Small and Large Intestines (2)
lecture 9-10 . Pathology
GASTROINTESTINAL TRACT
1
Types of intestinal polyps
Non neoplastic polyps:
Occasionally seen, long standing IBD: UC > Crohn. And has no
malignant
potential and commonly seen.
Comprises 90% of all epithelial polyps and found in >1/2 of all persons
over the age of 60.
1- Hamartomatous polyp (rare).
a- Juvenile.
b- Peutz Jeghers polyp.
2- Inflammatory polyp.
3- Hyperplastic polyps.
4- Lymphoid polyps
neoplastic polyps:
Adenomatous polyps Preneoplastic polyps
-tubular adenoma (very common)
-tubulovillous adenoma (seen less than TA)
-villous adenoma (occasionally seen)
Benign non-neoplastic polyps
Hyperplastic polyps
-very common.
-proliferation of mature goblet cells; size <0.5 cm
-commonly found in adults > 60 years old
Gross:
-nipple like
-hemispheric
Small and Large Intestines (2)
lecture 9-10 . Pathology
GASTROINTESTINAL TRACT
2
-smooth moist
protrusions of the
mucosa
-often multiple
-> 1/2 in recto-sigmoid
Micro:
-well formed glands
-crypts lined by non-neoplastic cells
-goblet cell/absorptive cell differentiation
-serrated lumen
Juvenile Polyps
-Rare; focal hamartomatous polyps
-virtually no malignant potential (exception: Juvenile polyposis
syndrome)
-commonly found in children younger than age 5
usually solitary.
-most frequently in rectum.
--isolated IP may be found in adults: “retention polyp” which are
smaller < 1 cm. with stalks up to 2 cm.
-Lamina properia is the bulk of the polyp with cystically dilated glands,
surface ulceration
-Rare autosomal dominant JP syndrome
does carry a risk of adenoma and hence adenocarcinoma
Hamartomatous Polyp: Peutz Jeghers polyp
Rare
Large polyp with arborizing (tree-like) projections with smooth muscle
present at the mucosal surface
Small and Large Intestines (2)
lecture 9-10 . Pathology
GASTROINTESTINAL TRACT
3
Polyps with no malignant potential, but patients at risk for other
malignancies: pancreas, breast, lung, ovary, and uterus
Neoplasms of the small intestines
Perplexingly uncommon compared to tumors in other segments of GI
tract
3-6% of GI tumors
Malignant
-Adenocarcinoma
-Primary lymphoma
-Carcinoids
-GISTS
Benign
-Adenomas
-Leiomyomas
-Lipomas
-Angiomas
Adenoma Adenomatous polyps
-25% of SI benign tumors
-mostly in ampulla of vater
-familial polyposis coli
prone to amp of v adenoma
-30-60 yrs
Neoplasms of the large intestines Adenomas
All adenomas show dysplastic epithelium
All are precancerous
May proceed to intramucosal or invasive carcinoma
May occur anywhere, most occur in the left colon, specifically, recto-
sigmoid
Risk of malignant transformation is dependent on polyp size,
architecture, severity of dysplasia
Small and Large Intestines (2)
lecture 9-10 . Pathology
GASTROINTESTINAL TRACT
4
Tubular adenoma
Pedunculated, composed of branching round/ tubular glands on a stalk
Can grow up to 4 cm in diameter
The larger the polyp the greater the chance of harboring carcinoma.
90% in the colon; rarely in the stomach and SI
Solitary in 50%
2 or more in the remaining 50%
VILLOUS ADENOMA
VILLOUS ADENOMA
-Sessile, broad base rather than a stalk
-Composed of numerous , finger-like projections of epithelium
-Greater than 50% villous
-More than 40% harbor carcinoma
TUBULOVILLOUS ADENOMA
-features of both adenomas
-25-50% (30%) villous
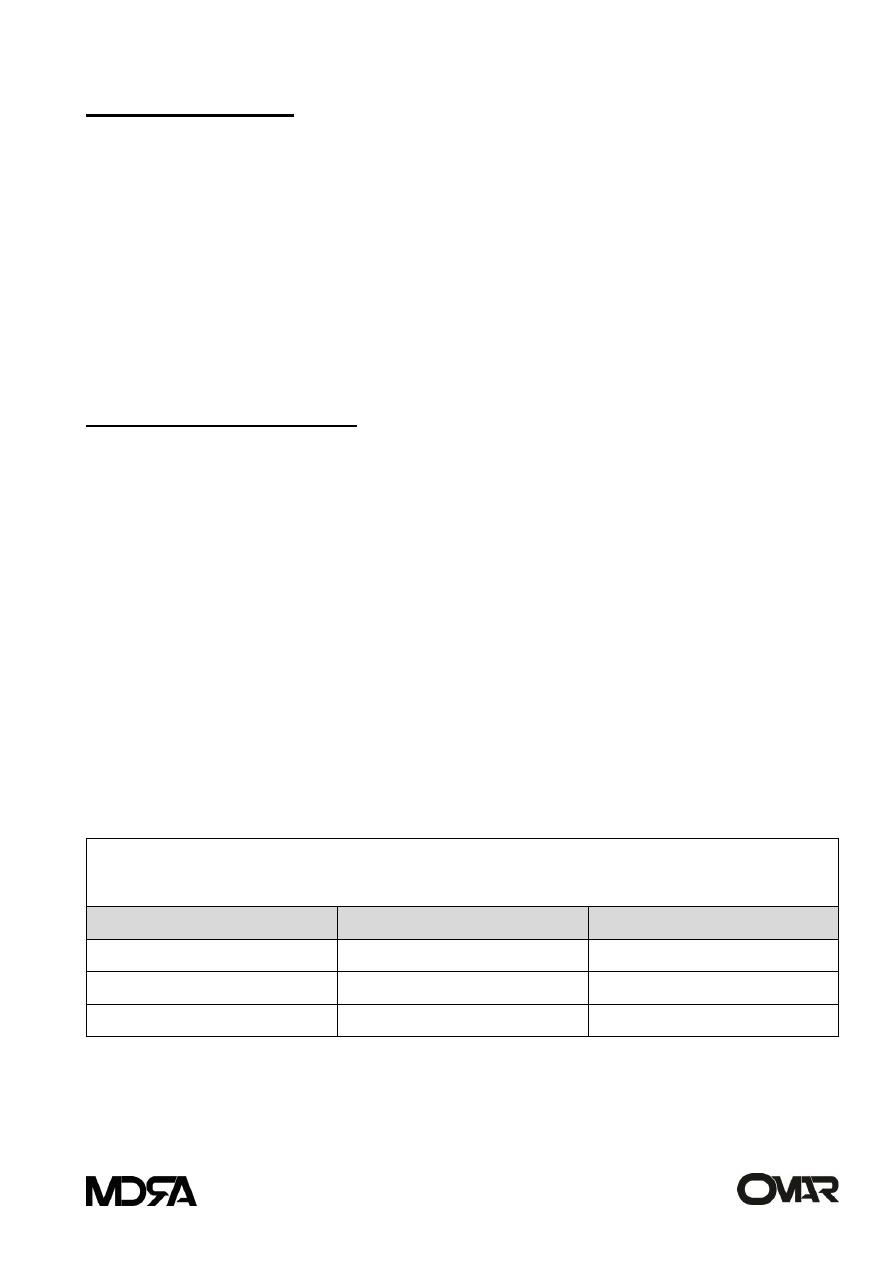
ADENOMAS OF THE COLON
Frequency of Invasive Tumor
Architecture
>1.0cm
<2.0cm
Tubular
0.3%
6.5%
Tubulovillous
1.5%
11.4%
Villous
2.5%
17.0%
-Cancer is rare in TA <1cm in size
-The risk of cancer is high (approximately 40%) in sessile villous lesions > 4cm
-Severe dysplasia when present is often seen in villous areas

Small and Large Intestines (2)
lecture 9-10 . Pathology
GASTROINTESTINAL TRACT
5
Familial syndromes
Familial syndromes
-Familial adenomatous polyposis
-Gardner syndrome
-Hereditary non polyposis colorectal cancer
Average onset of polyps in each of these adenomatous polyp syndromes is the
teens and twenties,
followed by cancer in 10-15 years unless surgical resections interrupt the
natural progression.
Familial adenomatous polyposis (FAP)
Rare, autosomal dominant; genetic defect is in the APC gene on Ch 5q21
Patients with 500-2500 polyps (min 100 polyps)
FAP - Cancer preventive measures by prophylactic colectomy as soon as
possible.
early detection of disease in siblings and
first degree relatives at risk
Gardner syndrome
a variant of FAP
also autosomal dominant
polyps similar to FAP but with multiple bone lesions and skin lesions
particularly mandible, skull, long bones, epidermal cysts and fibromatosis
Turcot syndrome: rare variant, GI polyps and CNS tumors, mostly gliomas.
Small and Large Intestines (2)
lecture 9-10 . Pathology
GASTROINTESTINAL TRACT
6
Malignant
-Adenocarcinoma
-Primary lymphoma
-Carcinoids
-Gastrointestinal stromal tumors (GISTS)
Adenocarcinoma: etiology:
Accounts for 10% of all cancer related deaths
peak incidence: 60-79 years (<20%: before 50)
worldwide: environment, diet, obesity, physical activity; no causal
relationship
FAP patients either inherit one defective copy of APC (one hit) or else
acquire it during embryogenesis. Deletion of the remaining good APC
gene in the colonic stem cell is all that is necessary to start down the
road to an adenoma.
Genetic Alterations: the path from normal to cancer
APC at Ch 5q21 (normal to hyperproliferative)
APC- B catenin -loss of DNA methyl (early adenoma)
Mutation of K- ras at Ch 12p12 (intermediate adenoma)
loss of DCC gene on Ch 18 (late adenoma)
Loss of p53 at Ch 17p13 (invasive cancer)
Adenocarcinoma: Morphology
-tumor will infiltrate wall of colon and metastasize to lymph nodes and liver
-prognosis is related to size and spread of the lesion
STAGING: Dukes (A,B,C) staging and Astler Coller System - pathologic
staging of colorectal cancer:
A – mucosa A: 5YSR - 100%
B - submucosa or muscularis properia B1; serosa B2B1: 67% B2: 54%
Small and Large Intestines (2)
lecture 9-10 . Pathology
GASTROINTESTINAL TRACT
7
C - B1 + lymph node met C1; B2 + lymph node met C2C1: 43%; C2: 23%
D - Distant mets to lung and liver
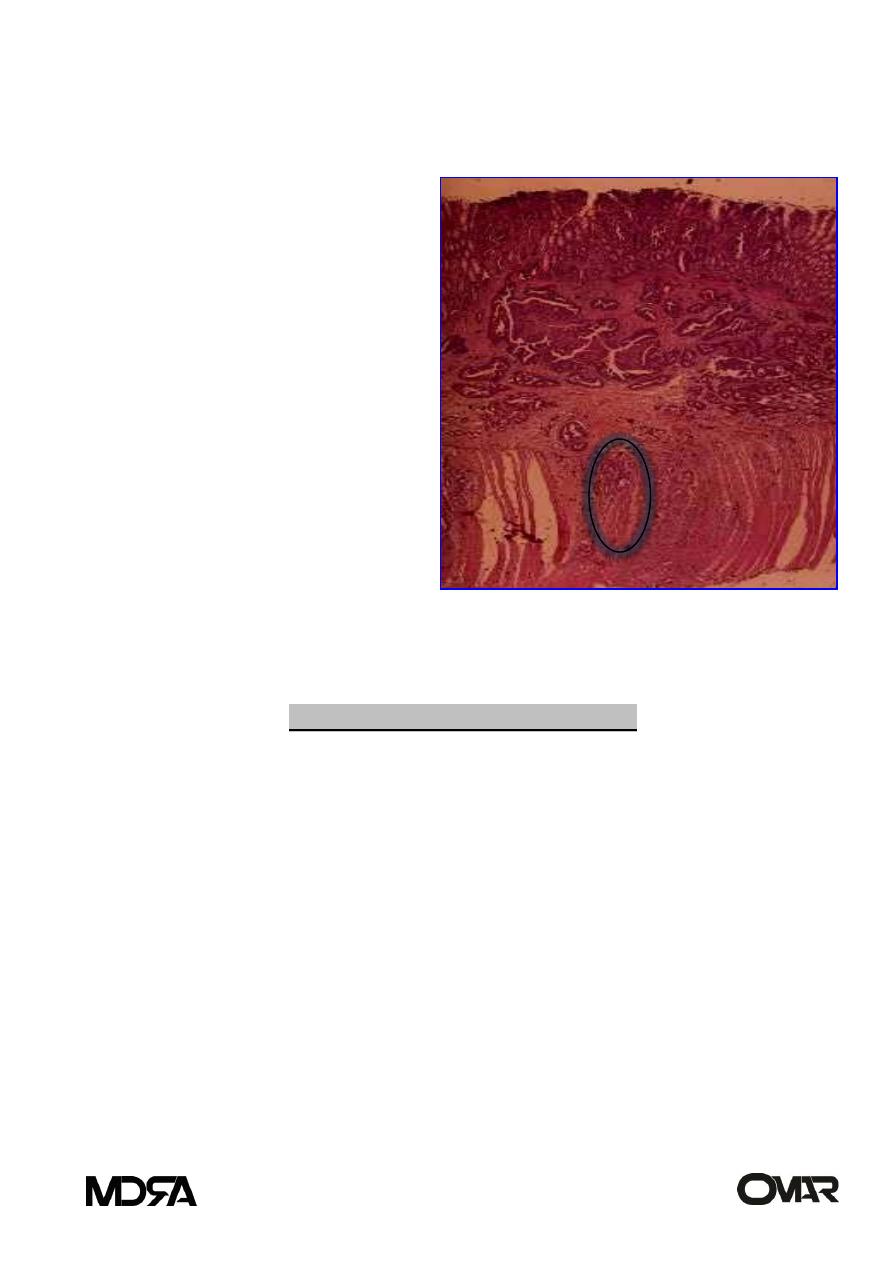
Invasive adenocarcinoma
The tumor has invaded
through the mucosa, into
submucosa (in this case it is
seen to the level of the
muscularis propria)
The submucosa contains
large lymphatics which are
conduits for metastases
Most worrisome lesions are
villous adenoma > 4 cm.
When invasive carcinoma
occurs, there is no stalk as a buffer zone
and invasion is directly into the wall of the colon (submucosa or deeper).
Adenocarcinoma: Clinical features
Left colon adenocarcinoma
-generally annular
-narrow the lumen
-change in bowel habits or
obstruction
-blood
in
stool
(maybe
obvious/bright red or occult)
-originating from ruptured vessels at
the edge of the ulceration
Right colon adenocarcinoma
-usually -asymptomatic for a long
period of time
-signs and symptoms of iron
deficiency anemia due to surface
ulceration and resulting blood loss
Polypoid, fungating
non-obstructing
right colon ca

Small and Large Intestines (2)
lecture 9-10 . Pathology
GASTROINTESTINAL TRACT
8
1- MALT lymphoma (sporadic)
-GI primary extranodal site
-1-4% of all GI malignancies
30-40 yrs
Location in:
Stomach: 50-60%
SI: 25-30%
Distal colon: up to 10%
Primary lymphoma
Arises from lymphoid aggregates in the wall with no evidence of other
primary sites
Gastric lymphomas are most common and have better prognosis than SI
or LI if early
refractory (celiac) sprue associated with TCL; mostly in jejunum
Etiology:
Due to random changes brought about by t(11;18)
H. pylori reactive T helper cells produces cytokine
that allows growth of monoclonal B cell population
Therefore Tx: H. pylori
sporadic but occur more
frequently on certain populations:
1. pxs with H. pylori
2. natives of Mediterranean region
3. pxs with immunodeficiency states
4. HIV infected individuals
Small and Large Intestines (2)
lecture 9-10 . Pathology
GASTROINTESTINAL TRACT
9
5. pxs in immunosuppressive therapy
6. patients with refractory sprue
2- sprue associated lymphoma
Rare T cell tumors (Refractory sprue)
Long standing malabsorption syndrome, of gluten enteropathy, and occur
in young ages, 30-40 years, following 10-20 years MS.
Of T cell origin.
3- Mediterranean lymphoma:
B cell lymphoma, in children and young adults, type of heavy chain disease
(alpha), with plasma cell infiltration of the wall and of poor prognosis.
4- Burkitt’s lymphoma:
non African type in children and young adults, affects the
retroperitoneum and ovaries also. Characterized by monotonous cells
with round nuclei and multiple nucleoli, and interspersed macrophages
giving a starry sky appearance.
Carcinoids
arise from NE cells
common in SI (50% of SI malignancies; 2% of colorectal malignancies)
5 YSR: 90%
5 YSR with liver mets: 50%
if widespread – death
*Most common sites in the order of frequency:
Appendix-Ileum (SI)-Rectum-Stomach-Colon

Small and Large Intestines (2)
lecture 9-10 . Pathology
GASTROINTESTINAL TRACT
11
*Appendiceal and rectal carcinoids almost never metastasize.
*90% of ileal, gastric and colon carcinoids have already met to L.Ns at
time of diagnosis
Carcinoid syndrome
may secrete bioactive amines (serotonin: diarrhea, flushing of face,
broncho -spasm, cyanosis -carcinoid syndrome) Also diarrhea,
hepatomegaly, cardiac fibrosis, and diffuse fibrosis.
Carcinoid syndrome occurs in about 1% of all patients with carcinoid
tumors and 20% of those with widespread metastasis.
Excess elaboration of serotonin 5HT and 5 HIAA; present in blood and
urine. 5-HIAA is deactivated in the liver. Therefore in GI carcinoids, liver
metastases have to be present for the development of the syndrome. Not
true for ovary and lung carcinoids. Other products: Histamine, bradykinin
and prostaglandins
Morphology:
Form polypoid masses, solid tan in colour and firm. Microscopically
show islands and trabeculae of cells that are monotonous with granular
cytoplasm, and of uniform shape in low grade types of benign behavior
while it is in aggressive types of small cells or spindle cells.
Positive for chromogranin A, neuron specific enolase and synaptophysin.
Electron microscopy:
Neuro - Secretory granules
Gastrointestinal stromal tumor (GIST)
uncommon
arise in wall of bowel.
portrude into lumen; ulcerate; GI bleed

Small and Large Intestines (2)
lecture 9-10 . Pathology
GASTROINTESTINAL TRACT
11
mostly slow growing; cured by surgery
30% recurrence/liver mets within 10 years
may progress to high grade sarcoma
all are potentially malignant and may be low risk or high risk
high risk if > 5 cm in size and if mitosis >10/10 hpf
Neoplasms of appendix
Mucocele: benign dilatation of the lumen by mucinous secretions.
Mucinous cyst adenoma- proliferation of benign neoplastic cells-
dilatation by mucinous material -may rupture
Mucinous cyst -adenocarcinoma -invasion of neoplastic cells
Pseudomyxoma peritonei
term describing distention of the peritoneal cavity by the presence of semisolid,
mucin containing adenocarcinoma cells
Peritoneum
Inflammation
1. Sterile peritonitis due to bile or pancreatic juices
2. Surgical procedures
3. Endometriosis
4. Rupture of GI tract (Ruptured appendicitis, acute salpingitis, or diverticulitis)
Neoplasms
1. Primary mesothelioma -rare
2. Secondary malignancies -extension, seeding, or implantation (more
common).
