
GASTROINTESTINAL T
Lectures 1& 2
Depart. Of pathology
Oral Cavity and Oropharyngeal Cancer
Background Info.
Oral Cavity = Mouth
-
Lips, inside lining of the lips and cheeks, the teeth, the gums, the frontal
two-thirds of the tongue, the floor of the mouth below the tongue, the
bony roof of the mouth (hard palate), and the area behind the wisdom
teeth.
-
Oropharyngeal cancer develops in the part of the throat just behind the
mouth, called the oropharynx. The oropharynx begins where the oral
cavity stops. It includes the base of tongue (the back third of the tongue),
the soft palate, the tonsils and tonsillar pillars, and the back wall of the
throat.
-
The oral cavity and oropharynx assist in: breathing, talking, eating,
chewing, and swallowing. Minor salivary glands located throughout the
oral cavity and oropharynx make saliva that keeps the mouth moist and
helps digest food.
-
Contain several types of tissue and each of these tissues contains
several types of cells.
Leukoplakia, Erythroplakia, and Dysplasia.
Leukoplakia and Erythroplakia: an abnormal area in the mouth or throat.
-
Leukoplakia: is a white area.
-
Erythroplakia: is a slightly raised, red area that bleeds easily if scraped.
These white or red areas may be a cancer, or they may be a precancerous
condition called dysplasia. They could also be some relatively harmless
condition.
of
1
12
GASTROINTESTINAL T
Lectures 1& 2
Depart. Of pathology
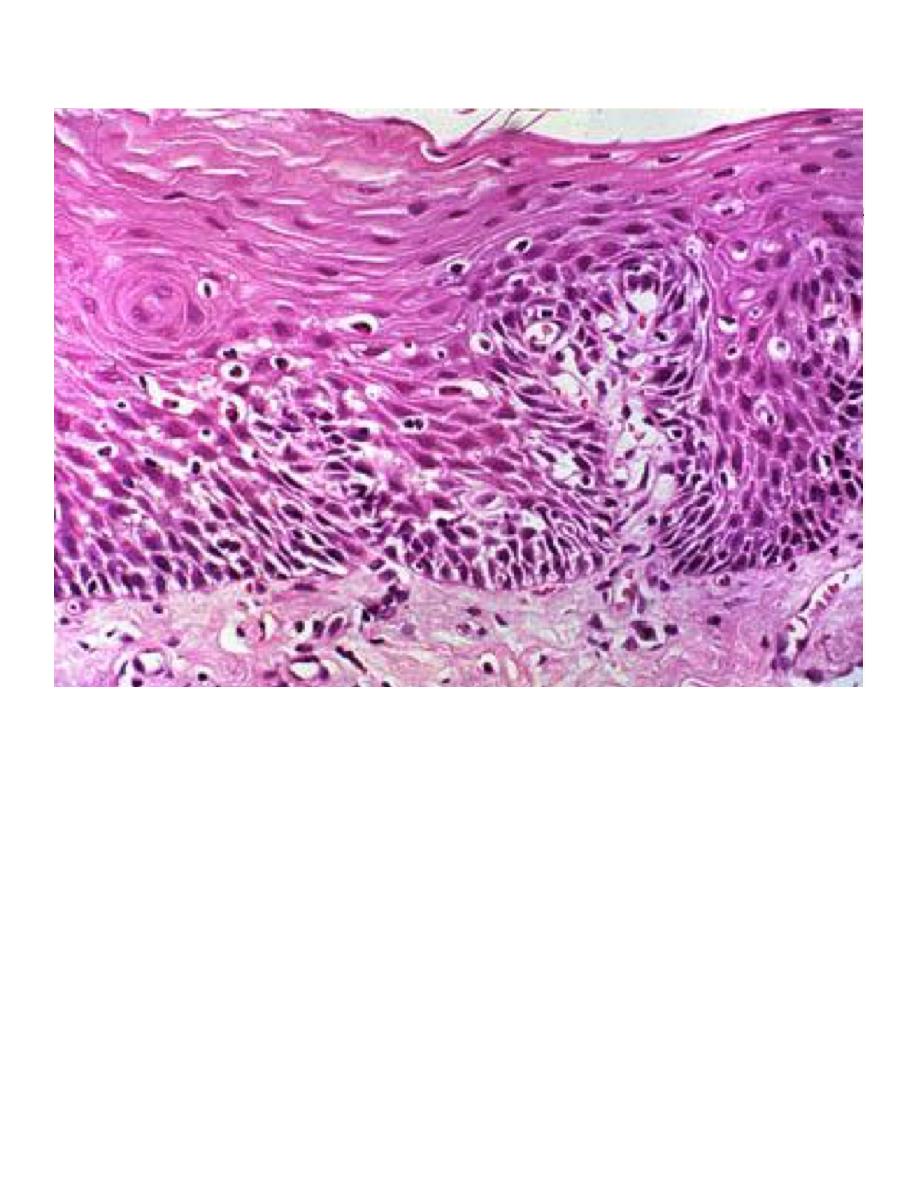
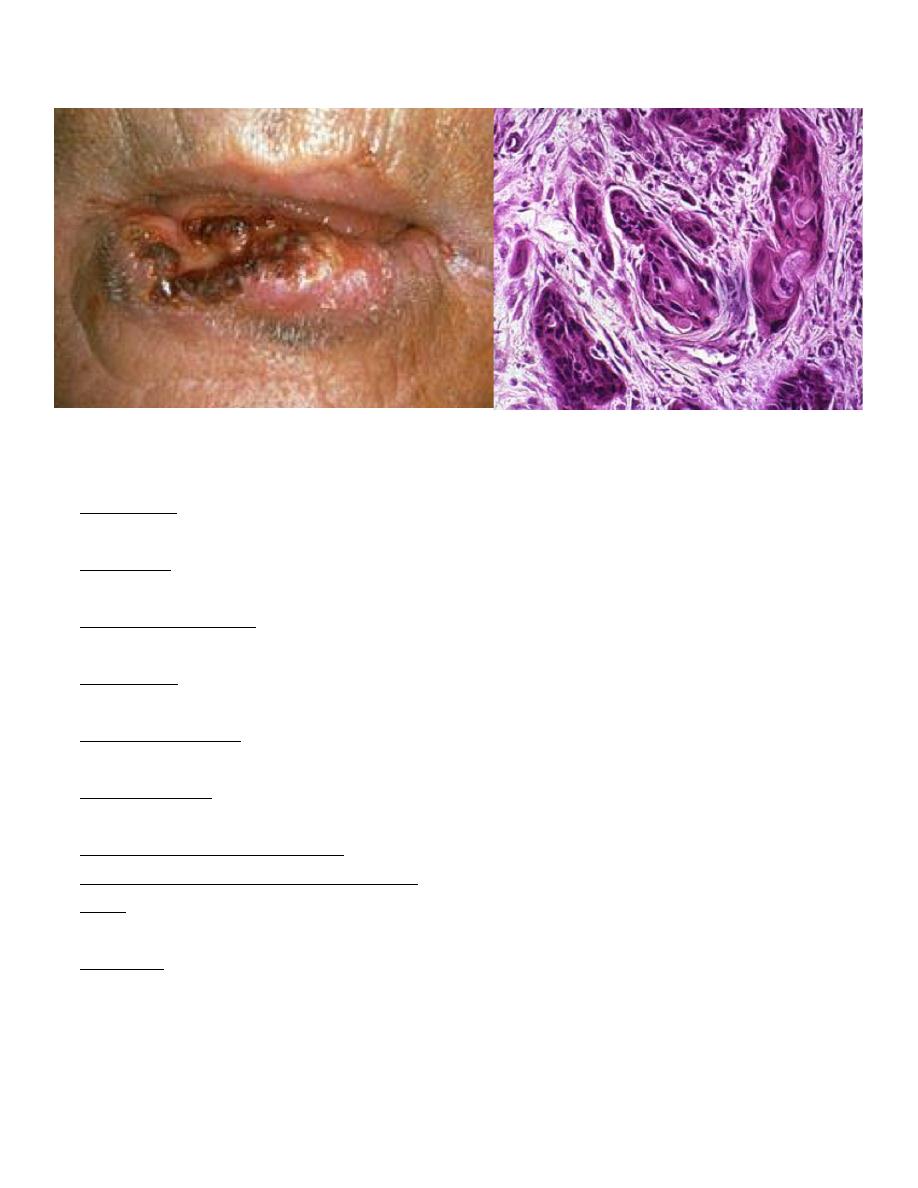
Malignant Oral Cavity and Oropharyngeal Tumors.
-
More than 90% of cancers of the oral cavity and oropharynx are
squamous cell carcinomas, also called squamous cell cancer.
-
Squamous cells are flat, scale-like cells that normally form the lining of the
oral cavity and oropharynx.
-
Invasive squamous cell cancer means that the cancer cells have spread
beyond this layer into deeper layers of the oral cavity or oropharynx.
of
2
12
GASTROINTESTINAL T
Lectures 1& 2
Depart. Of pathology
Risk Factors
-
Tobacco: About 90% of people with oral cavity and oropharyngeal cancer
use tobacco
-
Alcohol: Drinking alcohol strongly increases a smoker's risk of
developing oral cavity and oropharyngeal cancer.
-
Ultraviolet light: More than 30% of patients with cancers of the lip have
outdoor occupations associated with prolonged exposure to sunlight.
-
Irritation: Long-term irritation to the lining of the mouth caused by poorly
fitting dentures, sharp teeth.
-
Poor nutrition: A diet low in fruits and vegetables is associated with an
increased risk
-
Mouthwash: Some studies have suggested that mouthwash with a high
alcohol content
-
Human papilloma virus (HPV) infection:
-
Immune system suppression.
-
Age: The likelihood of developing oral and oropharyngeal cancer
increases with age, especially after age 35.
-
Gender: Oral and oropharyngeal cancer is twice as common in men as in
women
of
3
12
GASTROINTESTINAL T
Lectures 1& 2
Depart. Of pathology
Tobacco & Alcohol.
-
We know that tobacco and alcohol can damage cells in the lining of the
oral cavity and oropharynx, and that cells in this layer must grow more
rapidly to repair this damage. Many of the chemicals found in tobacco
cause damage to DNA, which contains the cell's instructions for repair
and growth.
-
Scientists are not sure whether alcohol directly damages DNA, but they
have shown that alcohol increases penetration of many DNA-damaging
chemicals into cells
Molecular changes of SCC.
A multistep process with activation of oncogenes & inactivation of TSGs &
chromosomal alterations.
-
Loss of chromosomal regions at ch 3 & 9 → inactivation of p16
gene( inhibitor of cyclin dependant kinase).
-
normal→ hyperplasia/ hyperkeratosis.
-
Mutation of p53 TSG→ progression to dysplasia / CIS.
-
Over-expression of cyclin D1 gene → Invasive SCC.
-
Alterations in EGFR, it is over expressed in HNSCC & it is used as a
target in the treatment of this disease.
How to Detect and Diagnose Oral Cancer.
-
Many cancers of the oral cavity and oropharynx can be found early,
during routine screening examinations by a doctor or dentist, or by self-
examination.
Symptoms
-
a sore in the mouth that does not heal (most common
symptom).
-
pain in the mouth that doesn't go away (also very
common).
of
4
12
GASTROINTESTINAL T
Lectures 1& 2
Depart. Of pathology
-
a persistent lump or thickening in the cheek.
-
a persistent white or red patch on the gums, tongue, tonsil, or lining of the
mouth.
-
a sore throat or a feeling that something is caught in the throat that
doesn't go away.
-
difficulty chewing or swallowing.
-
difficulty moving the jaw or tongue.
-
swelling of the jaw that causes dentures to fit poorly or become
uncomfortable.
-
loosening of the teeth or pain around the teeth or jaw.
-
voice changes.
-
a lump or mass in the neck.
-
weight loss.
-
persistent bad breath
of
5
12
GASTROINTESTINAL T
Lectures 1& 2
Depart. Of pathology
What's new in oral cavity and oropharyngeal cancer research
and treatment?
-
DNA changes:
One of the changes often found in DNA of oral cancer cells is a
mutation of the p53 gene. Recent studies suggest that tests to detect
these p53 gene alterations may allow very early detection of oral and
oropharyngeal tumors.
What’s New...
-
Tumor growth factors: Oral and oropharyngeal cancers with too many
EGF receptors tend to be especially aggressive. New drugs that
specifically recognize cells with too many EGF receptors are now being
tested in clinical trials. These drugs work by preventing EGF from
promoting reproduction of cancer cells, and may also help the patient's
immune system recognize and attack the cancer.
-
New chemotherapy.
-
New radiotherapy methods.
-
Vaccines: Some oral and oropharyngeal cancers contain DNA from
human papilloma viruses, vaccines against these viruses are being
studied as a treatment for these cancers .
-
Gene therapy: Another type of gene therapy adds new genes to the
cancer cells to make them more susceptible to being killed by certain
drugs.
Cysts of the Oral Region.
-
A cyst may be defined as an epithelium-lined pathologic cavity that may
contain fluid and cellular debris.
-
Some cysts are not “true” cysts because they are not epithelium-lined.
Therefore, the name - pseudocyst.
Radicular or Periapical Cyst.
-
Usually a result of dental caries.
of
6
12
GASTROINTESTINAL T
Lectures 1& 2
Depart. Of pathology
-
Usually seen as a well-circumscribed radiolucency around the apex of a
tooth.
-
By definition, the presence of non-vital pulp is necessary for the clinical
diagnosis of a radicular cyst to be made.
Neck swellings Differential diagnosis.
-
Neck divided into anterior and posterior triangles by sternocleidomastoid
m.
-
Cervical lymphadenopathy commonest cause of neck swelling.
Neck Swellings D/D (benign).
-
Congenital swellings; branchial cleft swellings, thyroglossal duct cyst,
laryngocoele, haemangiomas, cystic hygromas, dermoid.
-
Inflammatory: acute & chronic lymphadenitis (infectious mononucleosis,
toxoplasmosis, cat scratch fever, actinomycosis, histoplasmosis,
tuberculosis).
-
traumatic: aneurysms, av malformation, etc.
-
Miscellaneous: Pharyngeal pouch, cervical ribs, thyroid, etc.
-
Branchial cleft cyst:
-
Remnants of incompletely obliterated branchial clefts/pouches.
-
Located anterior & deep to sternomastoid.
-
Painless swelling.
-
Young adults.
-
M= F ratio.
-
Unilateral, 75% on left side.
-
Thyroglossal duct cyst:
-
70% of all congenital cysts.
-
Arrested migration of thyroid.
-
Painless midline swelling.
-
Sistrunk operation.
of
7
12
GASTROINTESTINAL T
Lectures 1& 2
Depart. Of pathology
Thyroglossal Tract Cyst:
-
Most common developmental cyst of the neck.
-
Its etiology relates to thyroid gland development.
-
Remember, the thyroid gland originates in the area of the foramen
cecum. From there, it grows downward to its permanent location in the
neck. The embryonic tract of thyroid tissue between the foramen cecum
and the cervical location of the thyroid gland eventually atrophies.
Thyroglossal Con’t:
-
Residual epithelial elements that do not
completely atrophy may give rise to cysts in
childhood or adulthood that may present in the
posterior portion of the tongue(lingual thyroid)
or in the neck. The majority occur at the
midline of the neck below the level of the hyoid
bone.
-
Asymptomatic - Surgical Excision
Neck swellings:
-
Cystic hygroma:
-
Collection of lymph sacs.
-
Present at the root of neck (post. Triangle), arm, groin.
-
Pharyngeal pouch:
-
Pulsion diverticulum.
-
Uncoordinated swallowing.
-
Sternomastoid tumour:
-
Birth trauma, infarcted segment , fibrosis, torticollis.
-
Cervical rib:
-
Extra cervical rib.
-
< 1% population.
-
Neurological and vascular problems.
of
8
12
GASTROINTESTINAL T
Lectures 1& 2
Depart. Of pathology
-
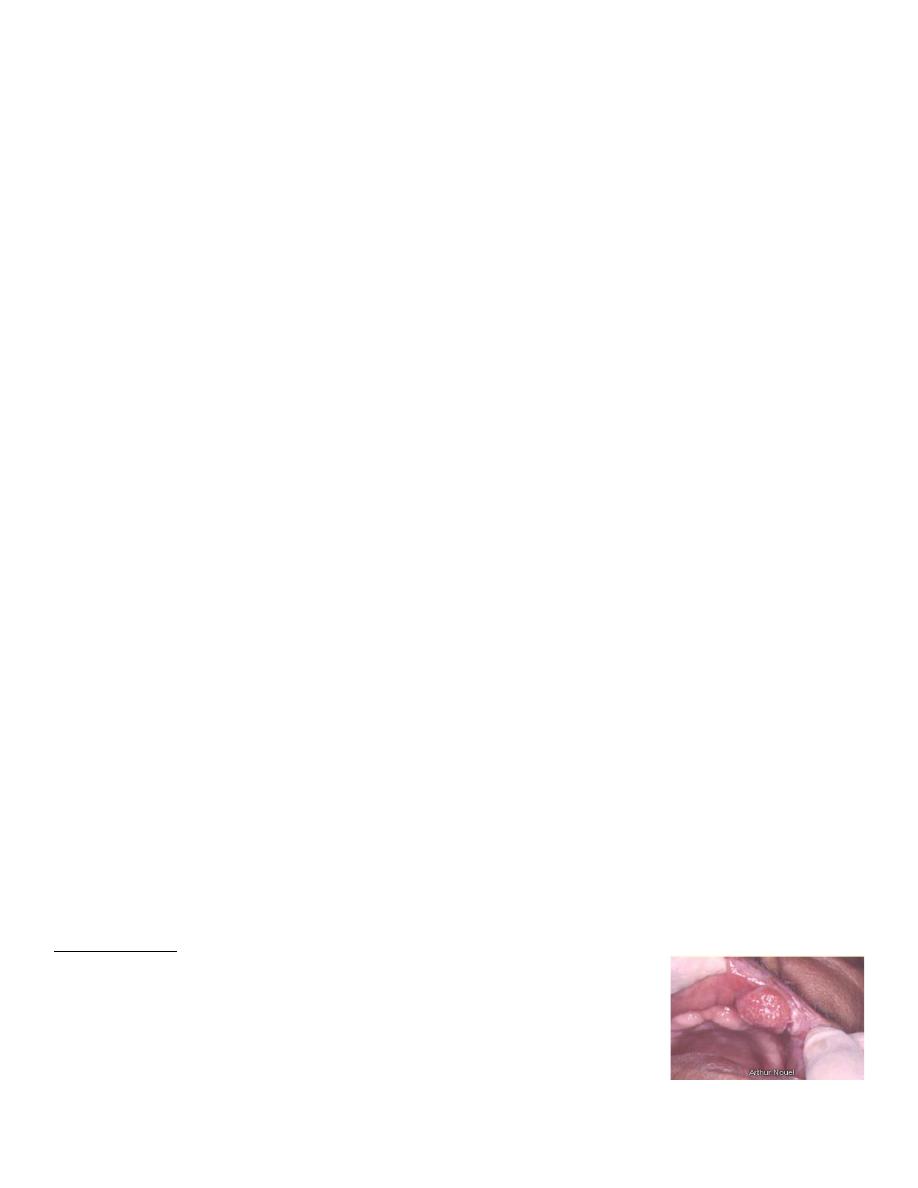
Ranula:
-
Mucous containing cyst in floor of mouth.
-
Painless midline, spherical, smooth, fluctuant, transilluminant.
-
Dermoid cyst.
-
Midline, asymptomatic, painful when infected.
-
Laryngocoele:
-
Diverticulum of laryngeal ventricle.
-
Lined by epithelium.
-
Common in glass blowers/wind instruments musicians, etc
Neck swellings Tumours:
-
Benign; Carotid body tumour, lipoma, soft tissue tumour.
-
Malignant: skin tumours( SCC, BCC, melanomas), thyroid tumours,
salivary gland tumours.
Carotid body tumour:
-
Sporadic occurrence 90%.
-
Familial 10%.
-
Unilateral, but bilateral/multi-centric 10% sporadic, 50% bilateral familial.
-
Grows 0.5 cms /year
Salivary Glands:
-
Three paired glands Parotid; largest of the major salivary glands.
-
Two Lobes divided by facial nerve.
-
Submandibular gland Deep to mylohyoid, superficial to hyoglossus .
-
Sublingual; Smallest of the salivary glands.
-
Common surgical disease; infection/calculi
of
9
12
GASTROINTESTINAL T
Lectures 1& 2
Depart. Of pathology
Salivary Glands {Benign conditions}:
-
Mumps:
-
Acute painful parotitis
-
Viral in etiology
-
Self limiting
-
Mikulicz’s Syndrome:
-
Bilateral enlargement of salivary & lacrimal glands.
-
Sjogren’s Syndrome:
-
Triad of dry eyes, dry mouth, dry joints
-
Autoimmune
-
Lymphocytic infiltration
-
Pyogenic parotitis:
-
Surgical, debilitated patients
-
Staphylococcus Swollen,
-
painful parotid glands
-
Pus from stensen’s duct
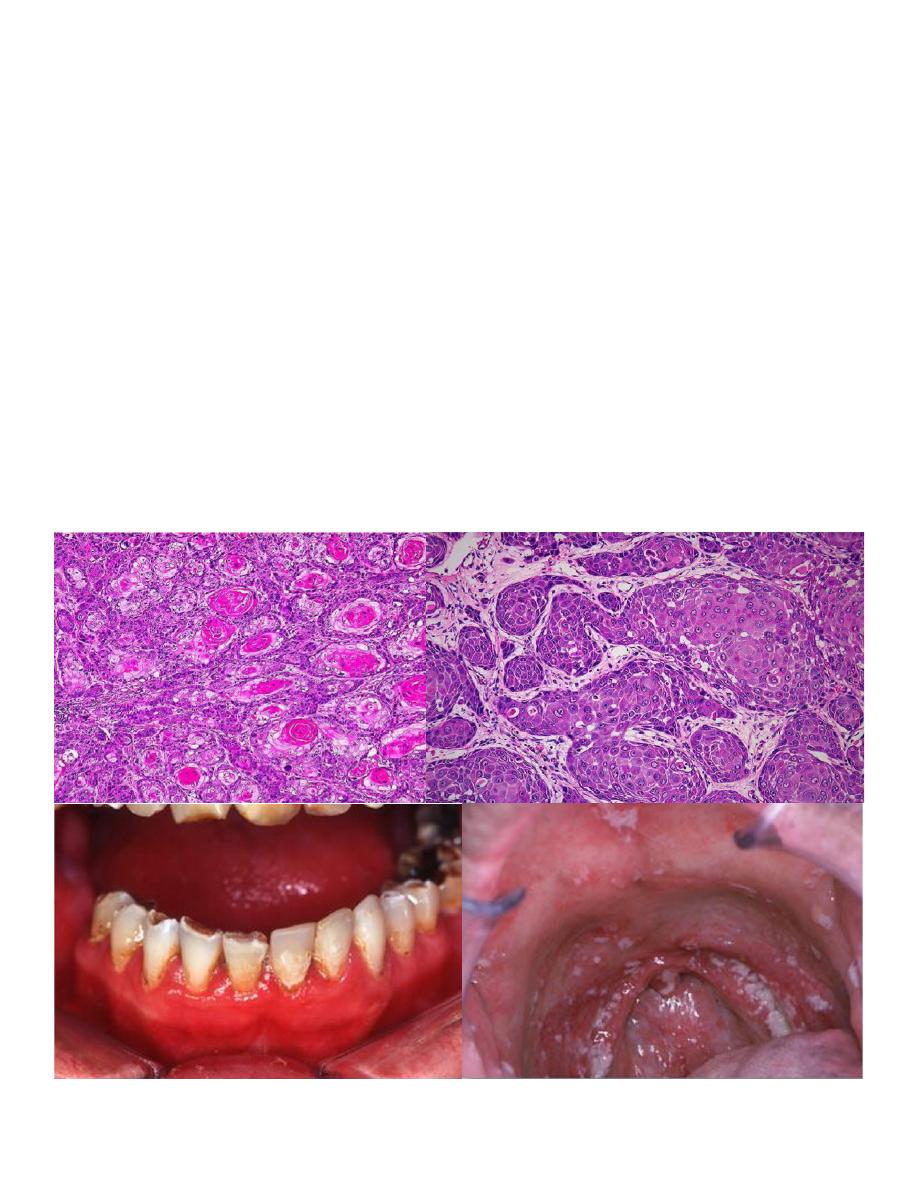
Salivary glands {Benign Tumours}:
-
Comprise 3% - 6% of all head & neck tumours.
-
Pleomorphic Adenoma.
-
Commonest tumour (53% - 71%).
-
Slowly growing, painless, solitary, firm, smooth, movable without
nerve involvement.
-
Both mesenchymal/epithelial elements.
-
FNA, CT, MRI.
-
Superficial parotidectomy
-
Warthin’s tumour(adenolymphoma, papillary cystadenoma
lymphomatosum).
-
6% - 10% .
-
Benign, bilateral, parotid gland only.
-
Older age group.
of
10
12
GASTROINTESTINAL T
Lectures 1& 2
Depart. Of pathology
-
Superficial location.
-
Malignant potential non existent
Salivary Glands MalignantTumours:
-
Locally aggressive.
-
Grow along neural pathways, may access skull base and brain
eventually.
-
Also lymphatic and haematogenous spread.
-
Mucoepidermoid Carcinoma:
-
Commonest malignant tumour.
-
50% of all salivary gland malignancies.
-
Parotid involved in 40% - 50%.
-
75% are low grade & have good prognosis.
-
1 – 5 year survival 85%.
-
High grade mucoepidermoid carcinomas invade locally, spread
regionally & distant mets.
-
5 year survival drops 30%.
-
Adenocystic carcinoma (Cylindroma):
-
Commonly involves submandibular (35% - 40%), only 7% of parotid
malignancies.
-
Slowly growing.
-
Perineural invasion.
-
30% lymph node mets, 50% distant mets.
-
5 year survival 75%.
-
10 year survival 30%.
-
20 year survival 13%.
-
Mixed malignant tumour:
-
Long standing pleomorphic adenoma.
-
Older age group.
-
Worse prognosis.
-
Lymph node mets 15%.
-
Distant mets 30%.
of
11
12

GASTROINTESTINAL T
Lectures 1& 2
Depart. Of pathology
-
5 year survival 40% - 50%.
-
15% year survival 20%.
-
Acinic cell carcinoma:
-
Low grade.
-
Slow growing.
-
10 % of malignant parotid tumour.
-
Lymph node mets 10% .
-
Aggressive tumours .
-
Radical parotidectomy.
-
Squamous cell carcinomas:
-
Infrequent occurrence 1% - 5%.
-
May have skin infiltration.
-
Total radical parotidectomy.
Salivary Glands Evaluation & Diagnosis:
-
History & clinical examination.
-
Sialography – of no value.
-
CT scans.
-
CT sialography for retromandibular/parapharyngeal.
-
MRI.
-
Incisional biopsy contraindicated.
-
FNAC
of
12
12
