
Diphtheria
Dr. Ameer kadhim Hussein.
M.B.Ch.B. FICMS (Community Medicine).

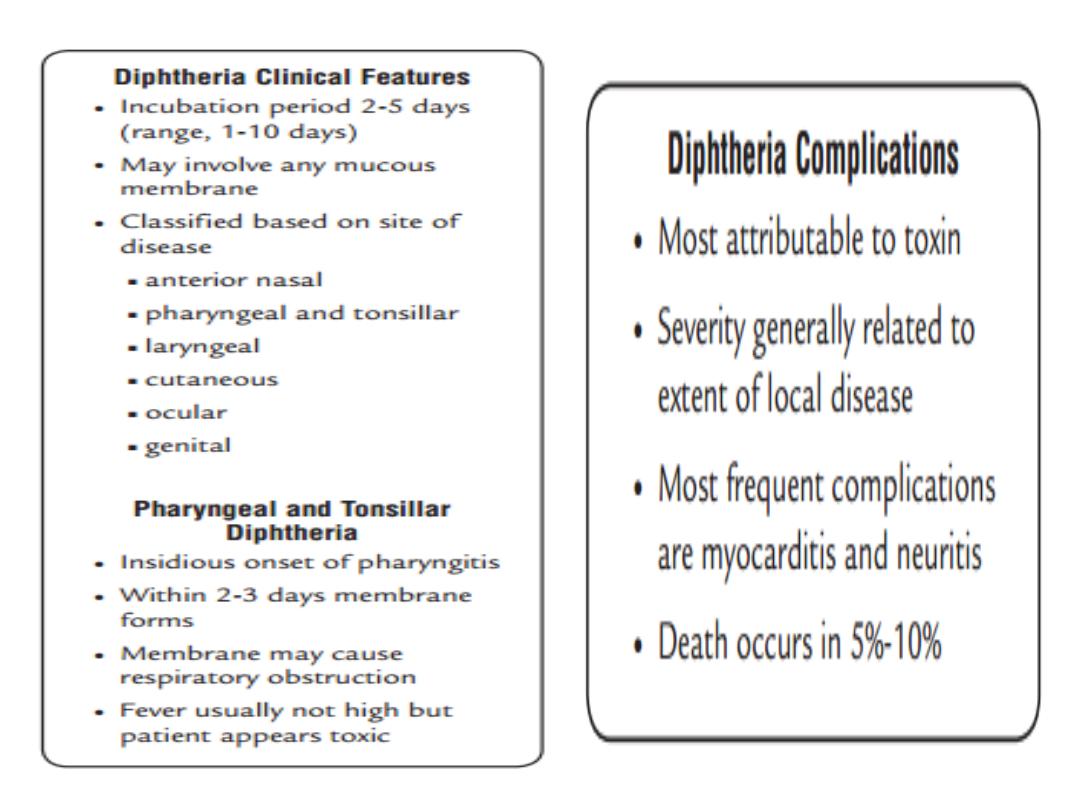
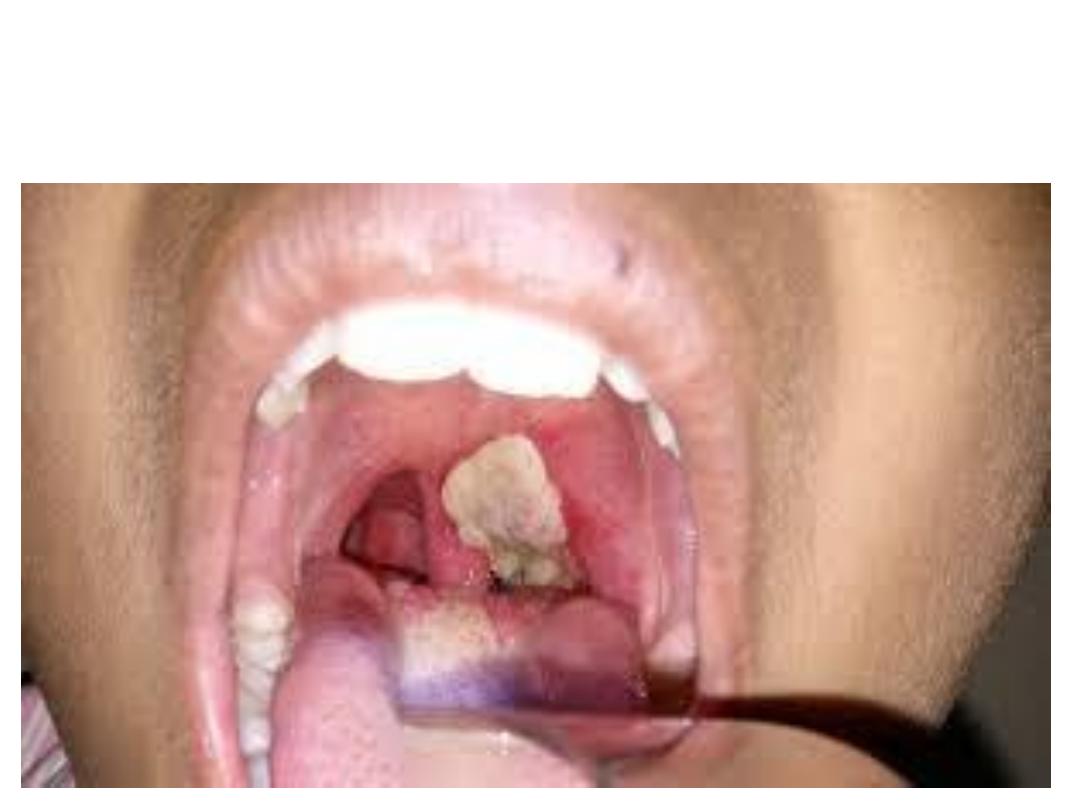
Identification
Diphtheria is an acute bacterial disease primarily involving
tonsils, pharynx, larynx, nose, skin and sometimes
conjunctivae or vagina.
It is infectious disease caused by toxigenic strain of
Corynebacterium diphtheriae, the bacilli multiply locally
usually in the throat and elaborate a powerful exotoxin
which is responsible for:
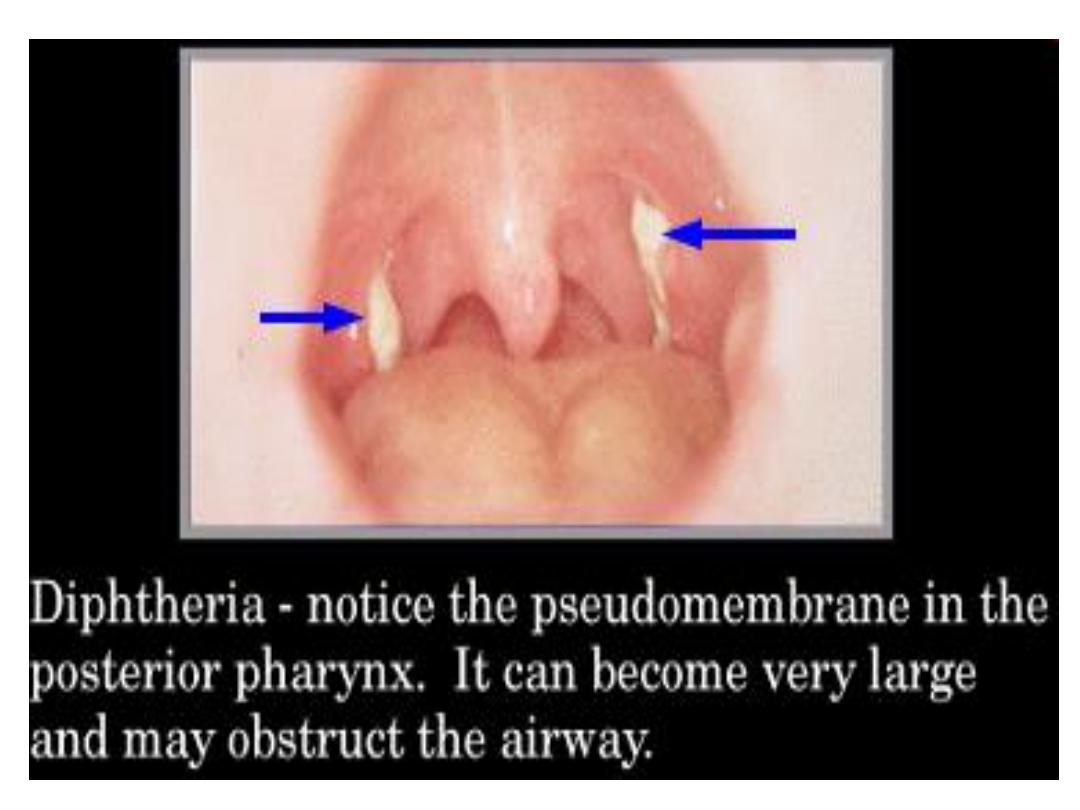
1. Formation of grayish or yellowish membrane (false
membrane) commonly over tonsils , pharynx or larynx.
2. Congestion, oedema and local tissue destruction.
3. Enlargement of regional lymph nodes and signs and
symptoms of toxemia.
Identification
Three major clinical types of diphtheria have been described:
1. anterior nasal diphtheria.
2. faucial ( tonsillo-pharyngeal) diphtheria.
3. laryngeal diphtheria.
other types include cutaneous, conjuctival, otitic and genital
diphtheria.
In apparent infection (colonization) outnumber the clinical cases.
Case fatality rate of respiratory diphtheria is 5-10 % even with
treatment with higher death rates (up to 20%) among persons younger
than 5 and older than 40 years of age.
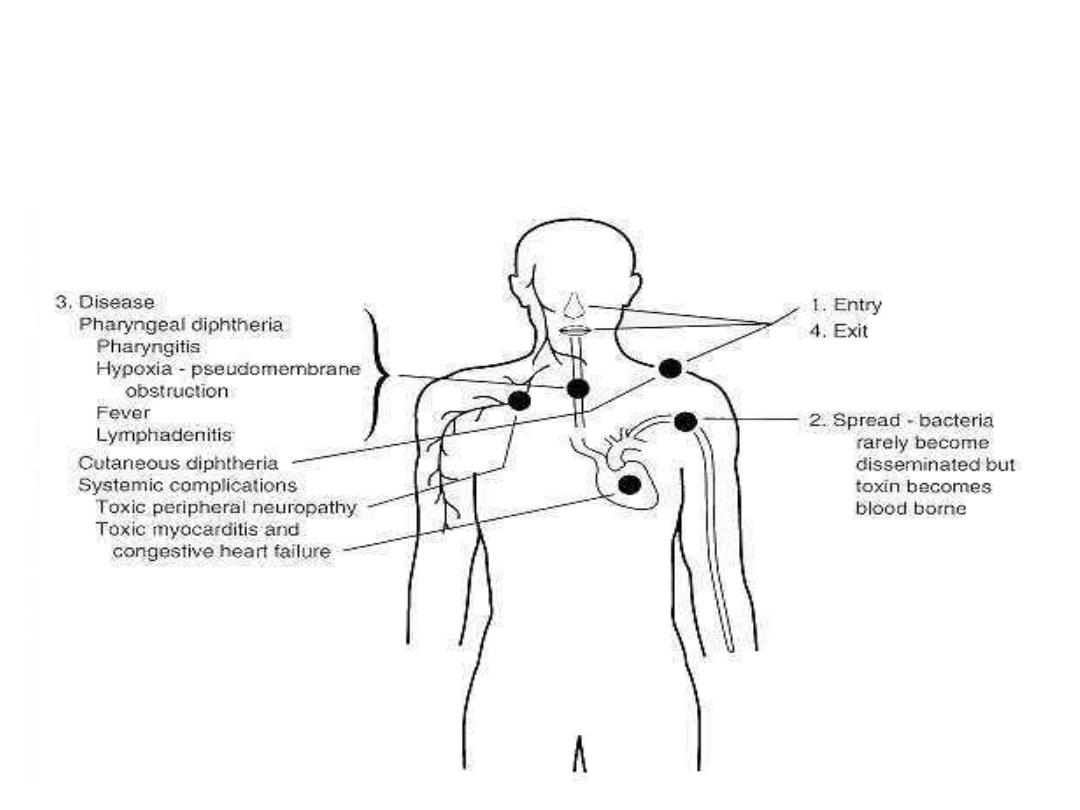
Pathogenesis of diphtheria

Cutaneous diphtheria

Infectious agent
•
toxin-producing strains of Corynebacterium diphtheriae
which of four types (gravis, mitis and intermedius and
belfanti). All types are pathogenic to man. C. diphtheriae
is gram positive non motile aerobic bacillus. It has no
invasive power but produce powerful exotoxin.

Occurrence
•
It is disease of colder months in temperate zones primarily involving
non immunized children under 15 years. In tropics the seasonal trends
are less district and in apparent, cutaneous and wound diphtheria are
more common.
•
According to the World Health Organization (WHO), diphtheria
epidemics remain a health threat in developing nations. The largest
epidemic recorded since widespread implementation of vaccine
programs was in 1990-1995, when a diphtheria epidemic emerged in
the Russian Federation, rapidly spreading to involve all Newly
Independent States (NIS) and Baltic States.

OCCURRENCE
•
This epidemic caused more than 157,000 cases and 5000
deaths according to WHO reports, high rates of death
were observed in individuals older than 40 years. This
epidemic accounted for 80% of cases reported worldwide
during this time period.
•
From 1993-2003, long epidemic in Latvia resulted in
1359 reported cases of diphtheria with 101 deaths. The
incidence fell from 3.9 cases per 100,000 in 2001 to 1.12
cases per 100,000 population in 2003. Most cases were
registered in unvaccinated adults.

OCCURRENCE
•
Overall rates of infection have decreased in Europe from
2000 to 2009, according to the Diphtheria Surveillance
Network.
•
This has been attributed to improved vaccination rates
creating herd immunity. However, issues with
vaccinations still occur, especially in eastern European
countries and Russia, and are thought to contribute to the
ongoing outbreaks.
•
Many case reports in the literature describe epidemics in
sub-Saharan Africa, France, India, and the United States.
Diphtheria
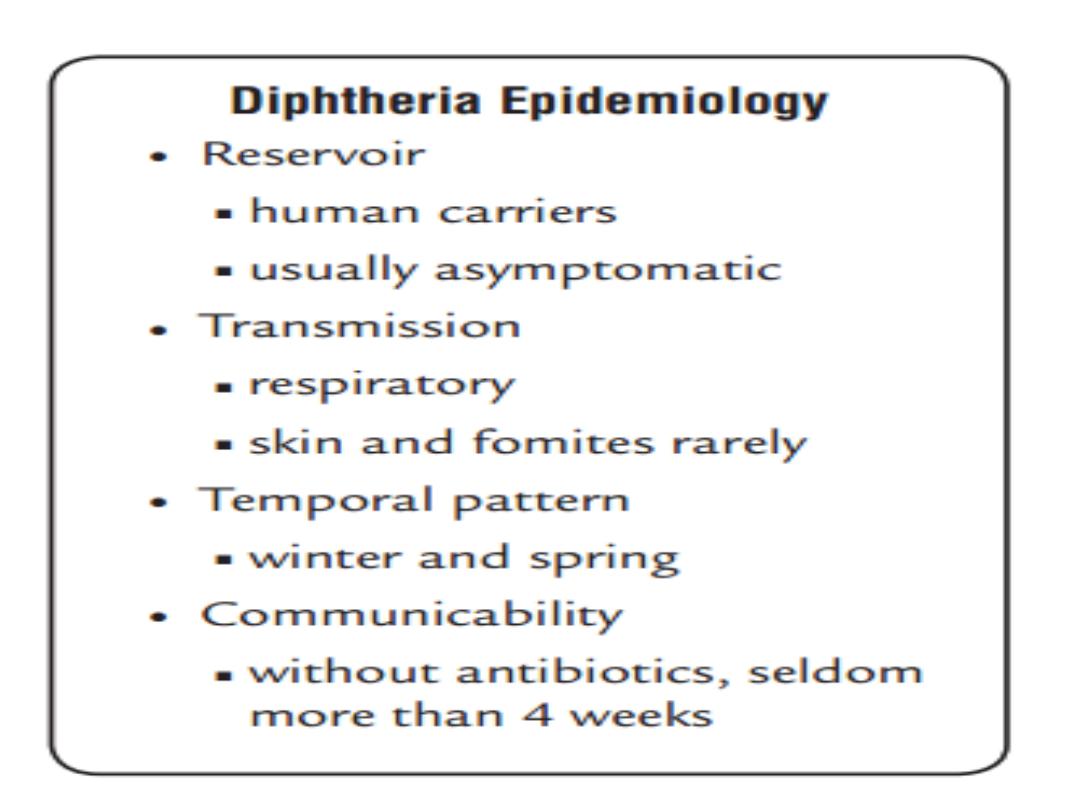
•
Reservoir: Humans.
•
Mode of transmission: Contact with cases or carriers and less
commonly contact with articles soiled with discharge from lesion
of infected people. Raw milk has served as a vehicle.
•
Incubation period: Usually 2 to 5 days and rarely may persist
for longer time.
•
Period of communicability:
•
It extend from 14 to 28 days from the onset of disease but
carrier may persist longer. Case or carrier considered non
infective when at least 2 cultures obtained from nose and throat
24 hours apart are negative for diphtheria bacilli. Effective
treatment promptly terminates the shedding of bacilli.

Susceptibility
Infants born to immune mothers have passive protection
which is usually lost before the 6
th
month of age.
Apparent or in apparent disease usually induce long lasting or
life long immunity.
Immunization with toxoid usually produce prolonged but not
lifelong immunity.
The immunity provide by vaccination with diphtheria toxoid
is of anti toxic type which protect against systemic disease
but not against colonization in the nasopharynx.
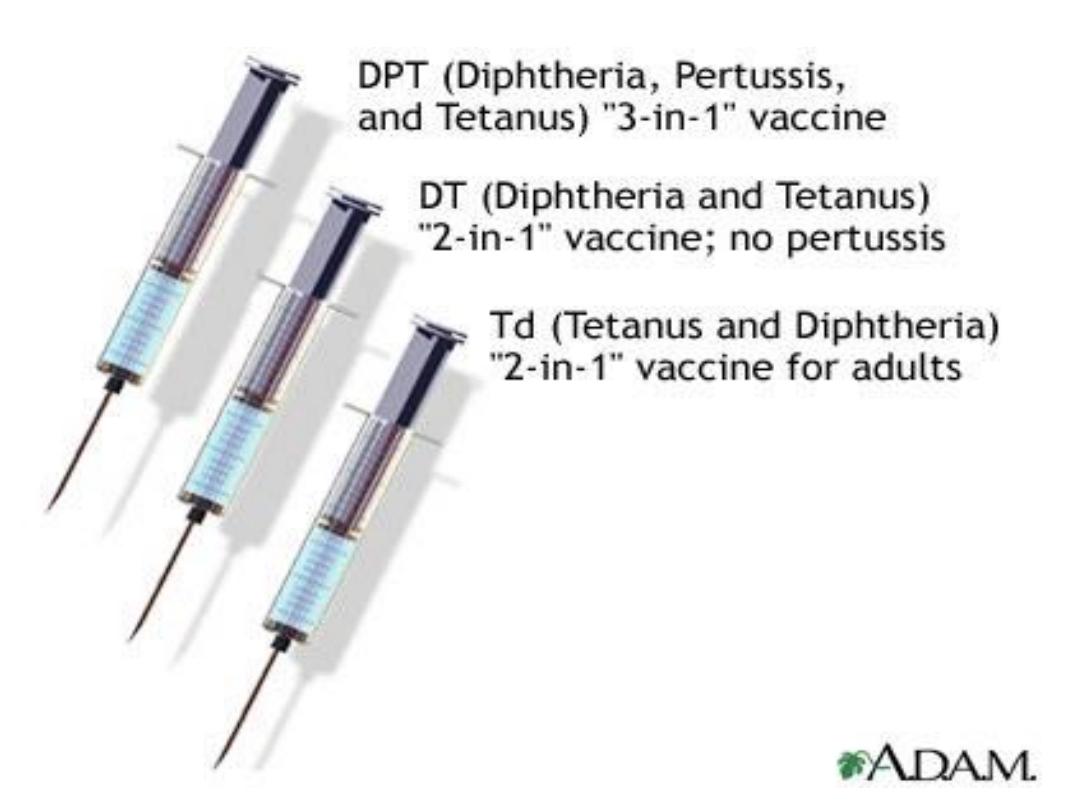
Methods of control
. Preventive measures:
A
1. Educational measures are important by informing the
parents of young children about hazards of diphtheria and
the importance of active immunization.
2. Active immunization with diphtheria toxoid which should
be initiated in infancy with a formulation containing
diphtheria toxoid, tetanus toxoid and either a cellular
pertussis or whole cell pertussis vaccine
(DTaP or DTP).
Formulation containing diphtheria toxoid , tetanus toxoid,
whole cell pertussis and Haemophilus influenzae type b
vaccine are also available.

Methods of control
The schedule of vaccination in Iraq was include 3
primary doses of diphtheria vaccine which given at 2
nd
, 4
th
and 6
th
month of life and 1
st
booster dose at 18
th
month
and 2
nd
booster dose at 4 to 6 years.
3. For children under 7 years if the pertussis component of
DTP is contraindicated we give diphtheria and tetanus
toxoid (DT).
4. For persons 7 years and older because of adverse effect
of diphtheria toxoid increase with age we give preparation
containing reduced concentration of diphtheria toxoid
(adult Td).
5. Active protection should be maintained by
administering a booster dose of Td every 10 years.

Methods of control
6. Special effort should be made to ensure that those at high
risk of exposure such as health workers should be fully
immunized and receive a booster dose of Td every 10 years.
7. Immune compromised patient should receive the same
schedule and dose of diphtheria immunization as immune
competent person.
Methods of control
B. Control of patient , contacts and immediate environment:
1. Report to local health authority.
2. Isolation: strict isolation for pharyngeal diphtheria and contact
isolation for cutaneous diphtheria until 2 culture 24 hours apart and
not less than 24 hours after cessation of antibiotics appear to be
negative for C. diphtheriae. When culture is impractical isolation
should be end after 14 days of starting of antibiotics.
3. Concurrent disinfection: for all articles in contact with the patients
or soiled with their discharge.
4. Quarantine: Adult contacts working in food handling or present in
contact with un immunized children should excluded from work until
treated and bacteriological examination proved them not to be
carriers.
Methods of control
5. Management of contacts:
All close contacts should have cultures taken from nose and
throat and kept under surveillance for 7 days.
Single dose of benzathine penicillin (IM) or 7-10 days course
of erythromycin is recommended for all persons with
household exposure to diphtheria regardless their
Immunization status. Those contact who don’t receive
prophylaxis should be monitored for 7 days and treated as
diphtheria if symptoms develop. Those contacts previously
immunized should receive booster dose of diphtheria toxoid
when more than 5 years past since the last dose while non
immunized contacts should take full course of immunization.
Adult contacts working in food handling or present in contact
with un immunized children should excluded from work until
treated and bacteriological examination proved them not to be
carriers.
Methods of control
6. Investigation of contacts and source of infection: Searching
for carriers by use of nose and throat cultures other than among
close contacts is neither useful nor indicated.
7. Specific treatment:
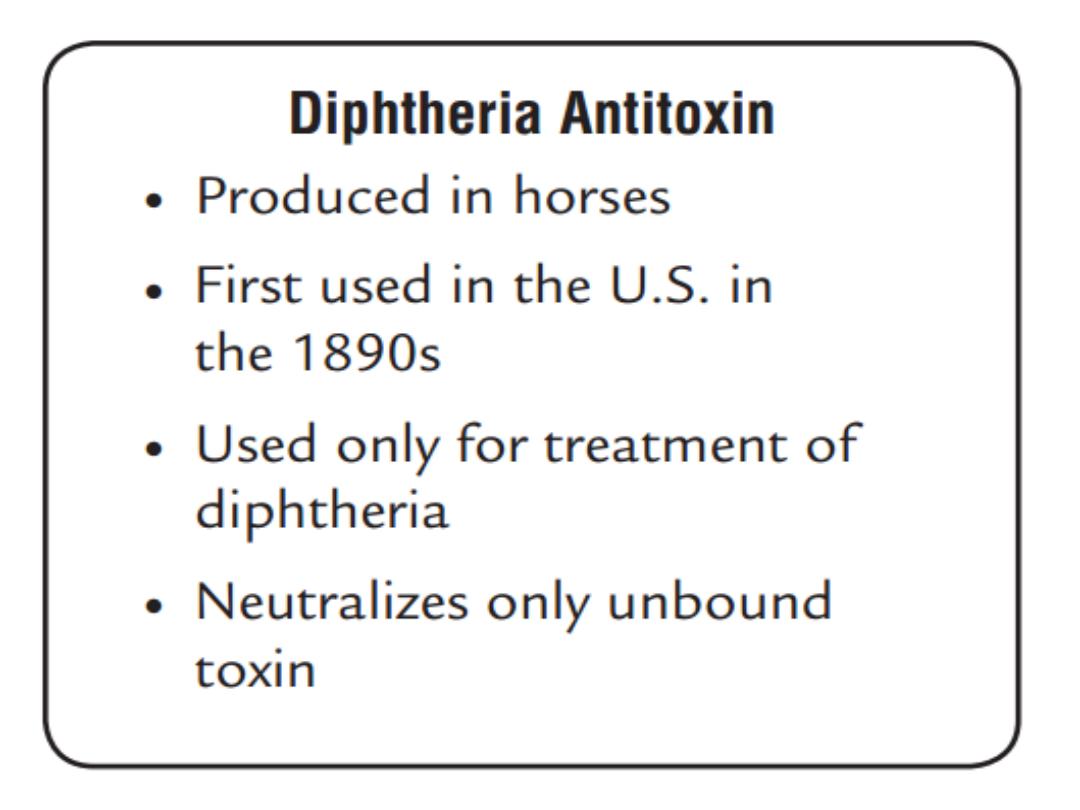
•a. Diphtheria antitoxin: It is specific treatment for diphtheria
but
•before giving antitoxin sensitivity test (skin or eye testing)
•must be done because antitoxin of equine origin is available.
After completion the test and hypersensitivity rule out single
dose of antitoxin should be given IM immediately after
bacteriological specimen are taken without waiting results.
Methods of control
b. Antibiotics: which not substitute for antitoxin but
will eliminate the bacteria, halt toxin production and
reduce communicability.
Procaine penicillin G (IM) or
parenteral erythromycin is recommended until the patient
can swallow comfortably. Oral penicillin V or
erythromycin orally can be used as substitution for total
treatment period of 14 days.
8. Treatment of carriers: by single dose of benzathine
penicillin G or 7-10 days course of erythromycin orally is
recomended.

Epidemic measures
1. Immunized the largest possible proportion of the population
group involved especially infants and preschool children. In
epidemic involving adult, immunize those who most affected or
those at high risk.
Repeat immunization 1 month later to provide at least 2 doses to
recipients.
2. Identify close contacts and those at high risk, carry out
field investigation of reported cases to confirm the diagnosis
and to determine the biotype and the toxigenicity of bacteria.
Disaster implication and international measures
Disaster implications:
When outbreaks occur in area of overcrowding
of susceptible groups especially infants and
children.
International measures:
People traveling to or through countries where
respiratory or cutaneous diphtheria is common
should receive primary immunization or booster
dose of Td for those previously immunized.
Thank you
