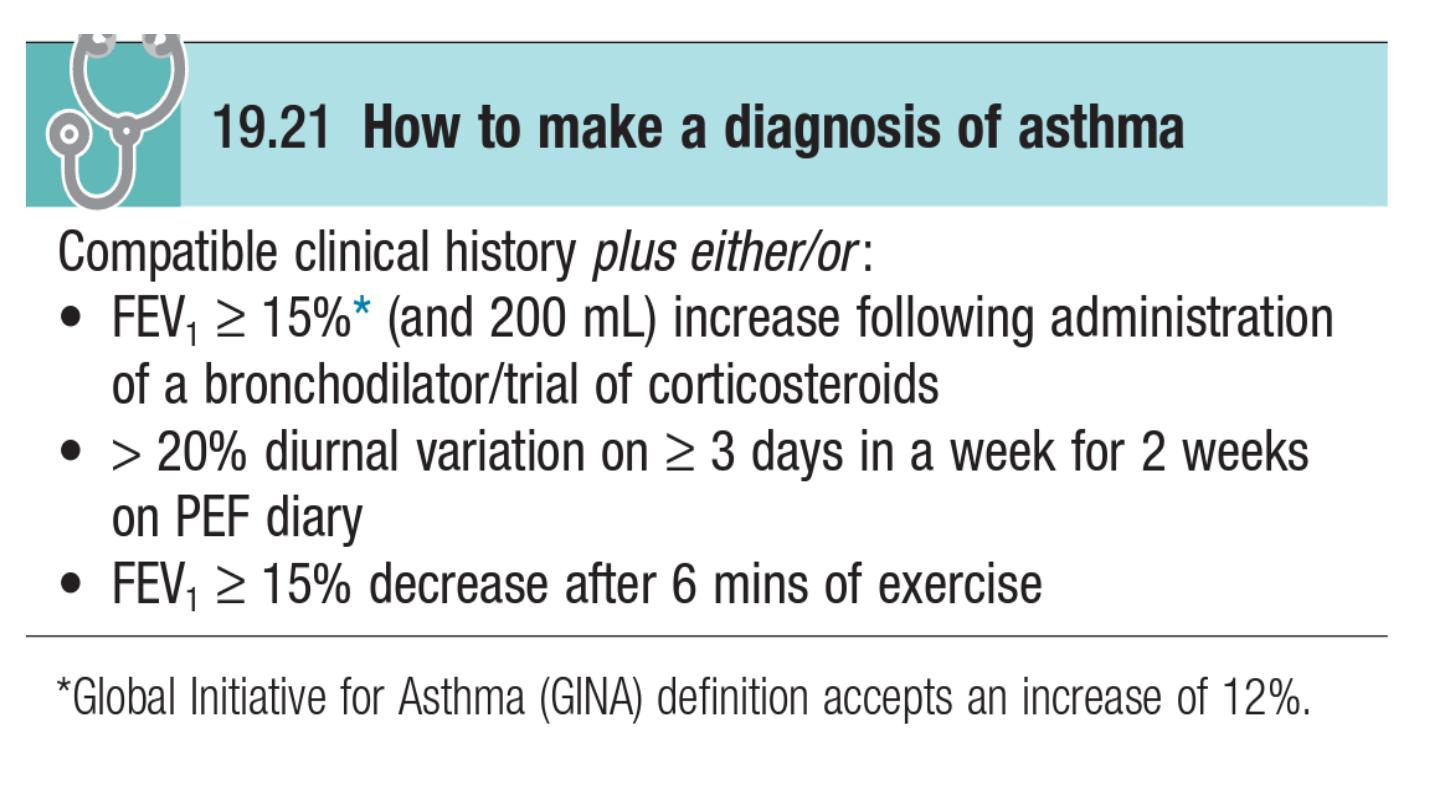
Diagnosis
The diagnosis of asthma is predominantly clinical and based on a characteristic
history.Supportive evidence is provided by the demonstration of variable airflow
obstruction, preferably by using spirometry .to measure FEV1 and VC. This identifies
the obstructive defect, a peak flow meter may be used. Patients should be instructed
to record peak flow readings after rising in the morning and before retiring in the
evening. A diurnal variation in PEF of more than 20% (the lowest values typically
being recorded in the morning) is considered diagnostic. A trial of corticosteroids (e.g.
30 mg daily for 2 weeks) may be useful in establishing the diagnosis, by
demonstrating an improvement in either FEV1 or PEF
.It is not uncommon for
patients whose symptoms are suggestive of asthma to have normal lung
function. In these circumstances, the demonstration of AHR by challenge tests may be
useful to confirm the diagnosis AHR is sensitive but non-specific.

Other investigations
• Measurement of allergic status: the presence of atopy may be demonstrated by skin prick tests. Similar
information may be provided by the measurement of total and allergen-specific IgE. A full blood picture
may show the peripheral blood eosinophilia
.•Radiological examination: chest X-ray appearances are often normal or show hyperinflation of lung
fields. An HRCT scan may be useful to detect bronchiectasis.
• Assessment of eosinophilic airway inflammation: an induced sputum differential eosinophil count of
greater than 2% or exhaled breath nitric oxide concentration (FENO) may support the diagnosis but is
non-specific.
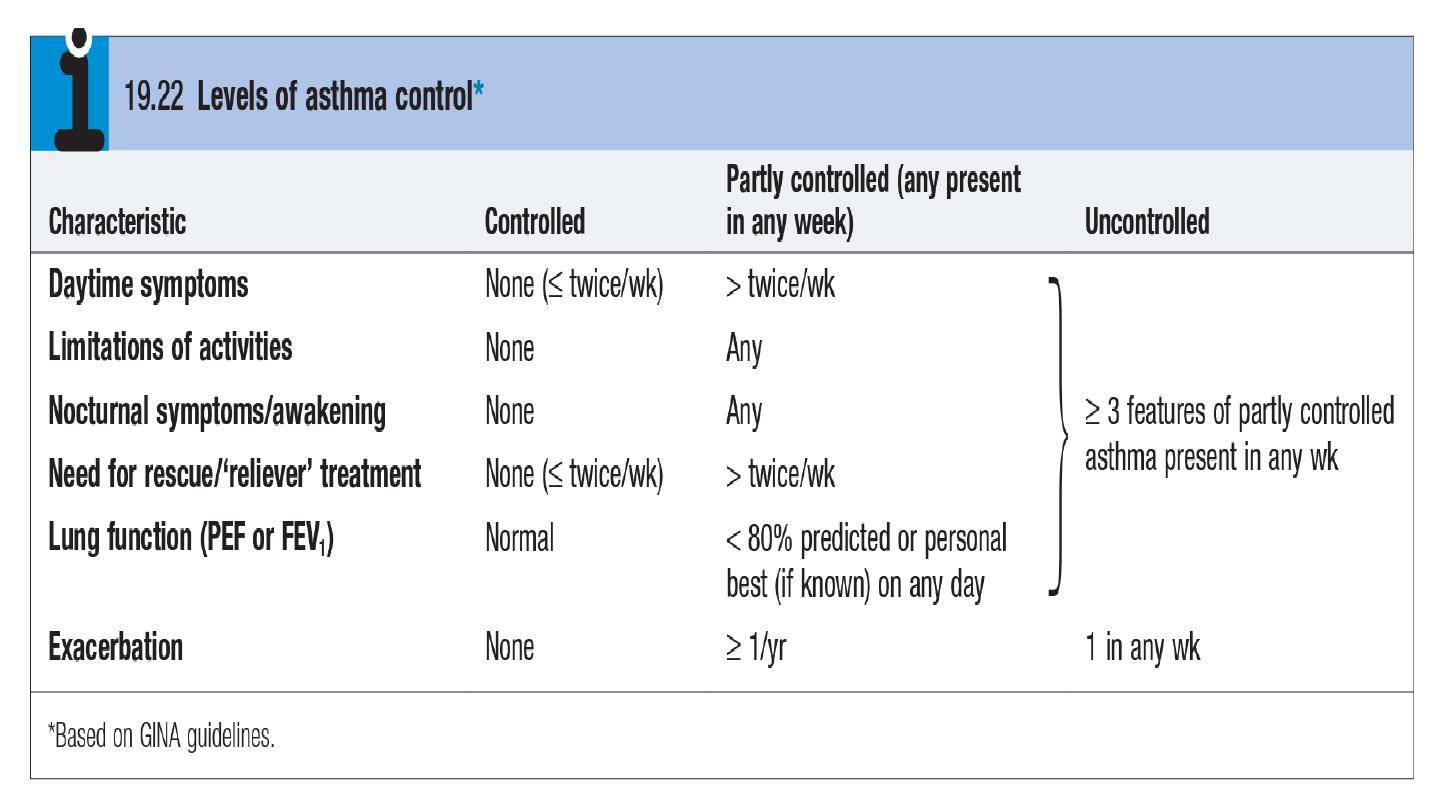
Management
Setting goals
The goal of treatment should be to obtain and maintain complete control , A full explanation of
the nature of the condition, the relationship between symptoms and inflammation, the
importance of key symptoms such as nocturnal waking, the different types of medication, and,
if appropriate, the use of PEF to guide management decisions, should be given.Avoidance of
aggravating factorsThis is particularly important in the management of occupational asthma
but may also be relevant in atopic patients, when removing or reducing exposure to relevant
antigens, such as a pet, may effect improvement. House dust mite exposure may be
minimized by replacing carpets with floorboards and using mite-impermeable
bedding.Smoking cessation is particularly important, as smoking not only encourages
sensitization, but also induces a relative corticosteroid resistance in the airway.
TREATMENT
Bronchodilators
The most common bronchodilator agents used for treatment of asthma are the
sympathomimetic agents, which act on β2 receptors to activate adenylate cyclase and
increase intracellular cyclic adenosine monophosphate (cAMP).
The second class of bronchodilator agents, the methylxanthines, is used much less frequently than β2
agonists. Theophylline, the prototype of this class, is generally believed to act by inhibiting the enzyme
phosphodiesterase (PDE), which normally is responsible for metabolic degradation of cAMP. When
degradation is inhibited, the levels of cAMP in smooth muscle and mast cells increase, resulting again
in broncho-dilation and decreased mediator release from mast cells.
The third class of bronchodilator agents, also used less frequently than β2 agonists in asthma
patients, consists of drugs that have an anticholinergic action. Anticholinergic agents dilate
bronchial smooth muscle by decreasing bronchoconstrictor cholinergic tone to airways.
Ipratropium, available as an aerosol for inhalation, is the primary short-acting example of this
class of agents.
Anti inflammatory drugs
the second major category of drugs used to treat asthma has included anti inflammatory
agents: corticosteroids, disodium cromoglycate (cromolyn), and nedocromil. They suppress the
inflammatory response by decreasing the number of eosinophils and lymphocytes infiltrating
the airway and decrease production of a number of inflammatory mediators

Agents with Specific Targeted Action
Specific agents that modify leukotrienes or leukotriene pathways include zafirlukast and
montelukast, which antagonize the action of LTD4 at its receptor, and zileuton, which inhibits
the enzyme 5-lipoxygenase and thus limits leukotriene production. On the basis of their mode
of action, drugs that either block leukotriene synthesis or antagonize their action have a
particularly important role in patients who are sensitive to aspirin or other NSAIDs.
The newest agent for treatment of asthma is omalizumab, a monoclonal antibody to IgE. On
the basis of the principle that IgE is an important component of the pathobiology of allergic
asthma, the drug was developed to prevent the binding of IgE to receptors on mast cells.
Bronchial Thermoplasty
Bronchial thermoplasty, a new procedure performed via a flexible bronchoscope, thermal energy
is delivered to the airways in an effort to reduce airway smooth muscle mass. Studies indicate
that the procedure can produce sustained benefit in patients with moderate and severe asthma,
but experience is limited.
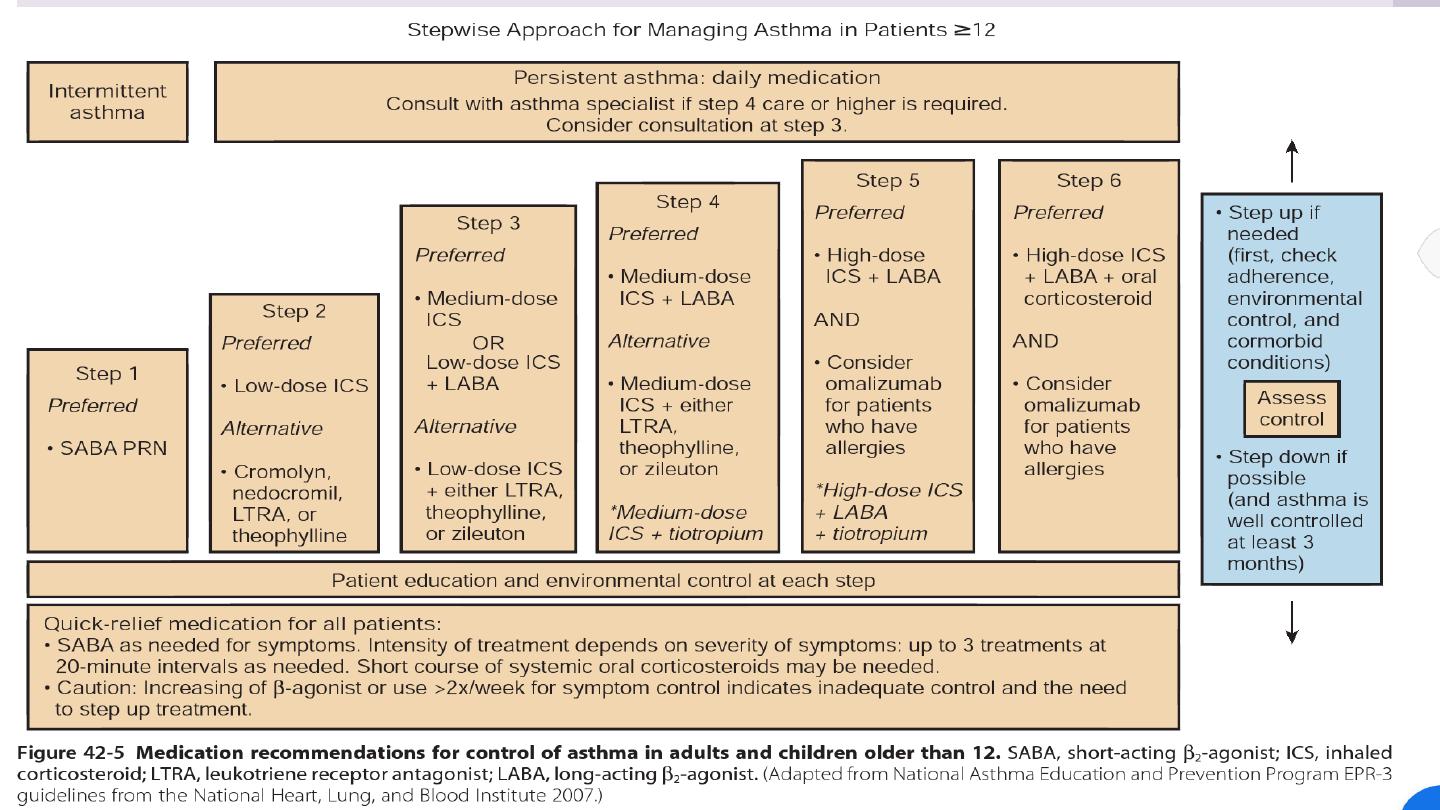
The stepwise approach to the management of asthma
Glucocorticoids are thought to bind to a cytoplasmic receptor present in nearly all cell types.
After the receptor binds to its glucocorticoid ligand, it moves to the cell nucleus, where it
interacts with transcription factors such as activator protein (AP)-1 and nuclear factor (NF)-κB,
which regulate transcription of other target genes.

Step 3: Add-on therapy
Step 4: Poor control on moderate dose of inhaled steroid and add-on therapy: addition of a
fourth drug
Step 5: Continuous or frequent use of oral steroids
Step-down therapy
Once asthma control is established, the dose of inhaled (or oral) corticosteroid should be
titrated to the lowest dose at which effective control of asthma is maintained. Decreasing the
dose of ICS by around 25–50% every 3 months is a reasonable strategy for most patients.
Step 2: Introduction of regular preventer therapy
• anti-inflammatory therapy (preferably inhaled corticosteroids (ICS), such as beclometasone,
budesonide (BUD), fluticasone or ciclesonide) should be started in addition to inhaled β2-agonists
taken on an as-required basis for any patient who:• has experienced an exacerbation of asthma in
the last 2 years . .
uses inhaled β2-agonists three times a week or more• reports symptoms three
times a week or more• is awakened by asthma one night per week.
Step 1: Occasional use of inhaled short-acting β2-adrenoreceptor agonist bronchodilators
patients with mild intermittent asthma (symptoms less than once a week for 3 months and fewer than
two nocturnal episodes per month), it is usually sufficient to prescribe an inhaled short-acting β2-
agonist, such as salbutamol or terbutaline, to be used as required.

Exacerbations of asthma
The course of asthma may be punctuated by exacerbations with increased symptoms,
deterioration in lung function, and an increase in airway inflammation.
Exacerbations are most commonly precipitated by viral infections, but moulds (Alternaria
and Cladosporium), pollens (particularly following thunderstorms) and air pollution are
also implicated.
Management of mild to moderate exacerbations
Short courses of ‘rescue’ oral cortico steroids (prednisolone 30–60 mg daily) therefore
are often required to regain control.
Indications for ‘rescue’ courses include: • symptoms and PEF progressively worsening day
by day, with a fall of PEF below 60% of the patient’s personal best recording
• onset or worsening of sleep disturbance by asthma
• persistence of morning symptoms until midday
• progressively diminishing response to an inhaled bronchodilator
• symptoms sufficiently severe to require treatment with nebulised or injected
bronchodilators.
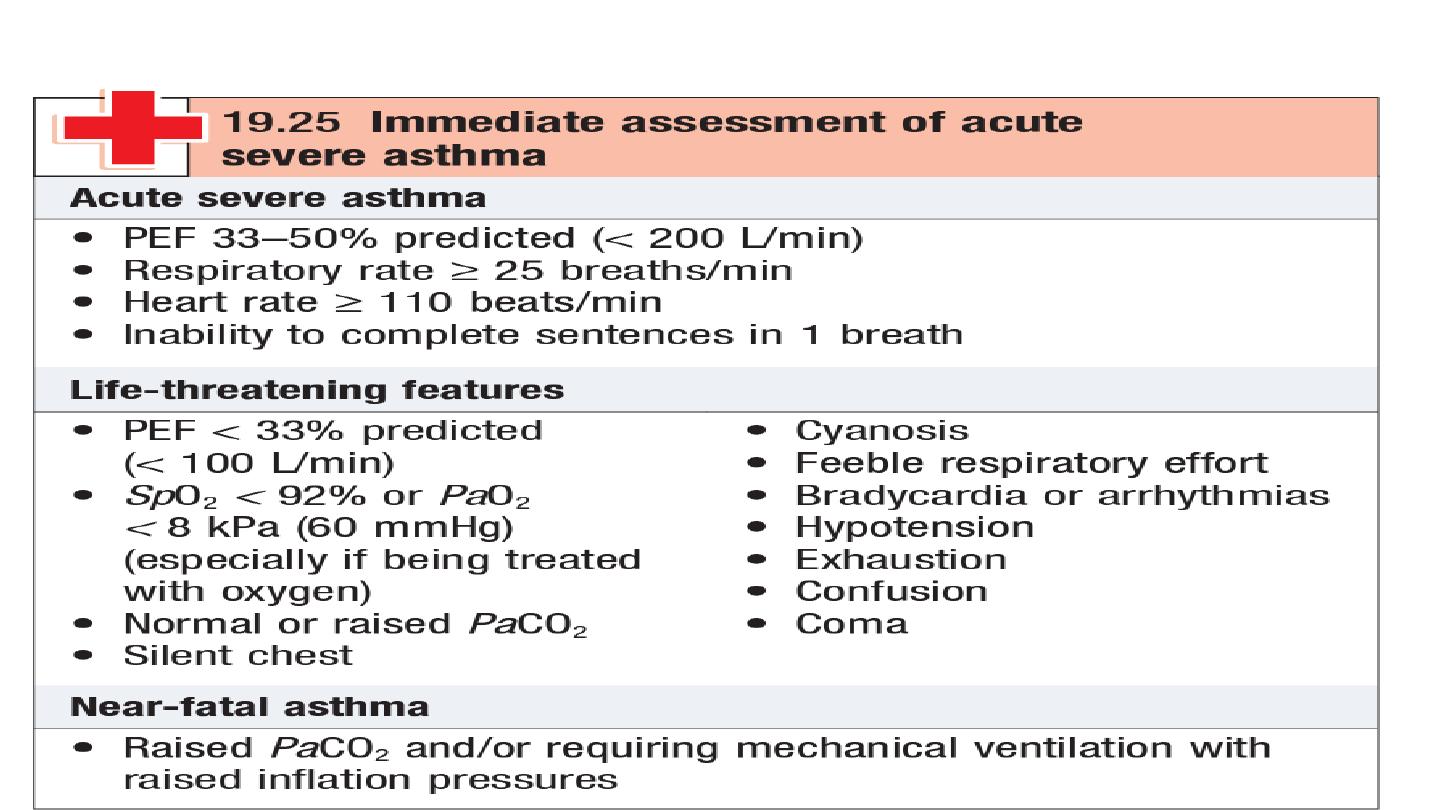
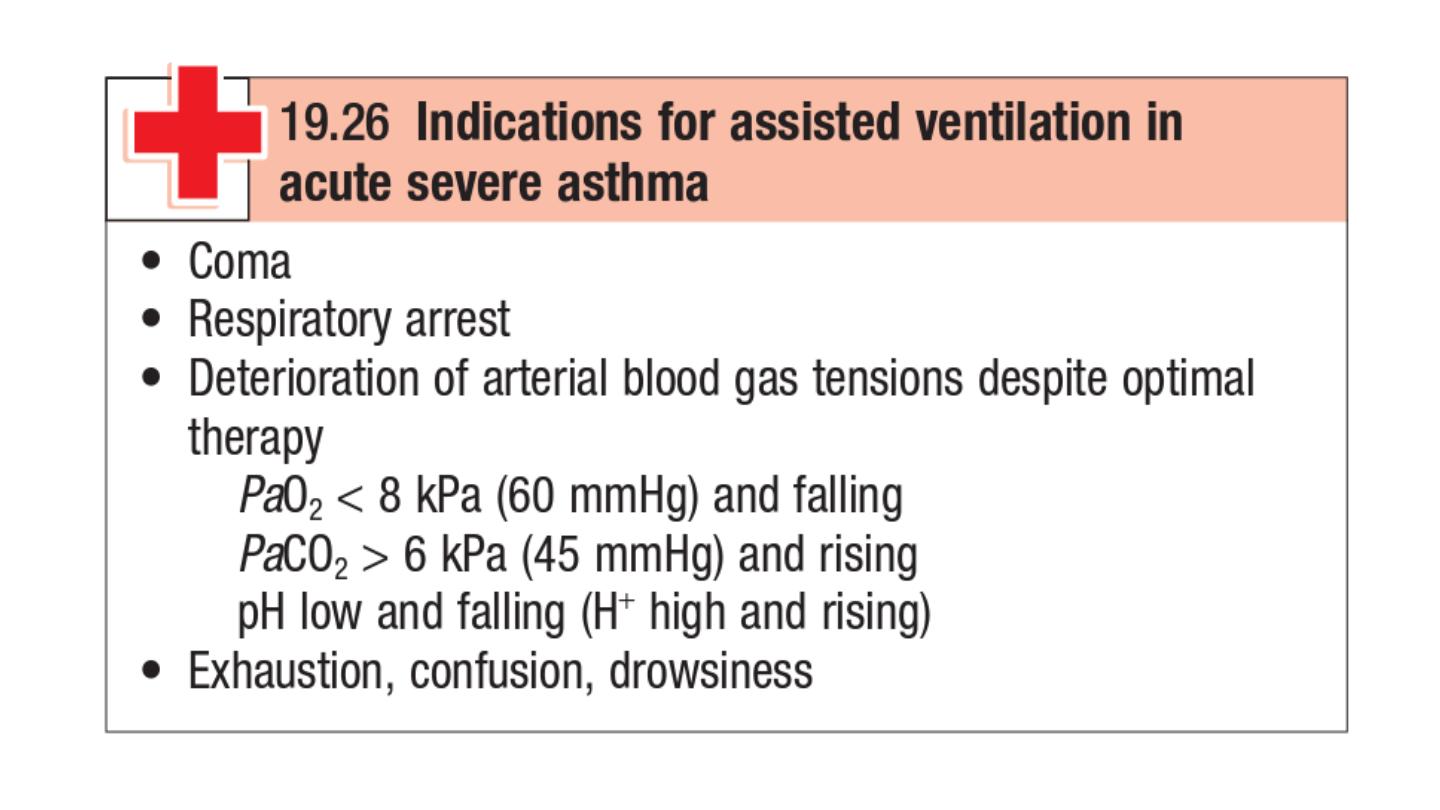
Management of acute severe asthma
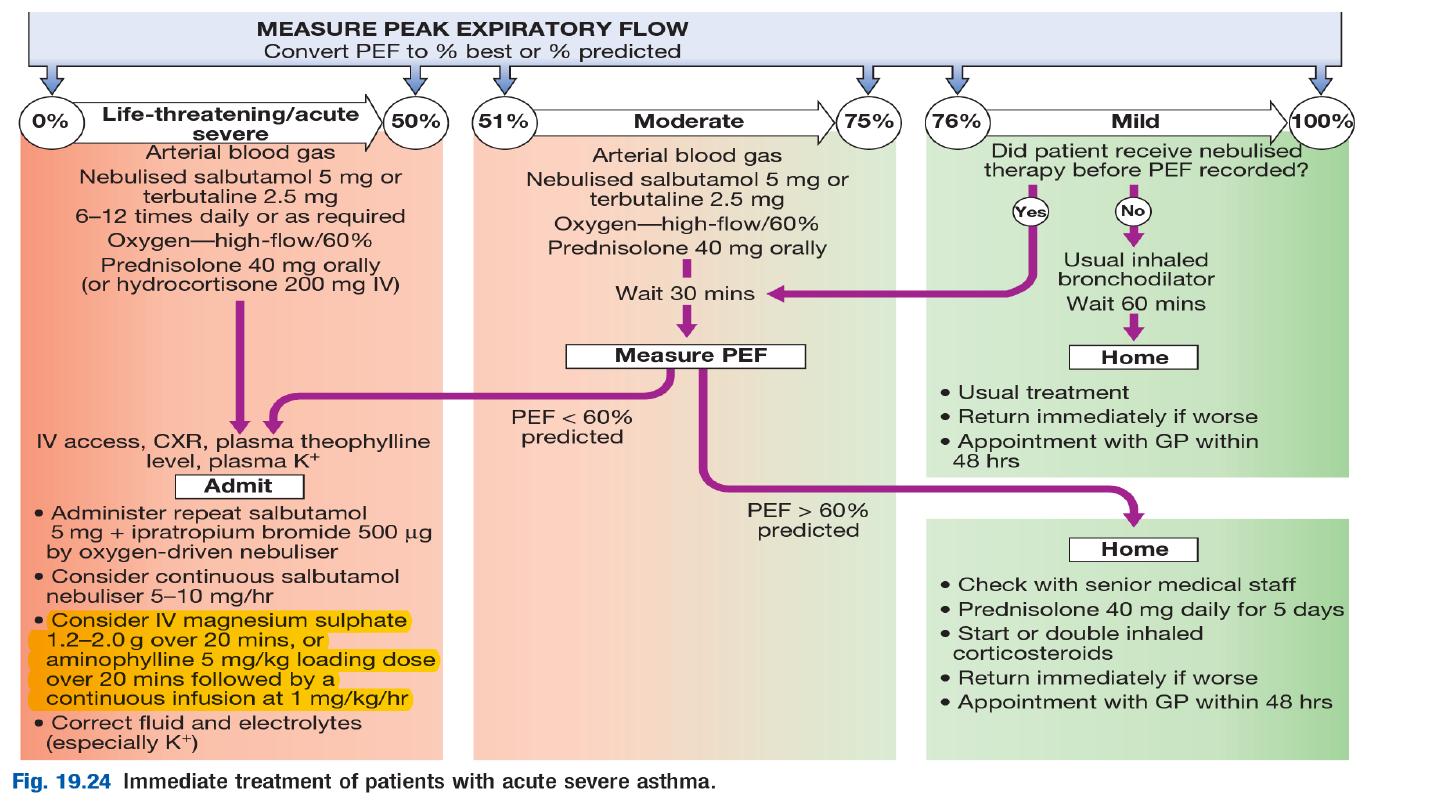

If patients fail to improve, a number of further options may be
considered
. Intravenous magnesium may provide additional
bronchodilatation in patients whose presenting PEF is below 30%
predicted. Some patients appear to benefit from the use of intravenous
aminophylline but cardiac monitoring is recommended.
PEF should be recorded every 15–30 minutes and then every 4–6 hours.
Pulse oximetry should ensure that SaO2 remains above 92%, but
repeat
arterial blood gases are necessary if the initial PaCO2 measurements
were normal or raised, the PaO2 was below 8 kPa (60 mmHg), or the
patient deteriorates.

Prior to discharge, patients should be stable on discharge medication (nebulised
therapy should have been discontinued for at least 24 hours) and the PEF should have
reached 75% of predicted or personal best.
