
Hypertensive Disorders of
Pregnancy
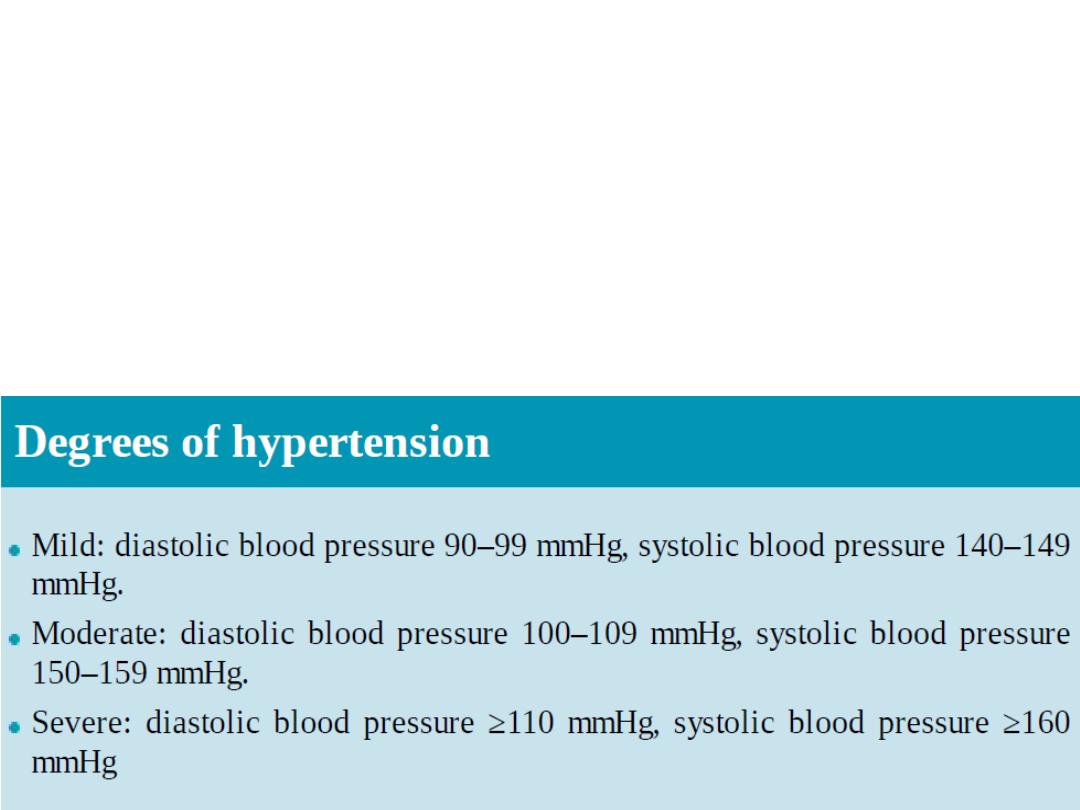
Hypertension:
•
One measurement of diastolic BP of 110
mmHg or more; or
• Two consecutive measurements of diastolic BP
of ≥ 90 mmHg 4 hours or more apart.
proteinuria:
• One 24-h urine collection with a total protein
excretion of 300 mg or more; or
• Two random clean-catch urine specimen with
a 1+ or more on reagent strip
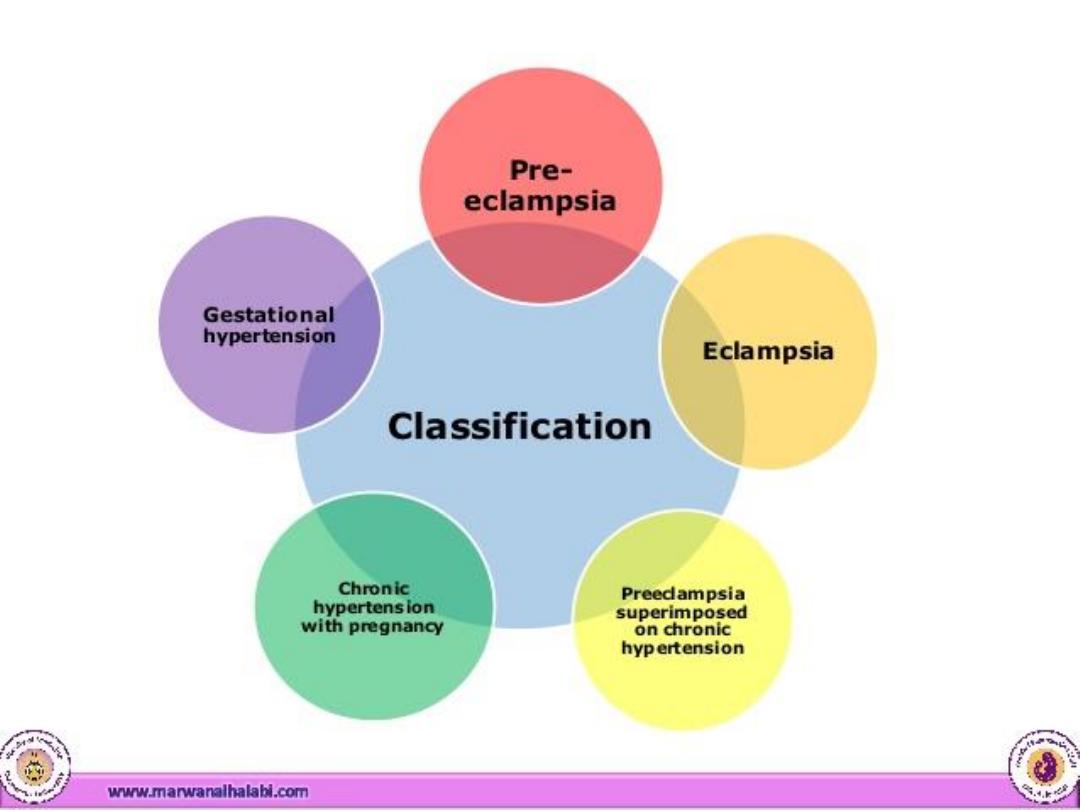

Pre-eclampsia
• hypertension + proteinuria after 20th week of
gestation in a previously normotensive
woman & resolving completely by the 6th
postpartum week.
• Eclampsia: tonic-clonic convulsion with
established pre-eclampsia, in the absence of
any other neurological or metabolic cause.

• non-proteinuric gestational HT: arising in the
second half of pregnancy without proteinuria.
• Chronic hypertension: prior to, in the first half of,
or persisting more than 6 weeks after pregnancy.
• superimposed pre-eclampsia: in the presence of
chronic hypertension, associated with a
worsening of the hypertension & the
development, or worsening of proteinuria.

Incidence of PE: 3-5 % of pregnancies
Risk Factors:
•
Antiphospholipid syndrome
•
Previuos Hx of PE
•
Family Hx : 3-4 fold increase risk
•
conditions in which the placenta is enlarged
•
pre-existing hypertension or renal disease.
•
pre-existing vascular disease (as in diabetes or
autoimmune vasculitis
•
Raised BMI
•
Age over 40
•
Raised diastolic BP > 80 mmHg

Aetiology:
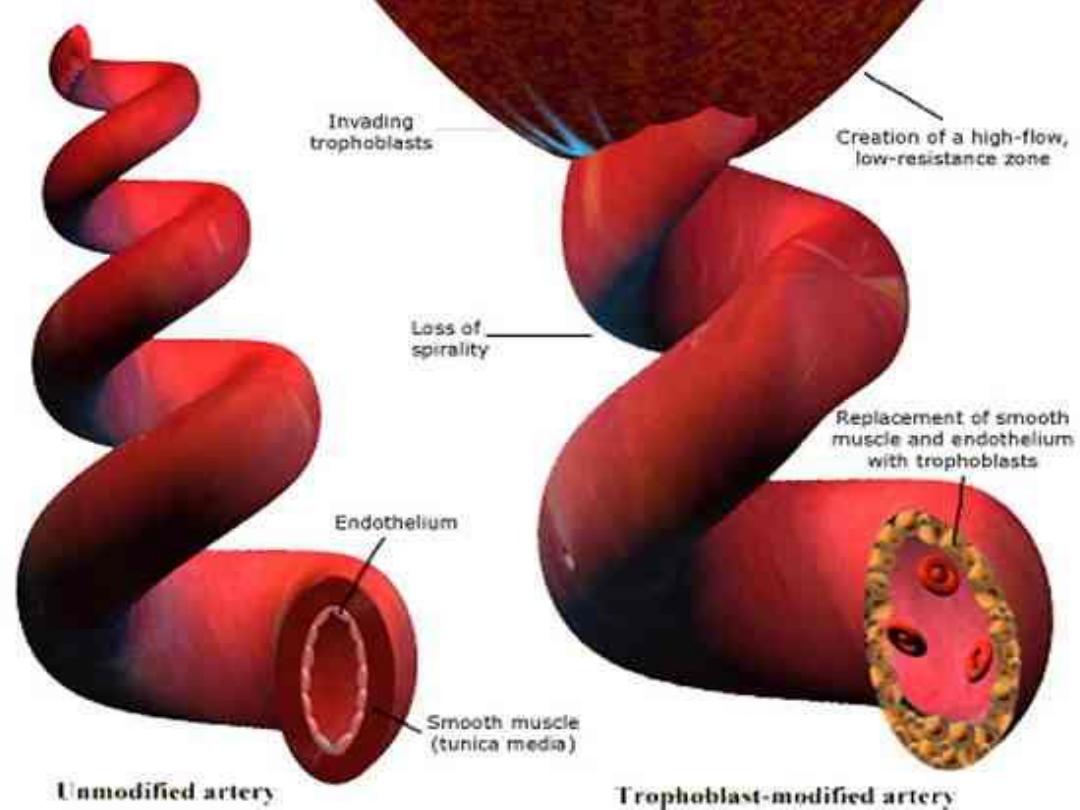
• normal pregnancy: the cytotrophoblast invade the
spiral arteries lead to dilatation & increased
intervillous blood flow.
• pre-eclampsia: trophoblast invasion is patchy & the
spiral arteries retain their muscular walls
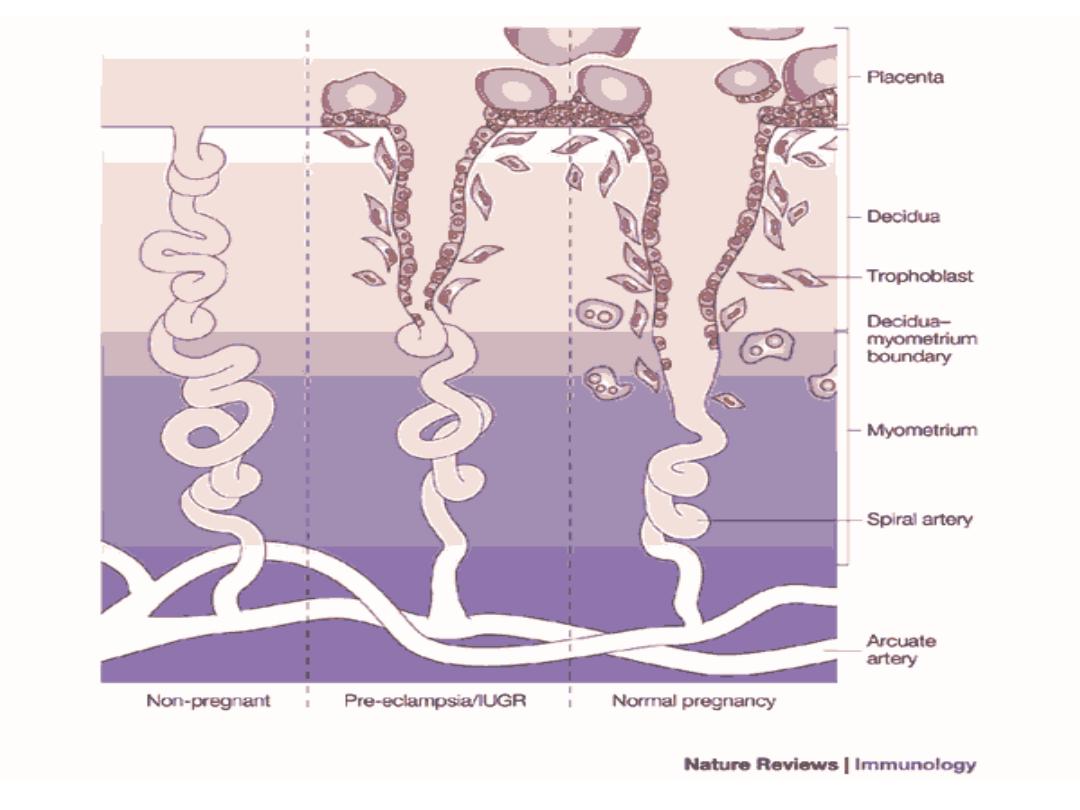
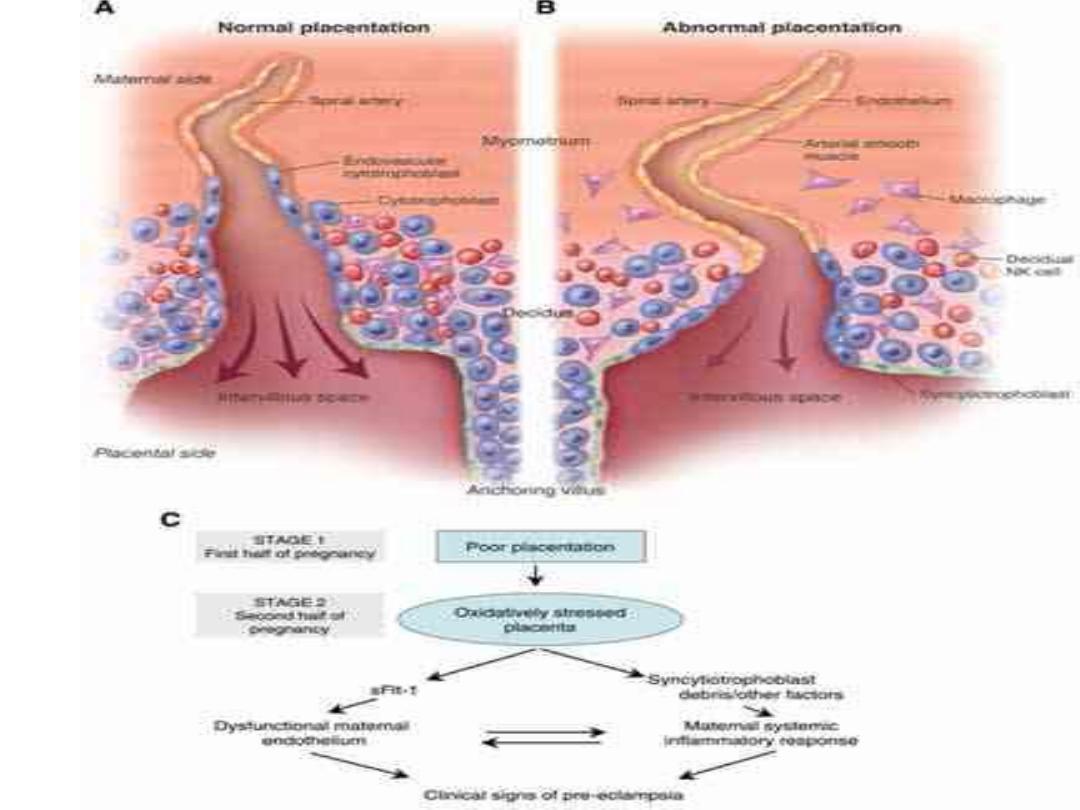

• Impaired perfusion of placenta & ischaemia
result in production of reactive oxygen species
& a condition of oxidative stress
• Placenta release certain factors (adhesion
molecules, von-Willebrand factor) into the
maternal circulation which target the vascular
endothelium & cause dysfunction.

Normal pregnancy:
• peripheral vasodilatation is accomplished
through a reduced vascular sensitivity to
vasoconstrictors such as angiotensin.
In pre-eclampsia the insensitivity to
vasoconstrictors is lost.
• Vasospasm & endothelial cell dysfunction,
with subsequent platelet activation & micro-
aggregate formation.
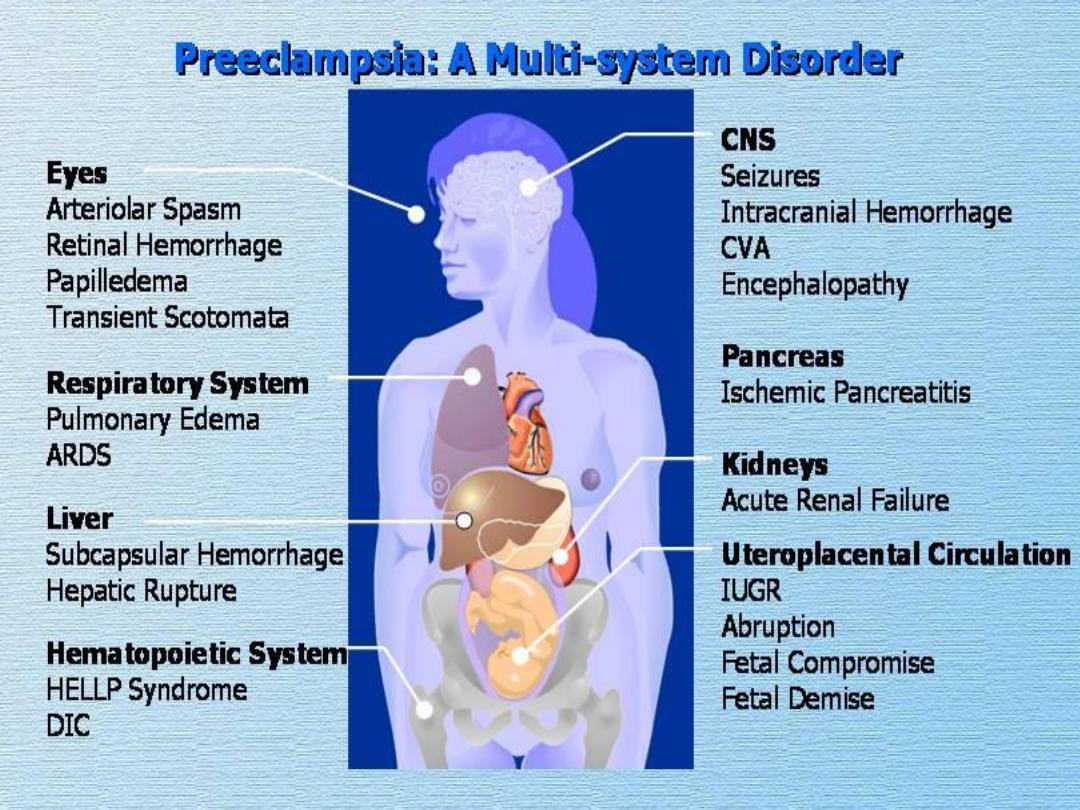
SYSTEMIC EFFECTS:
• Cardiovascular:
Generalized vasospasm
Increased peripheral resistance
• Haematological:
Platelet activation & depletion
Coagulopathy
Decreased plasma volume
Increased blood viscosity

• Renal:
Proteinuria
Decreased glomerular filtration rate
Decreased urate excretion
• Hepatic:
Periportal necrosis
Subcapsular haematoma
• Central nervous system:
Cerebral oedema
Cerebral haemorrhage

Symptoms of pre-eclampsia:
• asymptomatic
• Headache
• vomiting
• Visual disturbance
• Epigastric & right upper abdominal pain
Signs of pre-eclampsia:
• Elevation of blood pressure
• Fluid retention ( non-dependant oedema)
• Ankle clonus (more than three beats)
• Uterus & fetus may feel small for gestational age
Prevention:
Screening tests:
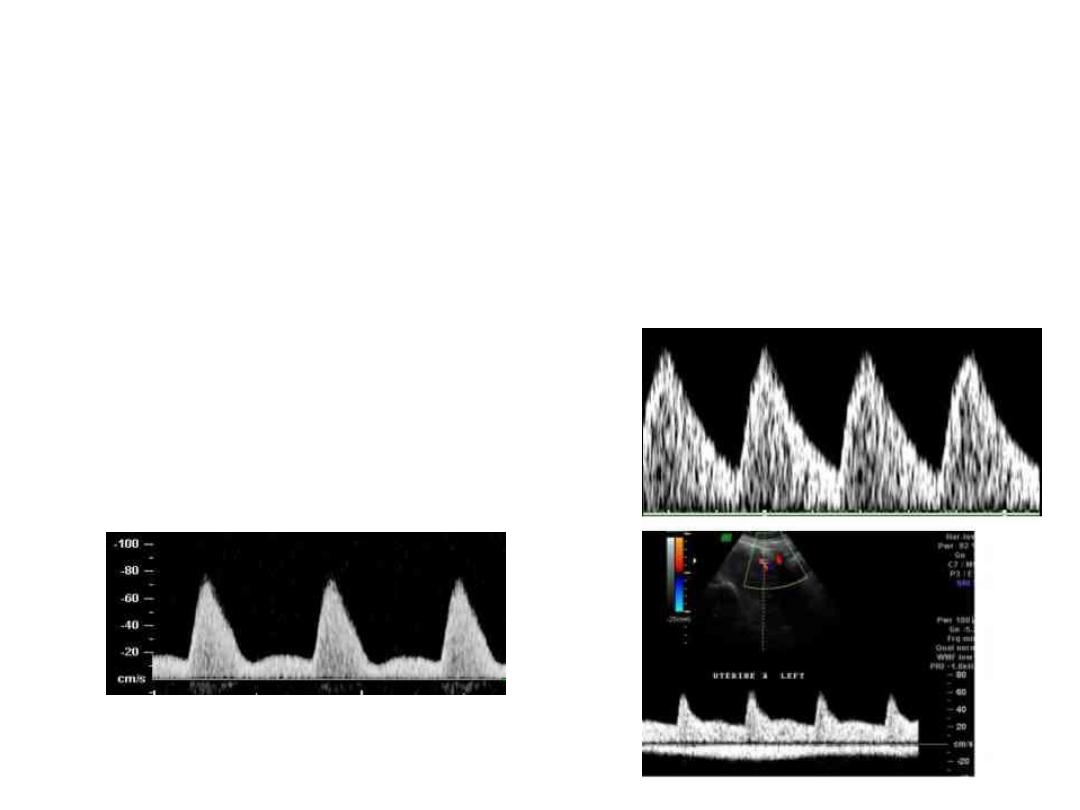
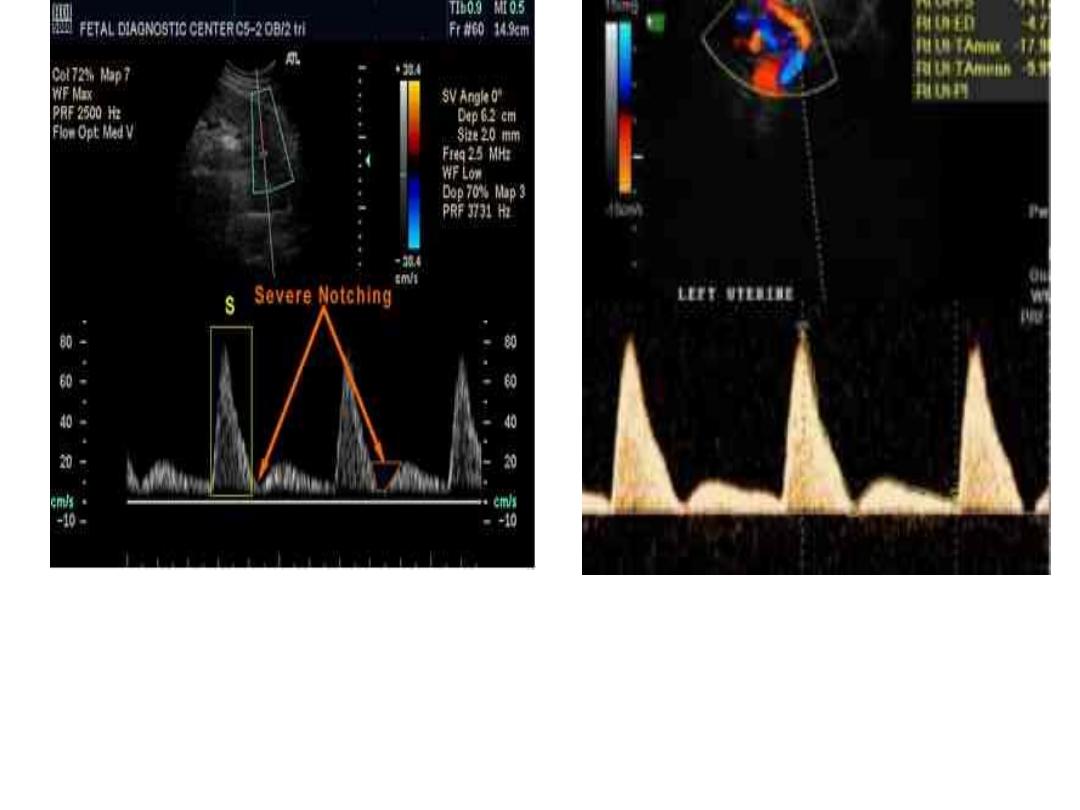
• Doppler ultrasound of the uterine artery
waveform analysis
• a characteristic 'notch' can be seen in the
waveform pattern.
The most commonly used preventive therapy
is low-dose aspirin (75 mg daily) started at 13
weeks of gestation.

Management:
Assess severity
• Urinalysis by dipstick
• 24-hour urine collection ( total protein & creatinine
clearance)
• Full blood count
• Blood chemistry ( renal function, protein
concentration)
• Plasma urate concentration
• Liver function
• Coagulation profile
• Ultrasound assessment:
– Fetal size
– amniotic fluid volume
– fetal Doppler
• Mild PE: diastolic BP 90-109 out patient management (after
assassment in day care unit) & frequent monitoring
• Severe PE: admission

Criteria of severe pre-eclampsia are:
• BP of ≥ 160 mmHg systolic or ≥ 110 mmHg
diastolic on at least two occasions at least 6 h
apart with patient at rest.
• Proteinuria of ≥ 5 g per 24 h.
• Oliguria ( ≤ 400 ml in 24 h ).
• Cerebral or visual disturbance.
• Epigastric pain.
• Pulmonary oedema or cyanosis.
• Impaired liver function.
• Thrombocytopenia

• The mainstay of treatment of PE is by termination of
pregnancy by delivering the fetus & the placenta.
For those who are remote from term :
• Corticosteroids are administered to accelerate lung
maturity for fetuses between 24 and 34 weeks
gestation

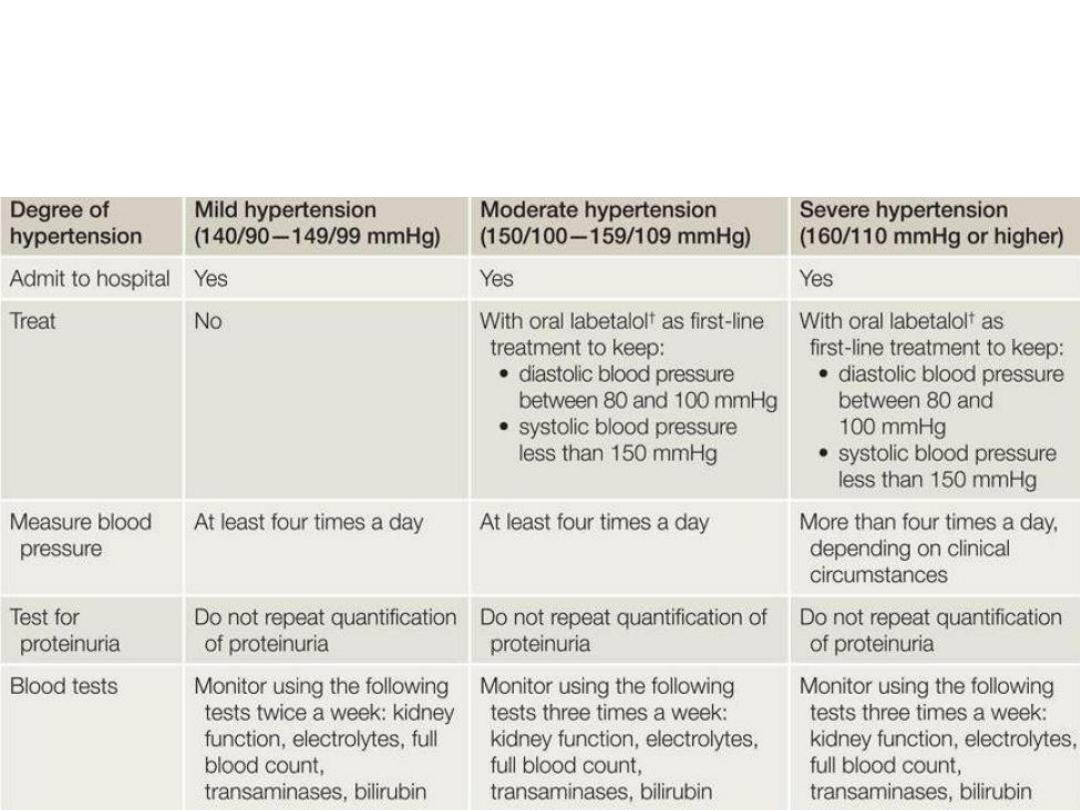
• Anti-hypertensives: for those with diastolic BP
≥100 & systolic ≥150
The aim of antihypertensive therapy is to lower
blood pressure & reduce the risk of maternal
cerebrovascular accident without reducing
uterine blood flow & compromising the fetus.

Types of Antihypertensives:
• Labetolol: alpha & beta- blocking agent
• Methyldopa: centrally acting antihypertensive
agent, takes up to 24 hours to take effect.
• Nifedipine: calcium channel blocker with a
rapid onset of action.
• Hydralazine: arterial vasodilator, used in
emergency situation for rapid control.

Management of labour & delivery
• expectant management should be
continued to 37-38 weeks gestation

Indication for preterm delivery are:
• severe uncontrolled hypertension ( ≥ 160/110
mmHg)
• haemolysis with thrombocytopenia &
elevated ALT
• progressive symptoms (headache, visual
disturbance, epigastric pain)
• pulmonary oedema
• renal compromise with oliguria
• eclampsia
• fetal distress

• The mode of delivery is determined by
gestational age, the state of the cervix & fetal
condition
• Prolonged pushing should be avoided
• ergometrine should not be used
• Fluid management is important in severe PE: 1
litre Ringer lactate / 12 h).
• diuretics should be confined to women with
pulmonary oedema

Postnatal councelling
• The risk of recurrence is increased with
increased severity of PE.
• increased risk of death from cardiovascular
disease in the future particularly in those who
remain hypertensive in the puerperium.
