GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
1
Congenital anomalies
1- Atresia and stenosis
Congenital intestinal obstruction
-Complete: Atresia
-Incomplete: Stenosis
Duodenal: most common
-Jejunum and ileum: equal
-Rectum: rare
Developmental failure
intrauterine vascular accidents, or
intussuception
Imperforate anus
2- Meckel’s Diverticulum
Persistence of omphalomesenteric duct (vitelline duct) (on anti-
mesenteric side)
True : all layers.
Disease of 2’s
-2% of population (mostly asymptomatic)
- 2:1, M:F
-2 inch in length
-2 ft of ileocecal valve
-2 types of ectopic tissue in 1/2 of cases (gastric and pancreatic)
-2 major complications (pain with inflammation; hemorrhage with ulcer)

GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
2
3- Congenital Aganglionic Megacolon “Hirschsprung Disease”
Absence of ganglia (failure of migration of the neural crest cells and
arrest at some points before reaching the anus).
Loss of both submucosal (Meissner) and myenteric (Auerbach) in a
segment and loss of neural coordination and functional obstruction.
M:F 4:1. and can be in sporadic or familial cases.
1 in 5000 to 8000.
Down syndrome (10% of HD) and (5%) serious neurologic abnormalities.
Genetic defects:
Endothelin 3
GCDGF
Receptor tyrosine kinase.
Acquired in Chagas disease (typanosomiasis), neoplastic obstruction,
toxic megacolon, and functional.
Clinical features
Presents in neonatal period (failure to pass meconium; abdominal
distention)
Risk of perforation, sepsis, enterocolitis, fluid disturbances and rupture
in advanced cases.
Alternating obstruction and diarrhea
The rectum is always affected, with variable involvement of proximal
segments,
Aganglionic segment causes functional obstruction with distention
proximal to aganglionic segment, which may be massive reach to 15-20
cm in diameter.

GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
3
Vascular diseases:
a. Ischemic bowel disease
b. Angiodysplasia
c. Hemorrhoids
a. Ischemic bowel disease:
Acute obstruction of one artery may lead to infarction of mm. 50-75%
death rate.
Old individuals, pain and tenderness, bloody diarrhea, rigid abdomen
and paralytic ileus.
Insidious loss has no effect (anastomosis), and present with chronic
ischemic colitis, with episodes of bloody diarrhea.
Transmural infarction result from mechanical obstruction of major
artery.
Mucosal or mural infarction more often results from hypoperfusion
(acute or chronic).
The predisposing conditions of ischemia are:
1- arterial thrombosis: in severe atherosclerosis, at origin of aa. Or
arteritis, surgical accidents, dissecting aneurysm, hypercoagulable
state.
2- arterial embolism.
3- venous thrombosis.
4- Non occlusive ischemia HF, shock, dehydration, drugs.
5- Miscellaneous as radiation, volvulus, stricture or hernia.
Embolus: superior mesenteric artery branches, source: embolus of
heart (mural thrombus, valvular vegetation)

GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
4
b. Angiodysplasia
-tortuous dilatation of the veins in the submucosal and mucosal blood
vessels with ectasia of veins.
Prone to rupture, and presents with massive GIT-bleeding (20% of
significant massive lower GIT bleeding),
Prevalence:<1%
Sixth decade, pathogenesis, mechanical, with vascular degenerative
changes in aging.
Osler-Weber-Rendu syndrome (hereditary hemorrhagic telangiectasia)
C.
Hemorrhoids
dilated veins of hemorrhoidal plexus
-Internal
-External
-(BPR or streaks on stool), thrombosis, pain
5% of population
elevated venous pressure
constipation
straining venous stasis of pregnancy
collateral channels in portal HTN
rare under 30 except in pregnant women
Enterocolitis
Infectious
Necrotizing
Pseudomembranous
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
5
Infectious
-Viral (Rotavirus)
-Bacterial
E. coli; Shigella; V. Cholerae; C. difficile
-Parasites and protozoa (nematodes; flatworms; protozoa -Giardia
lambdia; E. histolytica)
Diarrhea
Secretory Diarrhea
more than 500 ml per day fluid which is isotonic with
plasma and persist in fasting.
Osmotic diarrhea
output more than 500 ml per day osmotic forces by
luminal solutes that abate on fasting.
Exudative diarrhea
(WBC & RBC in stool) that persist in fasting.
Malabsorptive:
long term weight loss, voluminous bulky stools with increased osmolarity of
it due to unabsorbed nutrients, and excess fat.
Salmonella enteritidis:
Milk, beef, eggs, poultry ,Self limiting diarrhea, dysentery pain, bacteremia.
Shigella:
Person-to-person. Milk, poultry,Produce mucosal ulcer ,Fever, pain, Exudative
diarrhea ,dysentery, epidemic spread
Vibrio cholera:
Water borne,Watery diarrhea, cholera, pandemic spread
Giardiasis
Morphology, clinical features: malabsorptive diarrhea.
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
6
Staphylococcus aureus:
Milk product and fatty food.
Acute explosive Exudative diarrhea.
Clostridium difficile :
Following antibiotic use, nosocomial acquisition Fever,
pain,
bloody
diarrhea,
Campylobacter :
Milk, poultry, animal (dog) contact.
Fever, pain, Secretory Diarrhea, dysentery
Clostridium perfringens: Produce gas gangrene
Others
Necrotizing enterocolitis
Acute, necrotizing inflammation of small and/or large intestines
Most common acquired GI emergency in premature or low birth weight
neonate
Mild GI symptoms or fulminant illness
Tuberculous
infection→
Transverse ulcer and Caseating granuloma
Pseudomembranous
colitis→
C. difficile.,
Gross and Micro: pseudomemnrane
Amebiasis→
Bloody
exudative
diarrhea
Flask shaped ulcer, complications: liver
abscess
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
7
Multifactorial - immaturity of the gut’s immune system
Release of cytokines and endotoxins damages mucosa and blood supply
Edema to necrosis to gangrenous bowel
Terminal ileum or ascending colon
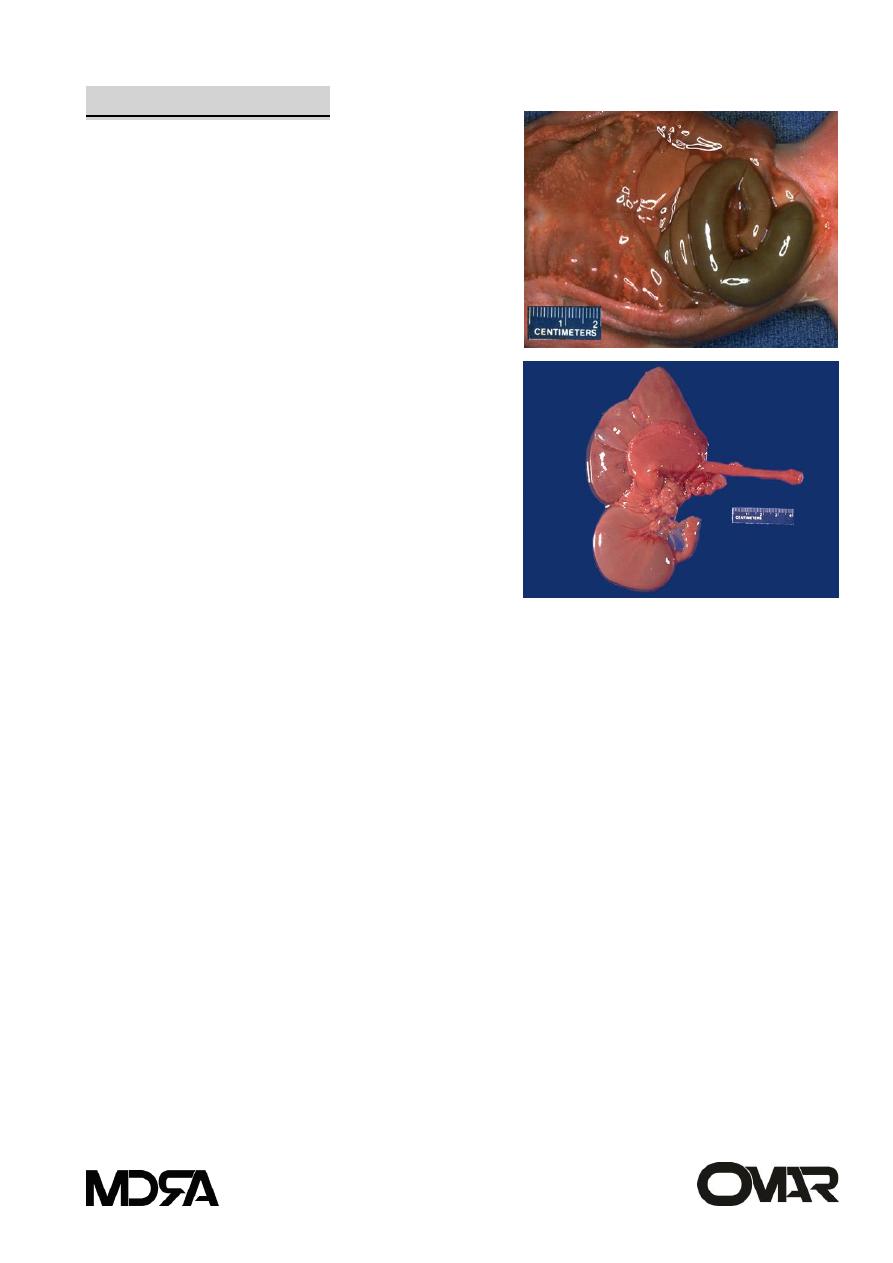
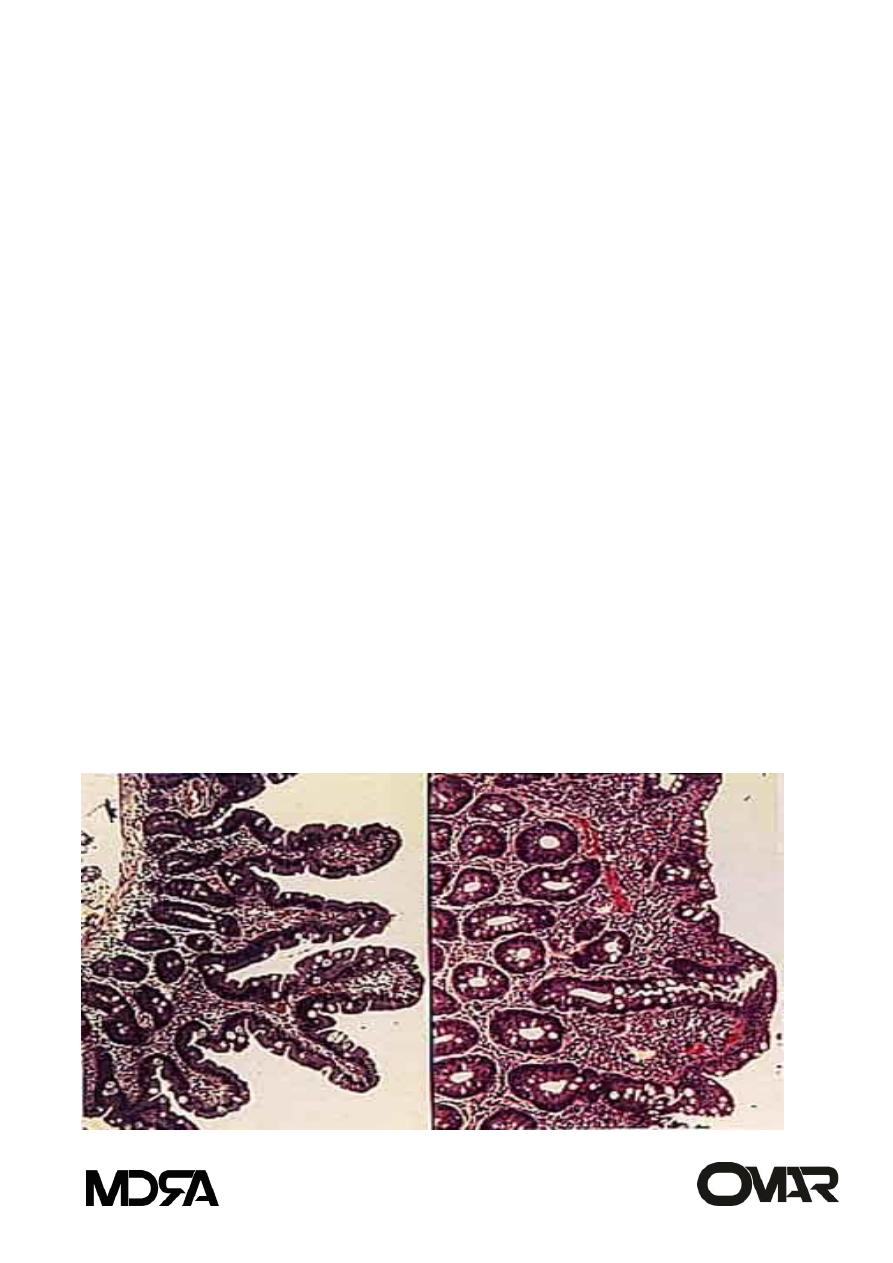
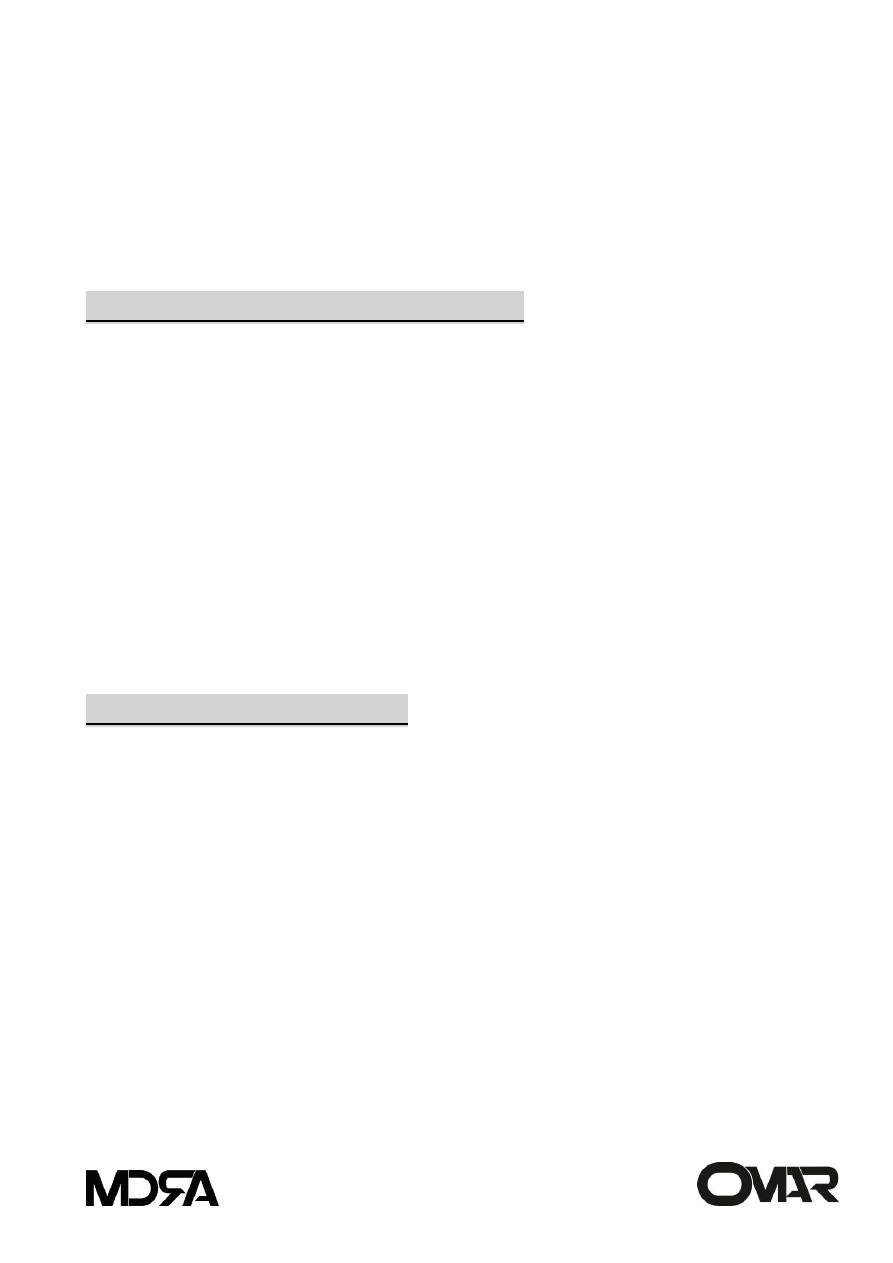
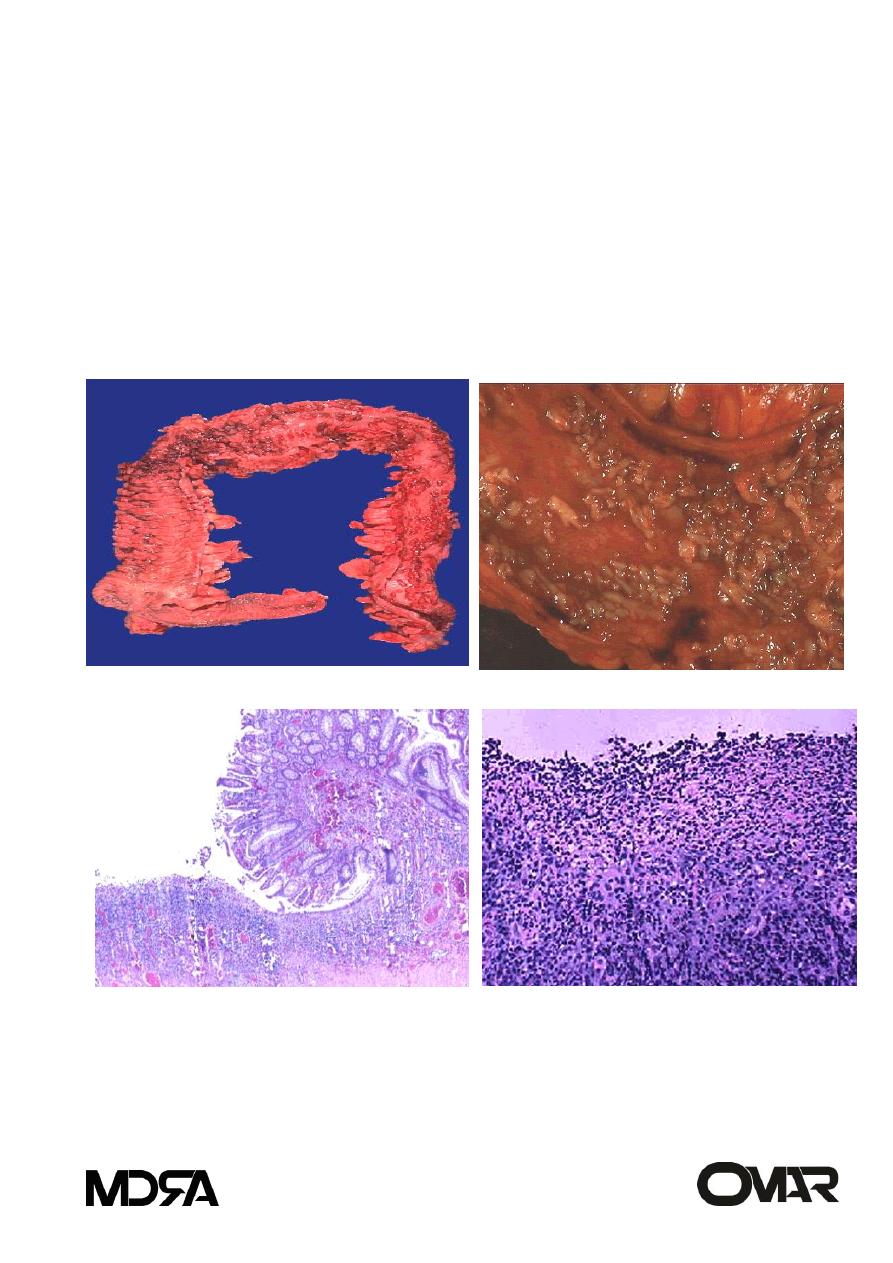
Morphology
NEC typically involve the terminal ileum,
cecum, & right colon. The involved
segment is .Distended, friable, and
congested, or it can be gangrenous.
Peroration with peritonitis is May be seen.
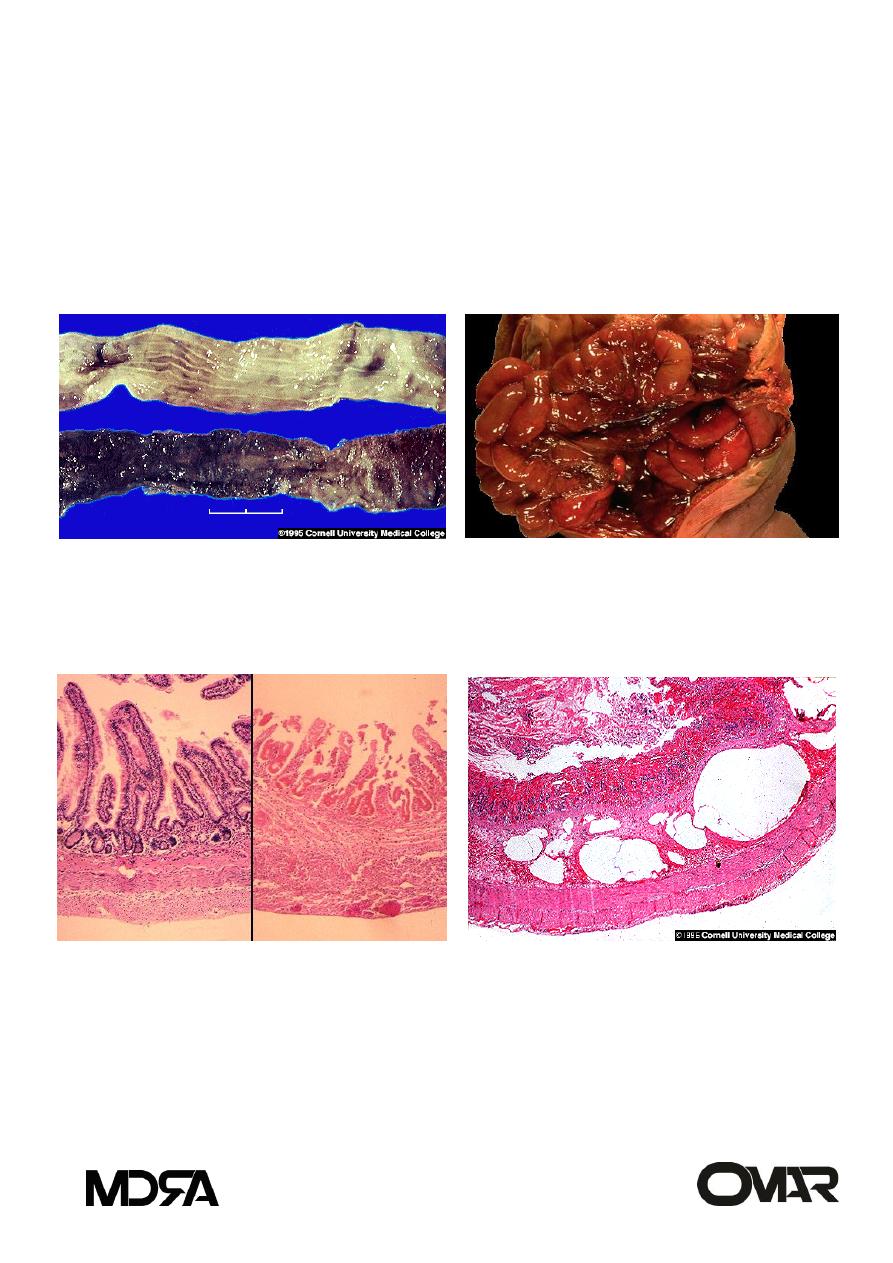
Necrotizing enterocolitis, mucosal surface (and
comparison with normal) .The bowel is
distended, congested, and often frankly
necrotic. (Compare the involved segment of
ntestine below with the more normal segment
above.)
Compared to normal bowel at the left,
bowel involved by NEC at the right shows
hemorrhagic
coagulative
necrosis,
beginning in the mucosa and extending to
involve the muscular wall, with the potential
for perforation.
Pneumatosis
intestinalis,
necrotizing
enterocolitis .Pneumatosis intestinalis, which
is present in many but not all cases, is
represented by submucosal or subserosal
gas-filled cysts.

GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
8
Transmural necrosis: when severe, the
necrosis may progressively involve all
layers of the bowel through to the serosa
(transmural).
This type of involvement, which begins at
the luminal aspect of the bowel, is typical
of ischemic injury.
The necrosis is accompanied by variable
amounts
of
inflammation
and
hemorrhage.
Pseudomembranous colitis
(antibiotic associated)
Yellow green false membrane (mixture of mucous and neutrophils)
Toxin produced by Clostridium difficile (acquired nasocomially in 20% of
pxs in long term hospitalization)
Antibiotics allow overgrowth of C. difficile
Sudden onset of fever and diarrhea in a patient who is seriously ill or
post operative who is receiving antibiotics
diarrhea, dehydration, shock death
Exotoxin A and B
binds to enteric receptors causing injury to actin filaments and
cell retraction
Malabsorption
Defect in the assimilation of food (digestion and absorption)
Intraluminal stage
a. Secretory Phase (Chronic pancreatitis/insufficiency)
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
9
b. Biliary Phase (Biliary obstruction due to calculus or tumor)
Intestinal Stage (terminal digestion)
a. Surface Phase (Celiac disease; bowel resection)
b. Cellular Phase (Disaccharidase deficiency)
Removal Stage (transepithelial transport)
a. Delivery Phase (Whipple diease)
Celiac sprue
Etiology and pathogenesis:
Gluten, gliadin protein in wheat, oat, barley, and rye
hypersensitivity (immunologic) reaction to gluten
90-95% - HLA DQ 2 or 8.
Whites - rare in native Africans, Japanese, Chinese
Gluten - malabsorption -gluten free - improvement
Long term risk of malignancy -lymphoma (2X normal)
Distinct from Tropical sprue
Infant
Failure to thrive
Apathy
Pallor
Anorexia
Abdominal distention/pain
Developmental Delay
Muscle wasting
Hypotonia
Stools soft, bulky, malodorous, clay-colored
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
10
Child
Anemia
Rickets
Low weight
Small stature
Irritability
Adult
Diarrhea/ steatorrhea
Weight loss
Cheilosis / glossitis / Apthous ulcers
Anemia
Anorexia/nausea/vomiting
Flatulence
Lactose/sucrose intolerance
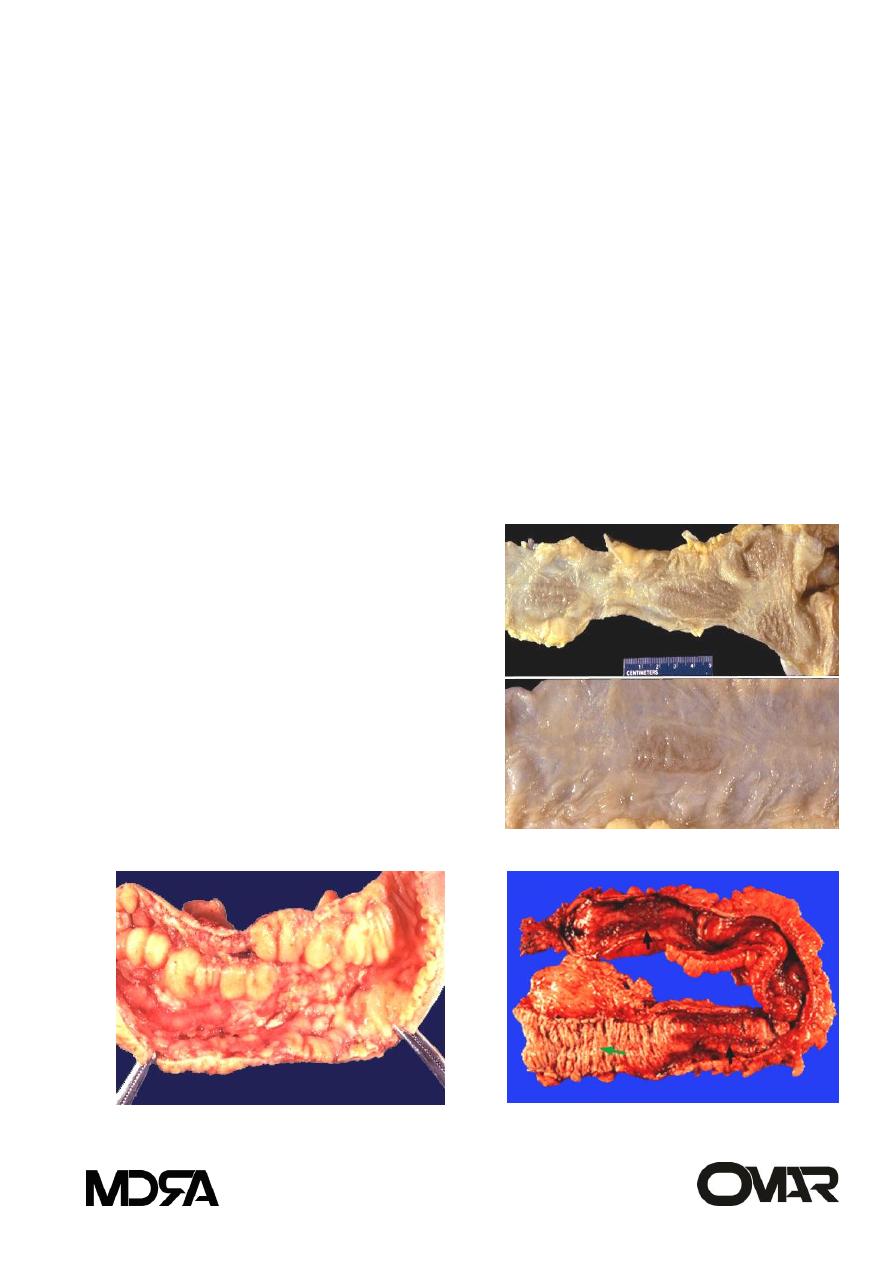
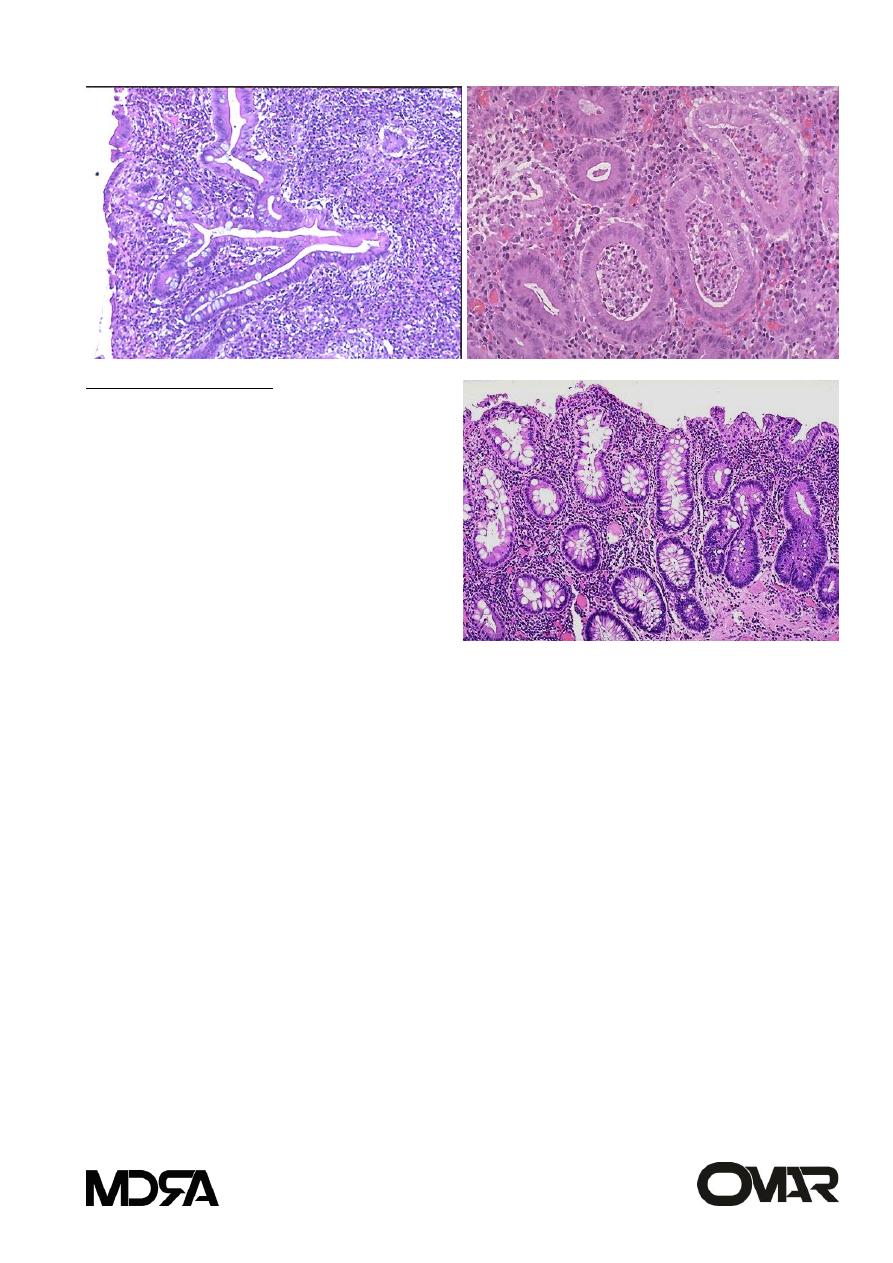
morphology
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
11
pathology
Excess lymphocytes
Hyperplastic crypts
Flattened villi
Hypoplasia
Blood tests
Antigliadin IgG and IgA
Endomysium IgA
Tissue transglutaminase IgA by ELISA
Total IgA
Tropical sprue
Occur in people living or visiting the tropics. (Caribbean, central and
south Africa, India, south east Asia, central and south America).
No specific cause.
Characterized by bacterial overgrowth by enterotoxigenic organisms,
e.g. E.coli, Hemophilus.
Morphology: variable, injury in cells, with increase in size of cells.
Malabsorption after the infection.
Treated by broad spectrum antibiotics.
Whipple disease
Rare systemic disease, affecting intestine, CNS and joints.
Gram positive rod shaped actinomycete: Tropheryma whippleli
Engulfed by macrophages (PAS positive diastase resistant)
Electron microscopy
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
12
Seen in intestinal mucosa, mesenteric lymph nodes, joints and other
systemic areas.
M:F 10:1, in fourth to fifth decade.
Mala, polyathritis, obscure CNS complaints.
Treated by antibiotics.
Bacterial overgrowth
The proximal small bowel is inhabitated by bacteria as in colon (aerobic
and anaerobic).
The small bowel is not sterile but the peristalsis prevents overgrowth,
which occur in:
1- Luminal stasis: stricture, fistula, diverticula, blind loop or pouch,
reduplication, motility disorders, post-surgical.
2- Hypochrlohydria or achlorhydria, by gastric mucosal atrophy or anti-
acid ingestion.
3- Immune deficiency.
The etiology of malabsorption will be multi-factorial:
1- bacterial deconjugation and dehydroxylation of luminal bile salts.
2- mucosal damage by bacterial enzymes.
3- bacterial inactivation of luminal lipase.
4- competition of nutrients.
Treated by appropriate antibiotics.
Disaccharidase deficiency
congenital = rare.
Acquired = common, by osmotic diarrhea.
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
13
Bacterial fermentation of unabsorbed sugar will cause hydrogen
production = pH of stool will be decreased.
Abetalipoproteinemia:
Autosomal recessive disease= no lipoprotein B accumulation of triglyceride in
mucosal cells.
Idiopathic Inflammatory Bowel disease
Inflammatory bowel disease (IBD) - single term to collectively refer to
either Crohn disease or ulcerative colitis
Etiology unknown
a. Genetic predisposition: HLA B27
b. Abnormal host immunoreactivity
C. infectious causes.
d. structural changes.
e. inflammation.
Inflammatory Bowel Disease
Consists of two inflammatory disorders - Crohn’s disease (CD) and
ulcerative colitis (UC)
Both are chronic, relapsing conditions of uncertain etiology
Both have systemic, extraintestinal inflammatory manifestations
Crohn disease: Regional enteritis GROSS EXAMINATION
1. Chronic inflammation involving all layers (transmural) of the SI
may occur at any point along the GI tract
primarily involving SI and LI.
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
14
40% SI Alone, 30% SI&LI, 30%colon alone. (may involve, duodenum,
stomach, esophagus and even mouth.
2. Mucosa shows linear ulceration and fistula
3. Segmental involvement/sparing
Serosal creeping fat
terminal ileitis as it was 1st described in 1930’s, regional ileitis,
granulomatous colitis.
4. Serosa is granular, dull and gray.
5. Wall is thick and rubbery.
6. Lumen is narrowed.
7. Sharp demarcation of diseased bowel
segment from adjacent un-involved
bowel wall. (when multiple segments
involved = skip lesions).
8. Cobble stone appearance.
9. Narrow fissures develop, penetrate
deeply cause bowel adhesion with fistula
formation, or sinus tract formation.
10. free perforation or localized abscess.
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
15
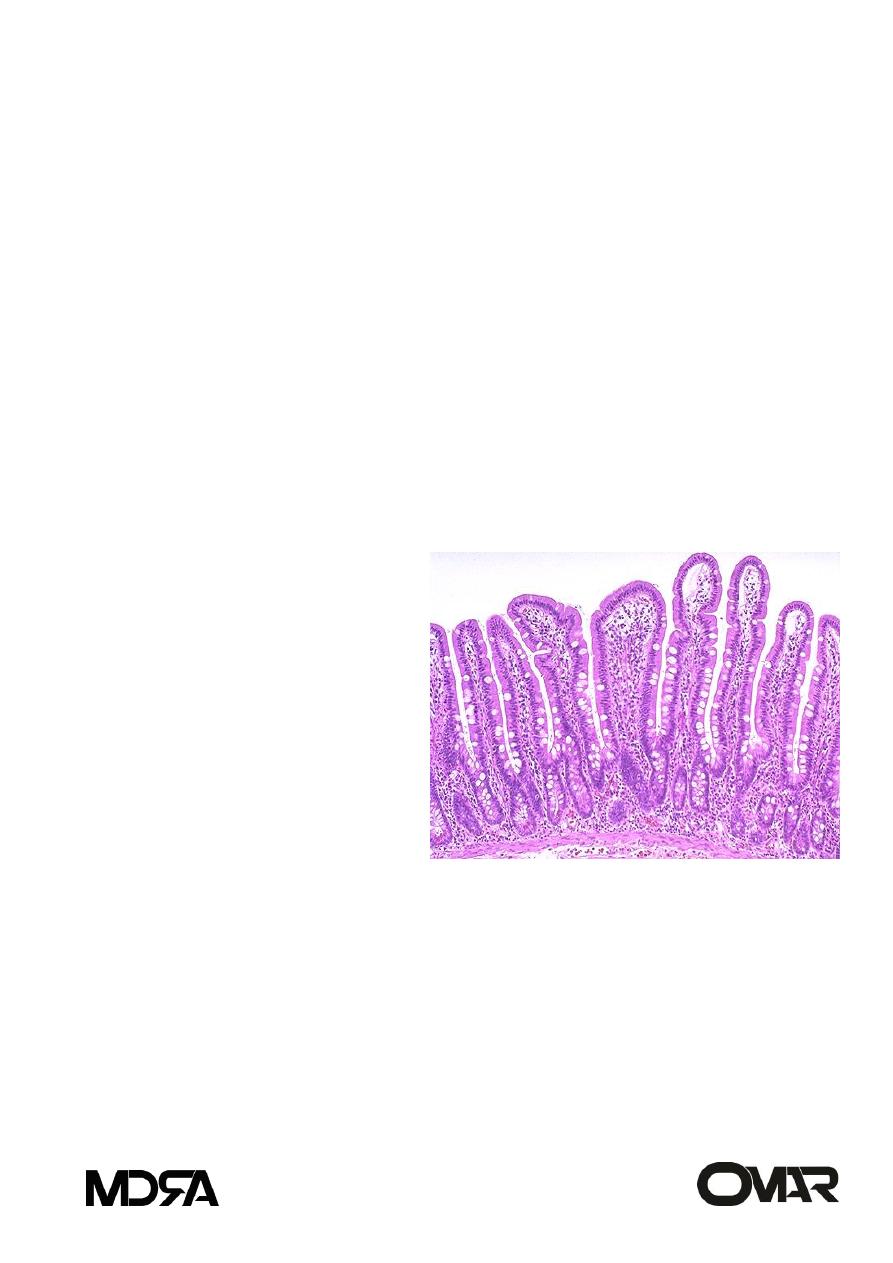
Crohn disease: microscopy:
Inflammation (transmural) spread through the bowel wall to adjacent
mesenteric fat.
Mucosal inflammation : neutrophils, and crypt abscess.
Ulceration in severe active disease.
Chronic mucosal damage (crypt distortion) with villous blunting in SI,
atrophic changes, and metapalsia.
-characteristic non-caseating granulomas ( seen in half of cases, in all
tissue layers, and involved and un involved areas).
CLINCAL FEATURES:
tends to occur in young
adults
diarrhea, crampy abdominal
pain, fever
complications:
1-fistula,
obstruction. 2- occult blood
loss, Fe++ def anemia. 3-
malabsorption,
malnutrition, weight loss. 4-
fistula and stricture. 5- extra intestinal manifestations: polyarthritis,
sacro ileitis, ankylosing spondilitis, erythematic nodosum, clubbing of
fingers, uveitis, amyloidosis, and increased incidence of cancer of SI and
colon in 5-6 fold increase in risk.
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
16
Ulcerative colitis
1. Inflammation primarily involving the mucosa of the colon.
2. Diffuse, continuous inflammation that begins in the rectum and progresses
proximally. Pancolitis in 20%, 10% of these have backwash ileitis, remaining
40-50% rectosigmoid.
3. Pseudopolyp formation.
4. With chronic disease, there is atrophy.
5. Serosa normal.
6. Bloody diarrhea, from ruptured vessels in inflamed mucosa
Toxic megacolon - rare complication - prominent dilatation and septic
shock.
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
17
MICROSCOPY:
Early phase: neutrophils accumulate within the depths of the crypts of
Leiberkuhn forming crypt abscesses.
Fibrosis cause crypt distortion. Mucous cell depletion.
Later phase: mucosa ulcerates and pseudo-polyps form
Late phase: after many years, mucosa becomes dysplastic, increasing
risk of colon carcinoma
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
18
Clinical features:
ATTACKS
OF
BLOODY
DIARRHEA.
days, weeks, months and then
subside.
Recur after months, and then
subside.
Could be only single attack.
PROGNOSIS:
60% mild disease.
97% relapse within 10 years.
30 % colectomy in first 3 years (uncontrollable disease).
Rarely fulminant = fatal.
RISK OF CANCER: dysplasia in multiple sites.
High in patients with pancolitis for 10 years or more, (20-30 fold increase
risk).
If 35 years, there is 30% cancer development.
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
19
Between Crohn and UC, this finding is more commonly seen in:
Non-neoplastic bowel diseases
a. Diverticular disease
b. Hernias
c. Adhesions
d. Intussusception
e. Volvulus
a-Diverticular disease:
Diverticulosis and Diverticulitis
Acquired herniation
Most common in left colon; particularly sigmoid colon
Acute or chronic inflammation may occur
Perforation, peritonitis, fistula
Acquired
rare under 30
western pop over 60 prevalence: 50%
Transmural inflammation--
Pseudopolyp---------------
Granuloma-----------------
Diffuse---------------------
skip lesions----------------
toxic Megacolon-----------
creeping fat----------------
Primary Sclerosing Cholangitis--
fissures and fistulas-------
Cancer----------------------
at any point in GI tract---
Rectum---------------------
Crohn
UC
Crohn
UC
Crohn
UC
Crohn
both but more in UC
Crohn
both but more in UC
Crohn
UC
Crohn
UC
Crohn
UC
Crohn
UC
Crohn
both but more in UC
Crohn
both but more in UC
Crohn
UC
GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
20
b- Hernias
-Serosal lined out-pouching of peritoneum
-Loop of intestines becomes trapped (incarcerated) within the hernia sac
-Bowel compressed, twisted at the mouth of hernia, compromising
blood supply - infarction (strangulation)
c- Adhesions
-string-like or band-like portions of scar tissue that form during healing
after surgery or peritonitis
-may result in obstruction (kinking, compression)
d- Intussusception
-caused by an in-folding or telescoping of one segment of bowel into the
adjacent distal segment
Infants and children: spontaneous and reversible
Adults: tumor is usually a lead point
e- Volvulus
-obstruction due to rotation or twisting of a loop of bowel around its
mesenteric base of attachment
Sigmoid - most common site (cecum next)
Inflammation
1. Miscellaneous
-graft vs. host
-drug induced
-radiation enterocolitis
-neutropenic colitis
-diversion colitis

GASTROINTESTINAL TRACT lecture 7-8 . Pathology Small and Large Intestines (1)
21
2. Acute appendicitis
-etiology: bacteria
-fecolith impairing circulation, causing ischemia, necrosis and bacterial
contamination
-acute abdomen -RLQ pain- McBurney’s point
-fever and leukocytosis
3. Collagenous and lymphocytic colitis
Etiology: unknown
possibly auto-immune
chronic watery diarrhea in middle aged and older women
spectrum of disease ranging from increased intraepithelial lymphocytes to
the presence of collagen band under the surface epithelium.
