
1
Babylon University Stage Fourth
College of Medicine Lecture 3
Dr. Athraa Falah
THE HEPATIC PATHOLOGY
CIRRHOSIS
Cirrhosis is the twelfth most common cause of death in the United States, accounting for most
liver-related deaths.
Classification of cirrhosis:
Primary(Cryptogenic Cirrhosis) 10%.
Secondary due to:
1-Alcohol abuse.
2-Chronic viral hepatitis.
3-Non-alcoholic steatohepatitis(NASH)
4-Biliary disease.
5-Iron overload
Cirrhosis, as the end stage of chronic liver disease, is defined by three main morphologic
characteristics:
• Bridging fibrous septa in the form of delicate bands or broad scars linking portal tracts with
one another and portal tracts with terminal hepatic veins.
• Parenchymal nodules containing hepatocytes encircled by fibrosis, with diameters varying
from very small (<3 mm, micronodules) to large (several centimeters, macronodules).
Nodularity results from cycles of hepatocyte regeneration and scarring.
• Disruption of the architecture of the entire liver.
Pathogenesis.
The central pathogenic processes in cirrhosis are death of hepatocytes, extracellular matrix
(ECM) deposition, and vascular reorganization.
-Activated kupffer cells lead to death and destruction of hepatocyte .
-Types I and III collagen are deposited in the space of Disse, creating fibrotic septal tracts.
-The vascular architecture of the liver is disrupted by the parenchymal damage and scarring, with
the formation of new vascular channels in the fibrotic septa that connect the vessels in the portal
region (hepatic arteries and portal veins) to terminal hepatic veins, shunting blood from the
parenchyma.

2
The predominant mechanism of fibrosis is the proliferation of hepatic stellate cells and their
activation into highly fibrogenic cells.
As they are converted into myofibroblasts, the cells release chemotactic and vasoactive factors,
cytokines, and growth factors. Myofibroblasts are contractile cells, capable of constricting
sinusoidal vascular channels and increasing vascular resistance within the liver parenchyma.
The stimuli for stellate cell activation may originate from several sources :
(a) Chronic inflammation, with production of inflammatory cytokines such as tumor necrosis
factor (TNF), lymphotoxin, and interleukin 1β (IL-1β), and lipid peroxidation products;
(b) Cytokine and chemokine production by Kupffer cells, endothelial cells and hepatocytes
(c) Direct stimulation of stellate cells by toxins.
Throughout the process of liver damage and fibrosis, the surviving hepatocytes are stimulated to
regenerate and proliferate as spherical nodules within the confines of the fibrous septa. The net
outcome is a fibrotic, nodular liver in which delivery of blood to hepatocytes and the ability of
hepatocytes to secrete substances into plasma are severely compromised. Disruption of the
interface between the parenchyma and portal tracts may also obliterate biliary channels, leading to
the development of jaundice.
Schematic of Stellate cell activation and liver fibrosis. Kupffer cell activation leads to secretion of multiple cytokines.
Platelet-derived growth factor (PDGF) and tumor necrosis factor (TNF) activate stellate cells, and contraction of the
activated stellate cells is stimulated by endothelin-1 (ET-1). Fibrogenesis is stimulated by transforming growth factor
β (TGF-β). Chemotaxis of activated stellate cells to areas of injury is promoted by PDGF and monocyte chemotactic
protein-1 (MCP-1).
Clinical Features.
About 40% of individuals with cirrhosis are asymptomatic until late in the course of the disease.
When symptomatic, they present with nonspecific clinical manifestations: anorexia, weight loss,
weakness, and, in advanced disease, symptoms and signs of hepatic failure .
3
The ultimate mechanism of deaths in most cirrhotic patients is (1) progressive liver failure, (2) a
complication related to portal hypertension, or (3) the development of hepatocellular carcinoma.
Intrahepatic Biliary Tract Disease
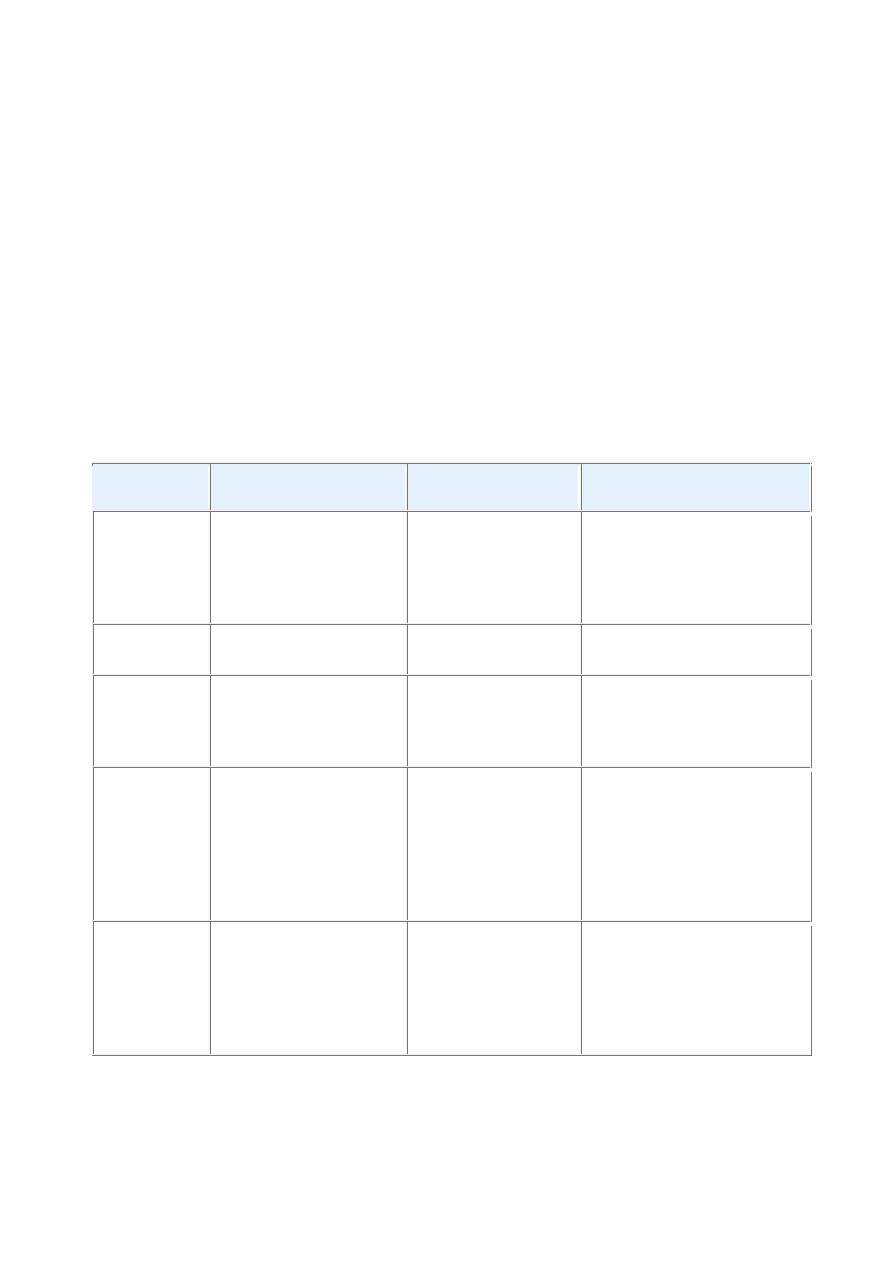
There are three disorders of intrahepatic bile ducts: secondary biliary cirrhosis, primary biliary
cirrhosis, and primary sclerosing cholangitis (summarized in Table below ).
Secondary biliary cirrhosis is a condition resulting most often from uncorrected obstruction of the
extrahepatic biliary tree.
Primary biliary cirrhosis is a destructive disorder of the intrahepatic biliary tree.
Primary selerosing cholangitis involves both the extrahepatic and intrahepatic biliary tree.
TABLE -- Distinguishing Features of the Major Intrahepatic Bile Duct Disorders
Secondary
Biliary
Cirrhosis
Primary
Billiary
Cirrhosis
Primary
Sclerosing
Cholangitis
Etiology
Extrahepatic bile duct
obstruction:
biliary
atresia,
gallstones,
stricture, carcinoma of
pancreatic head
Possibly autoimmune Unknown,
possibly
autoimmune; 50% to 70%
associated with inflammatory
bowel disease
Sex
predilection
None
Female to male, 6 : 1
Female to male, 1 : 2
Symptoms and
signs
Pruritus,
jaundice,
malaise, dark urine, light
stools,
hepatosplenomegaly
Same as secondary
biliary
cirrhosis;
insidious onset
Same as secondary biliary
cirrhosis; insidious onset
Laboratory
findings
Conjugated
hyperbilirubinemia,
increased serum alkaline
phosphatase
Same as secondary
biliary cirrhosis, plus
elevated serum IgM
autoantibodies
(especially M2 form
of anti-mitochondrial
antibody)
Same as secondary biliary
cirrhosis, plus elevated serum
IgM,
hypergammaglobulinemia
Important
pathologic
findings
before
cirrhosis
develops
Prominent bile stasis in
bile ducts, bile ductular
proliferation
with
surrounding neutrophils
Dense
lymphocytic
infiltrate
in
portal
tracts
with
granulomatous
destruction
of
bile
ducts
Periductal
portal
tracts
fibrosis

4
Metabolic Liver Disease
A distinct group of liver diseases is attributable to disorders of metabolism, either acquired or
inherited. The most common acquired metabolic disorder is non-alcoholic fatty liver disease.
Among inherited metabolic diseases, hemochromatosis, Wilson disease, and α
1
-antitrypsin
deficiency are most prominent.
Nonalcoholic Fatty Liver Disease (NAFLD)
NAFLD is a group of conditions that have in common the presence of hepatic steatosis (fatty
liver), in individuals who do not consume alcohol, or do so in very small quantities (less than 20 g
of ethanol/week).
NAFLD includes simple hepatic steatosis, steatosis accompanied by minor, non-specific
inflammation, and non-alcoholic steatohepatitis (NASH).
Steatosis with or without non-specific inflammation is generally a stable condition without
significant clinical problems.
In contrast, NASH is a condition in which there is hepatocyte injury that may progress to cirrhosis
in 10% to 20% of cases. The main components of NASH are hepatocyte ballooning, lobular
inflammation, and steatosis. With progressive disease fibrosis occurs.
NASH affects men and women equally and the condition is strongly associated with obesity,
dyslipidemia, hyperinsulinemia and insulin resistance.
Pathogenesis.
The precise mechanisms of steatosis and hepatocellular damage in NAFLD are not entirely
known, but genetics and environment play a role in the pathogenesis.
A “two-hit” model of pathogenesis has been proposed, encompassing two sequential events:
(1) hepatic fat accumulation and, (2) hepatic oxidative stress.
The oxidative stress acts upon the accumulated hepatic lipids, resulting in lipid peroxidation and
the release of lipid peroxides, which can produce reactive oxygen species.
Clinical Features.
Individuals with simple steatosis are generally asymptomatic.
Liver biopsy is the most reliable diagnostic tool for NASH and helps determine the extent of
steatosis, presence of steatohepatitis, and degree of fibrosis.
Serum AST and ALT are elevated in about 90% of patients with NASH. Despite the enzyme
elevations, patients may be asymptomatic. Others have general symptoms such as fatigue and
right-sided abdominal discomfort caused by hepatomegaly.

5
The current management strategy seeks to correct the underlying risk factors, such as obesity and
hyperlipidemia, and to treat insulin resistance.
WILSON DISEASE
Wilson disease is an autosomal recessive disorder caused by mutation of the ATP7B gene,
resulting in impaired copper excretion into bile and a failure to incorporate copper into
ceruloplasmin.
This disorder is marked by the accumulation of toxic levels of copper in many tissues and organs,
principally the liver, brain, and eye.
Morphology.
The hepatic changes are variable, ranging from relatively minor to massive damage. Fatty change
(steatosis) may be mild to moderate, with vacuolated nuclei and occasionally, focal hepatocyte
necrosis.
An acute hepatitis can show features mimicking acute viral hepatitis, except possibly for the
accompanying fatty change.
The chronic hepatitis of Wilson disease exhibits moderate to severe inflammation and hepatocyte
necrosis, with the particular features of macrovesicular steatosis, vacuolated hepatocellular nuclei,
and Mallory bodies. With progression of chronic hepatitis, cirrhosis will develop.
Nearly all patients with neurologic involvement develop eye lesions called Kayser-Fleischer
rings, green to brown deposits of copper in Desçemet's membrane in the limbus of the cornea.
Clinical Features.
The disorder usually manifests in affected individuals between 6 and 40 years of age. The most
common presentation is acute or chronic liver disease. Neuropsychiatric manifestations, including
mild behavioral changes, frank psychosis, or a Parkinson disease–like syndrome (such as tremor).
The biochemical diagnosis of Wilson disease is based on a decrease in serum ceruloplasmin, an
increase in hepatic copper content and increased urinary excretion of copper.
Benign neoplasms
Hepatic Adenoma
Benign neoplasms developing from hepatocytes are called hepatic adenomas or liver cell
adenomas. Hepatic adenomas most frequently occur in young women who have used oral
contraceptives; tumors generally regress if contraceptive use is terminated.
Hepatic adenomas have clinical significance for three reasons:
(1) When they present as an intrahepatic mass they may be mistaken for hepatocellular
carcinomas;

6
(2) Subcapsular adenomas have a tendency to rupture, particularly during pregnancy (under
estrogen stimulation), causing life-threatening intraperitoneal hemorrhage;
(3) Rarely, they may transform into carcinomas, particularly, when the adenoma arises in an
individual with glycogen storage disease, and adenomas in which mutations of the β-catenin gene
are present.
Pathogenesis.
The causal events are unknown, but it may be assosciated with
-Hormonal stimulation.
-Mutations in the genes encoding the transcription factor HNF1α and β-catenin .
-Multiple hepatic adenoma (adenomatosis) syndromes can occur in individuals with maturity-
onset diabetes of young (MODY3), with HNF1 mutations.
Morphology.
Liver cell adenomas are pale, yellow tan, and frequently bile-stained nodules, found anywhere in
the hepatic substance but often beneath the capsule. They may reach 30 cm in diameter. Although
they are usually well demarcated, encapsulation might not be present. The tumor commonly
presents as a solitary lesion, but multiple lesions can occur.
Histologically, liver cell adenomas are composed of sheets and cords of cells that may resemble
normal hepatocytes or have some variation in cell and nuclear size. Portal tracts are absent;
instead, prominent solitary arterial vessels and draining veins are distributed through the substance
of the tumor.
MALIGNANT TUMORS
Malignant tumors occurring in the liver can be primary or metastatic. Primary carcinomas of the
liver are relatively uncommon in North America and western Europe (0.5% to 2% of all cancers)
but represent 20% to 40% of cancers in many other countries. Most primary liver cancers arise
from hepatocytes and are termed hepatocellular carcinoma (HCC).
Hepatocellular Carcinoma (HCC)
It is the third most frequent cause of cancer deaths. About 82% of HCC cases occur in developing
countries with high rates of chronic HBV infection, such as in southeast Asian and African
countries; 52% of all HCC cases occur in China. There is a clear predominance of males.
Pathogenesis.
Four major etiologic factors associated with HCC have been established:
-Chronic viral infection (HBV, HCV),

7
-Chronic alcoholism,
-Non-alcoholic steatohepatitis (NASH), and
-Food contaminants (primarily aflatoxins).
Other conditions include tyrosinemia, glycogen storage disease, hereditary hemochromatosis, non-
alcoholic fatty liver disease, and α
1
-antitrypsin deficiency.
Many factors, including genetic factors, age, gender, chemicals, hormones, and nutrition, interact
in the development of HCC.
The pathogenesis of HCC may be different in high-incidence, HBV-prevalent populations versus
low-incidence Western populations, in which other chronic liver diseases such as alcoholism, non-
alcoholic steatohepatitis, chronic HCV infection, and hemochromatosis are more common.
In .high-prevalence regions the HBV infection begins in infancy by the vertical transmission of
virus from infected mothers, which confers a 200-fold increased risk for HCC development by
adulthood. Cirrhosis may be absent in as many as half of these patients, and the cancer often
occurs between 20 and 40 years of age.
In the Western world where HBV is not prevalent, cirrhosis is present in 75% to 90% of cases of
HCC, usually in the setting of other chronic liver diseases. Thus, cirrhosis seems to be a
prerequisite contributor to the emergence of HCC in Western countries but may have a different
role in HCC that develops in endemic areas.
In China and southern Africa, where HBV is endemic, there may also be exposure to aflatoxin, a
toxin produced by the fungus Aspergillus flavus, which contaminates peanuts and grains.
Aflatoxin can bind covalently with cellular DNA and cause a specific mutation in codon 249 of
p53 .
Although the precise mechanisms of carcinogenesis are unknown, several events have been
implicated.
-Repeated cycles of cell death and regeneration, as occurs in chronic hepatitis lead to the
accumulation of mutations during continuous cycles of cell division which may damage DNA
repair mechanisms and eventually transform hepatocytes.
-Progression to HCC might result from point mutations in selected cellular genes such as KRAS
and p53, and others .
-Recent global gene expression studies revealed that approximately 50% of HCC cases are
associated with activation of WNT or AKT pathways.
-A subgroup of tumors expresses a high proportion of genes present in fetal liver and liver
progenitor cells, suggesting that at least some HCCs may be generated from liver stem cells.
Universal vaccination of children against HBV in endemic areas can dramatically decrease the
incidence of HBV infection, and most likely, the incidence of HCC.

8
Morphology.
HCC may appear grossly as (1) a unifocal (usually large) mass ; (2) multifocal, widely
distributed nodules of variable size; or (3) a diffusely infiltrative cancer, permeating widely and
sometimes involving the entire liver.
HCCs are usually paler than the surrounding liver, and sometimes take on a green colour when
composed of well-differentiated hepatocytes capable of secreting bile. All patterns of HCCs have
a strong propensity for invasion of vascular structures. HCC spreads extensively within the liver
by obvious contiguous growth and by the development of satellite nodules.
Histologically HCCs range from well-differentiated to highly anaplastic undifferentiated lesions.
In well-differentiated and moderately differentiated tumors, cells that are recognizable as
hepatocytic in origin are disposed either in a trabecular pattern(cord like) or in an acinar,
pseudoglandular pattern.
In poorly differentiated forms, tumor cells can take on a pleomorphic appearance with numerous
anaplastic giant cells, can be small and completely undifferentiated.
Clinical Features.
Most patients have ill-defined upper abdominal pain, malaise, fatigue, weight loss, and sometimes
awareness of an abdominal mass or abdominal fullness. In many cases the enlarged liver can be
felt on palpation, with sufficient irregularity or nodularity to permit differentiation from cirrhosis.
Jaundice, fever, and gastrointestinal or esophageal variceal bleeding are inconstant findings.
Laboratory finding: Elevated levels of serum α-fetoprotein are found in 50% of persons with
HCC.
The natural course of HCC involves the progressive enlargement of the primary mass until it
seriously disturbs hepatic function, or metastasizes, generally first to the lungs .Death usually
occurs from (1) cachexia, (2) gastrointestinal or esophageal variceal bleeding, (3) liver failure with
hepatic coma, or, rarely, (4) rupture of the tumor with fatal hemorrhage. The 5-year survival of
large tumors is dismal, with the majority of patients dying within the first 2 years.
