HYPERTENSION
THE SILENT KILLER

introduction:
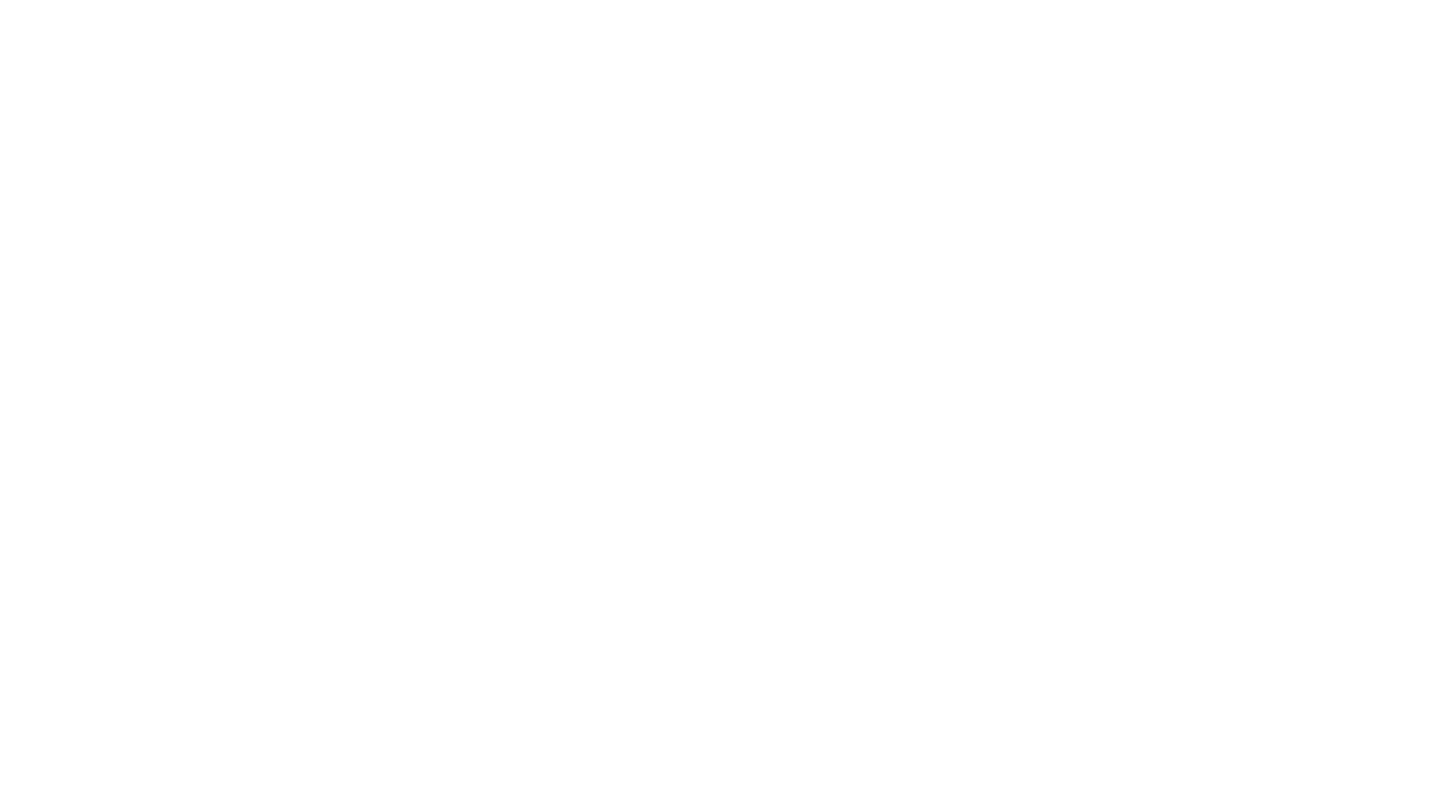
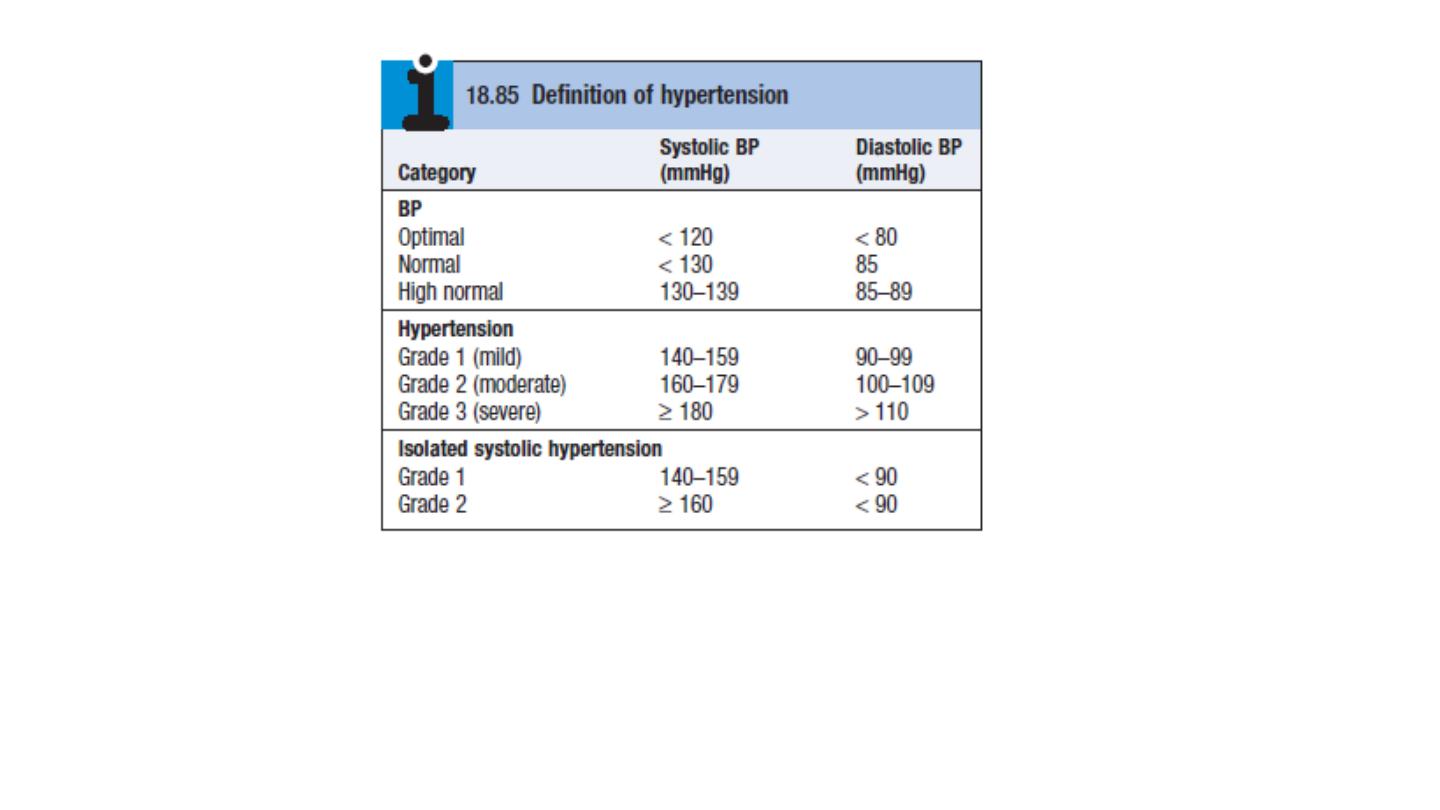
Blood pressure values are continuous variables, so the definition of
hypertension is arbitrary. Systemic BP rises with age.
incidence of cardiovascular disease (particularly stroke and coronary
artery disease) is closely related to average BP at all ages, even when
BP readings are within the so-called ‘normal range.
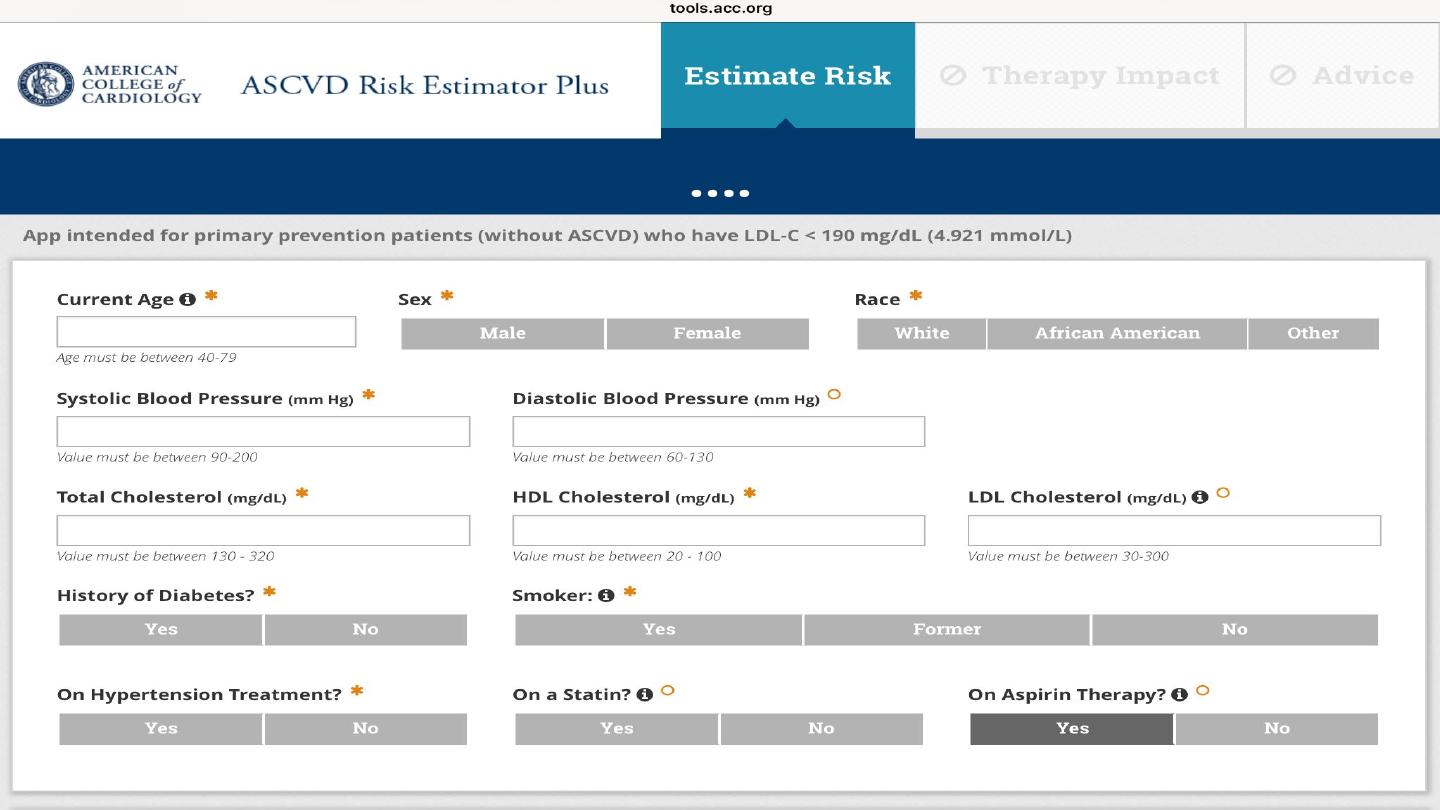
The cardiovascular risks associated with BP depend upon the
combination of risk factors in an individual, such as age, gender, weight,
physical activity, smoking, family history, serum cholesterol, diabetes
mellitus and pre-existing vascular disease

Etiology:
Primary , essential HPT account for 95%, no obvious cause can be
identified. The pathogenesis is not clearly understood. Many
factors may contribute to its development, including renal
dysfunction, peripheral resistance vessel tone, endothelial
dysfunction, autonomic tone, insulin resistance and neurohumoral
factors.
Hypertension is more common in some ethnic groups, particularly
African Americans and Japanese
, and approximately 40–60% is
explained by genetic factors.
Important environmental factors include a high salt intake, heavy
consumption of alcohol, obesity, lack of exercise and impaired
intrauterine growth. There is little evidence that ‘stress’ causes
hypertension

Hypertension is predominantly an asymptomatic condition and the
diagnosis is usually made at routine examination or when a
complication arises.
A BP check is advisable every 5 years in adults.

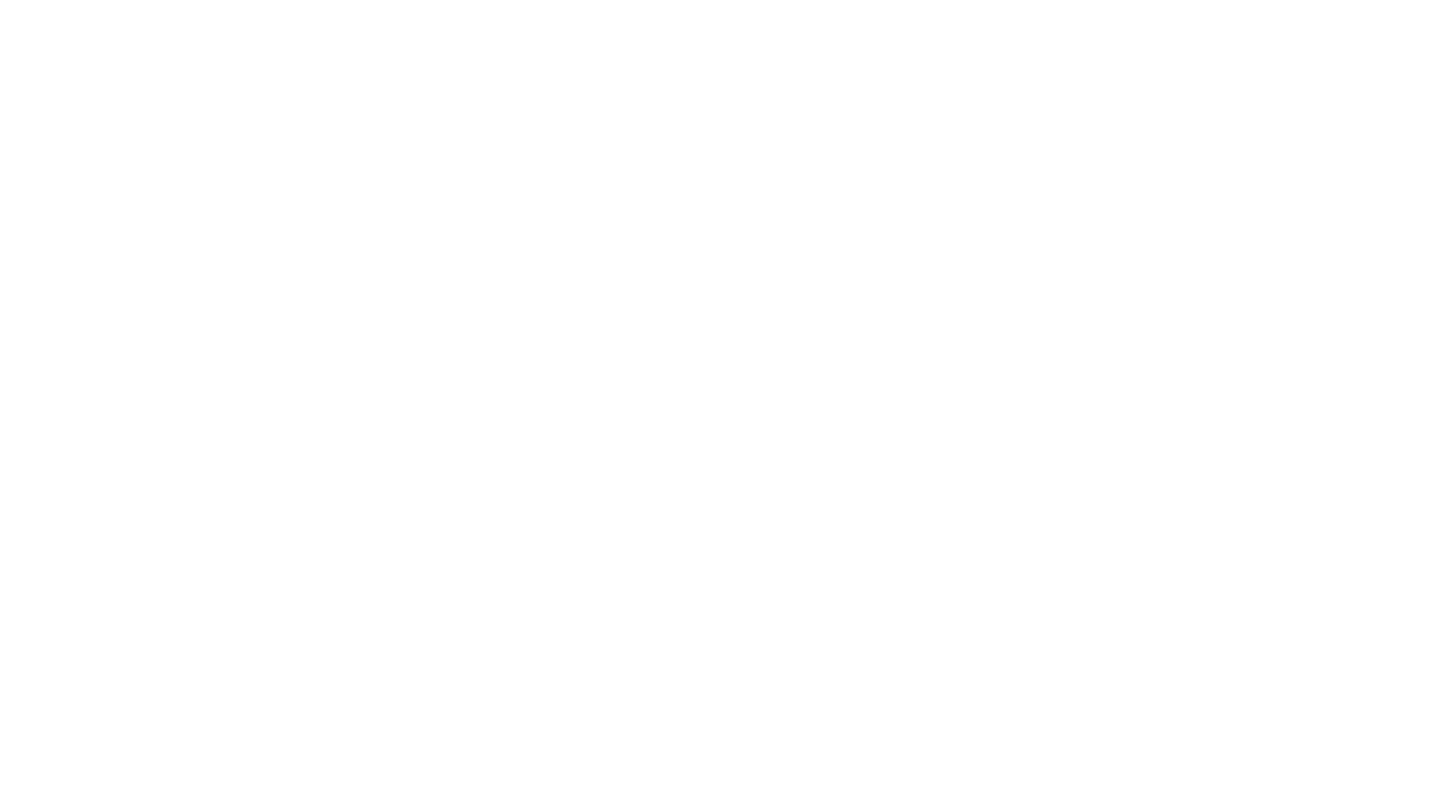
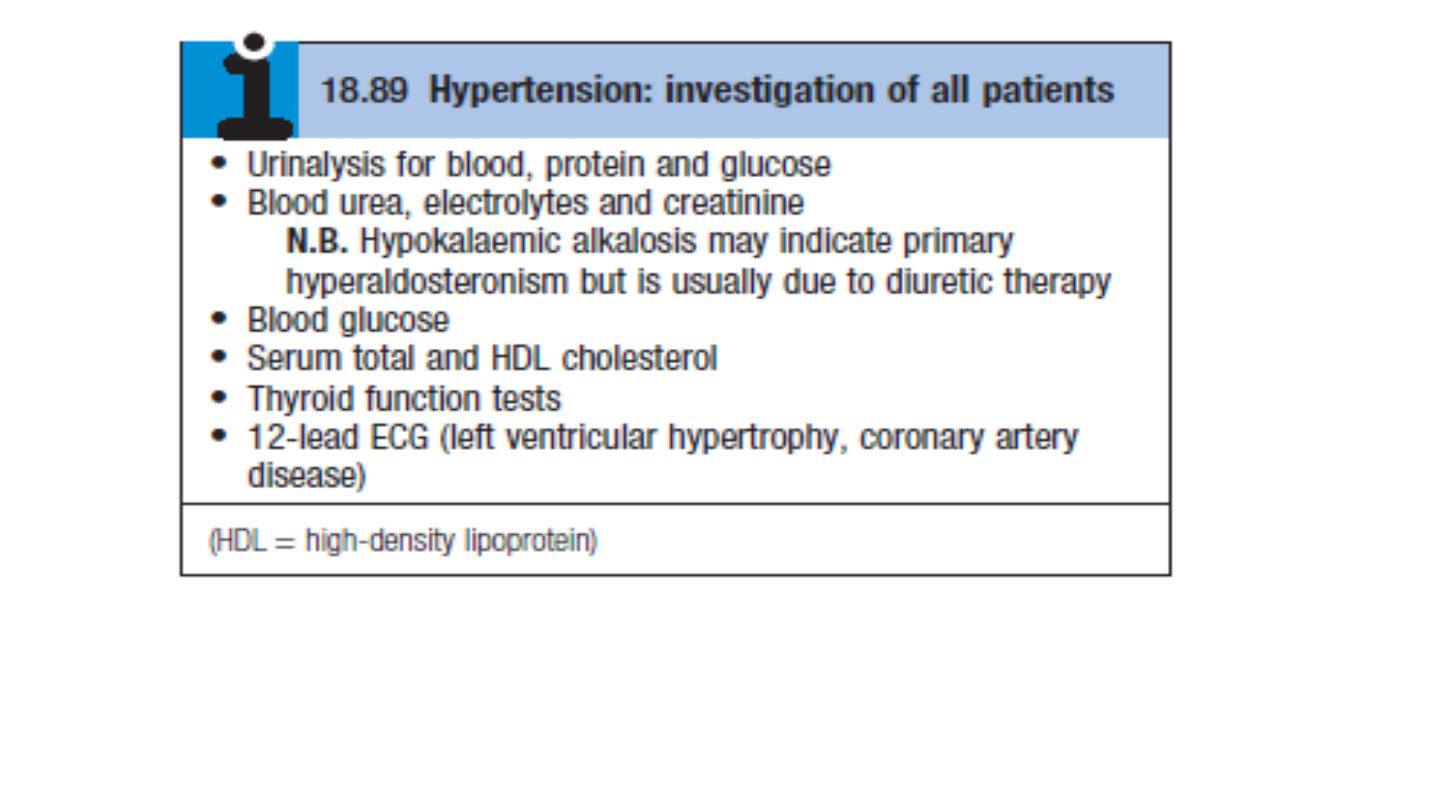
Initial evaluation
1. Accurate measurement of blood pressure
2. Identify possible secondary causes
3. Assess comorbidities and other risk factors
4. Detect any complication
This can be assessed by:
History
Physical examination
investigation
Measurement of blood pressure
Antihypertensive once started → life long treatment

Tight cuff → high pressure readings
Large cuff → low pressure readings
White coat hypertension:
Exercise, anxiety, discomfort and unfamiliar surroundings can all lead to
a transient rise in BP. as many as 20% of patients with apparent
hypertension in the clinic may have a normal BP when it is recorded by
automated devices used at home. The risk of cardiovascular disease in
these patients is less than that in patients with sustained hypertension
but greater than that in normotensive subjects.
ambulatory BP measurements obtained over 24 hours or longer
provides a better profile than a limited number of clinic readings and
correlates more closely with evidence of target organ damage than
casual BP measurements.

Home or ambulatory BP measurements are particularly helpful in
patients with unusually labile BP, those with refractory hypertension,
those who may have symptomatic hypotension, and those in whom
white coat hypertension is suspected.
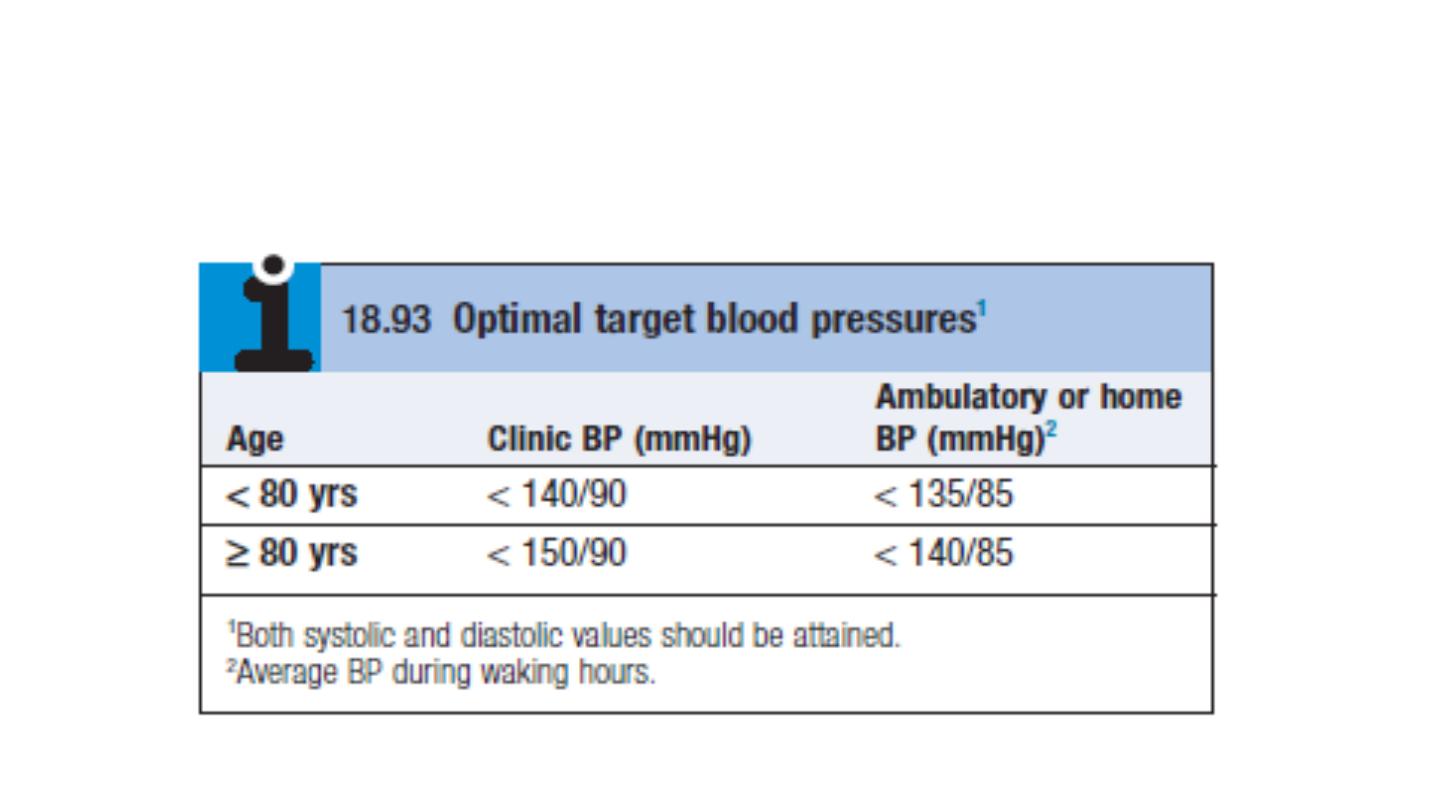
However, treatment thresholds and targets must be adjusted
downwards because ambulatory BP readings are systematically lower
(approximately 12/7mmHg) than clinic measurements.

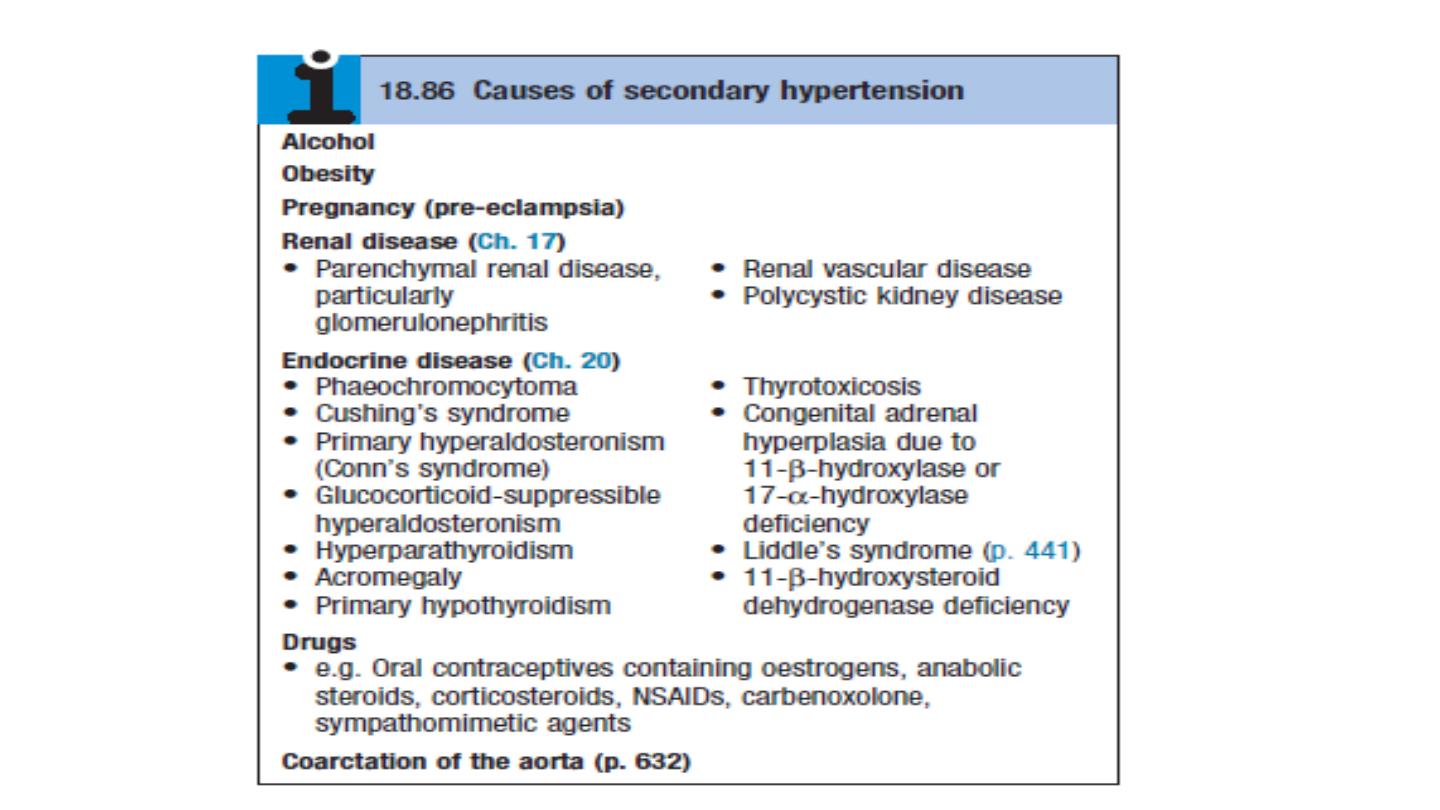
History
Family history, lifestyle (exercise, salt intake, smoking habit) and other risk
factors should be recorded.
A careful history will identify those patients with drug- or alcohol-induced
hypertension and may elicit the symptoms of other causes of secondary
hypertension such as phaeochromocytoma (paroxysmal headache,
palpitation and sweating or complications such as coronary artery disease
(e.g. angina, breathlessness).

EXAMINATION
Radio-femoral delay (coarctation of the aorta), enlarged kidneys
(polycystic kidney disease), abdominal bruits (renal artery stenosis) and
the characteristic facies and habitus of Cushing’s syndrome are all
examples of physical signs that may help to identify causes of
secondary hypertension .
Examination may also reveal features of important risk factors such as
central obesity and hyperlipidaemia (tendon xanthomas etc.).
Most abnormal signs are due to the complications of hypertension.
Non-specific findings may include left ventricular hypertrophy (apical
heave), accentuation of the aortic component of the second heart
sound, and a fourth heart sound. The optic fundi are often abnormal
and there may be evidence of generalised atheroma or specific
complications such as aortic aneurysm or peripheral vascular disease.

Target organ damage
1. Blood vessels
In larger arteries (> 1 mm in diameter), the internal elastic lamina is
thickened, smooth muscle is hypertrophied and fibrous tissue is
deposited. The vessels dilate and become tortuous, and their walls
become less compliant.
In smaller arteries (< 1 mm), hyaline arteriosclerosis occurs in the wall,
the lumen narrows and aneurysms may develop.
Hypertension is a major risk factor in the pathogenesis of aortic
aneurysm and aortic dissection.
Wide spread atherosclerosis

2. CNS
Stroke:
Stroke is a common complication of hypertension and
may be due to cerebral haemorrhage or infarction. Carotid
atheroma and transient ischaemic attacks are more common
in hypertensive patients. Subarachnoid haemorrhage is also
associated with hypertension
Hypertensive encephalopathy
is a rare condition characterised by
high BP and neurological symptoms, including transient disturbances of
speech or vision, paraesthesiae, disorientation, fits and loss of
consciousness. Papilloedema is common. A CT scan of the brain often
shows haemorrhage in and around the basal ganglia; however, the
neurological deficit is usually reversible if the hypertension is properly
controlled.

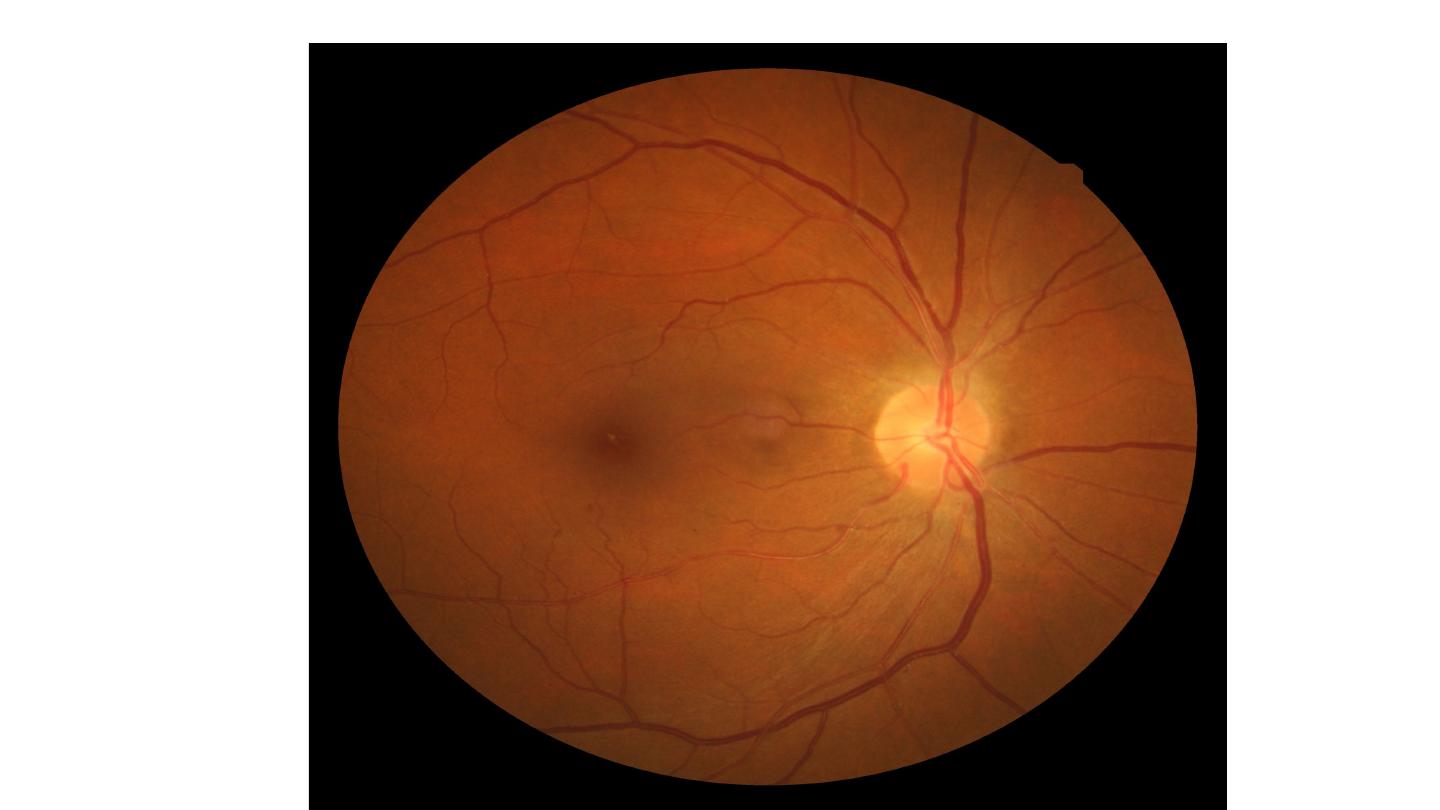
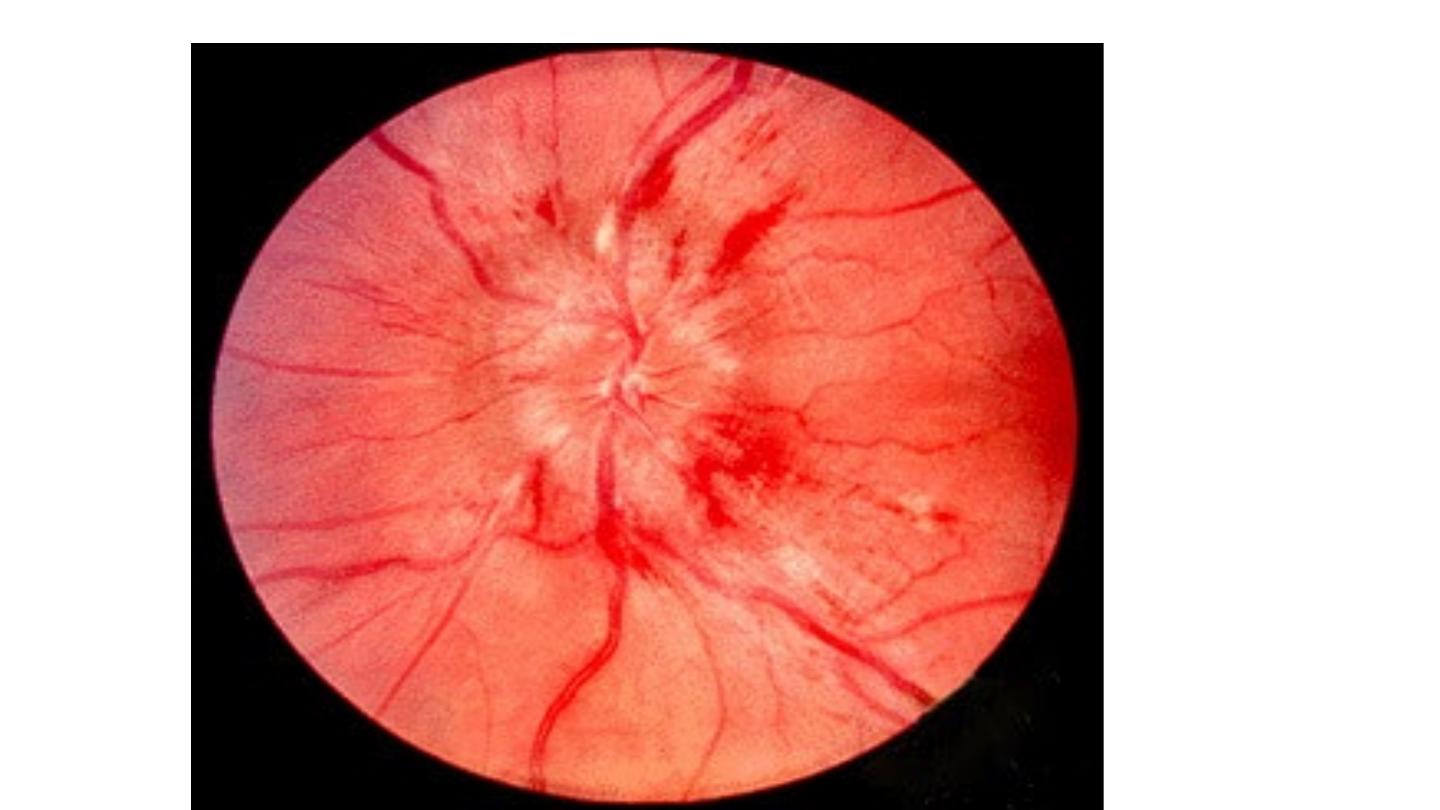
3. retina
Retina The optic fundi reveal a gradation of changes linked to the
severity of hypertension; fundoscopy can, therefore, provide an
indication of the arteriolar damage occurring elsewhere ‘Cotton wool’
exudates are associated with retinal ischaemia or infarction, and fade in
a few weeks . ‘Hard’ exudates (small, white, dense deposits of lipid)
and microaneurysms (‘dot’ haemorrhages) are more characteristic of
diabetic retinopathy . Hypertension is also associated with central
retinal vein thrombosis


4. Heart
The excess cardiac mortality and morbidity associated with hypertension are
largely due to a higher incidence of coronary artery disease. High BP places a
pressure load on the heart and may lead to left ventricular hypertrophy with
a forceful apex beat and fourth heart sound. ECG or echocardiographic
evidence of left ventricular hypertrophy is highly predictive of cardiovascular
complications and therefore particularly useful in risk assessment. Atrial
fibrillation is common and may be due to diastolic dysfunction caused by left
ventricular hypertrophy or the effects of coronary artery disease. Severe
hypertension can cause left ventricular failure in the absence of coronary
artery disease, particularly when renal function, and therefore sodium
excretion, is impaired.
5. Kidneys
Long-standing hypertension may cause proteinuria and progressive
renal failure by damaging the renal vasculature.

‘Malignant’ or ‘accelerated’ phase hypertension
characterised by accelerated microvascular damage with necrosis in the
walls of small arteries and arterioles (‘fibrinoid necrosis’) and by
intravascular thrombosis.
The diagnosis is based on evidence of high BP and rapidly progressive
end organ damage, such as retinopathy (grade 3 or 4), renal
dysfunction (especially proteinuria) and/or hypertensive
encephalopathy . Left ventricular failure may occur and, if this is
untreated, death occurs within months.

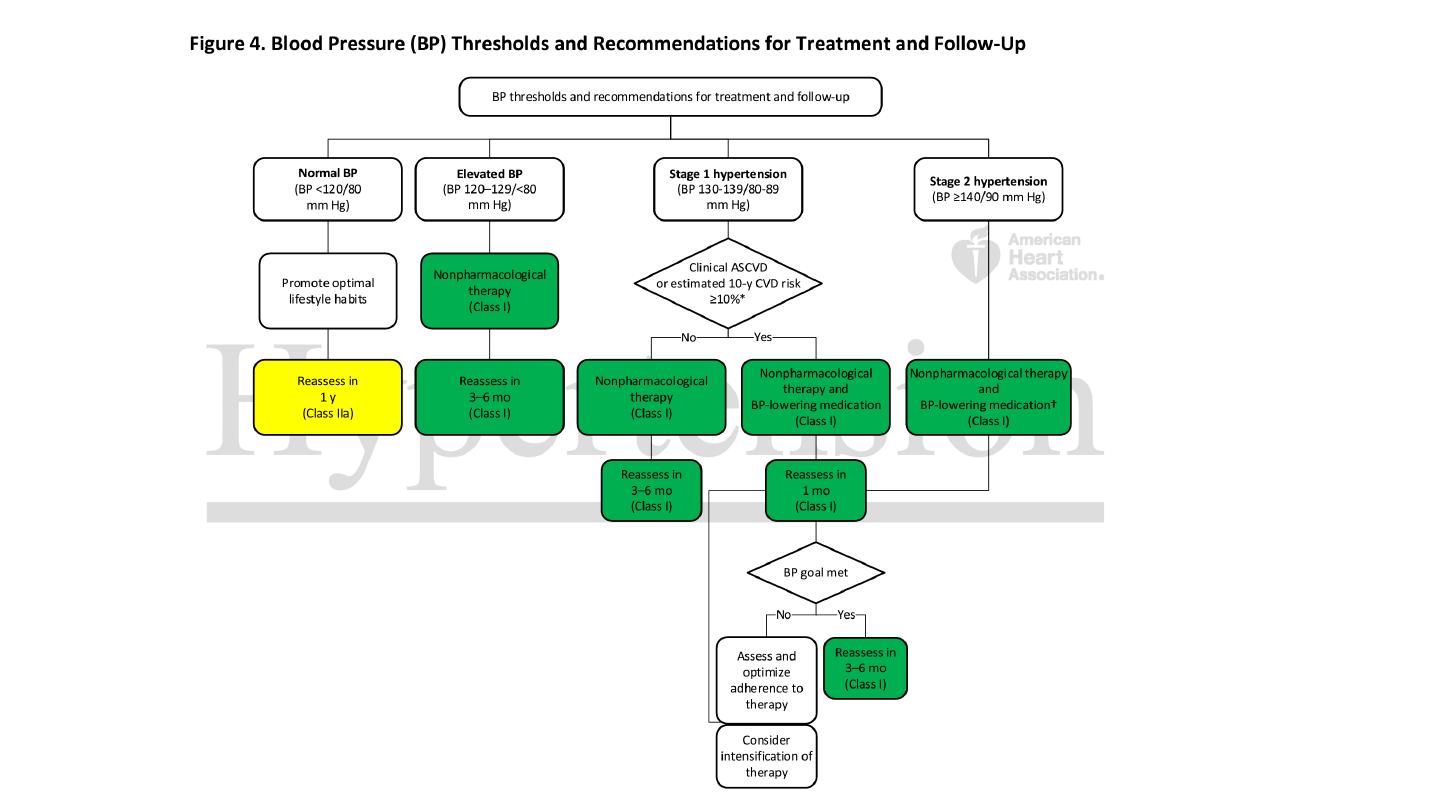
Threshold for intervention
Systolic BP and diastolic BP are both powerful predictors of
cardiovascular risk.

HPT IN ELDERLY
Prevalence: affects more than half of all people over the age of 60 yrs
(including isolated systolic hypertension).
Risks: hypertension is the most important risk factor for MI, heart failure
and stroke in older people.
Benefit of treatment: absolute benefit from therapy is greatest in older
people (at least up to age 80 yrs).
Target BP: similar to that for younger patients.
Tolerance of treatment: antihypertensives are tolerated as well as in
younger patients.
Drug of choice: low-dose thiazides but, in the presence of coexistent disease
(e.g. gout, diabetes), other agents may be more appropriate.

Management
The sole objective of antihypertensive therapy is to reduce the
incidence of adverse cardiovascular events, particularly coronary
artery disease, stroke and heart failure.
The relative benefit of antihypertensive therapy (approximately
30% reduction in risk of stroke and 20% reduction in risk of
coronary heart disease) is similar in all patient groups, so the
absolute benefit of treatment (total number of events
prevented) is greatest in those at highest risk.

Threshold for intervention
Systolic BP and diastolic BP are both powerful predictors of
cardiovascular risk. The British Hypertension Society
management guidelines therefore utilise both readings, and
treatment should be initiated if they exceed the given threshold
Diabetes and established cardiovascular at particular higher risk, so the
threshold for initiation of therapy is lower.
Patients taking antihypertensive therapy require follow-up at 3 monthly
intervals to monitor BP, minimize side-effects and reinforce lifestyle
advice.

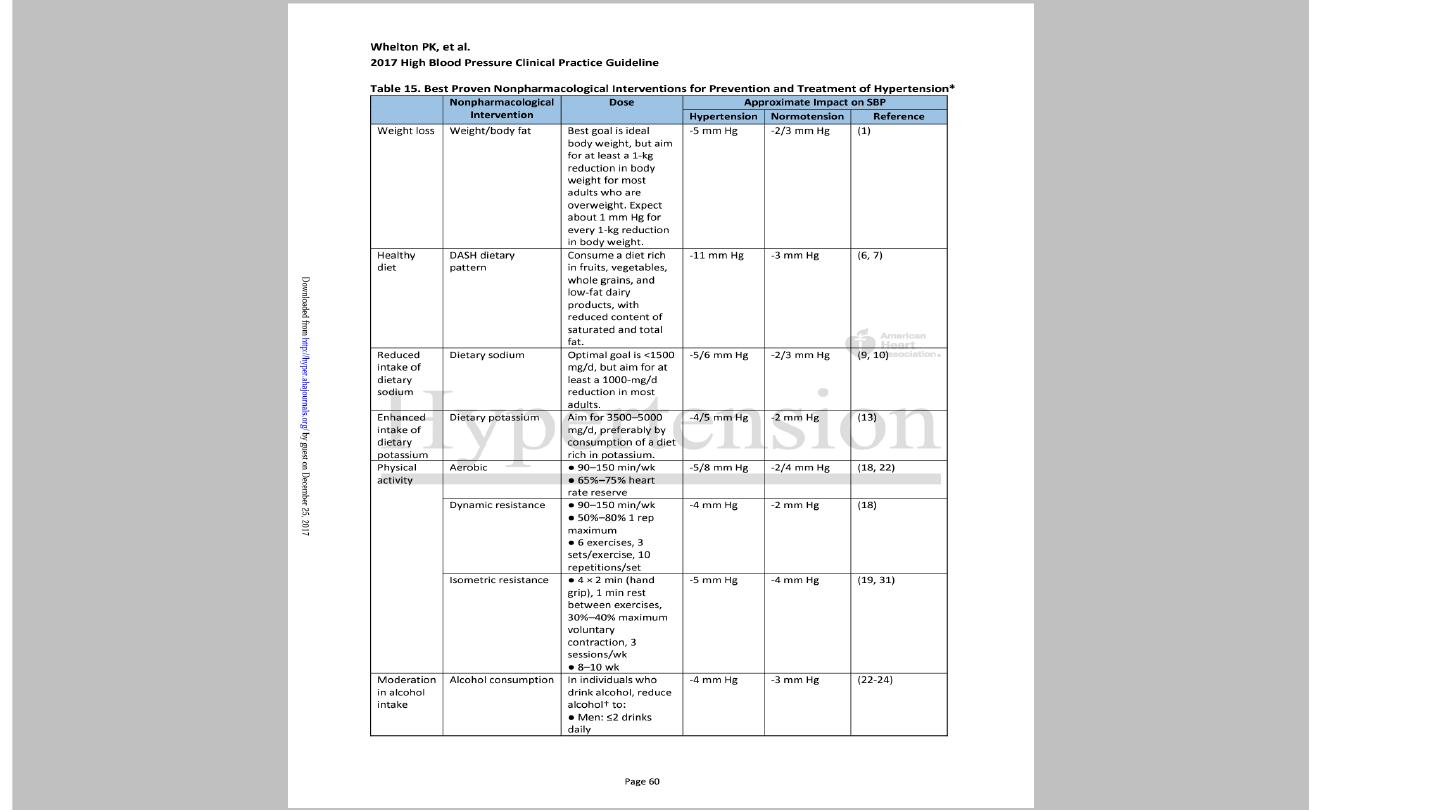
Non drug therapy
Correcting obesity, reducing alcohol intake, restricting salt intake,
taking regular physical exercise and increasing consumption of fruit
and vegetables can all lower BP.
Moreover, quitting smoking, eating oily fish and adopting a diet that is
low in saturated fat may produce further reductions in cardiovascular
risk.

Antihypertensive drugs
Diuretics
Thiazide :
The mechanism of action of these drugs is incompletely understood and it may take up to a
month for the maximum effect to be observed.
e.g Bendroflumethiazide 2.5 mg, Hydrochlorthalidone 50 mg, indapamide 1.5 mg.
S.E : hypokalemia, hyperyrecemia ( can cause gout), hyprglycemia, hypertryglycemia
Loop diuretics
: used as antihypertensive in cases with CRF, GFR less than 30 ml/kg/min
Angiotensin converting enzyme inhibitors:
Angiotensin l converted via ACE to angiotensin ll which cause
vasoconstriction and Stimulate the release of aldosterone from adrenals.
Blocking this pathway result in hypotensive effect.
ACE inhibitors should be used with particular care in patients with impaired
renal function or renal artery stenosis because they can reduce the filtration
pressure in the glomeruli and precipitate renal failure.
Electrolyte should be checked 1 to 2 weeks after initiation of therapy up to
30 % woresning in renal function is accepted, more woresning indicate
stopping ACE inhibitors.
e.g Captopril , enalopril, lisinporil, ramipril, perindopril.
S.E: Dry cough 15 %, angioedema 1 %, hyperkalemia, rash, renal
dysfunction, Neutropenia(captopril)
•
Bradykinin is inflammatory mediators which promote vasodilatation,
degraded by ACE, ACE inhibitors result in accumulation of bradykinin
which give additional antihypetensive effect.
•
Bradykinin is the cause of ACE inhibitors dry cough.
•
ACE inhibtors induced dry cough is indication to stop ACE I hibitors
and to swich to ARB

ARB: angiotensin receptor blockers
e.g: Losartan, Valsartan, telmisartan, candesartan, irbesartan.
Block angiotensin 2 receptor.
Combination of ACE and ARB has no additional antihypertensive effect ,
carry high risk of hyperkalemia and should be avoided.
ARB causing No dry cough, no angioedema, but share the same side
effect with ACE inhibitors Hyperkalemia and renal dysfunction.

Calcium channel antagonists
Dihyropyridine: Nifedipine, felodipine, amlodipine
Non dihydropidine : diltiazim, verapamil
S.E: Flushing , leg edema, effect on HR ( tachycardia with
dihydropyridine and bradycardia with non dihydropyridine)
Constipation

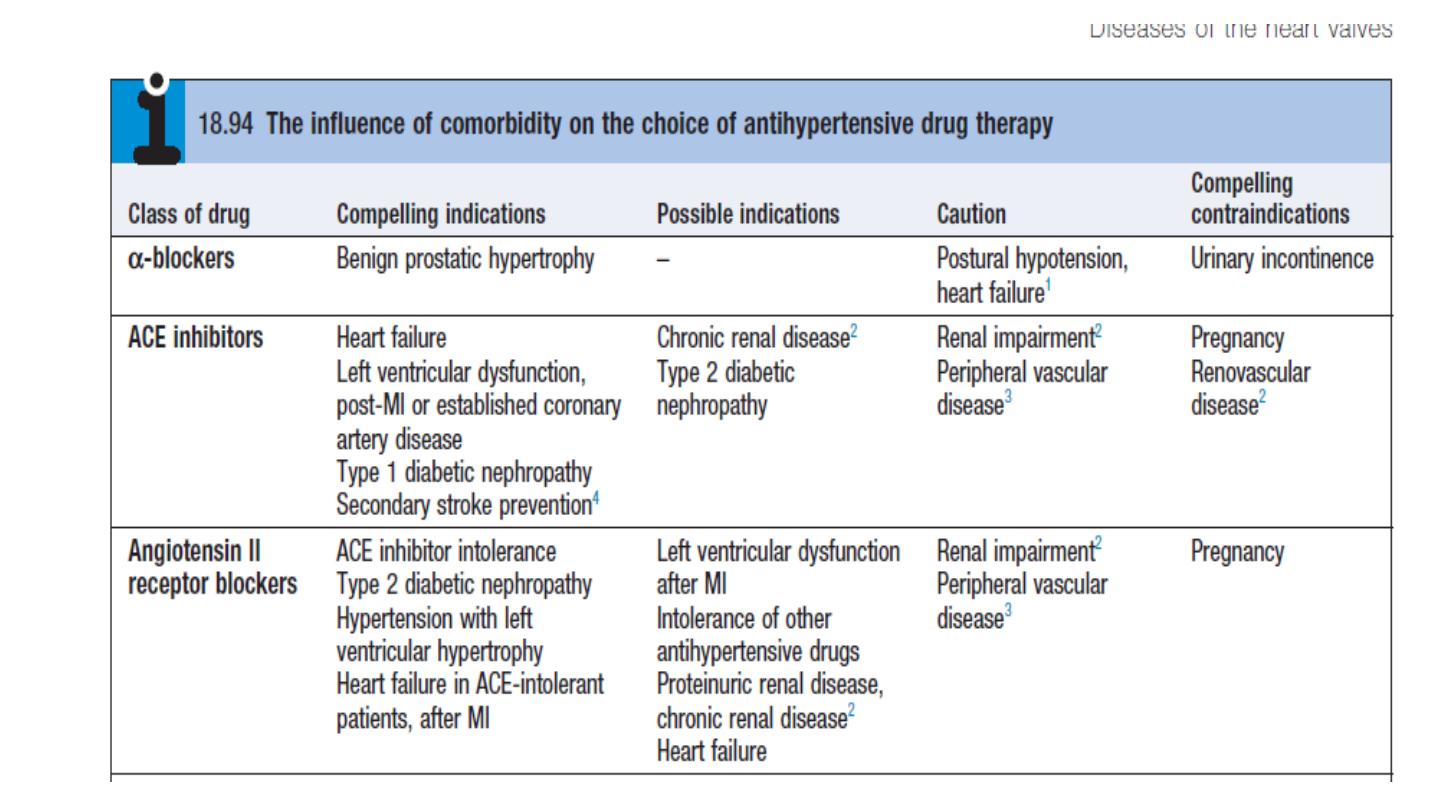
Beta-blockers.
These are no longer used as first-line antihypertensive therapy, except
in patients with another indication for the drug (e.g. angina).
Carvedilol and labetalol combined alpha and beta blocker

OTHER DRUGS
Alpha blockers: such as prazosin (0.5–20 mg daily in divided doses),
indoramin (25–100 mg twice daily) and doxazosin (1–16 mg daily
Alpha methyl dopa
Direct vasodilator: hydralazine (25–100 mg twice daily) and minoxidil
(10–50 mg daily).
Side-effects include first-dose and postural hypotension, headache,
tachycardia and fluid retention. Minoxidil also causes increased facial
hair and is therefore unsuitable for female patients.

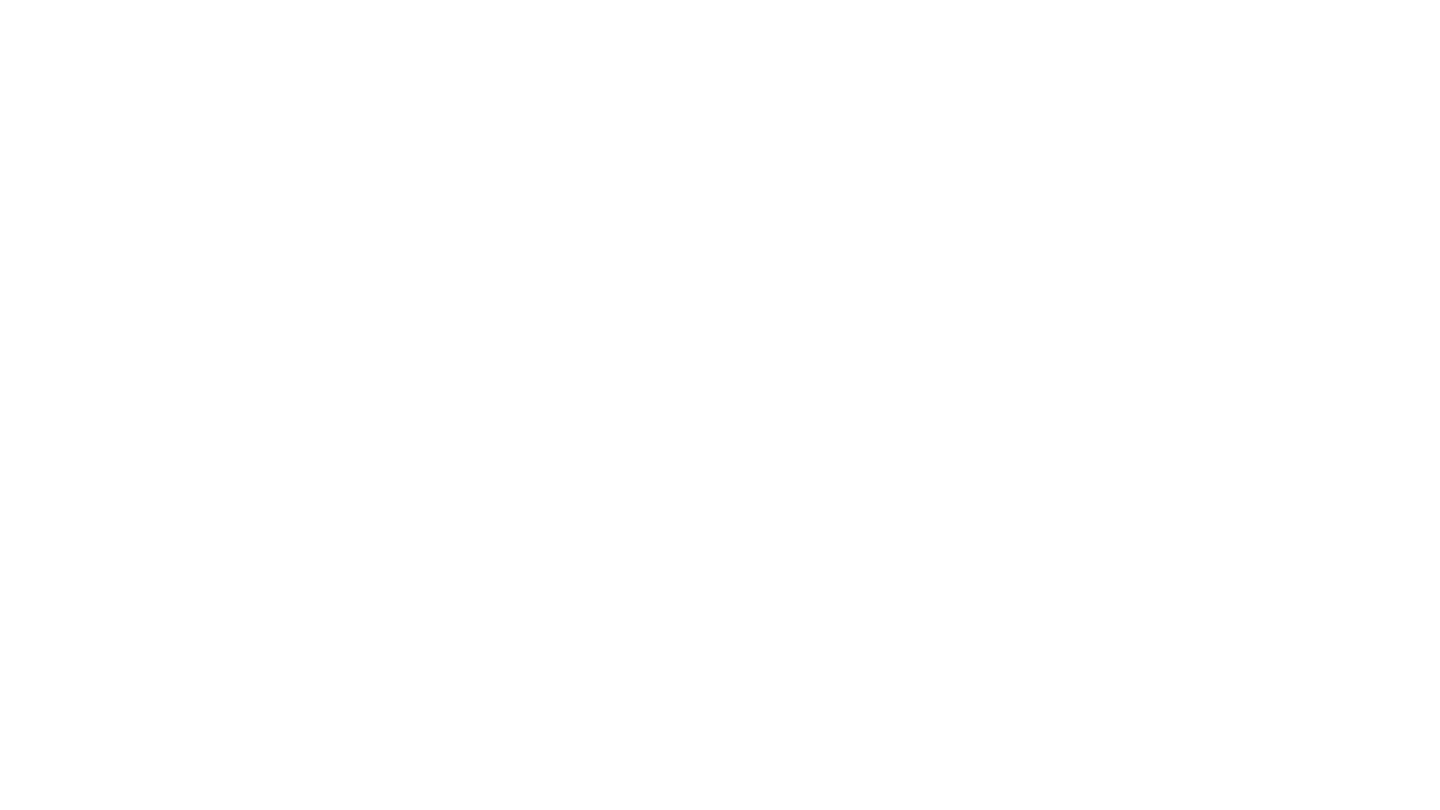
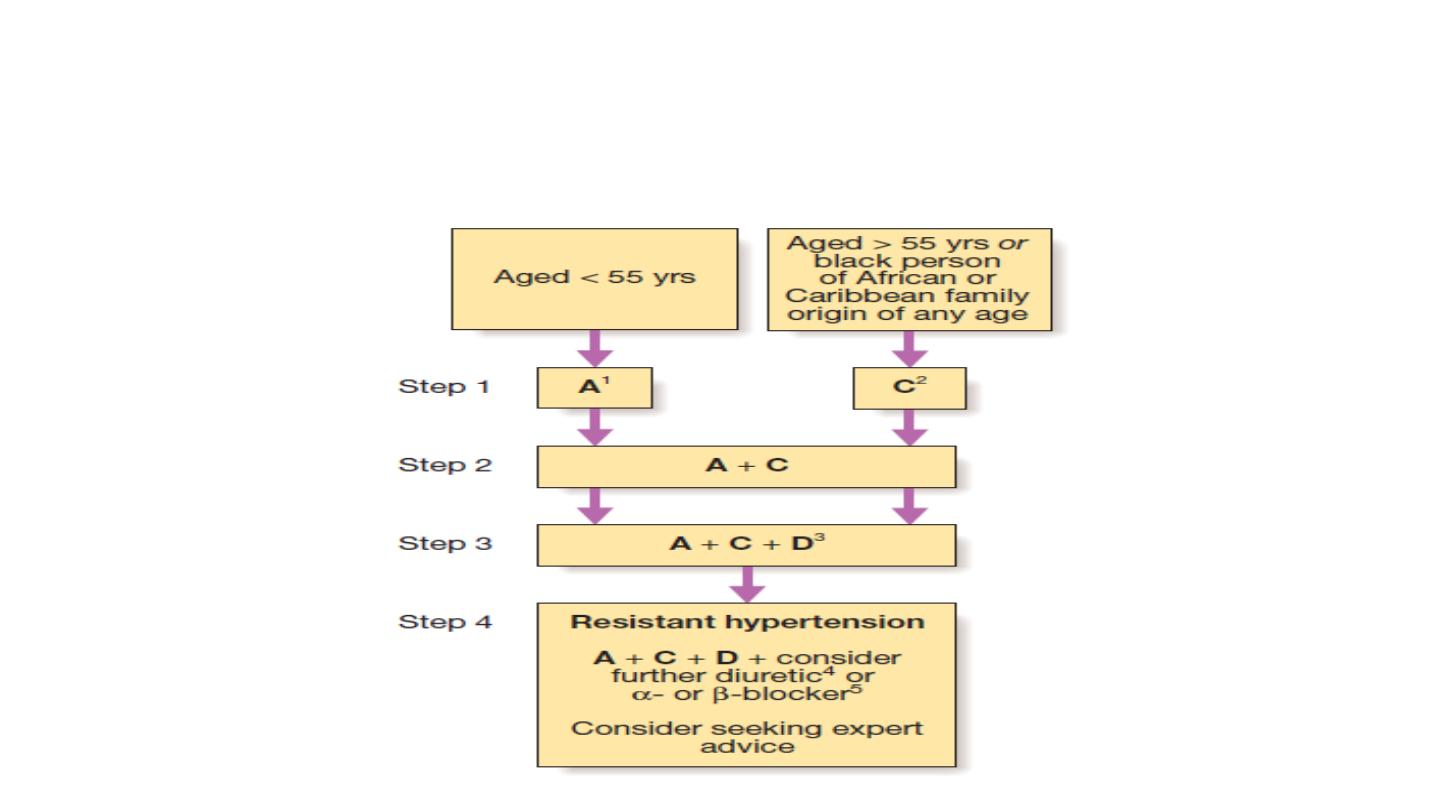
Choice of antihypertensive
:
Trials that have compared thiazides, calcium antagonists, ACE inhibitors
and angiotensin receptor blockers have not shown consistent differences
in outcome, efficacy, side-effects or quality of life. Beta-blockers, which
previously featured as first-line therapy in guidelines, have a weaker
evidence base.
The choice of antihypertensive therapy is initially dictated by the patient’s
age and ethnic background, although cost and convenience will affect the
exact drug and preparation used. Response to initial therapy and side-
effects dictate subsequent treatment. Comorbid conditions also have an
influence on initial drug selection for example, a β-blocker might be the
most appropriate treatment for a patient with angina. Thiazide diuretics
and dihydropyridine calcium channel antagonists are the most suitable
drugs for the treatment of high BP in older people
Choice of antihypertensives drugs according to
age

Combination versus monotherapy
Although some patients can be satisfactorily treated with a single
antihypertensive drug, a combination of drugs is often required to
achieve optimal BP control.
Combination therapy may be desirable for other reasons; for example,
low-dose therapy with two drugs may produce fewer unwanted effects
than treatment with the maximum dose of a single drug. Some drug
combinations have complementary or synergistic actions; for example,
thiazides increase activity of the renin–angiotensin system while ACE
inhibitors block it.

Emergency treatment of accelerated phase or malignant hypertension
In accelerated phase hypertension, lowering BP too quickly may compromise
tissue perfusion (due to altered autoregulation) and can cause cerebral
damage, including occipital blindness, and precipitate coronary or renal
insufficiency.
Even in the presence of cardiac failure or hypertensive encephalopathy, a
controlled reduction to a level of about 150/90 mmHg over a period of 24–48
hours is ideal.

In most patients, it is possible to avoid parenteral therapy and
bring BP under control with bed rest and oral drug therapy.
Intravenous or intramuscular labetalol (2 mg/min to a maximum
of 200 mg), intravenous glyceryl trinitrate (0.6–1.2 mg/hr),
intramuscular hydralazine (5 or 10 mg aliquots repeated at half
hourly intervals) and intravenous sodium nitroprusside (0.3–1.0
μg/kg body weight/min) are all effective but require careful
supervision, preferably in a high dependency unit.

Causes of refractory hypertension:
Poor compliance
Inadeqaute therapy
Secondory cause
Feature suggestive of secondary HPT:
AGE less than 30 , above 55 years, REFRACTORY HPT
