Pre-labour rupture of membranes (PROM), or premature
rupture of membranes:
when there is
occurs
is a condition that
It
more than
and
one hour before the onset of
It is considered prolonged when it occurs more than 18
hours before labour.
PROM is preterm when it occurs before 37 weeks
gestation, and is called Preterm Premature Rupture of
Membranes (or PPROM).
.
– Incidence:PPROM complicates only 2% of
pregnancies.
• Approximately, 8-10% of term pregnancies
will experience spontaneous PPROM prior to
the onset of uterine activity

• Complications of PROM :
• Preterm Labour:It is associated with 40% of preterm
deliveries and can result in significant neonatal
morbidity and mortality.
• The three causes of neonatal death associated with
PPROM are; prematurity,
• sepsis;
• and pulmonary hypoplasia.
• Women with intrauterine infection deliver earlier than
non-infected women and infants born with sepsis have
a mortality four times higher than those without sepsis.

• chorio-amnionitis:
• It’s maternal and foetal infection, it is the
second major complication of PPROM,it
complicates 10-36% of PPROM.
• There are maternal risks associated with
chorio-amnionitis.
• Early and accurate diagnosis is necessary to
appropriately manage patients with PROM .
• Potter Syndrome: (extreme flexion and
wrinkling of the skin.

• Aetiology and Risk factors:
• Risk factors for PROM include:
• 1- Intra-amniotic infection :
• There is evidence demonstrating an association
between ascending infection from the lower genital
tract and PPROM.
• In patients with PPROM, about one-third of
pregnancies have positive amniotic fluid cultures and
Current evidence suggests that infection is a cause
rather than a consequence of amniorrhexis.

• 2- decidual haemorrhage (placental abruption):
• occurring remote from term, may release proteases
into the chorio-decidual tissues and amniotic fluid,
leading to rupture of membranes, placental abruption
is seen in 4-12% of pregnancies complicated by PPROM,
and is more common in pregnancies prior to 28 weeks
of gestation.
• However, whether it is the cause of PPROM or a
consequence of acute uterine decompression is not
known.

• 3- Obstetrical invasive procedures performed during
pregnancy (such as amniocentesis, cordocentesis,
chorionic villous sampling, fetoscopy, and cervical
cerclage) can damage the membranes, causing them to
leak, but these are rare causes of PPROM.
• 4- bacterial infection.
• 5- smoking.
• 6- anatomic defect in the structure of the amniotic sac,
uterus, or cervix.

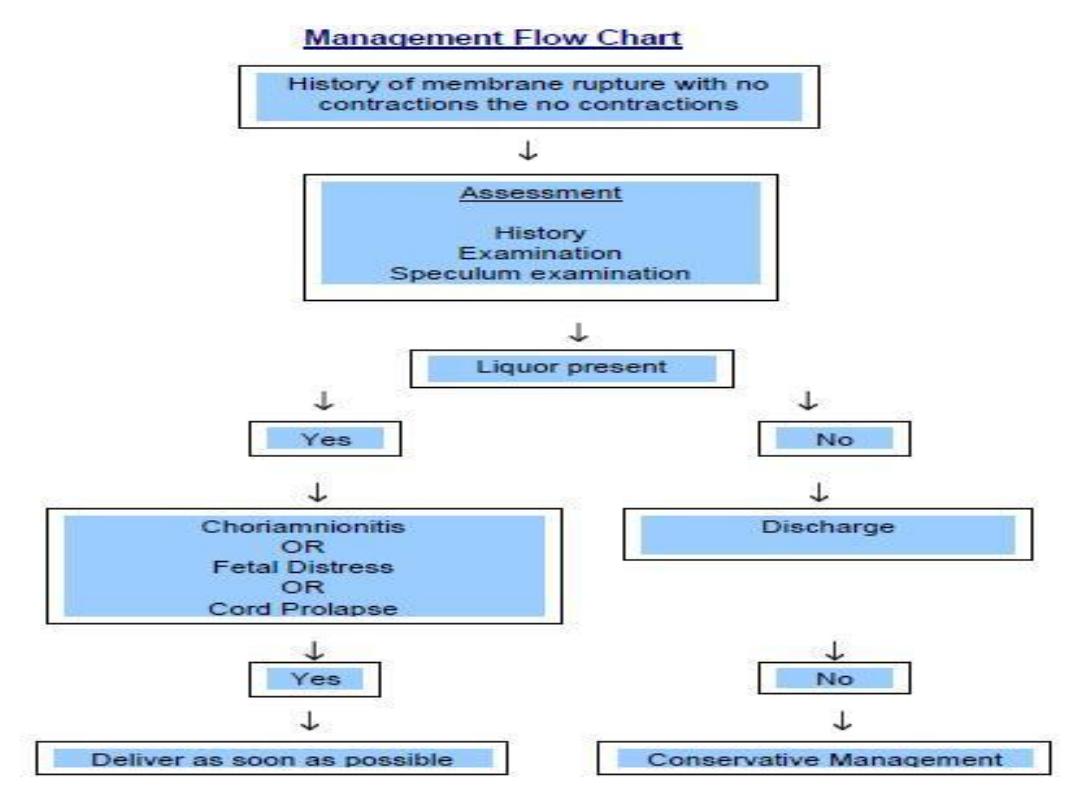
• Management of PPROM:
• Diagnosis:
• The initial evaluation of premature preterm rupture of
membranes is the diagnosis which include :
• History:
• Rupture of the membranes typically presents as a large
gush of clear vaginal fluid or as a steady trickle. Clinical
diagnosis may be easy when patients are presenting
with heavy watery vaginal discharge or when clear
fluid can be seen leaking from the cervical os.
• In 47% of the cases, clinicians are uncertain regarding
the diagnosis based on clinical examination by sterile
speculum examination and patient history alone .

• Diagnosis is difficult when leakage of fluid is tiny
and/or intermittent and/or ultrasound examination
shows a normal to low index of amniotic fluid. In these
cases, non-invasive biochemical tests can help in
diagnosis.
• Risk factors.
• The criteria for the diagnosis of clinical
chorioamnionitis include maternal pyrexia,
tachycardia,leucocytosis,uterine tenderness, offensive
vaginal discharge and foetal tachycardia

• PHYSICAL EXAM.:
• . Maternal vital signs should be documented.
• Obstetrical exam. Fundal height, the lie and the
presenting part.
• . Cardiotocography is useful continuous foetal
monitoring initially to establish foetal status and
foetal tachycardia is used in clinical chorio-
amnionitis.
• . Digital examination should be avoided, it shorten
latency and increase risk of infections
.

• a sterile speculum examination to document ROM.
The presence of a pool of fluid in the vagina at
speculum examination is suggestive of
amniorrhexis.
• Cervical cultures including
Chlamydia trachomatis
and
Neisseria gonorrhoeae
and ano-vaginal cultures
for
Streptococcus agalactiae
should be obtained
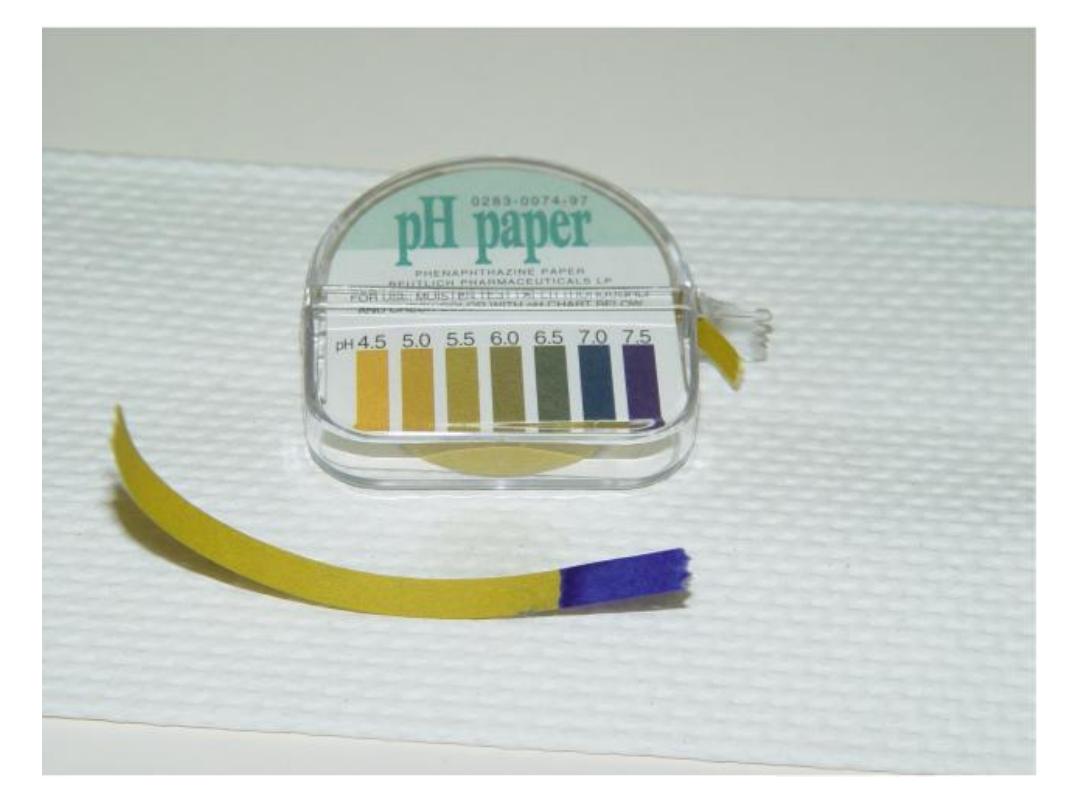
• Nitrazine test: represented by an alkaline pH of the
cervico-vaginal discharge demonstrated by seeing
the paper’s colour turns from yellow to blue .

.
microscopic examination of the vaginal fluid for the
characteristic ferning of the crystalline pattern of dried
amniotic fluid owing to its sodium chloride and protein
content.
Examination, for lanugo hair and foetal epithelial cells
stained with Nile blue.
• the absorbent pad (AmnioSense). This 12 cm × 4 cm pad
has a central strip that changes colour with fluid with a pH
>5.2.
• Ultra-sound, should be performed to confirm gestational
age ,viability ,anomalies , estimated foetal weight,
presentation, amniotic fluid index.

• The differential diagnosis includes:
• leakage of urine (urinary incontinence).
• excessive vaginal discharge, such as physiologic discharge
• or bacterial vaginosis.
. cervical mucus (show) as a sign of impending labour.
After confirmation of the diagnosis:
-In PPROM, the rule should be hospitalization after viability
in an institution where care for a premature neonate can
be provided.

• Informed consent should be obtained for expectant
management versus delivery.
• Indications for Delivery:
• 1- Gestational age more than 34 weeks of
gestation.
• 2- Signs of chorio-amnionitis.
• 3- If the mother susceptible for infection:
• - Women on immunosuppressant drugs.
• - Women with rheumatic heart disease.
• - Diabetic patients .
• - If infected cerclage.
• - If pregnancy with IUCD and still in utero.

• 4- advanced labour,
• 5- foetal distress.
• 6- placental abruption with non-reassuring foetal
surveillance.
• 7- If foetal lung maturity has been documented by
either amniocentesis or collection of vaginal fluid,
delivery should be facilitated.
• 8- In a non-cephalic foetus with advanced cervical
dilatation (more than or equal to 3 cm), the risk of
cord prolapse may also outweigh the benefits of
expectant management and delivery should be
considered.
• 9-Intra uterine death and foetal anomalies.

Expectant Management of PPROM:
• If after initial evaluation of the mother and foetus, they
are both determined to be clinically stable, expectant
management of PPROM may be considered to improve
foetal outcome.
• The primary maternal risk with expectant management
of PPROM is infection. This includes:
• chorioamnionitis (13-60%),
• endometritis (2-13%),
• sepsis (< 1%).
• maternal death (1-2 cases per 1000).
• Complications related to the placenta include abruption
(4-12%) and retained placenta or postpartum
haemorrhage .

• The risks and potential benefits of expectant
management should be discussed with the
patient and her family, and informed consent
should be obtained.
• The maternal and foetal status need to be re-
evaluated daily, and the safety and potential
benefits of expectant management should be
reassessed.
• If the condition remains stable, the immature
foetus may benefit from expectant
management, even if for a short period, to allow
administration of steroids and antibiotics.

• Patients with PROM before 32 weeks' gestation should
be cared for expectantly until they have completed 33
weeks of gestation, provided there are no maternal or
foetal contraindications.
• Digital cervical examination should be avoided in
patients with PROM unless they are in active labour or
unless imminent delivery .
• Women with PROM before potential foetal viability
should be counselled about the impact of immediate
delivery and the risks and potential benefits of
expectant management
.

• To prolong pregnancy and to reduce infectious and
gestational age–dependent neonatal morbidity, :
• a 48-hour course of intravenous ampicillin and
erythromycin, followed by five days of amoxicillin and
erythromycin, is recommended .
• All women with PROM and a viable foetus, including
those who are known carriers of group B streptococcus
(GBS) or who deliver before their GBS status can be
determined, should receive intra-partum
chemoprophylaxis to prevent vertical transmission of
GBS.

• A single course of antenatal corticosteroids
should be given to women with PROM at 24 to
34 weeks' gestation to reduce the risk of
prenatal mortality, respiratory distress
syndrome, and other morbidities as, necrotizing
enterocolitis, and intraventricular haemorrhage
were all lower when either;
• 12 mg of betamethasone IM was given twice in
a 24-hour interval or;
• dexamethasone 6 mg q12h was given for 4
doses.

• If pulmonary immaturity is documented, corticosteroid
treatment at 32-33 weeks of completed gestation may
be beneficial.
• Corticosteroid use before foetal age of viability is not
recommended.
• magnesium sulphate for foetal neuro-protection should
be used with either a 4- or 6-g bolus and a maintenance
dose of 1-2 g.
• Tocolysis in women with PPROM is not recommended
because this treatment does
• not significantly improve peri-natal outcome.

The criteria for the diagnosis of clinical chorio-amnionitis
include;
• maternal pyrexia,tachycardia,uterine tenderness,fetal
tachycardia,offensive vaginal discharge and
leucocytosis.
• .During observation, the woman should be regularly
examined for signs of intrauterine infection and foetal
status.
• The frequency of maternal temperature, pulse and
foetal heart rate auscultation should be between every
4 and 8 hours.
• Treatment of chorio-amnionitis include broad
spectrum antibiotics and termination of pregnancy.

• Antibiotics:
• Bactericidal ,combined covering G +VE ,&G –VE and
parenteral route.
• Mode of Delivery, depends on Maternal and foetal
conditions which can be by induction of labour or
operative delivery according to:
• Maternal; obstetrical history, her G.A., complications
during pregnancy and maternal condition.
• Foetal presentation and foetal wellbeing ,any foetal
compromise, anomalies or foetal death.
