The Esophagus
Congenital anomalies
Atresias :“a thin, noncanalized cord replaces a segment of
esophagus, causing a mechanical obstruction” with a proximal
blind pouch connected to the pharynx and a lower pouch
connected to the stomach.
Fistula
:
Esophagus connects with the bronchus or trachea.
Fistulae can lead to aspiration, suffocation, pneumonia, and severe
fluid and electrolyte imbalances.
Stenosis, webs, rings:
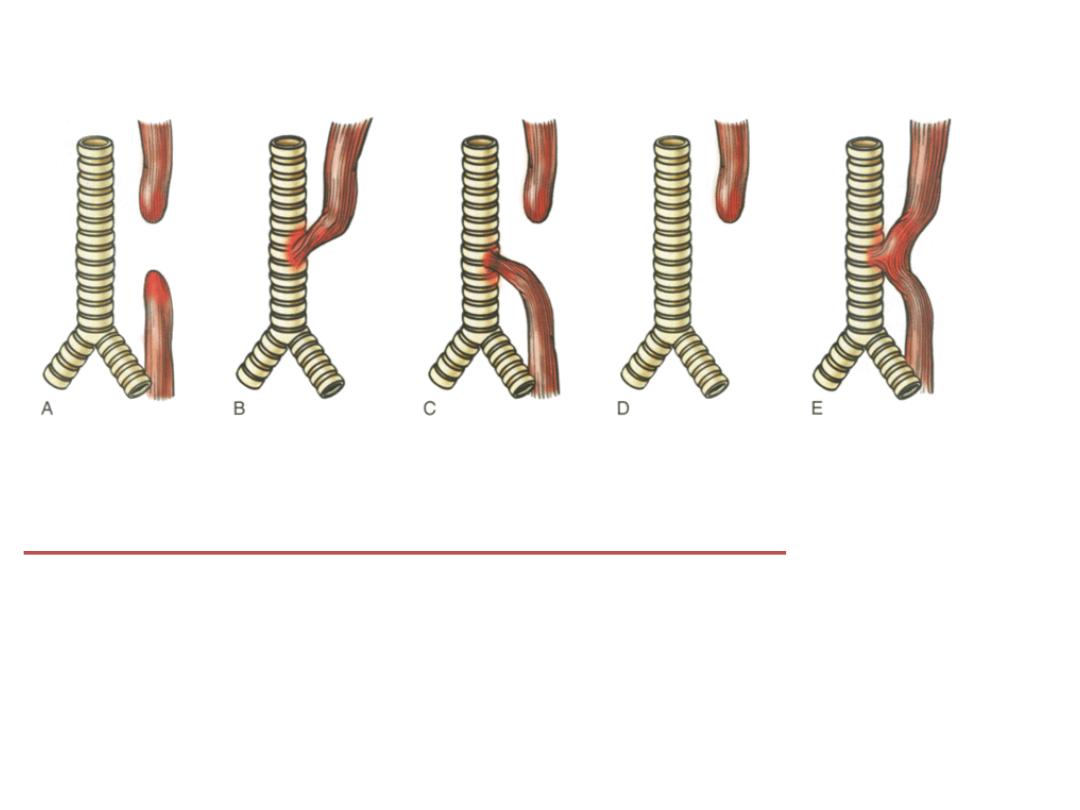
Esophageal atresia and tracheoesophageal fistula.
A
, Blind upper and lower esophageal segments.
B,
Fistula between
blind upper segment and trachea.
C,
Blind upper segment,fistula
between blind lower segment and trachea.
D,
Blind upper segment
only.
E,
Fistula between patent esophagus and trachea.
Type C is the
most common variety.
Diaphragmatic Hernia, Omphalocele, and Gastroschisis
Diaphragmatic hernia occurs when incomplete formation of the
diaphragm allows the abdominal viscera to herniate into the
thoracic cavity.
When severe, the space-filling effect of the displaced viscera
can cause pulmonary hypoplasia that is incompatible with life
after birth.
Omphalocele occurs when closure of the abdominal
musculature is incomplete and the abdominal viscera herniate
into a ventral membranous sac. This may be repaired surgically,
but as many as 40% of infants with an omphalocele have other
birth defects, including diaphragmatic hernia and cardiac
anomalies.
Gastroschisis is another ventral wall defect similar to
omphalocele except that it involves all of the layers of the
abdominal wall, from the peritoneum to the skin.
Ectopia
Ectopic tissues (developmental rests) are common in the
GI tract. The most frequent site of ectopic gastric mucosa is
the upper third of the esophagus, where it is referred to as
an inlet patch. While generally asymptomatic, acid
released by gastric mucosa within the esophagus can result
in dysphagia, esophagitis, Barrett esophagus, or, rarely,
adenocarcinoma.
Ectopic pancreatic tissue occurs less frequently and can be
found in the esophagus or stomach. Like inlet patches,
these nodules are most often asymptomatic but can
produce damage and local inflammation.

Benign conditions
Achalasia:
• dilatation of the esophagus above the LES.
• wall may be of normal or increased thickness.
• may be primary or secondary to diabetic
neuropathy, malignancy, Chagas disease or
amyloidosis
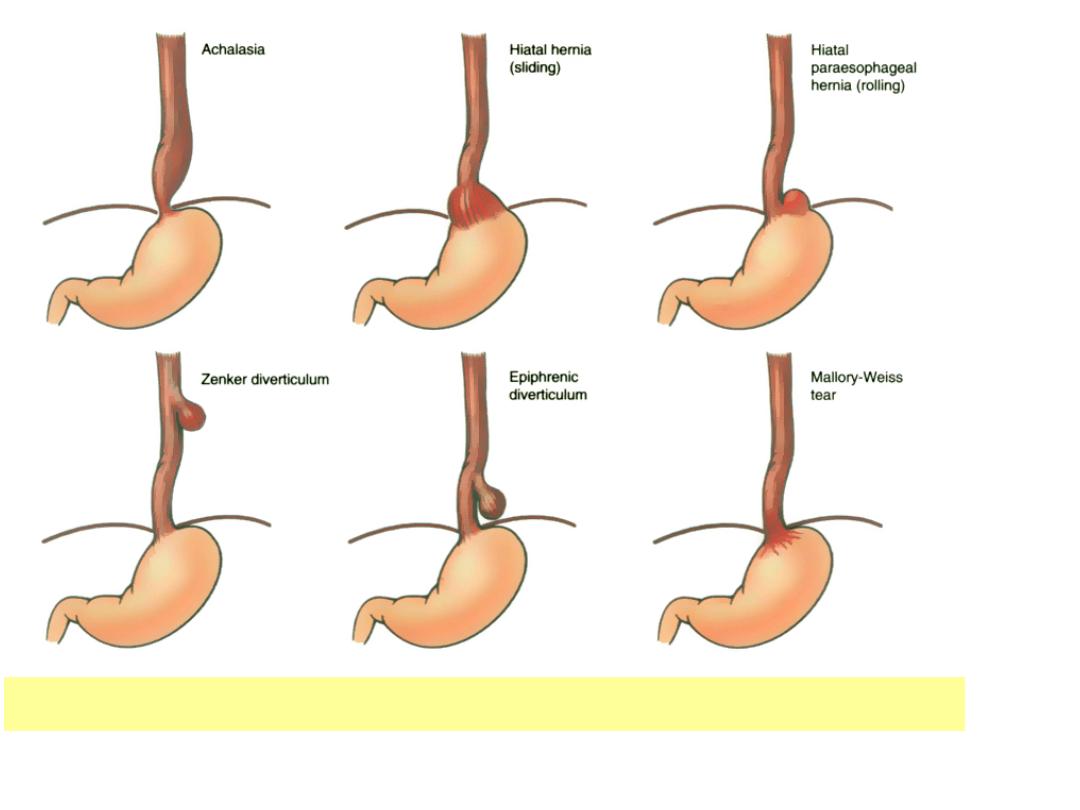
Major conditions associated with esophageal motor dysfunction

There are three major abnormalities:
• A peristalsis.
• Partial relaxation of LES with swallowing.
• Increased LES pressure.
Microscopically:
Myenteric ganglia are absent from the body
of esophagus.

Complications of achalasia include:
1. Severe dysphagia
2. Nocturnal regurgitation and aspiration.
3. 5% of patients it may be complicated by the
development of squamous cell carcinoma.

Hiatal hernia
• acquired herniation of the stomach due to
widening of the space between the muscular crura
of the diaphragm and the esophageal wall.
• herniation may be axial (sliding) or non-axial
(paraesophageal).
• sliding hernia – herniation of the esophagogastric
junction through the hiatus into the thorax ; sliding
– most common (95%)
• paraesophageal
through
hiatus
alongside
esophagus (esophagogastric junction remains in the
abdomen)
Hernias may be found in up to 20% of adult
subjects (asymptomatic).
Infants and children may also have hiatal
hernias
complications
:
1. Bleeding and perforation
2. Strangulation or obstruction may complicate
paraesophageal hernias
Esophagitis
Reflux esophagitis is due to reflux of gastric contents.
Causes:
1. Associated with an altered LES tone ( CNS depressants,
hypothyroidism, pregnancy, alcohol or tobacco
exposure)
2. Hiatal hernia as well as delayed gastric emptying may
also play a role.
3. Inflammation is due to acid peptic action upon the
mucosa.

Microscopic features include:
a) Inflammatory cells in the epithelial layer:
eosinophils, neutrophils, lymphocytes.
b) Basal zone hyperplasia (over 20% of epithelial
thickness)
c) Elongation of lamina propria papillae with
congestion, up to the upper third of the
epithelial layer.
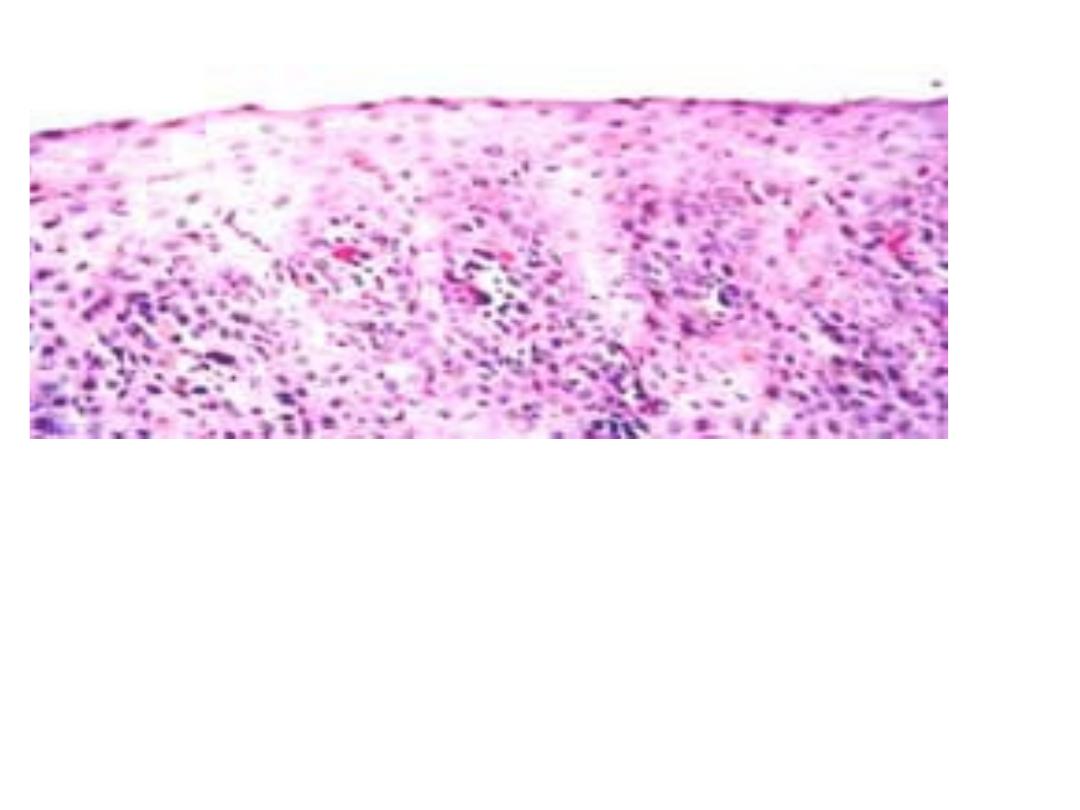
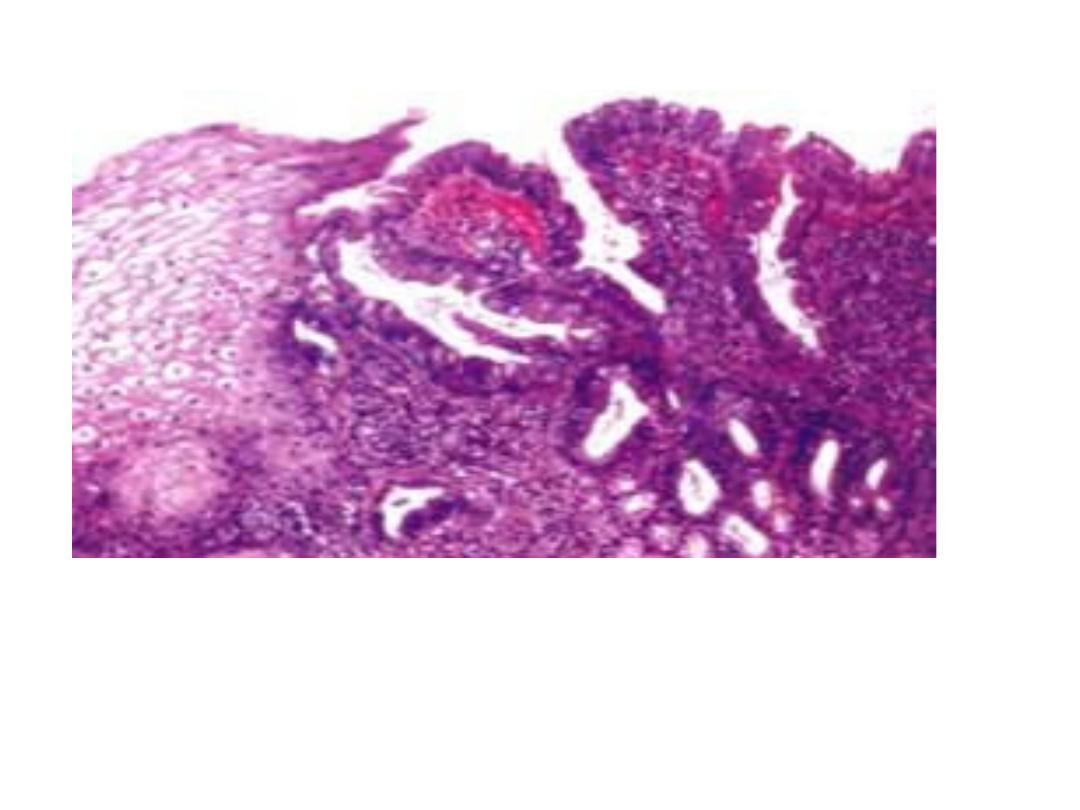
Reflux esophagitis.
Low-power view of the superficial portion of the mucosa.
Numerous eosinophils within the squamous epithelium,
elongation of the lamina propria papillae, and basal zone
hyperplasia are present.
Barrett Esophagus
As a c
omplication of long-standing
gastroesophageal reflux.
Pathology:
The distal squamous mucosa is replaced by
metaplastic columnar epithelium.
Pathogenesis:
Inflammation and ulceration, followed by
ingrowth of metaplastic columnar epithelium,
intestinal type.
Grossly or endoscopically:
1.
Seen as red, velvety mucosa located between the
pale, white squamous mucosa.
2. It may be in small tongues or patches extending up
from the GE junction or displacing in a broad fashion
the squamo-columnar junction upwards.
3. The small tongue or patches are called short
segment Barrett mucosa.
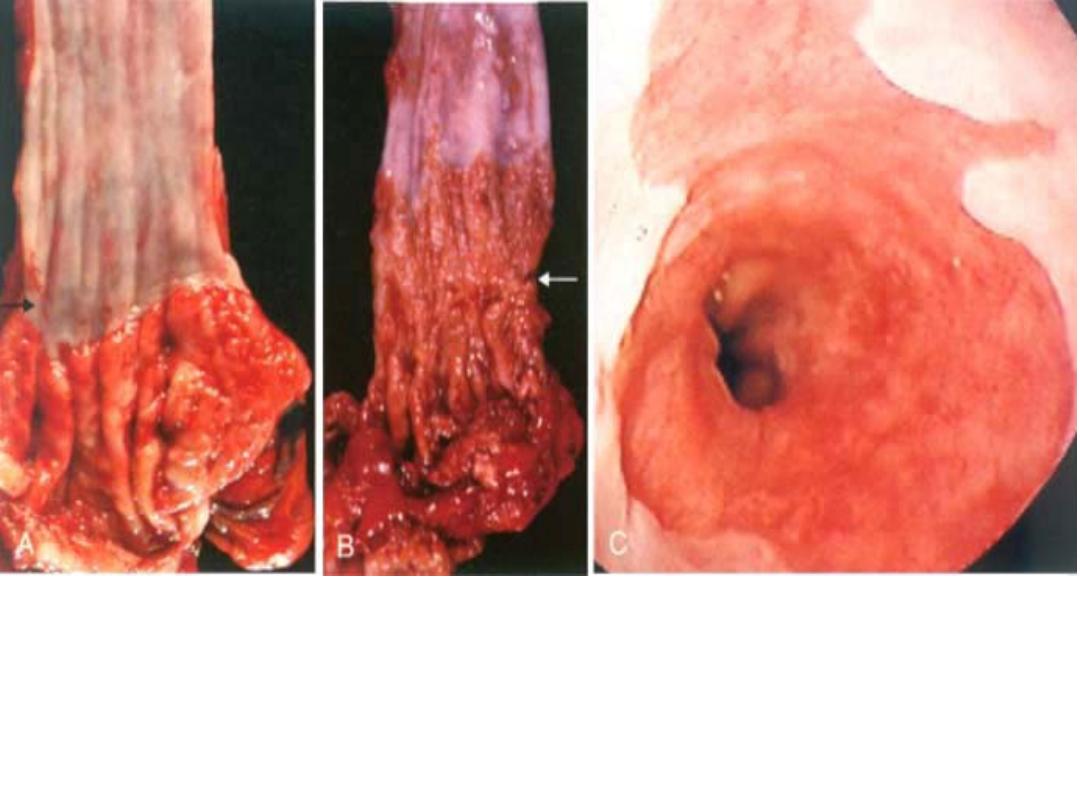
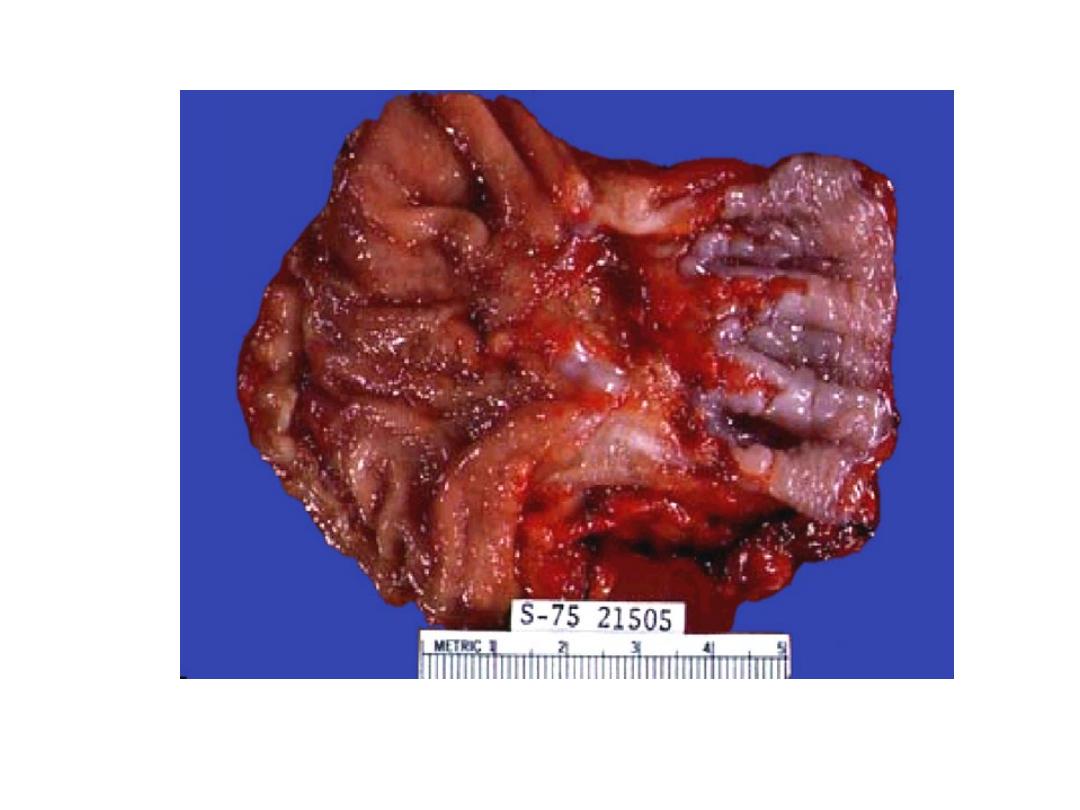
Barrett esophagus.
A, B,
Gross view of distal esophagus
(top)
and proximal
stomach
(bottom),
showing
A,
the normal gastroesophageal junction
(arrow)
and
B,
the granular zone of Barrett esophagus
(arrow). C,
Endoscopic view of
Barrett esophagus showing red velvety gastrointestinal mucosa extending
from the gastroesophageal orifice. Note the paler squamous esophageal
mucosa.
Microscopy:
Dysplastic changes may occur during the course of
Barrett mucosa, consisting of enlarged, crowded and
stratified nuclei.
Two types of dysplasia are recognized:
1. Low grade, with basal orientation of nuclei.
2. High grade with nuclei reaching the apex of the
epithelial cells.
Adenocarcinoma may occur in both short and long
segment Barrett mucosa.
Barrett esophagus. Microscopic view showing squamous
mucosa and intestinal-type columnar epithelial cells (goblet
cells) in a glandular mucosa

Infectious and chemical esophagitis
The ingestion of mucosal irritants may cause
inflammation of the esophagus; e.g. corrosive
acids or alkali, hot fluids, alcohol, heavy smoking.
Other causes of esophagitis include cytotoxic
anticancer therapy, infection after bacteremia or
viremia.
In immunosuppressed patients herpes simplex
and cytomegalovirus (CMV) are the most
common organisms; in debilitated patients fungal
infections e.g. candida, may occur.
Esophageal varices:
Caused by portal hypertension, mainly due to
cirrhosis of the liver.
Collaterals develop in the lower esophagus,
eventually becoming tortuous, protruding into
the lumen mucosa may be inflamed and
eroded.
Varicosal dilatation may lead to rupture, with
massive hemorrhage as a severe complication.
In patients with cirrhosis, ruptured varices may
lead to death in 40% of patients in the first
episode of bleeding.

EsophagEal NEoplasms

Esophageal Neoplasms
Benign tumors
The most common benign tumors are of smooth muscle
origin, called leiomyomas.
Other benign tumors include: fibromas, lipomas,
hemangiomas, squamous papillomas and
inflammatory polyps
Malignant tumors
Carcinoma of the esophagus represents 6% of G.I. cancers.
Two main types are recognized:

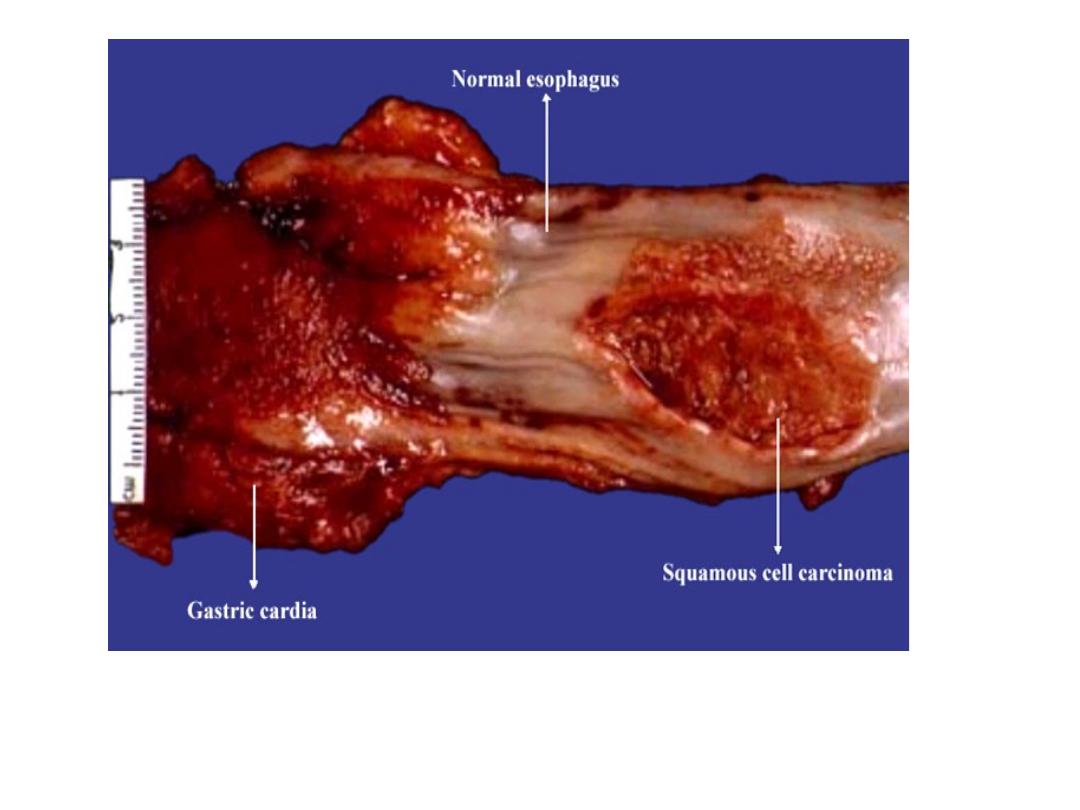
Squamous cell carcinoma
1. Occur in adults over the age of 50 years.
2. Male – female ratio from 2:1 to 20:1
3. Worldwide in distribution but the incidence varies
according to different regions.
4. High incidence areas include Central Asia, Northern
China, Puerto Rico and Eastern Europe, where it
may exceed 100 per 100,000.
5. Blacks are at higher risk than are whites.

Etiology-Pathogenesis:
1. Dietary and environmental factors are
described as major risk factors.
2. Genetic predisposition is thought to play a
minor role.
3. Alcohol and tobacco usage are main factors in
the US and Europe.
4. In other parts of the world, carcinogens such as
fungus contaminated and nitrosamines in
foodstuffs play a major role in China and South
Africa.
5. Human papilloma virus DNA is found in tumors
from high incidence regions.

• More than half of cancers have p53 mutations.
• Also p16 and allelic loss, indicating stepwise
accumulation of genetic alterations.
• There are, however, no K-ras or APC gene
mutations identified in squamous cell carcinomas

Morphology:
• 20% of tumors are located in the upper third of the
esophagus, 50% in the middle third, 30% in the lower
third.
• Tumors appear as exophytic polypoid lesions in 60% of
cases; flat in 10% and excavated-necrotic
ulceration in 25% of cases
• May erode into the respiratory tree or aorta, invade the
mediastinum and pericardium.
• Rarely it is superficial, confined to the epithelial layer or
submucosa.
• Usually well differentiated.
-Tumors located in the upper third metastasize to cervical
lymph nodes
-The mid esophagus tumors metastasize to mediastinal
lymph nodes and the lower esophageal tumors to gastric
and celiac nodes
Clinically:
The tumors produce dysphagia and obstruction; patients
experience weight loss.
Hemorrhage and sepsis may result from tumor ulceration.
Five year survival is 75% for superficial carcinoma, 25% for
patients undergoing curative surgery;
overall is 5% survival for esophageal carcinoma.
Adenocarcinoma
Up to half of all esophageal cancers are
adenocarcinomas, in association with Barrett
esophagus.
Alterations include overexpression of p53 and
allelic losses in 17p.
The tumors are usually in the distal esophagus,
may invade the cardia and grow to be large
nodular masses.
Microscopically
They are mucin producing, occasionally with
Signet ring types.
Clinically :
• Adenocarcinomas are more common in men than
women, more frequent in white than black males.
• Symptoms are similar to those in squamous cell
carcinomas.
• Prognosis is poor, with 30% 5 year survival
• Cancers limited to mucosa and submucosa have a
5-year survival of 80%