By
Dr. Ameer kadhim Hussein
M.B.Ch.B. FICMS (Community Medicine)
TUBERCULOSIS

TB is an infectious disease caused by the bacillus
Mycobacterium tuberculosis
. It typically affects the
lungs (pulmonary TB) but can affect other sites as well
(extra pulmonary TB). The disease is spread in the air
when people who are sick with pulmonary TB expel
bacteria for example by coughing.
TB is also more common among men than women, and
affects mostly adults in the economically productive age
groups.
INTRODUCTION
Mycobacterium tuberculosis complex which include :
M. Tuberculosis.
M. Bovis.
M. Africanum.
M. Microti.
M. Canetti
.
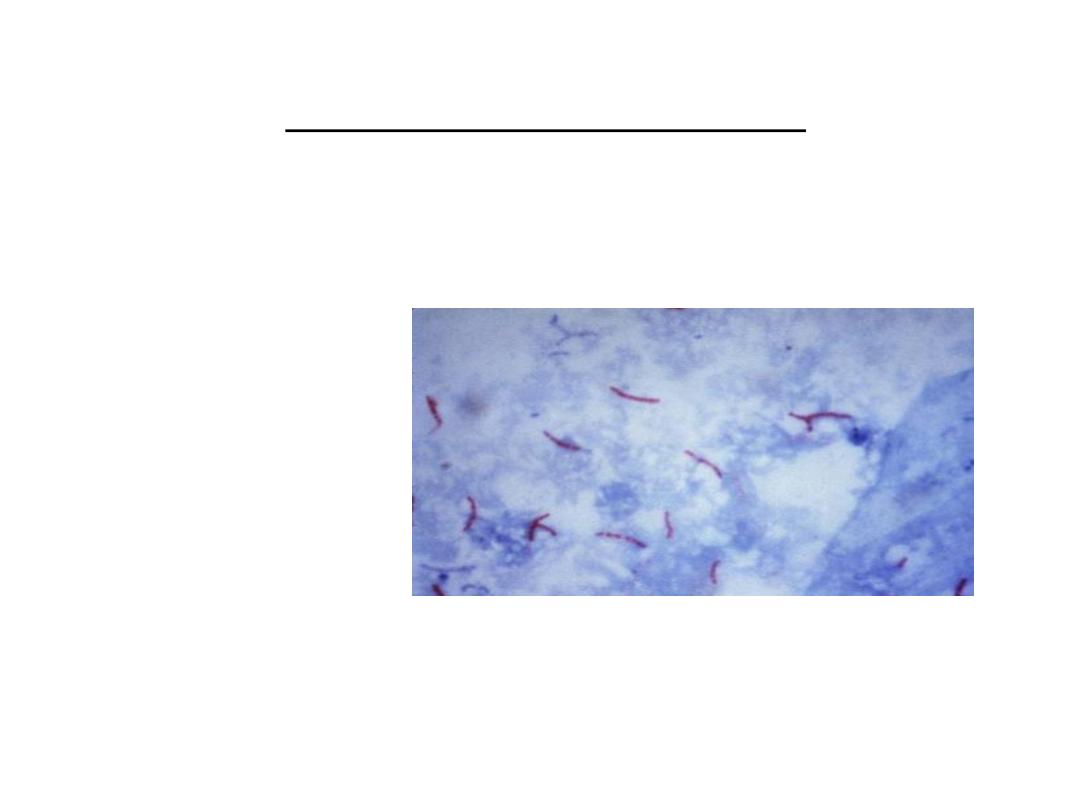
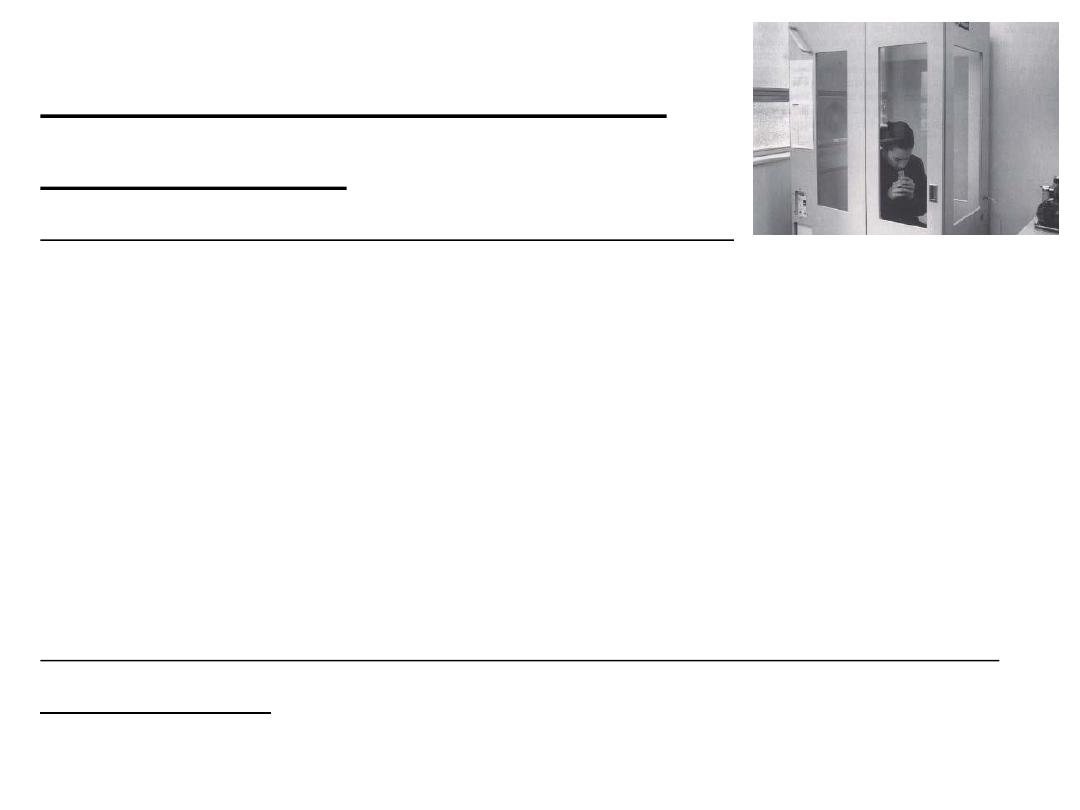
M. tuberculosis visualization by Ziehl–Neelsen stain
INFECTIOUS AGENT
TB TRANSMISSION
TB spread from person to person through the air via droplet nuclei.
M. tuberculosis may be expelled when an infectious person (Cough,
Sneeze, Speaks, Sings).
Transmission occurs when another person inhales droplet nuclei.
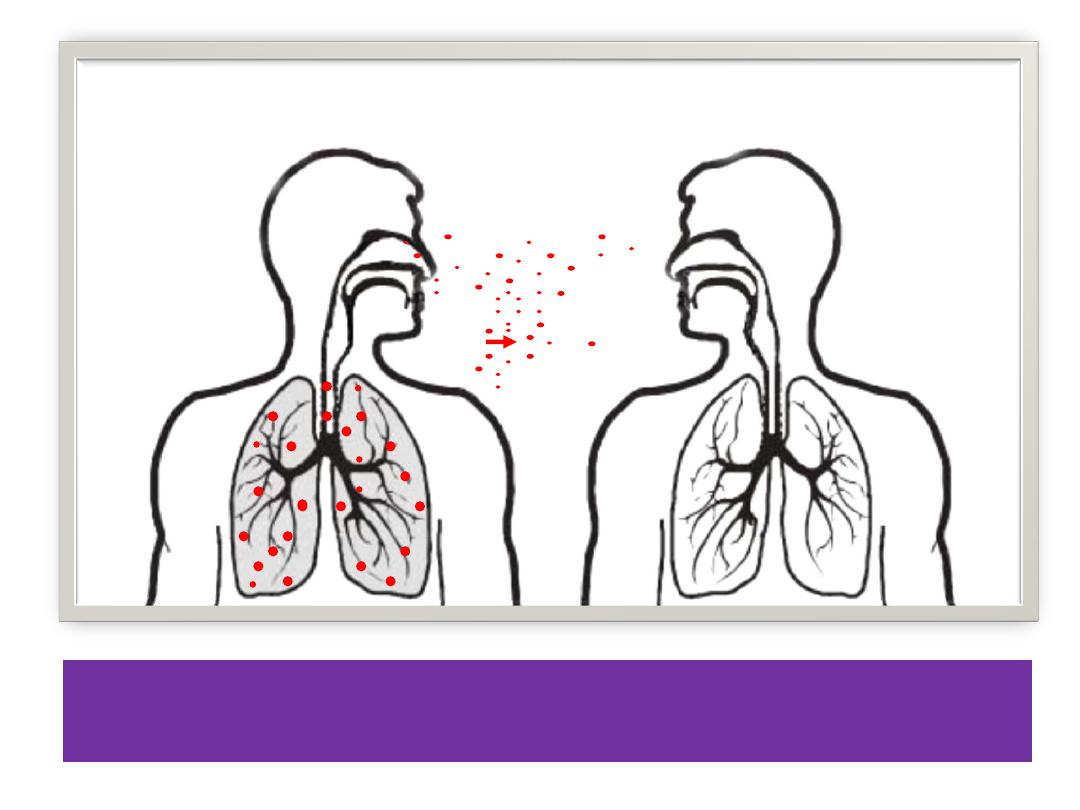
DOTS IN AIR REPRESENT DROPLET NUCLEI
CONTAINING M. TUBERCULOSIS
Probability that TB will be transmitted depends on:
1. Infectiousness of person with TB disease.
2. Environment in which exposure occurred.
3. Length of exposure.
4. Virulence (strength) of the tubercle bacilli.
The best way to stop transmission is to:
1. Isolate infectious persons.
2. Provide effective treatment to infectious persons as soon as
possible.
TB PATHOGENESIS
Pathogenesis is defined as how an infection or disease develops in the
body.
a. Latent TB Infection (LTBI):
Occurs when tubercle bacilli in the body, but the immune system is
keeping them under control. This infection usually detected by the Mantoux
tuberculin skin test.
b. TB Disease:
Develops when immune system cannot keep tubercle bacilli under control. It
may develop very soon after infection or many years after infection. About
10% of all people with normal immune systems who have LTBI will develop
TB disease at some point in their lives. People with TB disease are often
infectious.
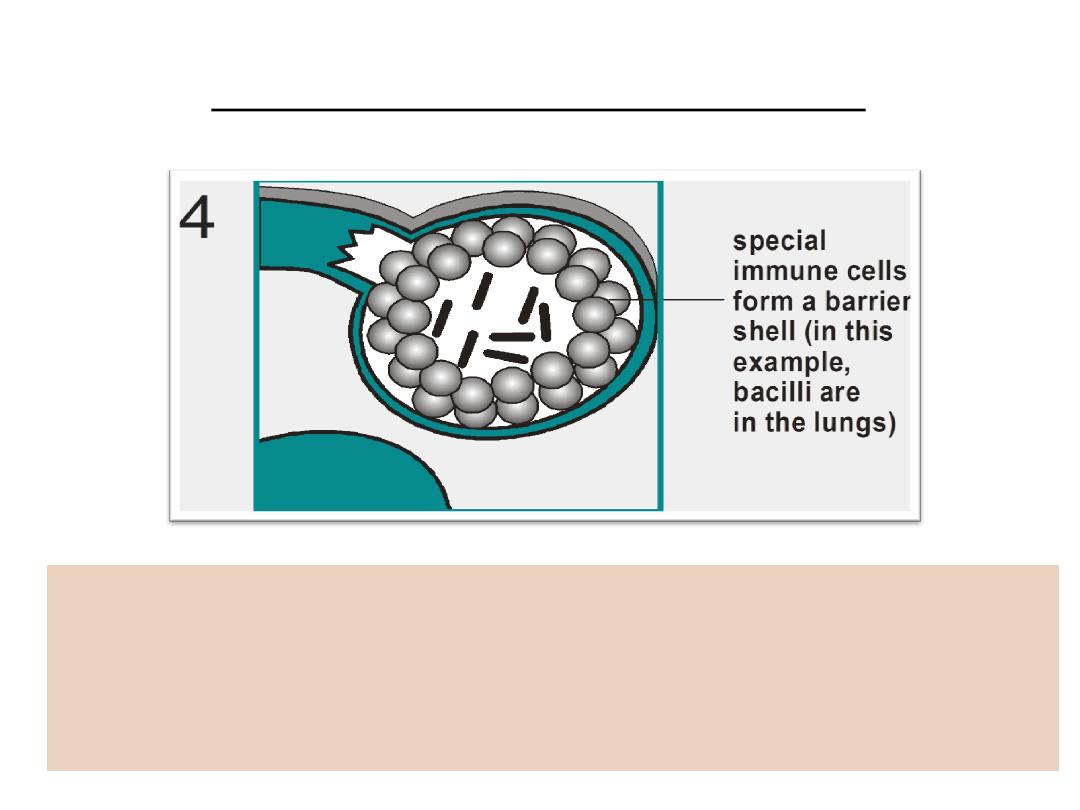
TB PATHOGENESIS (LTBI)
a. Within 2 to 8 weeks the immune system produces special immune
cells called macrophages that surround the tubercle bacilli
b. These cells form a barrier shell that keeps the bacilli contained
and under control (LTBI)
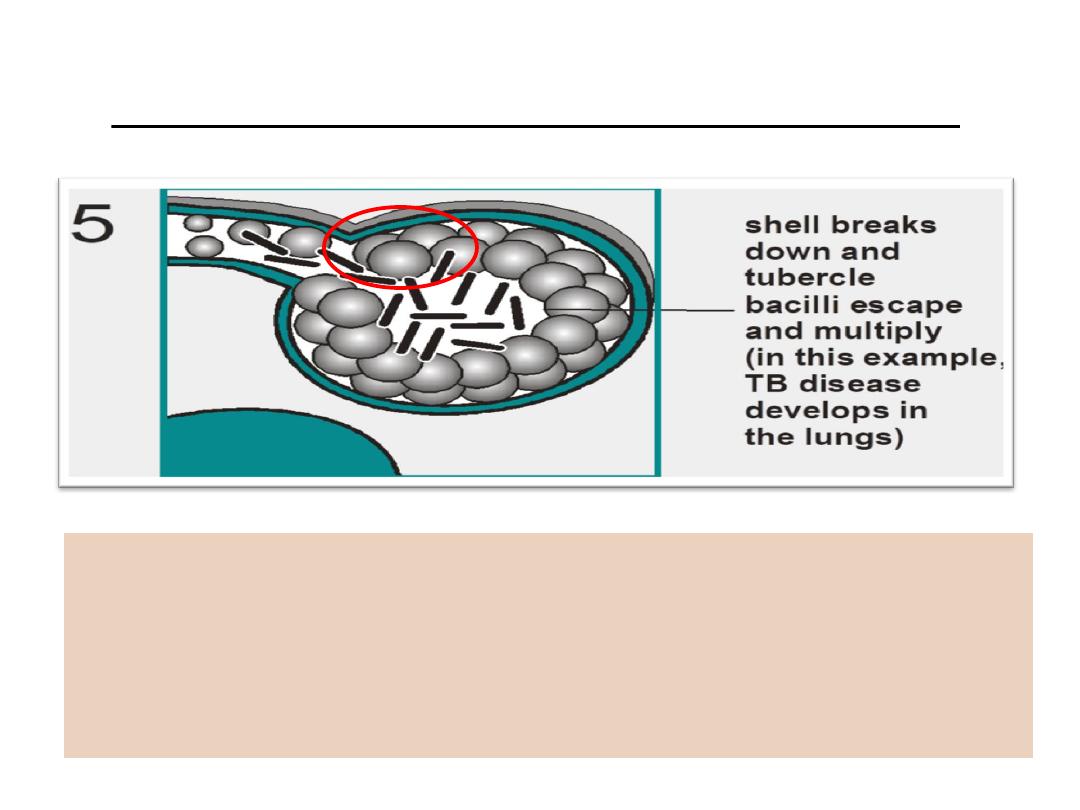
TB PATHOGENESIS (TB DISEASE)
a. If the immune system CANNOT keep tubercle bacilli under
control, bacilli begin to multiply rapidly and cause
TB disease.
b. This process can occur in different places in the body.
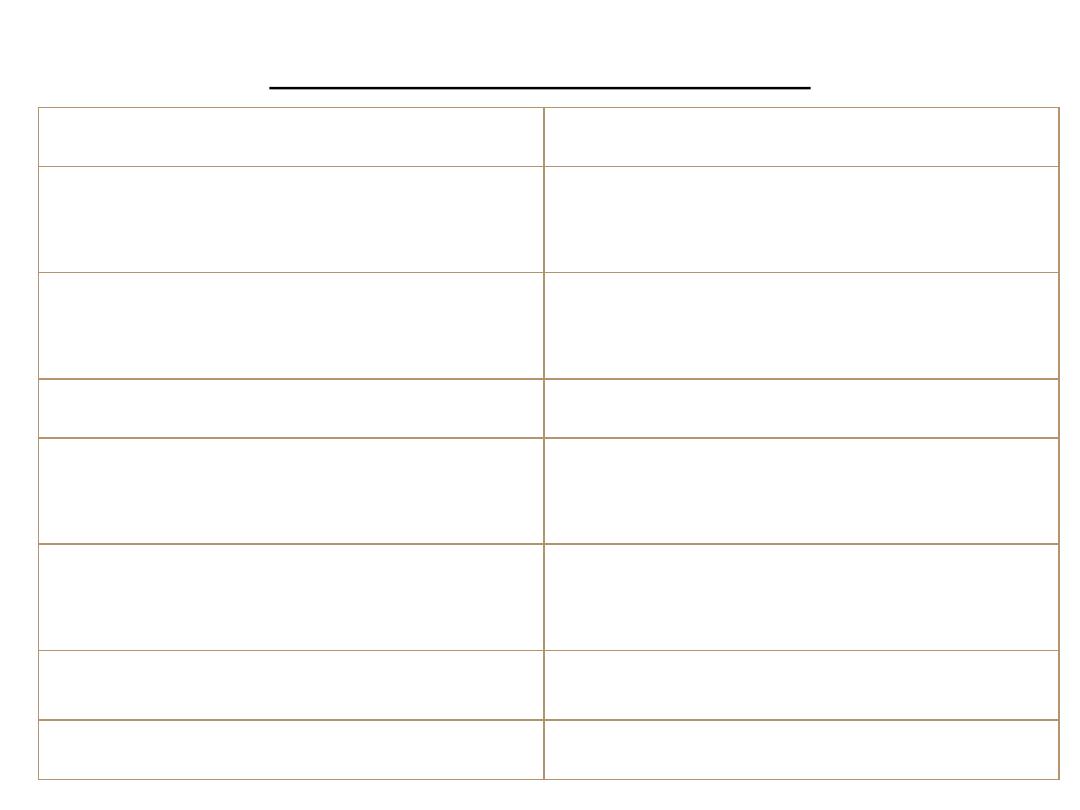
LTBI VS. TB DISEASE
Latent TB Infection (LTBI)
TB Disease (in the lungs)
Inactive, contained tubercle
bacilli in the body
Active, multiplying tubercle
bacilli in the body
TST or blood test results usually
positive
TST or blood test results usually
positive
Chest x-ray usually normal
Chest x-ray usually abnormal
Sputum smears and cultures
negative
Sputum smears and cultures may
be positive
No symptoms
Symptoms such as cough, fever,
weight loss
Not infectious
Often infectious before treatment
Not a case of TB
A case of TB
Some conditions increase probability of LTBI progressing to TB disease which
include:
1.Infection with HIV.
2.Chest x-ray findings suggestive of previous TB.
3.Substance abuse.
4.Recent TB infection.
5. Prolonged therapy with corticosteroids and other immunosuppressive therapy.
6. Low body weight.
7. Organ transplant.
8. Silicosis.
9. Diabetes mellitus.
10. Severe kidney disease.
11. Certain types of cancer.
12 .Certain intestinal conditions.
PROGRESSION TO TB DISEASE
SITES OF TB DISEASE
Site
Location
Frequency
Pulmonary TB
Lungs
Most TB cases are
pulmonary
Extra
pulmonary TB
Places other than lungs
such as: Larynx,
Lymph nodes, Pleura
Brain, Kidneys
Bones and joints
Found more often in: HIV-
infected or other immuno–
suppressed persons and
young children.
Miliary TB
Carried to all parts of
body through blood
stream
Rare
EPIDEMIOLOGY OF TB
TB is one of the leading causes of death due to infectious
disease in the world.
Almost 2 billion people are infected with M. tuberculosis.
Each year about:
9 million people develop TB disease. 2 million people die of
TB.
In 2012, an estimated 8.6 million people developed TB and
1.3 million died from the disease.
TB occur world wide and majority of cases in developing
countries.
Reservoir:
Humans. For M. bovis cattle and variety of other mammals.
Incubation period:
2-10 weeks from infection to demonstrable primary lesion
and positive TST. 10% of infected persons will develop TB
disease in their lifetimes half of them during 2 years after
initial infection.
Period of communicability:
As long as viable tubercle bacilli are discharged in the sputum
Effective chemotherapy usually eliminates communicability
within 2-4 weeks.
Susceptibility:
The risk of infection with the turbercle bacillus is directly
related to the degree of exposure and less to genetic or other
host factors.
The risk of TB disease is highest among:
1. Children under 3 years.
2. HIV infected persons.
3. First 12-24 months after primary infection.
Also risk of TB increase among adolescents, young adults,
elderly persons and immuno-compromised patients.
Diagnosis
DIAGNOSIS OF LTBI
Available testing methods for
M. tuberculosis
infection include:
1. Mantoux tuberculin skin test (TST).
2. Blood tests known as interferon-gamma release assays
(IGRAs).
Mantoux Tuberculin Skin Test:
TST is administered by injection. Tuberculin is made from proteins
derived from inactive tubercle bacilli. Most people who have TB
infection will have a reaction at injection site.
0.1 ml of 5 tuberculin units of liquid tuberculin are injected between
the layers of skin on forearm.
Forearm should be examined within 48 - 72 hours , reaction is an area
of induration (swelling) around injection site. Induration is measured
in millimeters. Erythema (redness) is not measured.
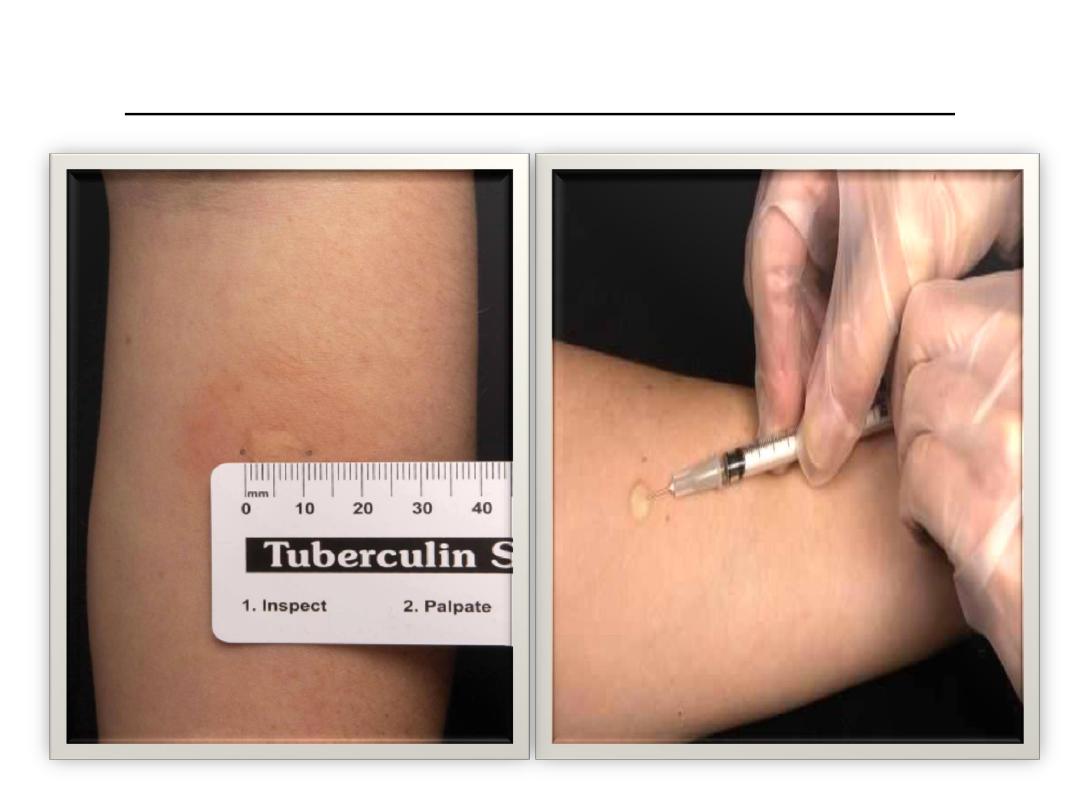
MANTOUX TUBERCULIN SKIN TEST

Diagnosis of TB disease
Medical evaluation:
Components of medical evaluation:
1. Medical history.
2. Physical examination.
3.Test for TB infection.
4. Chest x-ray.
5. Bacteriological examination.
1. Medical history:
General Symptoms of TB Disease:
Fever, Chills, Night sweats, Weight loss, Appetite loss, Fatigue and
Malaise.
Symptoms of Pulmonary TB Disease:
Cough lasting 3 or more weeks , Chest pain and Coughing up sputum
or blood.
Symptoms of extra pulmonary TB disease depend on part of body
that is affected.
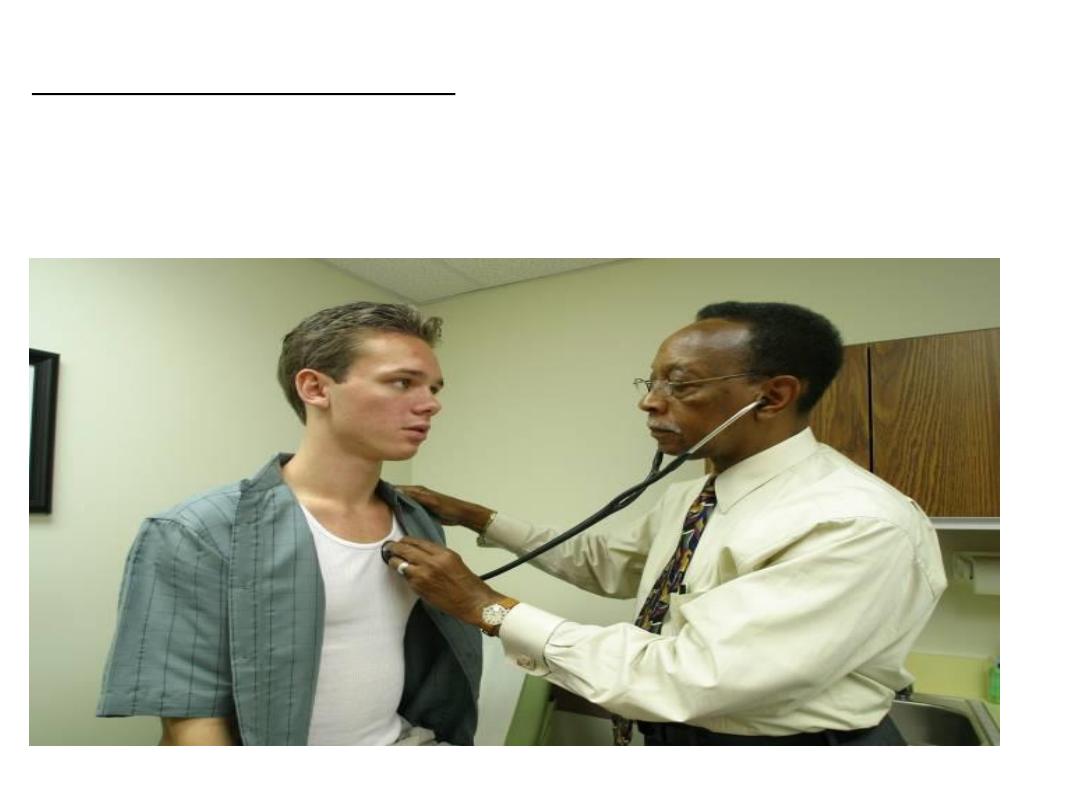
b. Physical examination:
A physical examination cannot confirm or rule out TB
disease, but can provide valuable information.
3.Test for TB Infection: By using tuberculin skin test.
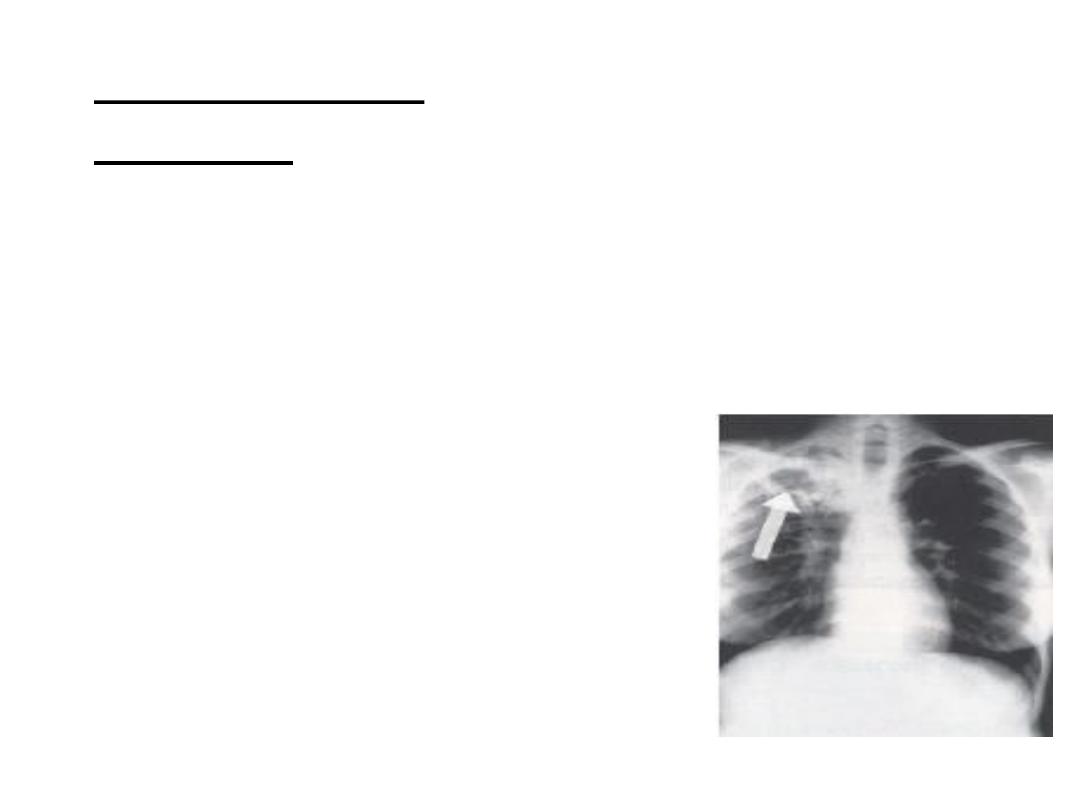
4.Chest x-rays:
When a person has TB disease in lungs, the chest x-ray usually
appears abnormal. It may show:
a. Infiltrates (collections of fluid and cells in lung tissue).
b. Cavities (hollow spaces within lung).
Chest x-rays cannot confirm TB disease.
.BACTERIOLOGIC EXAMINATION
5
Specimen Collection:
For pulmonary TB, specimens can be collected by:
Sputum sample, Induced sputum sample, bronchoscopy and Gastric
washing. Easiest and least expensive method is to have patient cough
into sterile container. Should have at least 3 sputum specimens examined
(Collected in 8-24 hour intervals and at least one early morning
specimen).
Diagnosis of TB depend on demonstration of acid fast bacilli (AFB) in
stained smear of sputum by (Ziehl–Neelsen stain).
For extra-pulmonary TB, specimens may be obtained depends on part
of body affected.
Treatment of LTBI
LTBI is treated to prevent the development of TB
disease. LTBI is treated with medication.
LTBI Treatment Regimens by using:
a. Isoniazid: Preferred regimen is isoniazid (INH) daily
for 9 months .INH may also be given for 6 months.
b. Rifampin (RIF): should be given daily for 4 months
and is recommended for people who:
1. Cannot tolerate INH.
2. Have been exposed to INH-resistant TB.
Treatment of TB Disease
Initial Phase
include first 8 weeks of treatment
Most bacilli killed during this phase
4 drugs used.
Continuation Phase
start after first 8 weeks of treatment.
directed toward bacilli remaining after
initial phase which treated with at
least 2 drugs.
Relapse
Occurs when treatment is not
continued for long enough.
Surviving bacilli may cause TB
disease at a later time.

TREATMENT OF TB DISEASE
Initial regimen should contain
the following four drugs:
1. Isoniazid (H)
2. Rifampin (R)
3. Pyrazinamide (Z)
4. Ethambutol (E)
DOTS strategy:
DOTS (directly observed treatment, short-course) is the
strategy which primary health services are using to detect
and cure TB patients. Health workers counsel and observe
their patients swallowing each dose of medicine and
monitor the patient’s progress until cured.
Types of Patients:
1- New case (Positive, Negative& Extra- pulmonary).
2- Defaulter.
3- Relapse.
4- Chronic Case (drug resistances MDR-TB).
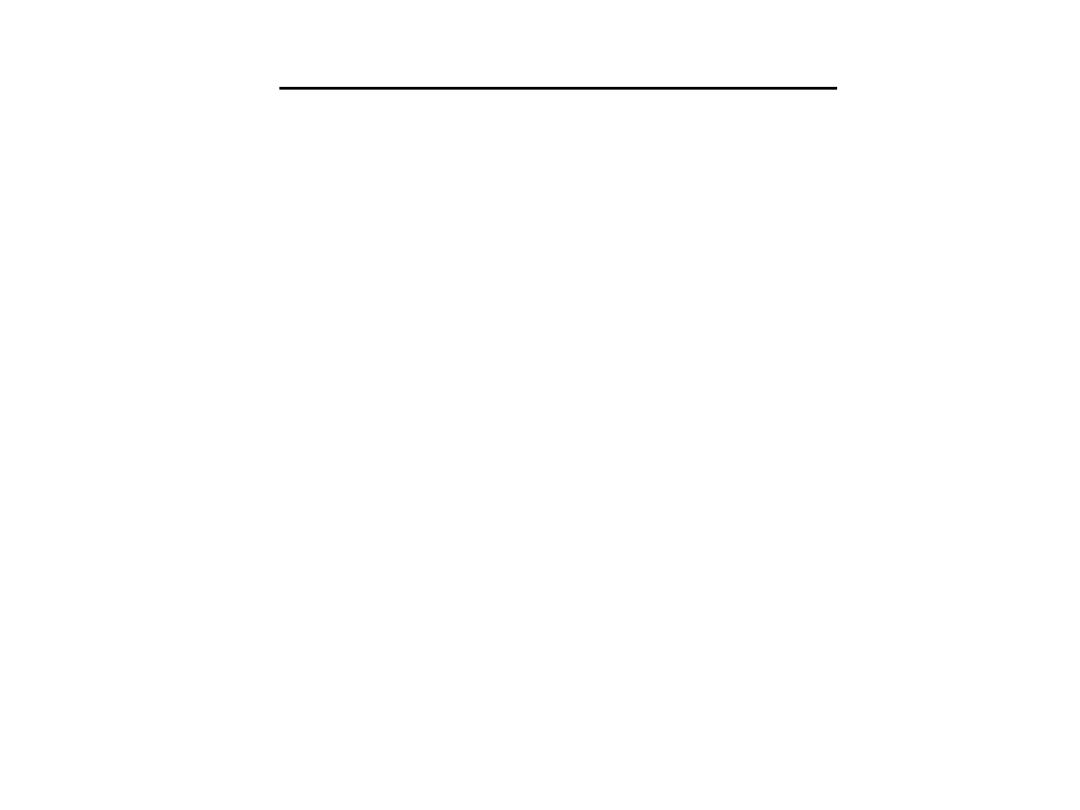
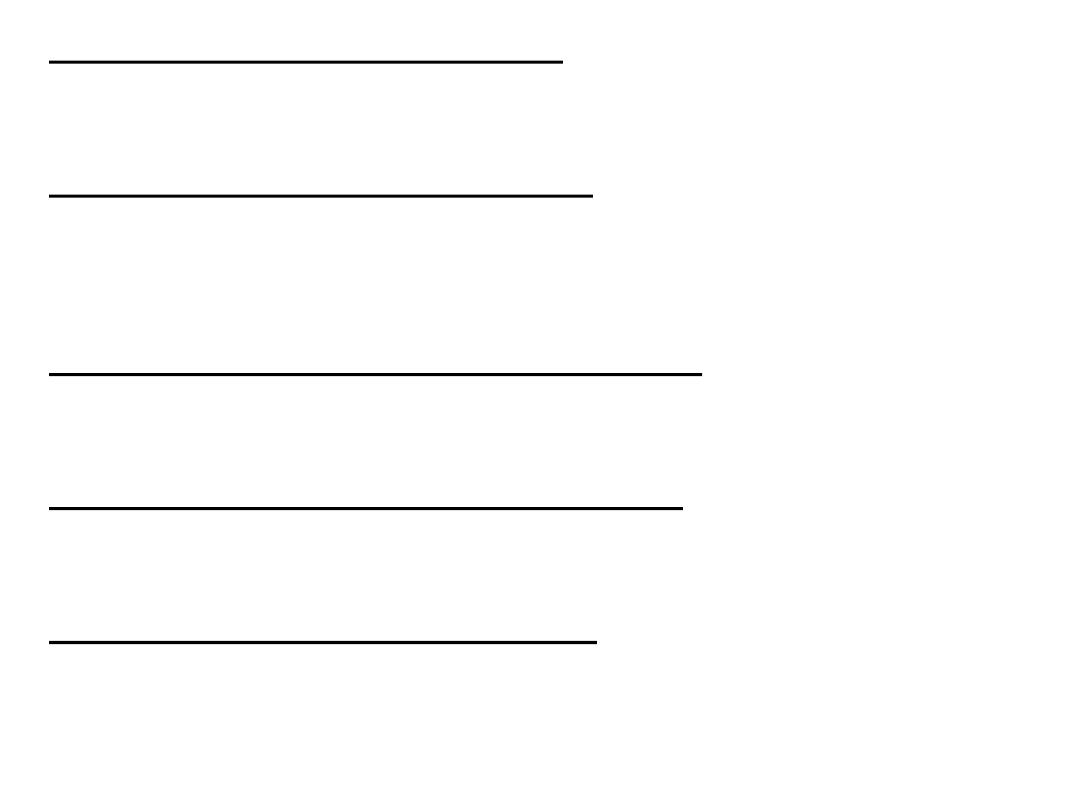
Treatment category
CATEGORY - I TREATMENT
TYPE OF Patients
1. New sputum positive.
2. New sputum negative and seriously ill (Extensive
parenchyma damage).
3. New extra pulmonary seriously ill (Severe form).
CATEGORY - II TREATMENT
TYPE OF PATIENTS
1. Sputum smear positive relapse.
2. Sputum smear positive treatment after default.
3. Sputum smear positive failure.
4 .Other previously treated.
CATEGORY III TREATMENT
-
TYPE OF PATIENTS :
1. New sputum negative and not seriously ill.
2. New extra pulmonary and not seriously ill.
3. New primary TB in children.
4. New not extensive in pregnancy.
Treatment category
pulmonary TB
-
Classification of extra
Not seriously ill
Seriously ill
Lymph node TB
TB meningitis
Pleural effusion (unilateral)
Disseminated TB
Bone (excluding spine)
TB pericarditis
TB Peripheral joint(s)
TB peritonitis & intestinal TB
Bilateral or extensive pleurisy
Spinal TB with neurological
complications
Genito-urinary tract TB
STANDARD SHORT COURSE REGIMEN OF
TB DRUGS (WHO)
-
ANTI
Category I : 2HRZE/4HR.
Category II : 2HRZES/HRZE/5HRE.
Category III : 2HRZ/4HR.
Category IV: Chronic case with MDR-TB.
MDR-TB:
Multi drug-resistant tuberculosis defined as resistance
to at least isoniazid and rifampin which emerged as a
threat to TB control .
MDR-TB treatment requires the use of second-line
drugs that are less effective, more toxic, and costlier
than first-line isoniazid- and rifampin-based regimens.
Isoniazid (INH) Adverse Reactions:
a. Hepatitis.
b. Peripheral Neuropathy.
Refampicin (RIF) Adverse Reactions:
1. Orange discoloration of urine, saliva, and tears.
2. Interaction with other drugs, such as birth control pills and implants,
warfarin, and methadone.
Pyrazinamide (PZA) Adverse effects include:
1. Hepatotoxicity.
2.Non-gouty polyarthralgia ,hyperuricemia and acute gouty arthritis.
Ethambutol (EMB) Adverse effects include:
1. Optic neuritis (impaired perception of the red and green colors).
2. Cutaneous reactions.
Streptomycin Adverse effects include:
1.Vestibular disturbances.
2. Nephrotoxicity.
Treatment follow up
Initial phase: follow up at least weekly (in chest
clinic while under DOTs) to:
a. Reinforce patient education.
b. Watch out for adverse drug reactions
c. Routine blood tests usually not necessary unless there was
clinical features suspicious of hepatitis, underlying liver disease,
etc.
CXR: at 2nd or 3rd month to assess progress.
Sputum:
If pretreatment sputum positive, recheck at 2nd month to assess
conversion to negativity. If still positive at 2nd month, recheck
at 3rd month.
At the end of six month’s treatment:
Assessment:
Repeat chest radiograph.
Sputum examination.
Health education, maintenance of a healthy lifestyle and
awareness of suspicious symptoms.
Methods of control
measures:
a. Preventive
1.The best prevention of TB is prompt diagnosis and treatment
especially of infectious sputum smear –positive cases.
2. Ensure clinical, laboratory and radiology facilities for prompt
identification of suspects and examination of patients and contacts.
3. Educate the public regarding mode of spread, methods of control
and importance of early diagnosis and continued adherence to
treatment.
4. Reduce or eliminate social and economic conditions that increase
the risk of infection and progression to disease (including
malnutrition, silicosis, smoking, alcohol abuse and indoor air
pollution).
5. Establish and maintain effective TB control program and
treat LTBI as mentioned.
6. Persons infected with HIV should be screened for TB once
their infection is identified.
7.Ensure each patient receives directly observed therapy short
course for TB disease and ensure contacts investigations are
conducted to identify and treat latent TB infection among contacts.
8. BCG : (Bacillus-Calmette-Guirine) is the current vaccine for
tuberculosis. It contain a live attenuated strain of Mycobacterium
bovis. BCG used for protection against miliary TB and TB
meningitis during infancy. In Iraq the vaccine given routinely
directly after delivery.
9. Eliminate bovine tuberculosis among cattle and pasteurize or boil
milk and dairy products for human consumption.
b. Control patient, contacts and immediate
environment
1. Report to local health authorities.
2. Isolation: for pulmonary tuberculosis, control of infectivity is
most efficiently achieved through drug therapy which lead to disappearance
of vital organism in the sputum in 2-4 weeks and full clearance of sputum
within 4-8 weeks.
Indications of hospitalization in TB include the following:
a. Complications of pulmonary tuberculosis eg. Pleural effusion and
pneumothorax.
b. Complications of treatment, e.g., severe reactions like drug intolerance,
hypersensitivity reactions, hepatitis, etc.
c. Concomitant diseases, e.g., uncontrolled DM.
d. Psychosocial problems, e.g., alcoholics, drug addicts, previous defaulters.
e. Difficulty in attending clinics for DOTs, e.g., elderly, hemiplegic, living in
remote areas, etc.
f. Extra pulmonary TB for special investigation.
3.Concurrent disinfection: Hand washing and good house keeping
practice should be maintained with decontamination of air by
ventilation ,filtration and ultraviolet light.
4. Quarantine: for drug resistant TB ( MDR-TB and XDR-TB ).
5. Management and investigation of contacts and source of infection:
Investigation of exposed contacts is recommended at time of diagnosis
by tuberculin skin test with clinical evaluation and chest x-ray for those
with tuberculin test positive. In developing countries investigation of
contacts is depend on sputum microscopy for those contacts with
clinical manifestation suggest TB.
6. Specific treatment: by DOTS regimen which describe previously.
Epidemic measures:
a. Diagnosis and treatment of each person with contagious TB disease.
b. Active case finding for secondary cases among contacts with
appropriate treatment.

