1
Respiratory diseases د. سرى سلمان عجام
Emphysema : -
Definition: is characterized by irreversible enlargement of the airspaces distal to the
terminal bronchiole, accompanied by destruction of their walls without obvious
fibrosis.
Incidence.
COPD is a major public health problem. It is the fourth leading cause of morbidity
and mortality in the United States
Types of emphysema:-
Emphysema is classified according to its anatomic distribution within the lobule.
Recall that the lobule is a cluster of acini, the terminal respiratory units
there are four major types: (1) centriacinar, (2) panacinar, (3) paraseptal, and (4)
irregular. Of these, only the first two cause clinically significant airflow obstruction
. Centriacinar emphysema is far more common than the panacinar form,
constituting more than 95% of cases.
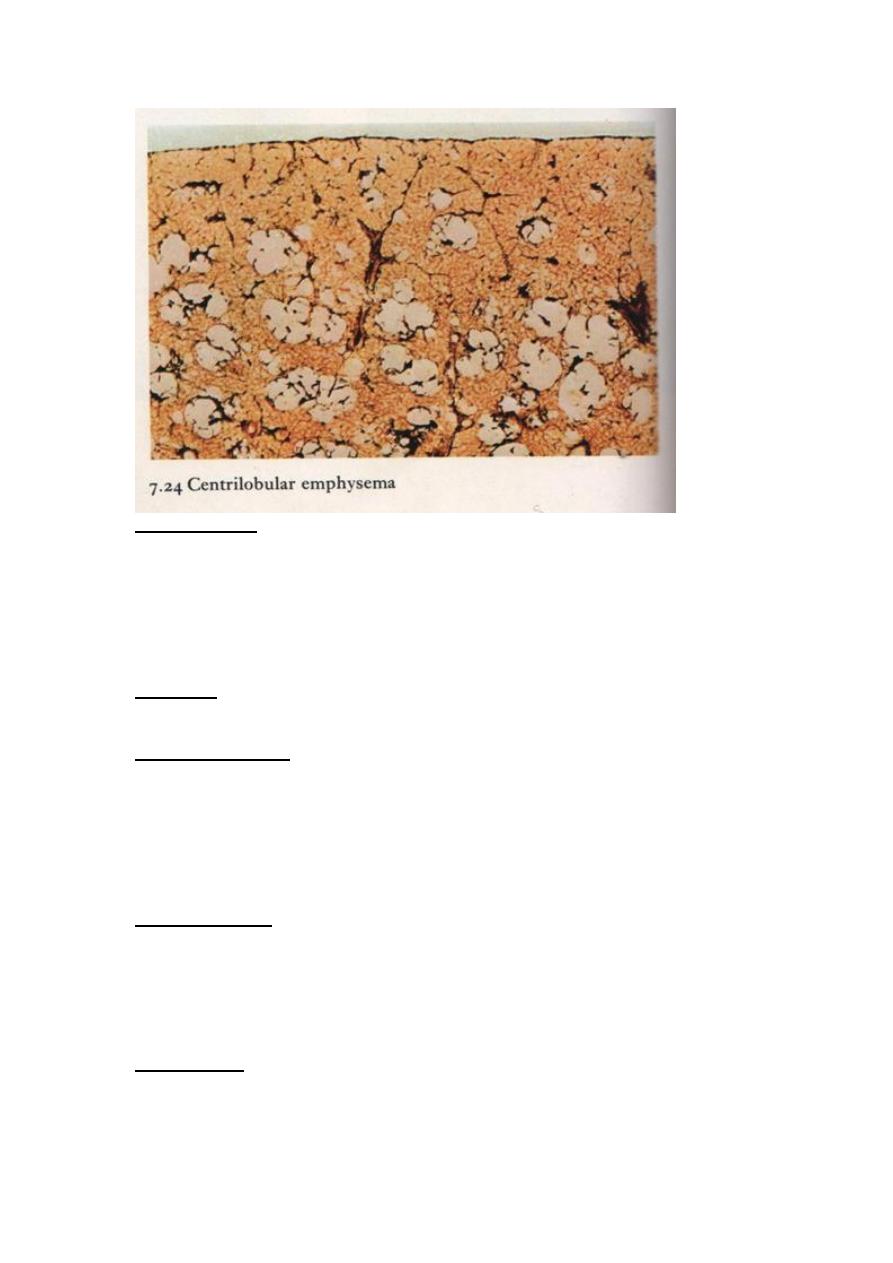
1- centriacinar ( centrlobular) emphysema:
In which the central and proximal part of acinus are affected ( formed by respiratory
bronchioles )
The lesions are more sever and common in upper lobes particularly in apical airspaces
or segments . emphysematous spaces often contain large amounts of black pigment In
sever centriacinar emphysema , the distal acinus also becomes involved.
This type of emphysema is most commonly seen as a consequence of cigarette
smoking and often in association with chronic bronchitis.
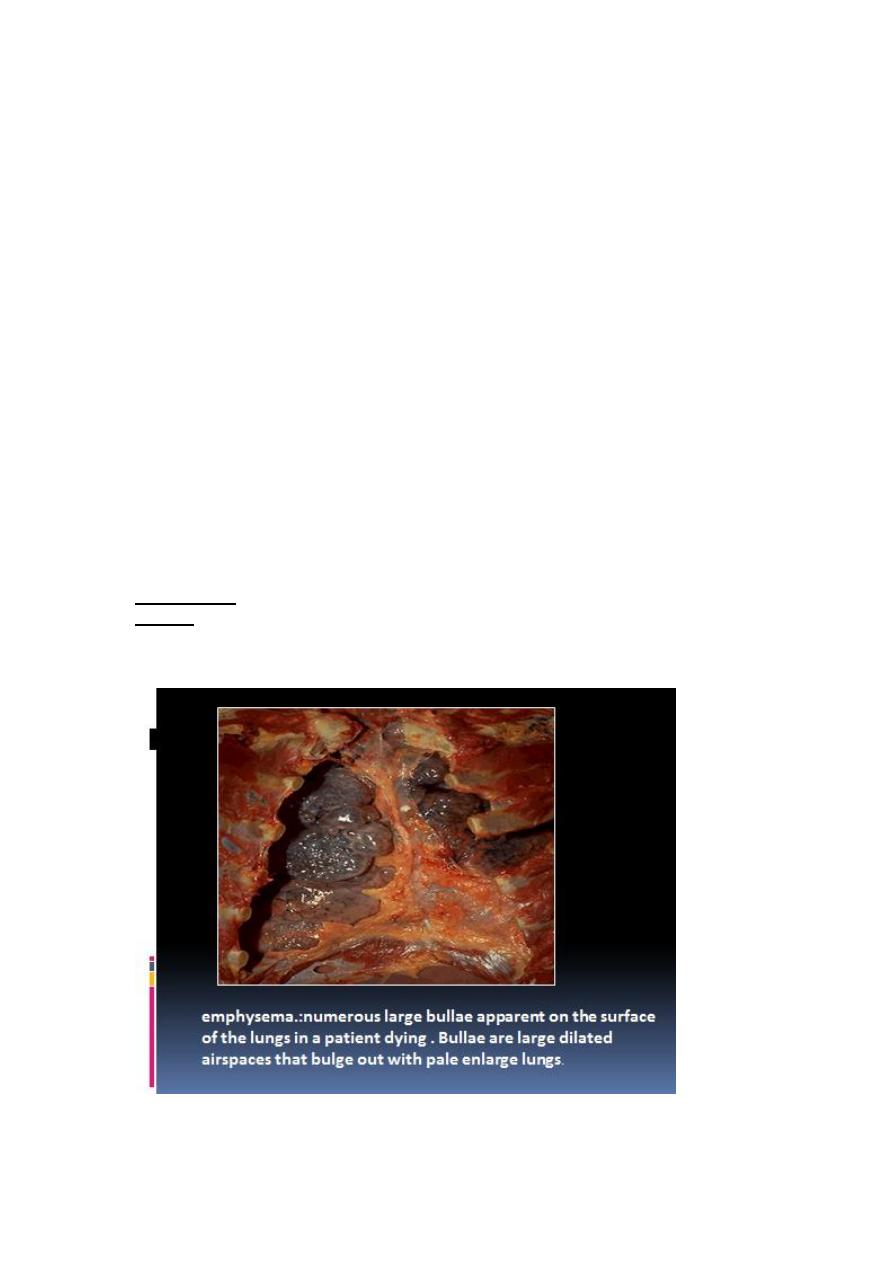
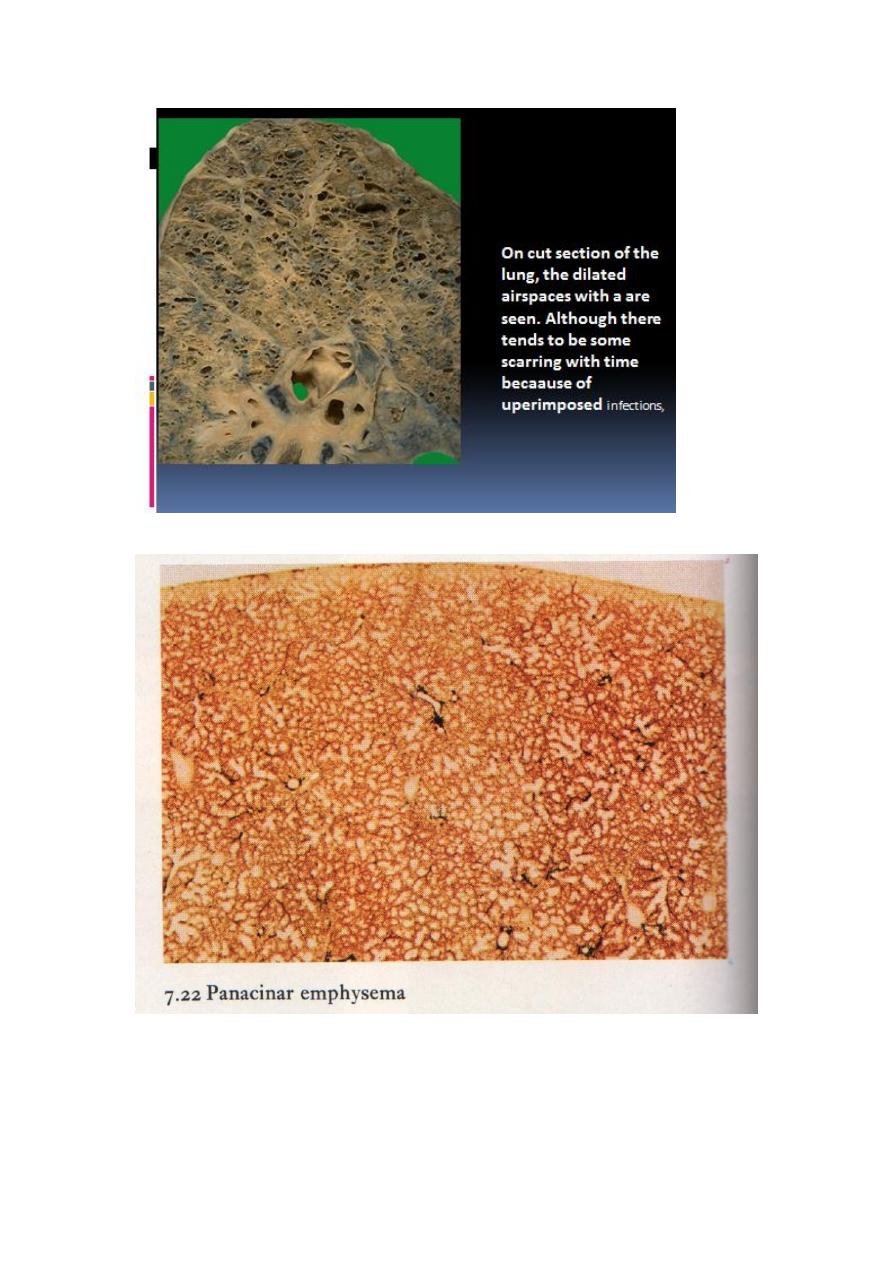
2- panacinar emphysema :
In this type of emphysema, the acini are uniformly enlarged from the level of the
respiratory bronchiole to the terminal blind alveoli
The prefix ―pan‖ refers to the entire acinus but not to the entire lung. In contrast to
centriacinar emphysema, panacinar emphysema tends to occur more commonly in the
lower zones and in the anterior margins of the lung, and it is usually most severe at
the bases
It tends to occur more commonly in the lower lung zones and is the type of
emphysema that occurs in α1-antitrypsin deficiency.
3- Distal Acinar ( paraseptal) Emphysema
In this form, the proximal portion of the acinus is normal but the distal part is
dominantly involved.
The emphysema is more striking adjacent to the pleural margin of the lobules. It
occurs adjacent to areas of fibrosis, scarring, or atelectasis and is usually more severe
in the upper half of the lung .
The characteristic findings are of multiple, continuous, enlarged airspaces from less
than 0.5 cm to more than 2.0 cm in diameter, sometimes forming cystlike structures.
2
This type of emphysema probably underlies many of the cases of spontaneous
pneumothorax in young adults.
4-Airspace Enlargement with Fibrosis (Irregular Emphysema)
Irregular emphysema, so named because the acinus is irregularly involved, is almost
invariably associated with scarring. Thus, it may be the most common form of
emphysema, because careful search of most lungs at autopsy shows one or more scars
from a healed inflammatory process. In most instances, these foci of irregular
emphysema are asymptomatic and clinically insignificant
Clinical Features:
1- Dyspnea is usually the first symptom. In patient with no "bronchitic" component ,
barrel-chest is a prominent feature . Because of dyspnea , there is adequate
oxygenation of Hb . and patient called ( pink puffers ).
2- in patient with underlying bronchitis , there are cough and wheezing with purulent
sputum with loss of dyspnea lead to hypoxia patient called blue bloaters
3- weight loss is common and may be so sever as to suggest a hidden malignancy and
the patient may die from:
1- respiratory failure
2- right sided heart failure.
Pathogenesis :
Emphysema arising as a consequence of two critical imbalances : protease -
antiprotease and oxidant – antioxidant imbalances.
The protease- antiprotease imbalance is the underlying cause of pulmonary
emphysema in patient with genetic deficiency of α1 – antitrypsin
.
α1 – antitrypsin normally present in serum , tissue fluids and macrophages is a major
inhibitor of protease (elastase) secreted by neutrophils during inflammation, α1-
antitrypsin is encoded by codominantly expressed genes on the proteinase inhibitor
(Pi) locus on chromosome 14. The Pi locus is extremely polymorphic, with many
different alleles. Most common is the normal (M) allele and the corresponding
phenotype. Approximately 0.012% of the US population is homozygous for the Z
allele, associated with markedly decreased serum levels of α1antitrypsin. More than
80% of these individuals develop symptomatic panacinar emphysema, which occurs
at an earlier age and with greater severity if the individual smokes. The following
sequence is postulated:
1. Neutrophils (the principal source of cellular proteases) are normally
sequestered in peripheral capillaries, including those in the lung, and a few
gain access to the alveolar spaces.
2. Any stimulus that increases either the number of leukocytes (neutrophils and
macrophages) in the lung or the release of their protease-containing granules
increases proteolytic activity.
3. With low levels of serum α1-antitrypsin, elastic tissue destruction is
unchecked and emphysema results.
3
In smoking:
1- the direct chemoattractant effect of nicotine and effect of reactive oxygen species in
smoke These activate the transcription factor NF-κB, which switches on genes that
encode TNF and chemokines, including IL-8. These, in turn, attract and activate
neutrophils. .
2-With accumulation of neutrophils which release their protease ( elastase ) leading to
tissue damage because of oxidative injury of smoking that lead to inactivation of α1 –
antitrypsin
3- smoking also enhances elastic activity in macrophage which is not inhibited by α1
– antitrypsin
4- the abundant reactive oxygen species will deplete the antioxidants tat are normally
present in the lung to keep oxidative damage to a minimum thereby inciting tissue
damage.
the loss of elastic tissue in the walls of alveoli that surround respiratory bronchioles
reduces radial traction and thus causes the respiratory bronchioles to collapse during
expiration.
In addition the air way obstruction can be caused by
• goblet cell hyperplasia & mucus plug
• inflammatory edema
• muscle hypertrophy
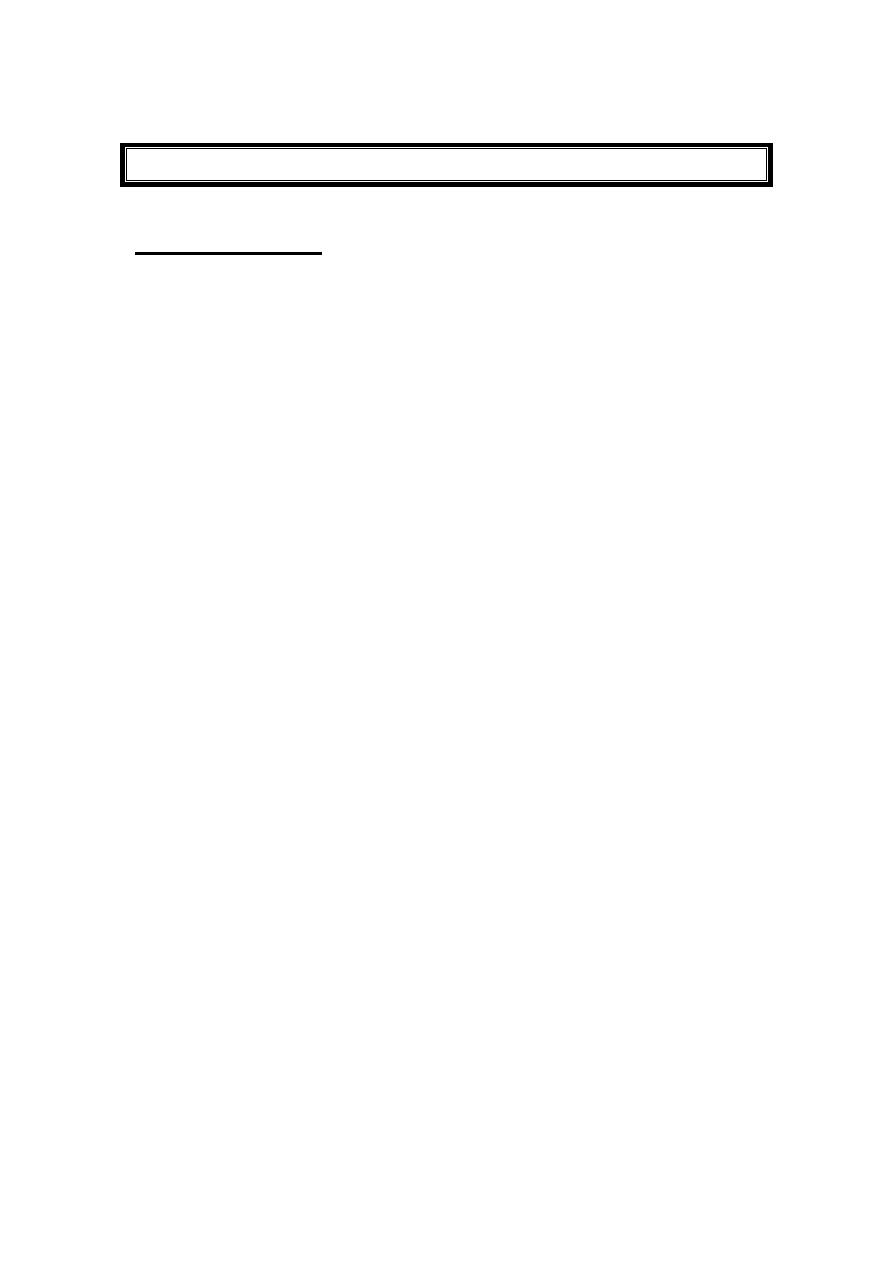
Morphology:
Grossly : the lung in panacinar emphysema when well developed , appears pale,
voluminous , and obscure the heart when anterior chest wall removed at autopsy.
In centriacinar emphysema , the lungs are deeper pink and less voluminous .
In extreme cases, emphysematous bullae may be visible .
4
5
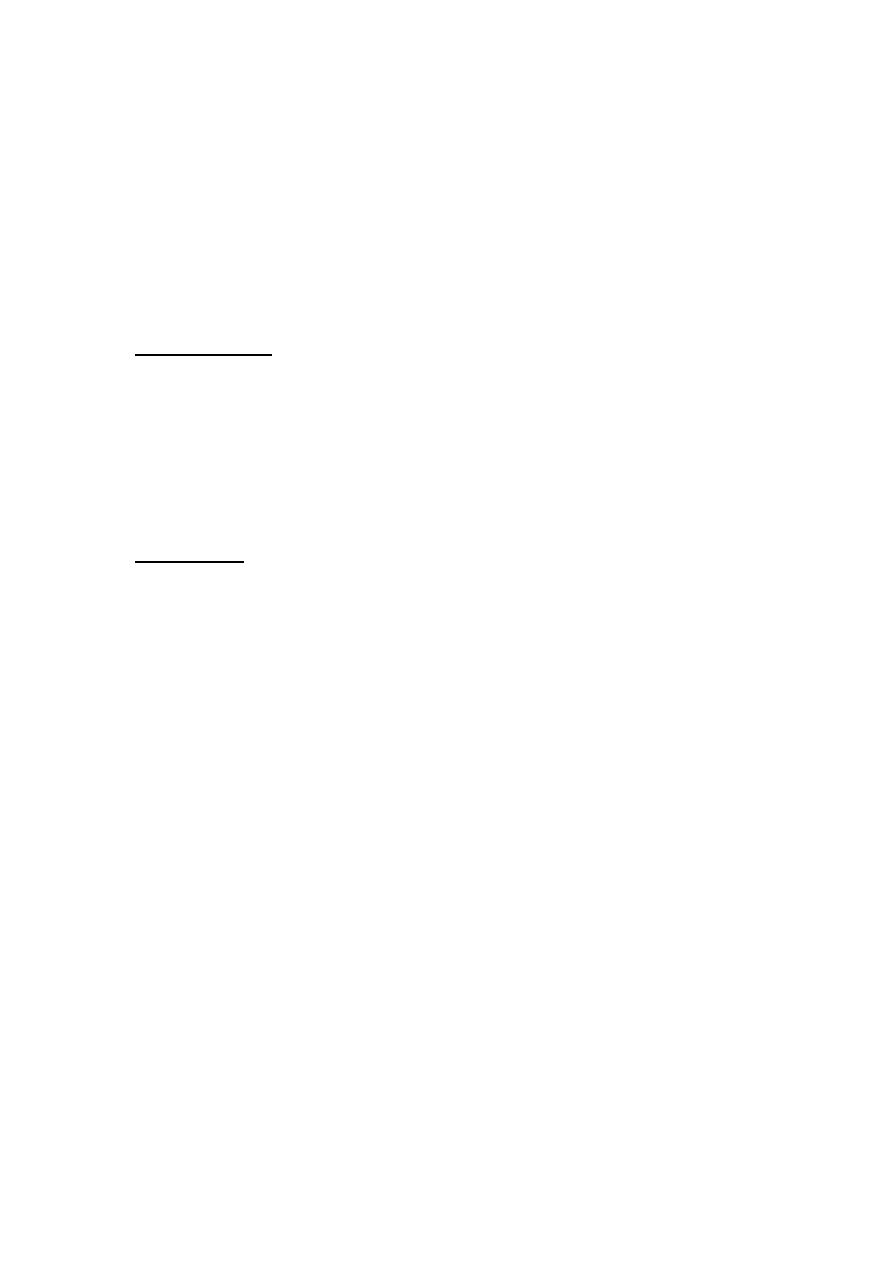
Microscopically :
1- there is thinning and destruction of alveolar walls. with advanced disease , adjacent
alveoli become confluent creating large airspaces.
2- terminal bronchi and bronchioles may be deformed because of loss of septa that
help tether those structure in parenchyma .
There is also fibrosis of bronchioles with evidence of bronchitis and bronchiolitis .
Inflammatory changes in small airways were described earlier
Treatment options include bronchodilators, steroids, bullectomy, and, in selected
patients, lung volume reduction surgery and lung transplantation. Substitution therapy
with α
1
-AT is being evaluated
Chronic bronchitis :
Definition : - is persistent productive cough for at least 3 consecutive months in at
least 2 consecutive years , in the absence of any other identifiable cause.
It is common in cigarette smokers and people who expose to air pollutants , such as
sulfur dioxide and nitrogen dioxide .
When persistent for years, it may (1) progress to COPD, (2) lead to cor pulmonale and
heart failure, or (3) cause atypical metaplasia and dysplasia of the respiratory
epithelium, providing a rich soil for cancerous transformation
Clinical features :
1- prominent cough and production of sputum may persist without ventilator
dysfunction and some patients may progress to chronic obstructive disease with
hypoxemia and cyanosis .
2- chronic bronchitis is complicated by recurrent infection , pulmonary hypertension
and cardiac failure .
Pathogenesis :
The primary or initiating factor in the genesis of chronic bronchitis seems to be long-
standing irritation by inhaled substances such as tobacco smoke (90% of patients are

6
smokers), and dust from grain, cotton, and silica. The earliest feature of chronic
bronchitis is hypersecretion of mucus in the large airways, associated with
hypertrophy of the submucosal glands in the trachea and bronchi.
[24]
Proteases
released from neutrophils, such as neutrophil elastase and cathepsin, and matrix
metalloproteinases, stimulate this mucus hypersecretion. As chronic bronchitis
persists, there is also a marked increase in goblet cells of small airways—small
bronchi and bronchioles—leading to excessive mucus production that contributes to
airway obstruction. It is thought that both the submucosal gland hypertrophy and the
increase in goblet cells are protective metaplastic reactions against tobacco smoke or
other pollutants (e.g., sulfur dioxide and nitrogen dioxide).
The role of infection seems to be secondary. It is not responsible for the initiation of
chronic bronchitis but is probably significant in maintaining it and may be critical in
producing acute exacerbations. Cigarette smoke predisposes to infection in more than
one way.
1-It interferes with ciliary action of the respiratory epithelium, it may cause direct
damage to airway epithelium,
2- it inhibits the ability of bronchial and alveolar leukocytes to clear bacteria.
Viral infections can also cause exacerbations of chronic bronchitis.
Morphollogy : -
Grossly : the mucosal lining of larger airways is usually hyperemic and swollen and
edema fluid . It is often covered by a layer if mucopurulent sputum.
Microscopically:
1- trachea and larger bronchi:
A. the major change is in the size of the mucous gland (hyperplasia).
This increase can be assessed by the ratio of the thickness of the mucous
gland layer to the thickness of the wall between the epithelium and the
cartilage (Reid index). The Reid index (normally 0.4) is increased in
chronic bronchitis, usually in proportion to the severity and duration of
the disease.
B. Increase umber of goblet cells in lining epithelium with concomitant loss
of ciliated epithelial cells .
C. Squamous metaplasia frequently develops followed by dysplastic
changes. A sequence of events that may lead to evolution of
bronchogenic carcinoma.
D. A variable density of inflammatory cells largely mononuclear but
sometimes admixed with neutrophils is frequently present in the
bronchial mucosa , the tissue neutrophilia increases during bronchitic
exacerbations. Unlike asthma , eosinophils don not constitute prominent
component except in patient with asthmatic bronchitis.
2- bronchioles:
A. Goblet cell metaplasia
B. Inflammation
C. Fibrosis
Smooth muscle hyperplasia.
.
D

7
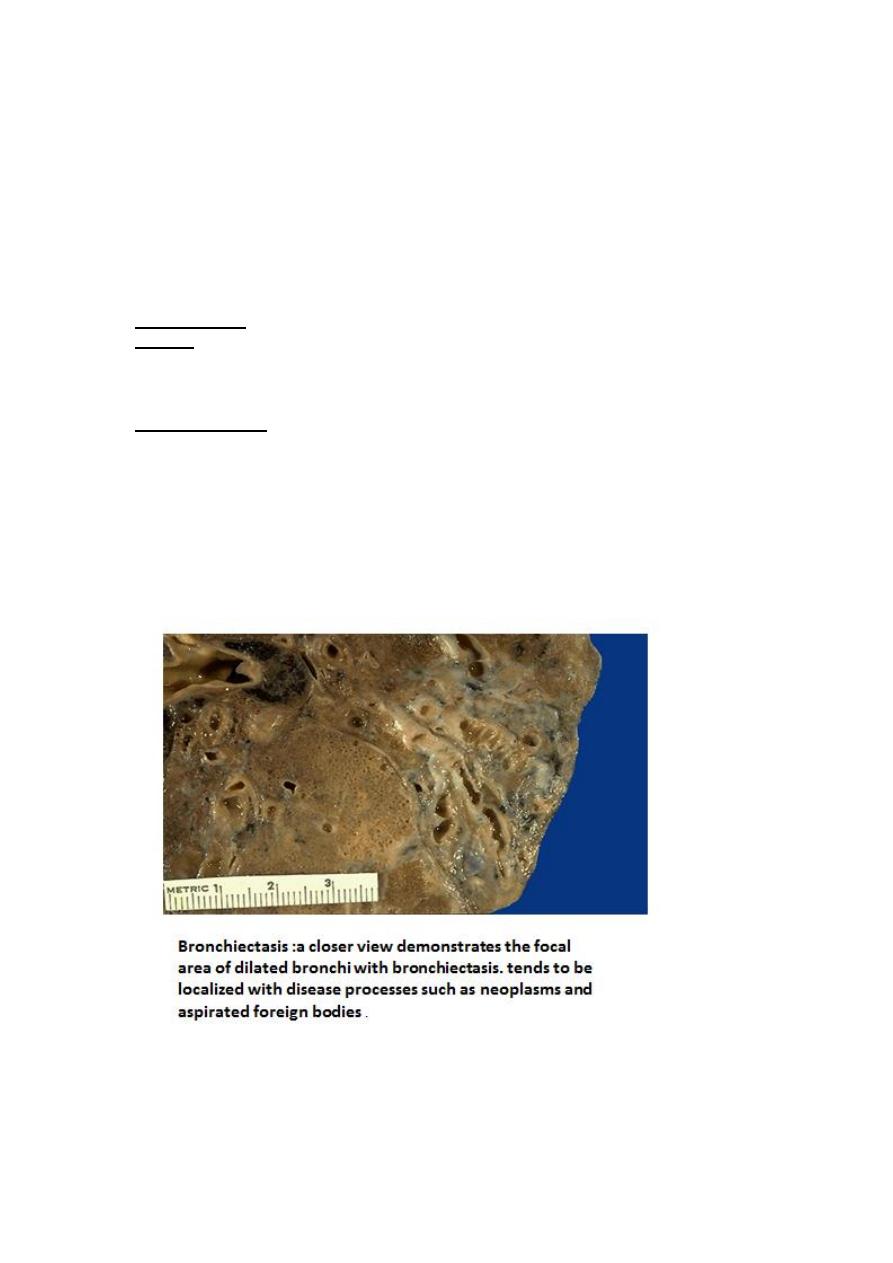
Bronchiectasis :–
Definition: is the permanent dilation of bronchi and bronchioles caused by destruction
of muscle and supporting elastic tissue resulting from or associated with chronic
necrotizing infections. It is not a primary disease but rather is secondary to persisting
infection or obstruction caused by variety of conditions.
The condition that most commonly predispose to bronchiectasis include the
following:
1- Bronchial obstruction:
Common causes are tumors, foreign bodies, and
occasionally impaction of mucus. Under these conditions, the bronchiectasis is
localized to the obstructed lung segment. Bronchiectasis can also complicate atopic
asthma
2- congenital or hereditary conditions
:
A-cystic fibrosis the primary defect in ion transport leads to defective mucociliary
action, and accumulation of thick viscid secretions that obstruct the airways. This
leads to a marked susceptibility to bacterial infections, which further damage the
airways. With repeated infections there is widespread damage to airway walls, with
destruction of supporting smooth muscle and elastic tissue, fibrosis, and further
dilatation of bronchi. The smaller bronchioles become progressively obliterated as a
result of fibrosis (bronchiolitis obliterans).
B- In immunodeficiency states, particularly immunoglobulin deficiencies,
bronchiectasis is prone to develop because of an increased susceptibility to repeated
bacterial infections
C- Kartagener syndrome, an autosomal recessive disorder, is frequently associated
with bronchiectasis. Structural abnormalities of the cilia impair mucociliary clearance,
leading to persistent pulmonary infections.
(Kartagener syndrome ) ( bronchiectasis, sinusitis, dextrocardia and male sterility)
3- Postinfectious conditions
, including necrotizing pneumonia caused by
bacteria (Mycobacterium tuberculosis, Staphylococcus aureus, Haemophilus
influenzae,
Pseudomonas),
viruses
(adenovirus,
influenza
virus,
human
immunodeficiency virus [HIV]), and fungi (Aspergillus species)
Etiology and Pathogenesis
.
Obstruction and infection are the major conditions associated with bronchiectasis, and
it is likely that both are necessary for the development of full-fledged lesions,
although either may come first. After bronchial obstruction, normal clearing
mechanisms are impaired, there is pooling of secretions distal to the obstruction, and
there is inflammation of the airway. Conversely, severe infections of the bronchi lead
to inflammation, often with necrosis, fibrosis, and eventually dilation of airway
.
8
Clinical features
1- persistent cough with expectoration of mucopurulent sputum. The sputum may
contain flecks of blood; frank hemoptysis can occur.
2- clubbing of fingers.
3- hypoxemia , hypercapnia m pulmonary hypertension and core pulmonale.
4- metastatic brain abscesses and reactive amyloidosis are less frequent
complications.
Morphology :-
Grossly :- bronchiectatic involvement of lungs usually affects the lower lobes
bilaterally , particularly those air passages that are more vertical. The most sever
involvement is found in the more distal bronchi and bronchioles. The airways may be
dilated to as much as 4 times their usual diameter.
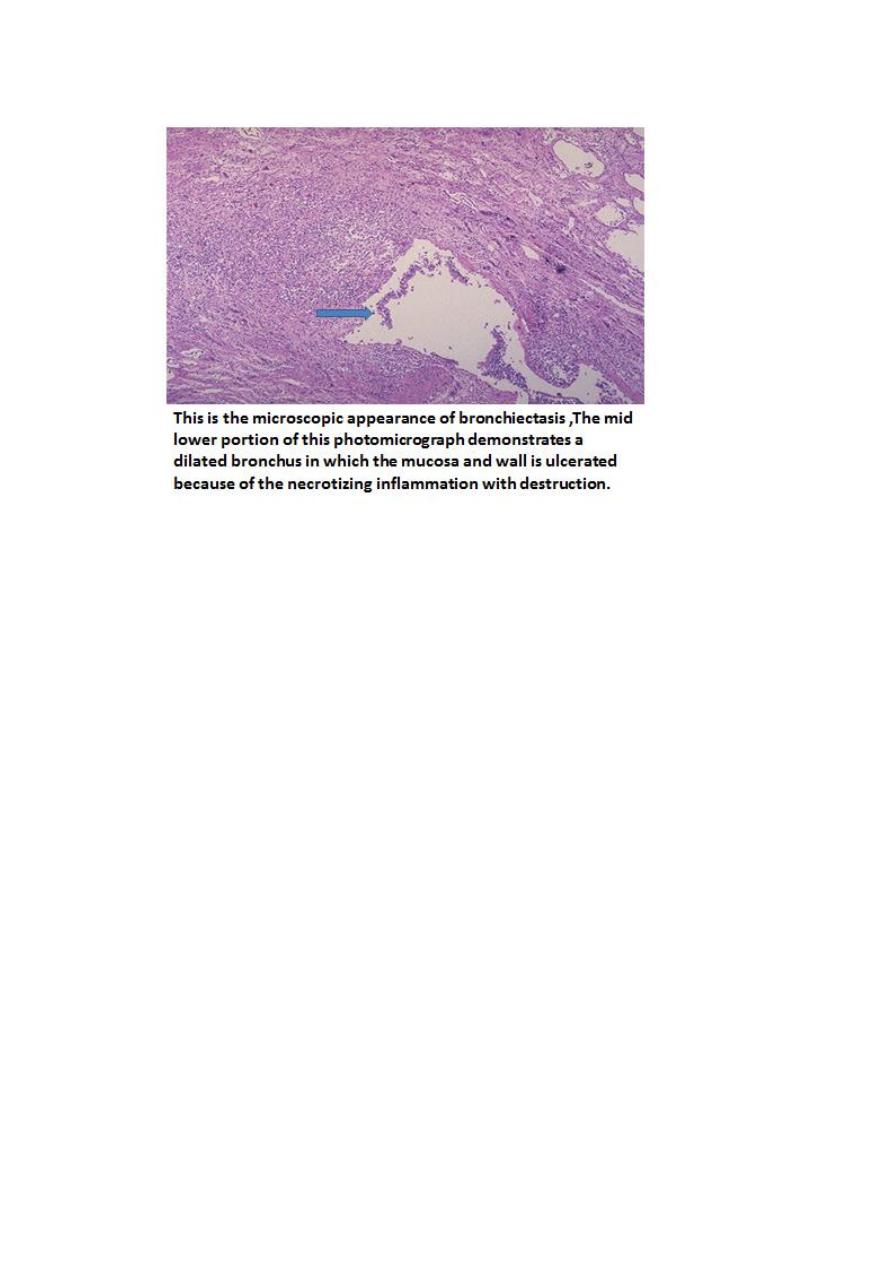
Microscopically :
The histologic findings vary with the activity and chronicity of the disease. In the full-
blown picture of disease, an intense acute and chronic inflammatory exudate within
the walls of the bronchi and bronchioles and the desquamation of lining epithelium
cause extensive areas of ulceration.
Fibrosis of bronchial and bronchiolar walls develop in more chronic cases.
When healing occurs , the lining epithelium may regenerate completely , however so
much injury has occurred that abnormal dilation and scarring has occurred.
Necrosis destroys the bronchial and bronchiolar walls and forms lung abscess.
9
