Heart failure

Heart failure describes the clinical syndrome that develops when the heart
cannot maintain adequate output, or can do so only at the expense of
elevated ventricular filling pressure.
In mild to moderate forms of heart failure, symptoms occur only when
the metabolic demand increases during exercise or some other form of
stress. In severe heart failure, symptoms may be present at rest.
In clinical practice, heart failure may be diagnosed when a patient with
significant heart disease develops the signs or symptoms of a low cardiac
output, pulmonary congestion or systemic venous congestion at rest or on
exercise

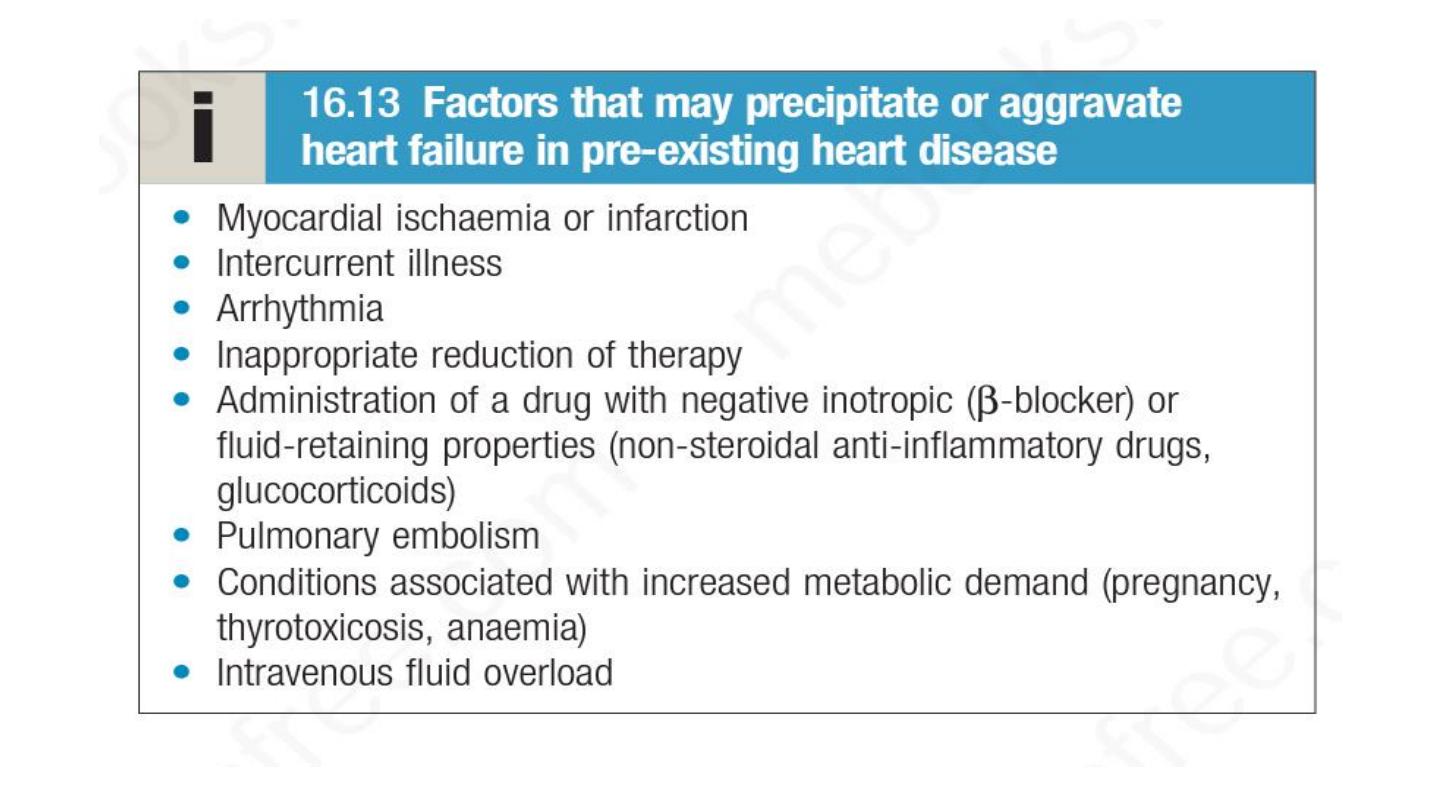
Left heart failure
:
This is characterised by a reduction in left ventricular output and an
increase in left atrial and pulmonary venous pressure.
If left heart failure occurs suddenly – for example, as the result of an
acute MI – the rapid increase in left atrial pressure causes pulmonary
oedema.
If the rise in atrial pressure is more gradual, as occurs with mitral
stenosis, there is reflex pulmonary vasoconstriction, which protects the
patient from pulmonary oedema.
However, the resulting increase in pulmonary vascular resistance causes
pulmonary hypertension, which in turn impairs right ventricular function.

Right heart failure
This is characterised by a reduction in right ventricular output and an
increase in right atrial and systemic venous pressure.
The most common causes are chronic lung disease, pulmonary embolism
and pulmonary valvular stenosis.
The term ‘cor pulmonale’ is used to describe right heart failure that is
secondary to chronic lung disease.

Biventricular heart failure
In biventricular failure, both sides of the heart are affected. This
may occur because the disease process, such as dilated
cardiomyopathy or ischaemic heart disease, affects both ventricles
or because disease of the left heart leads to chronic elevation of
the left atrial pressure, pulmonary hypertension and right heart
failure.

Prognosis
Although the outlook depends, to some extent, on the
underlying cause of the problem, untreated heart failure generally
carries a poor prognosis; approximately
50%
of patients with
severe heart failure due to left ventricular dysfunction will die
within
2 years
because of either pump
failure or malignant
ventricular arrhythmias.
The most common causes are coronary artery disease and
myocardial infarction but almost all forms of heart disease can
lead to heart failure

Pathogenesis
:
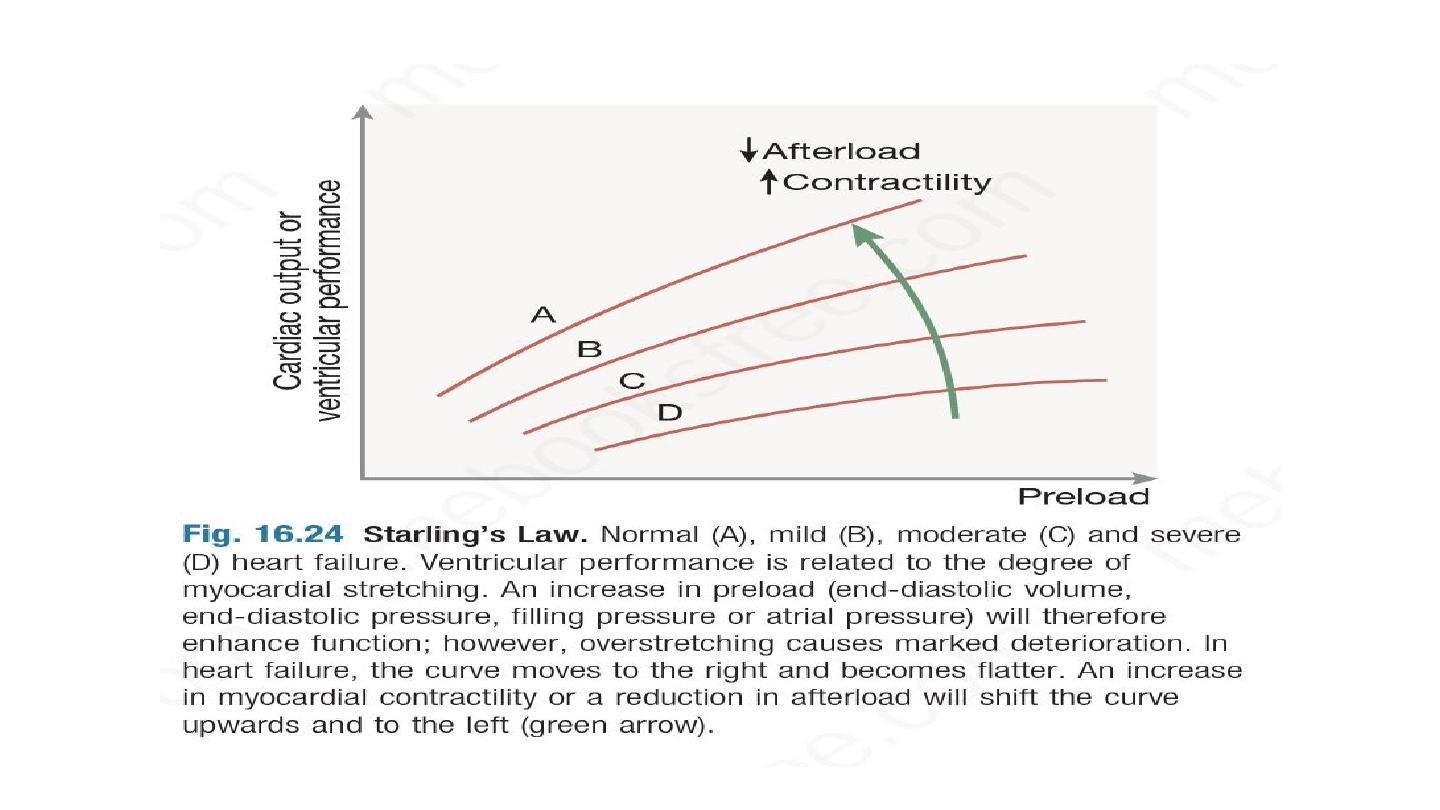
Heart failure occurs when cardiac output fails to meet the
demands of the circulation. Cardiac output is determined by
preload
(the volume and pressure of blood in the ventricles at the
end of diastole),
afterload
(the volume and pressure of blood in
the ventricles during systole) and
myocardial contractility
, forming
the basis of Starling’s Law.
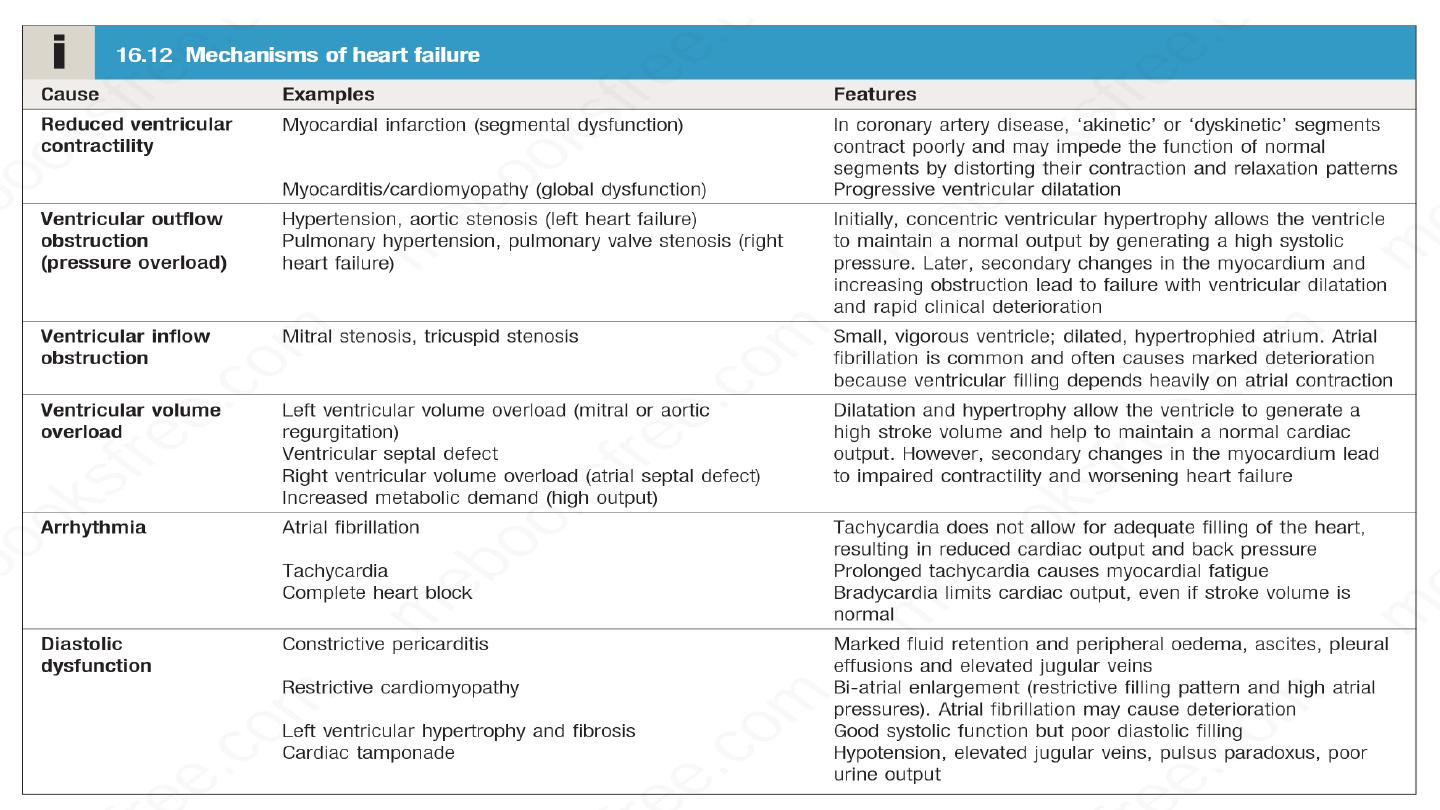

Ventricular dysfunction
Ventricular dysfunction is the most common cause of heart failure. This
can occur because of impaired systolic contraction due to myocardial
disease, or diastolic dysfunction where there is abnormal ventricular
relaxation due to a stiff, non-compliant ventricle. This is most commonly
found in patients with left ventricular hypertrophy. Systolic dysfunction
and diastolic dysfunction often coexist, particularly in patients with
coronary artery disease.
Ventricular dysfunction reduces cardiac output, which, in turn, activates
the sympathetic nervous system (SNS) and renin angiotensin aldosterone
system (RAAS). Under normal circumstances, activation of the SNS and
RAAS supports cardiac function but, in the setting of impaired
ventricular function, the consequences are negative and lead to an
increase in both afterload and preload.
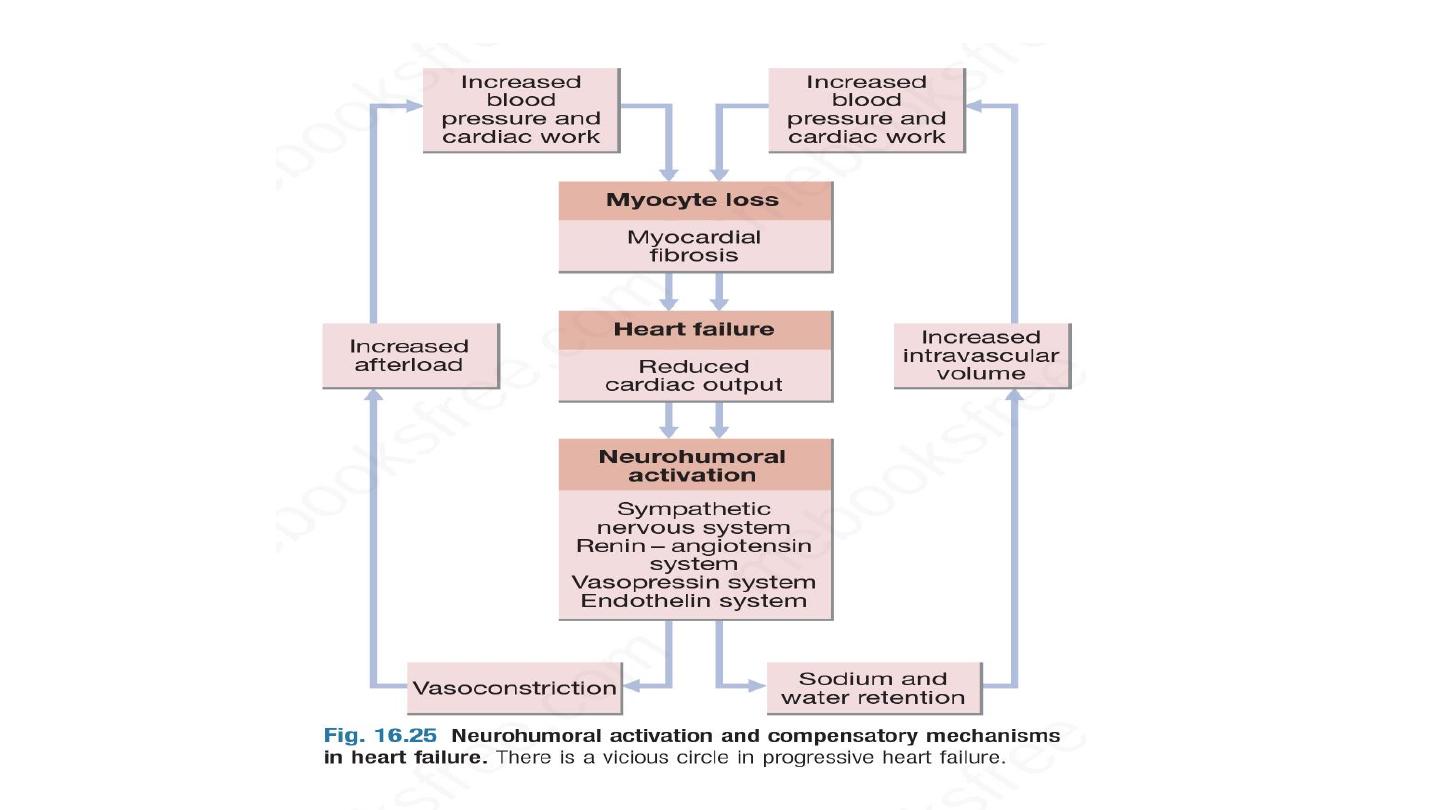
Activation of the RAAS causes vasoconstriction and sodium and water
retention. This is primarily mediated by angiotensin II, a potent constrictor of
arterioles, in both the kidney and the systemic circulation.
Activation of the SNS also occurs and can initially sustain cardiac output
through increased myocardial contractility and heart rate. Prolonged
sympathetic stimulation has negative effects, however, causing cardiac myocyte
apoptosis, cardiac hypertrophy and focal myocardial necrosis.
Sympathetic stimulation also contributes to vasoconstriction and predisposes
to arrhythmias. Sodium and water retention is further enhanced by the release
of aldosterone,
endothelin-1
(a potent vasoconstrictor peptide with marked
effects on the renal vasculature) and in severe heart failure,
vasopressin
(antidiuretic hormone, ADH).

Natriuretic peptides are released from the atria in response to atrial dilatation
and compensate to an extent for the sodium-conserving effect of aldosterone,
but this mechanism is overwhelmed in heart failure.
Pulmonary and peripheral oedema occurs because of high left and right atrial
pressures, and is compounded by sodium and water retention, caused by
impairment of renal perfusion and by secondary hyperaldosteronism.
If the underlying cause is a myocardial infarction, cardiac contractility is
impaired and SNS and RAAS activation causes hypertrophy of non-infarcted
segments, with thinning, dilatation and expansion of the infarcted segment.
This leads to further deterioration in ventricular function and worsening heart
failure.

High-output failure
Sometimes cardiac failure can occur in patients without heart
disease due to a large arteriovenous shunt, or where there is an
excessively high cardiac output due to beri-beri, severe anaemia or
thyrotoxicosis.

Classification of heart failure
Left , right, congestive HF
Acute versus chronic HF
Systolic versus diastolic HF
Forward versus backward HF
Cardiac cachexia
Stages of heart failure

Complications
Several complications may occur in advanced heart failure
Renal failure is caused by poor renal perfusion due to low cardiac output and
may be exacerbated by diuretic therapy, ACE inhibitors and angiotensin receptor
blockers (ARBs).
Hypokalaemia may be the result of treatment with potassium-losing diuretics or
hyperaldosteronism caused by activation of the renin–angiotensin system and
impaired aldosterone metabolism due to hepatic congestion. Most of the body’s
potassium is intracellular and there may be substantial depletion of potassium
stores, even when the plasma concentration is in the reference range.
Hyperkalaemia may be due to the effects of drugs that promote renal resorption
of potassium, in particular the combination of ACE inhibitors, ARBs and
mineralocorticoid receptor antagonists. These effects are amplified if there is renal
dysfunction due to low cardiac output or atherosclerotic renal vascular disease.
Hyponatraemia is a feature of severe heart failure and is a poor
prognostic sign. It may be caused by diuretic therapy, inappropriate
water retention due to high vasopressin secretion, or failure of the
cell membrane ion pump.
Impaired liver function is caused by hepatic venous congestion and
poor arterial perfusion, which frequently cause mild jaundice and
abnormal liver function tests; reduced synthesis of clotting factors can
make anticoagulant control difficult.
Thromboembolism. Deep vein thrombosis and pulmonary embolism
may occur due to the effects of a low cardiac output and enforced
immobility. Systemic emboli occur in patients with atrial fibrillation or
flutter, or with intracardiac thrombus complicating conditions such as
mitral stenosis, MI or left ventricular aneurysm.

Atrial and ventricular arrhythmias are very common and may be
related to electrolyte changes such as hypokalaemia and
hypomagnesaemia, the underlying cardiac disease, and the pro-
arrhythmic effects of sympathetic activation. Atrial fibrillation occurs in
approximately 20% of patients with heart failure and causes further
impairment of cardiac function. Ventricular ectopic beats and runs of
non-sustained ventricular tachycardia are common findings in patients
with heart failure and are associated with an adverse prognosis.
Sudden death occurs in up to 50% of patients with heart failure and
is most probably due to ventricular fibrillation.

Investigation
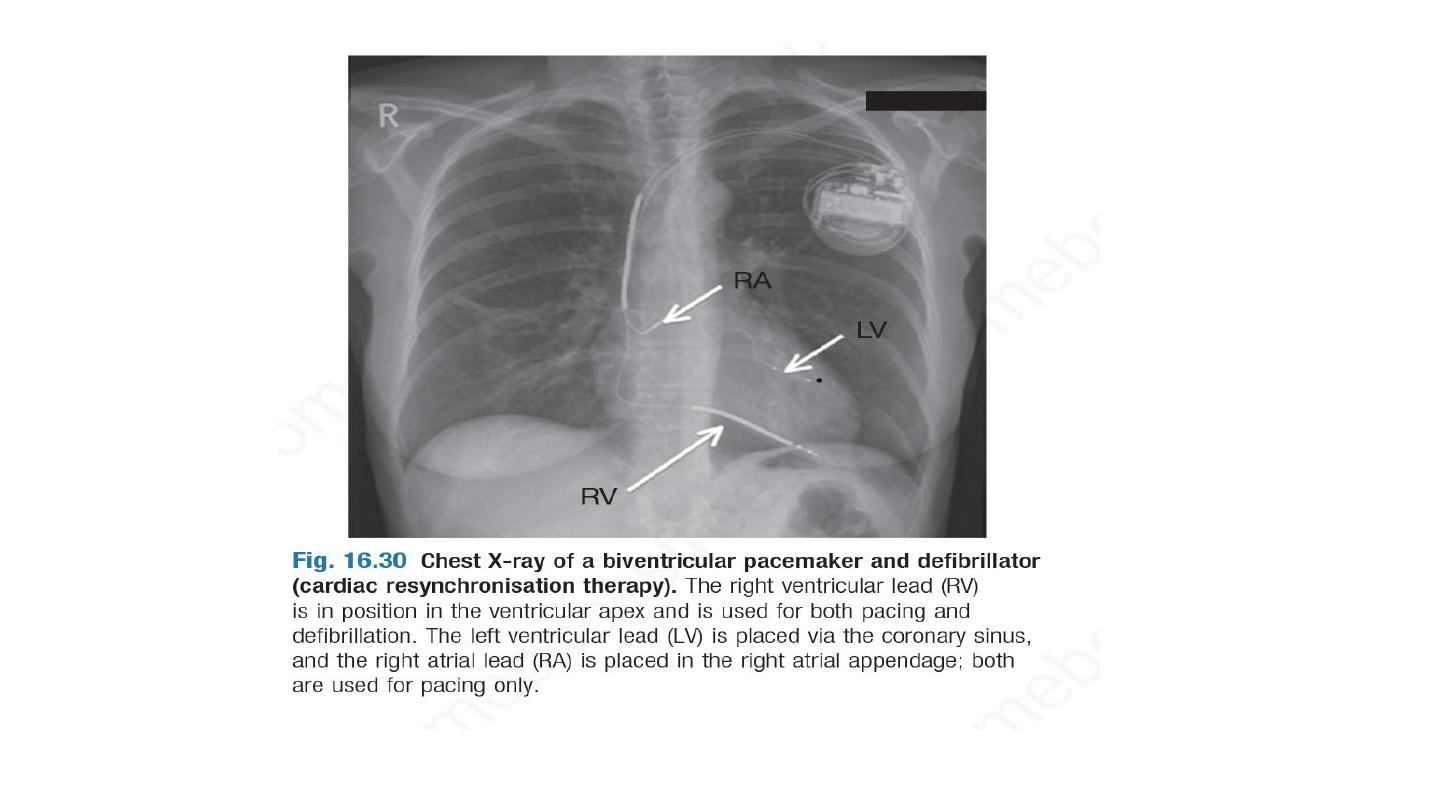
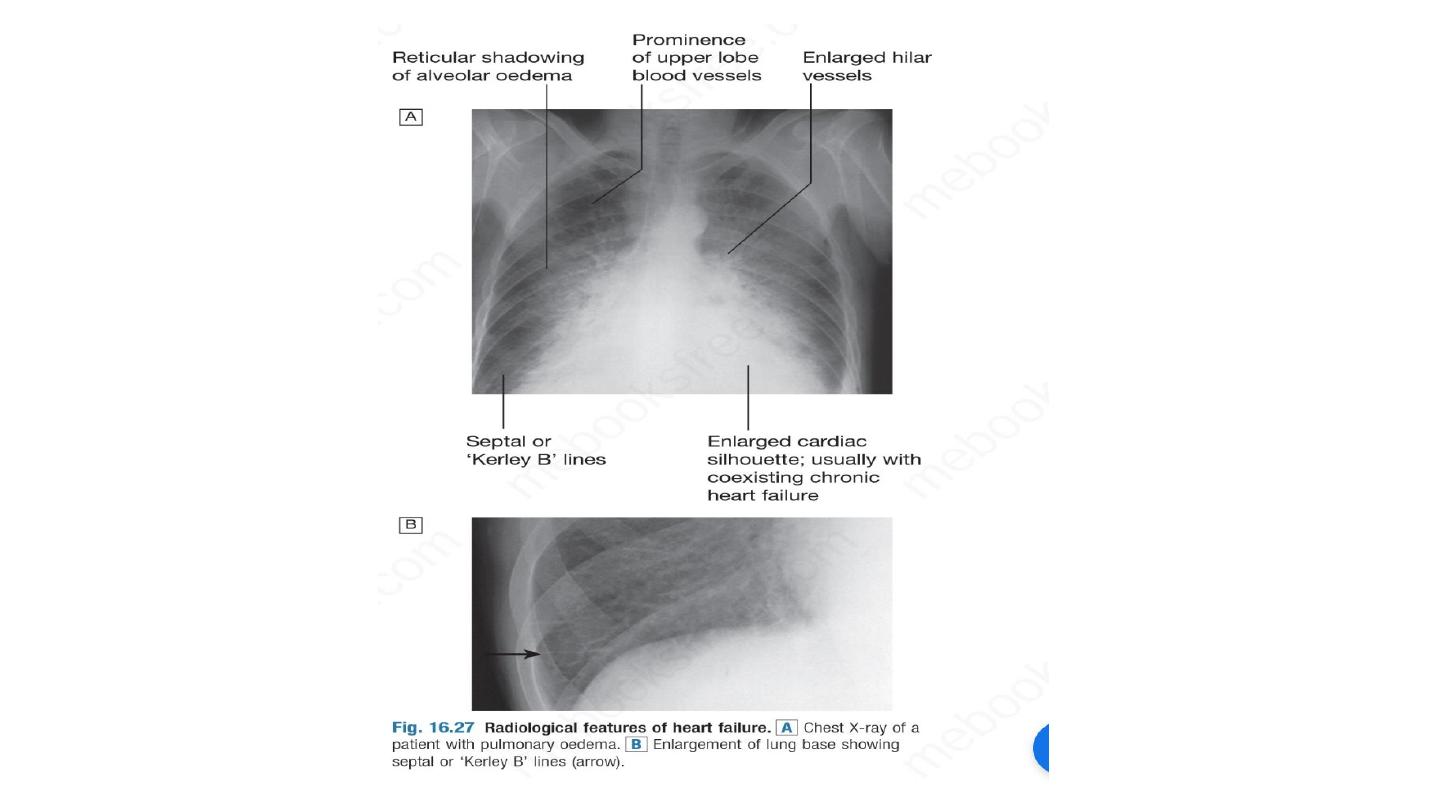
CXR
A chest X-ray should be performed in all cases. This may show
abnormal distension of the upper lobe pulmonary veins with the
patient in the erect position. Vascularity of the lung fields becomes
more prominent and the right and left pulmonary arteries dilate.
Subsequently, interstitial oedema causes thickened interlobular
septa and dilated lymphatics. These are evident as septal or kerely B
line.
More advanced changes due to alveolar oedema cause a hazy
opacification spreading from the hilar regions, and pleural effusions

Echocardiography
Echocardiography is very useful and should be considered in all
patients with heart failure in order to:
determine the aetiology
detect hitherto unsuspected valvular heart disease, such as occult
mitral stenosis, and other conditions that may be amenable to
specific remedies
identify patients who will benefit from long-term drug therapy.

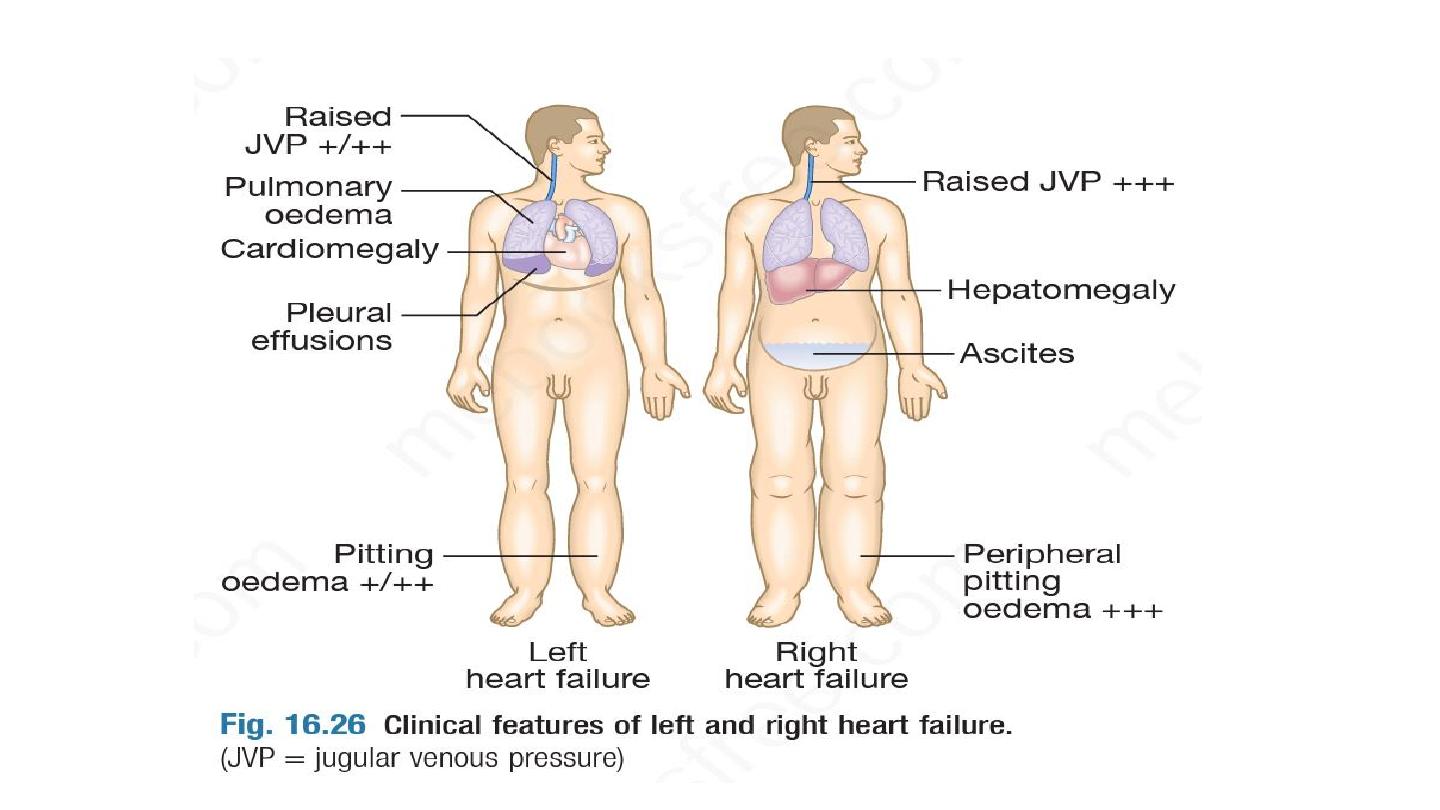
Serum urea, creatinine and electrolytes, haemoglobin and thyroid
function may help to establish the nature and severity of the
underlying heart disease and detect any complications. BNP is
elevated in heart failure and is a prognostic marker, as well as
being useful in differentiating heart failure from other causes of
breathlessness or peripheral oedema.

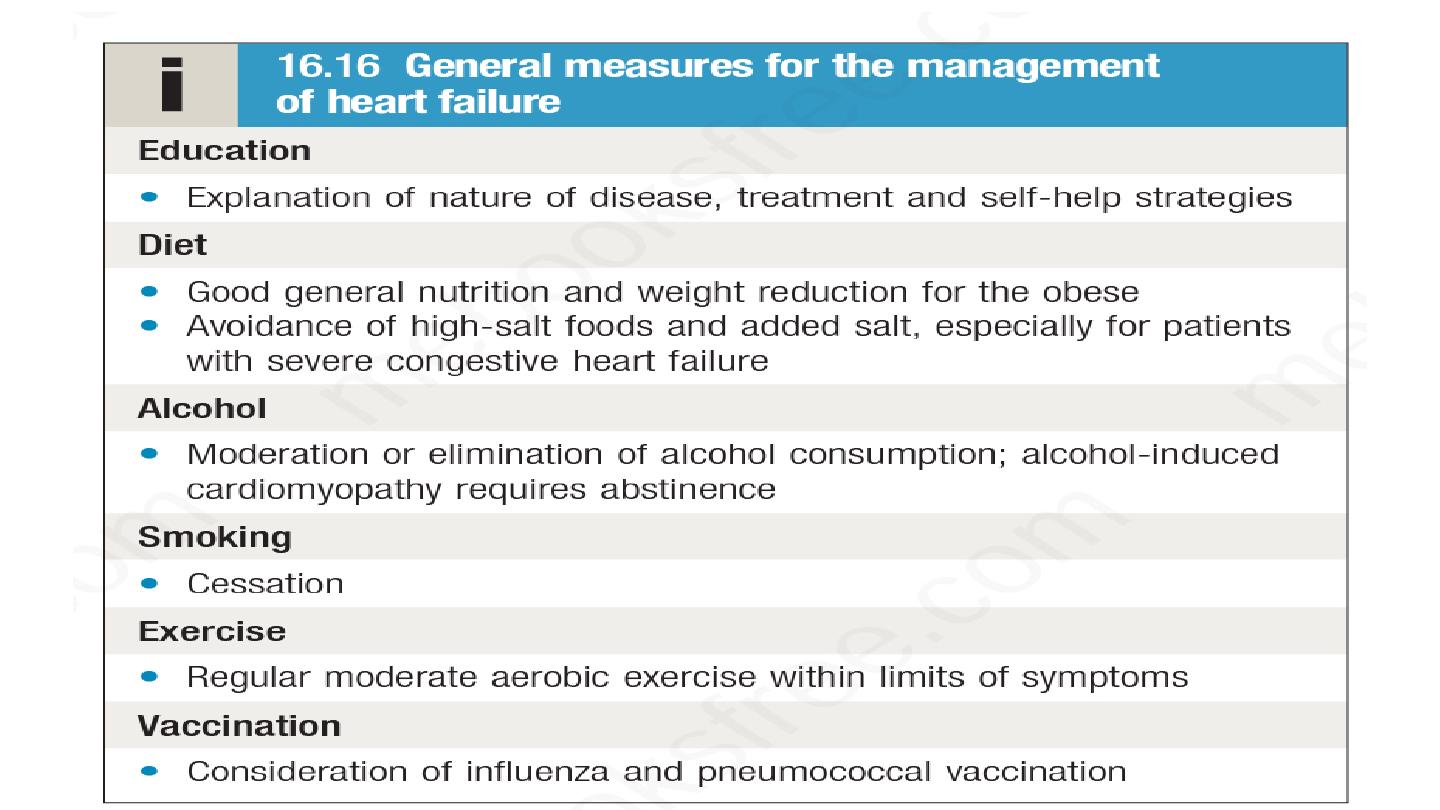
Management of HF
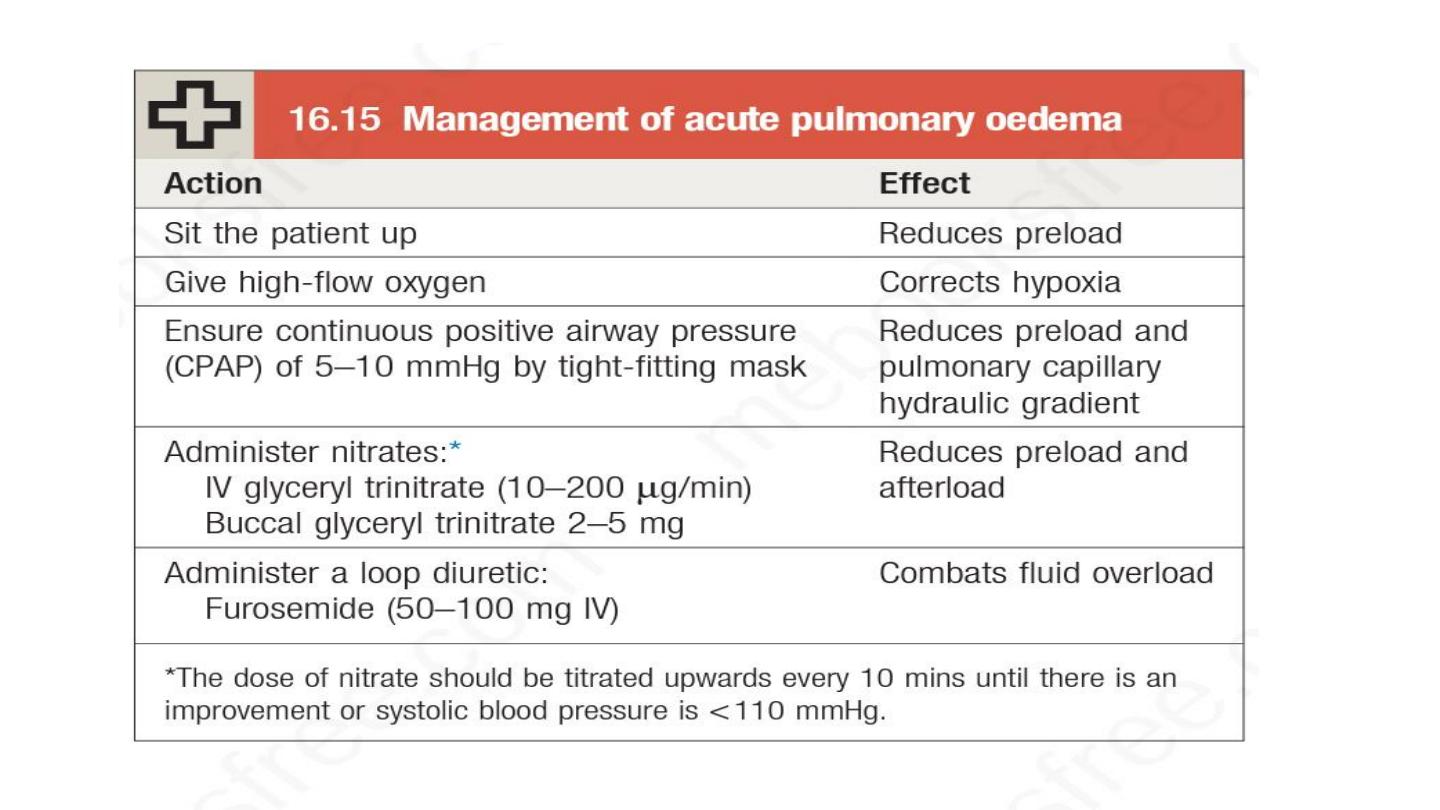
Management of acute heart failure

If these meaures prove ineffective then
Dobutamine
IABC

Management of chronic heart failure
Aim

Drug treatment
A wide variety of drug treatments are now available for the treatment
of heart failure
.
Drugs that reduce preload
are appropriate in patients
with high end-diastolic filling pressures and evidence of pulmonary or
systemic venous congestion, whereas
those that reduce afterload
or
increase myocardial contractility are more useful in patients with signs
and symptoms of a low cardiac output

• Diuretics
Loop diuretics
Thiazide
Mineralocorticoid receptors antagonist

• ACE inhibitors
• ARBs
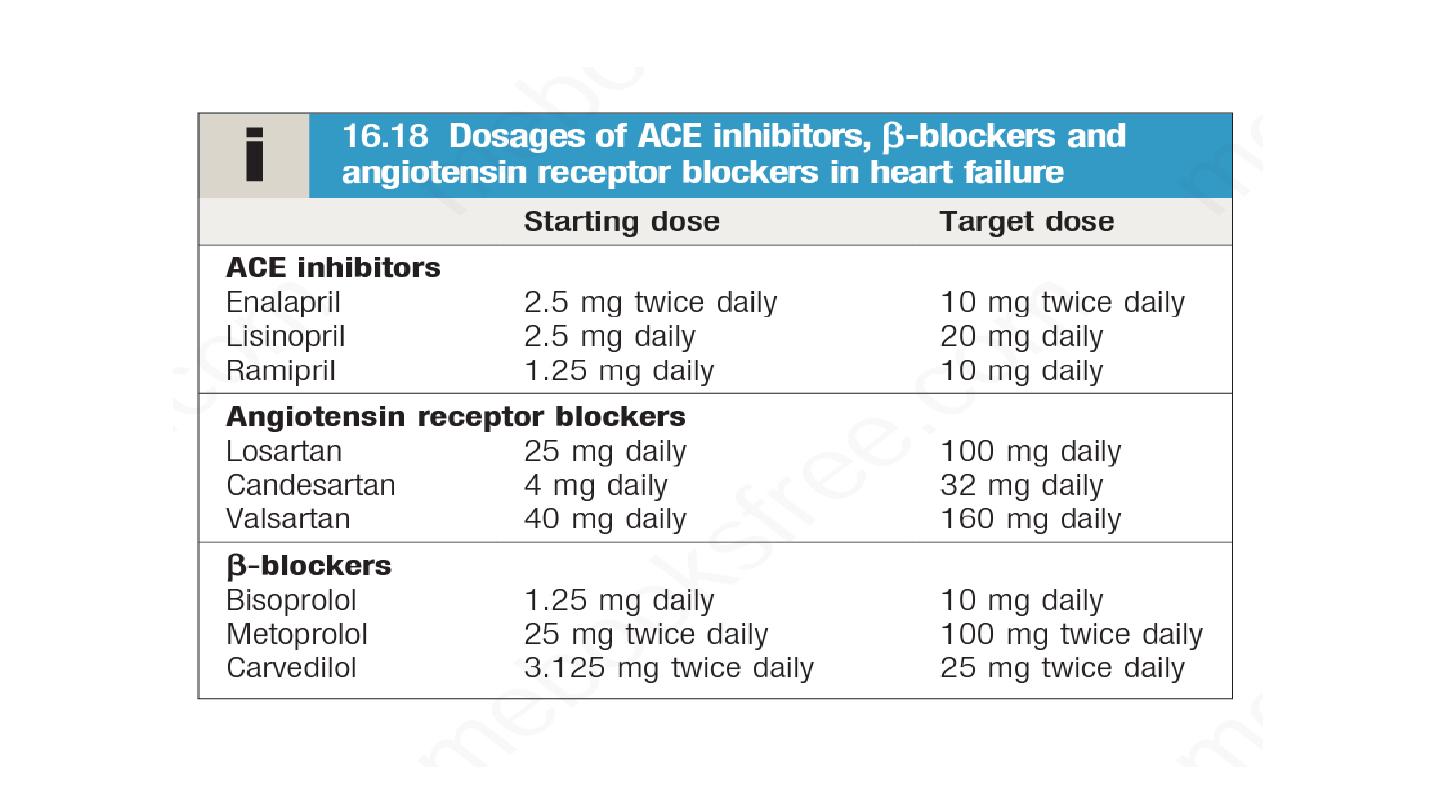
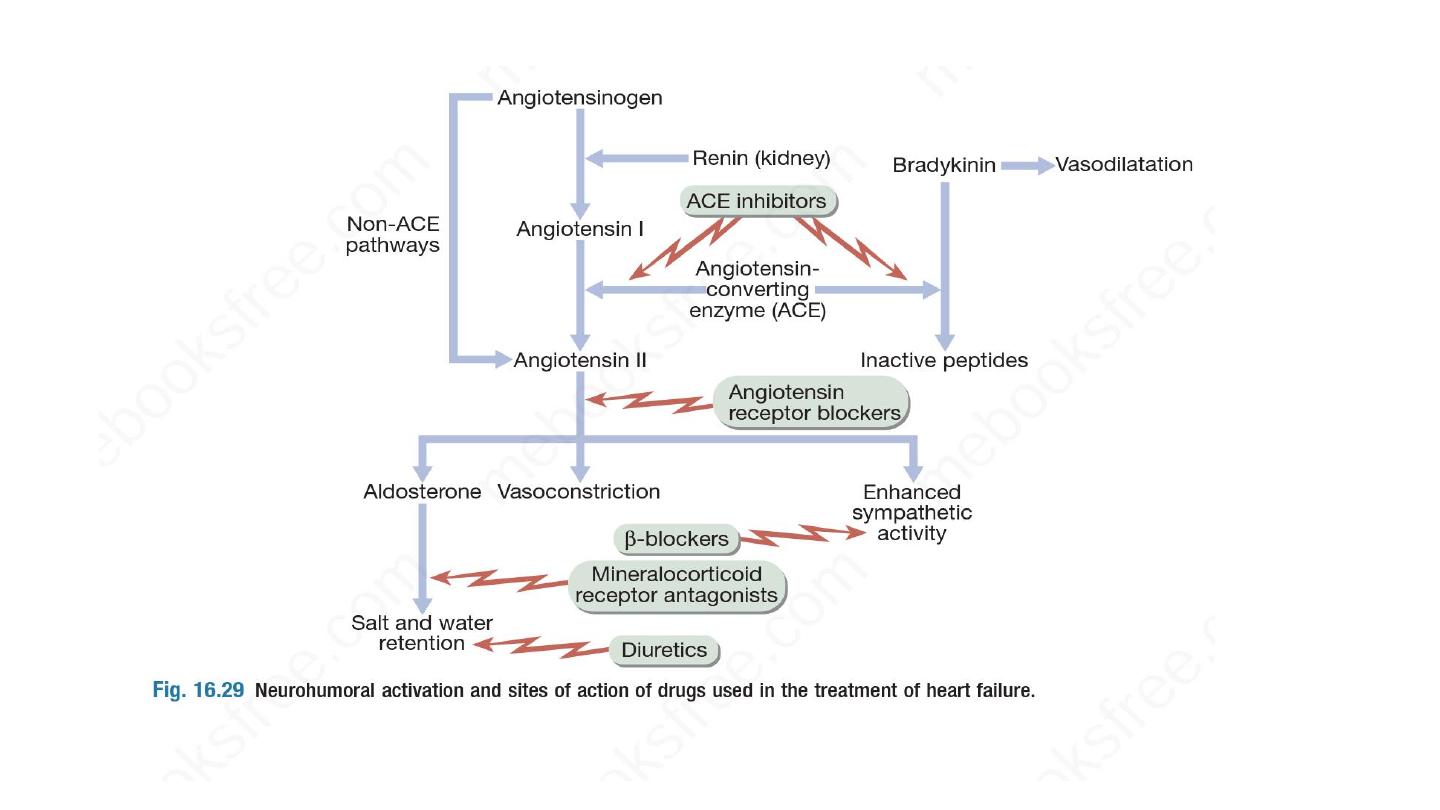

• Beta blocker
• Beta -blockers are more effective at reducing mortality than ACE
inhibitors, with a relative risk reduction of 33% versus 20%,
respectively.
• Ivabradine
• Digoxin
• Amiodarone

• Vasodilators
• Nitrate and hydralazine

• Neprilysin inhibitors
Sacubtril
ARNI
• Calcium channel blocker

Non pharmacological treatment
• ICD
• CRT
• Coronary revascularization : stunned and hibernating myocardium
• VAD
• Cardiac trasplant