
Rheumatic heart disease

Acute rheumatic fever
Incidence :
Children and young adult 5-15 yr
Rare in high income countries
Endemic in India , africa and south america
Pathogenesis
Triggered by an immune-mediated delayed response to infection with
specific strains of group A streptococci, which have antigens that may cross-
react with cardiac myosin and sarcolemmal membrane protein
Histologically, fibrinoid degeneration is seen in the collagen of
connective tissues. Aschoff nodules are pathognomonic and occur only in
the heart.

Clinical features
• multisystem disorder that usually presents with fever, anorexia, lethargy
and joint pain, 2
–3 weeks after an episode of streptococcal pharyngitis.
• Only about 25% of patients will have a positive culture for group A
streptococcus
• Serological evidence of recent infection with a raised antistreptolysin O
(ASO) antibody titre is helpful.
• A presumptive diagnosis of acute rheumatic fever can be made without
evidence of preceding streptococcal infection in cases of isolated chorea
or pancarditis, if other causes for these have been excluded
• The diagnosis, made using the revised Jones criteria
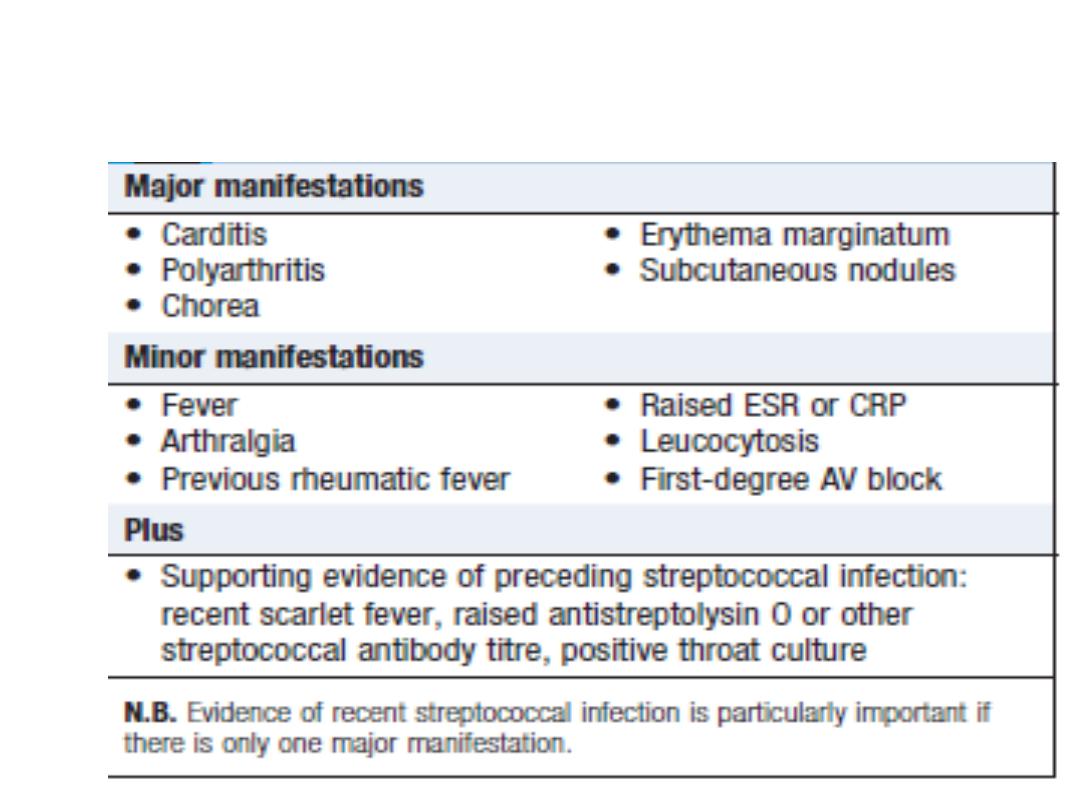
Revised Jones Criteria
Carditis
• Pancarditis
• Incidence declines with increasing age
• Manifestation :
SOB ….. HF and PE
Palpitation
Chest pain
Tachycardia
Murmur …. Systolic and diastolic ( Carey coombs )
AR in 50 %
Pericarditis
ECG …. ST-T ; conduction defect

Arthritis
• The most common major manifestation ( 75 %)
• Occurs early when streptococcal antibody titres are
high
• Acute painful asymmetric and migratory inflammation
of the large joints typically affects the knees, ankles,
elbows and wrists
• The pain characteristically responds to aspirin; if not,
the diagnosis is in doubt

Skin lesions
• Erythema marginatum : Occurs in less than 5 % ; occur mainly on the
trunk and proximal extremities but not the face.
• Subcutaneous nodules occur in 5–7% of patients. They are small (0.5–
2.0 cm), firm and painless, and are best felt over extensor surfaces of
bone or tendons. They typically appear more than 3 weeks after the onset
of other manifestations and therefore help to confirm rather than make
the diagnosis.
• Other systemic manifestations are rare but include pleurisy, pleural
effusion and pneumonia.

Sydenham’s chorea (St Vitus dance)
• late neurological manifestation , appears at least 3 months
after the episode of acute rheumatic fever
• Occurs in up to one-third of cases
• more common in females
• Spontaneous recovery usually occurs within a few months.
• one-quarter of affected patients will go on to develop chronic
rheumatic valve disease.
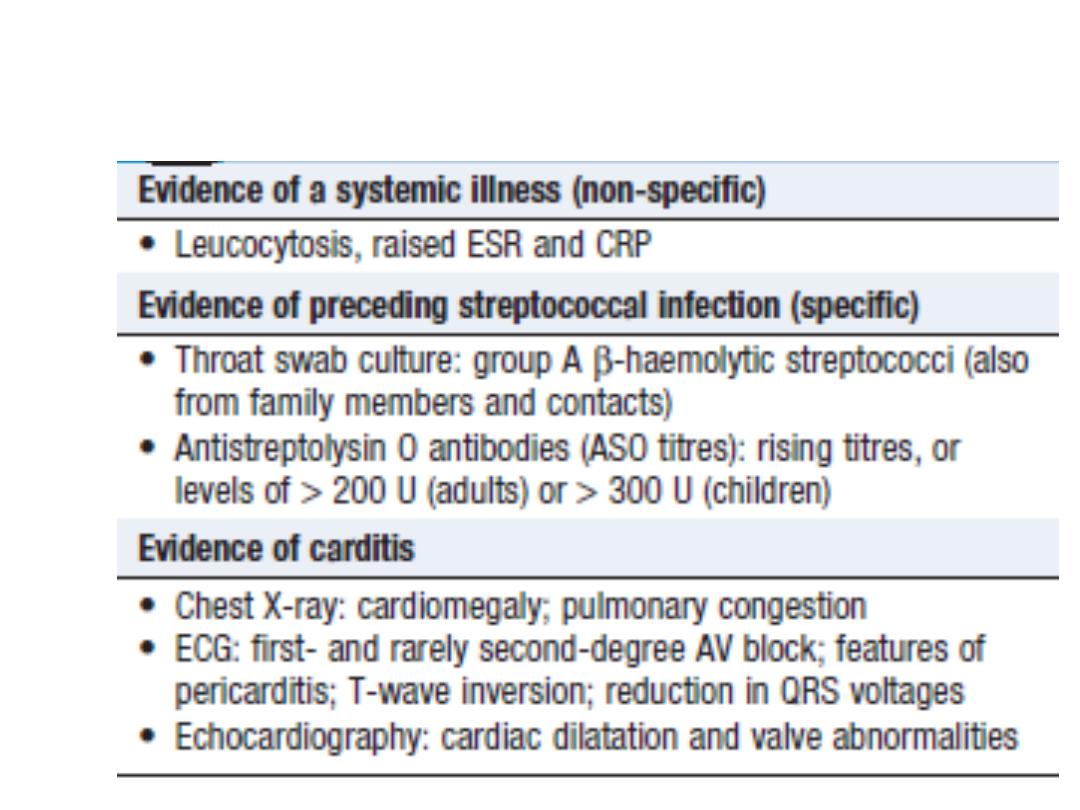
Investigations

Management of the acute attack
• A single dose of benzyl penicillin (1.2 million U IM) or oral
phenoxymethylpenicillin (250 mg 4 times daily for 10 days)
•
Bed rest and supportive therapy
•
Aspirin
•
Corticosteroids
Secondary prevention
• Long term prophylaxis with penicillin should be given as
benzathine penicillin (1.2 million U IM monthly), if compliance
is in doubt, or oral phenoxymethylpenicillin (250 mg twice
daily). Sulfadiazine or erythromycin may be used if the patient
is allergic to penicillin
• Further attacks of rheumatic fever are unusual after the age of
21
• In those with residual heart disease, prophylaxis should
continue until 10 years after the last episode or 40 years of
age, whichever is later.

Chronic rheumatic heart disease
• Chronic valvular heart disease develops in at least half of
those affected by rheumatic fever with carditis.
• Twothirds of cases occur in women
• it is only possible to elicit a history of rheumatic fever or
chorea in about half of all patients with chronic rheumatic
heart disease.
• The mitral valve is affected in more than 90% of cases
