Haemolytic anaemias
Normal red cell destruction:
Red cell destruction usually occurs after a mean life span of 120 days when
the cells are removed extravascularly by the macrophages in the bone
marrow ,liver and spleen.
The breakdown of the haem from red cells liberates iron for re circulations
via plasma transferrin to marrow erythroblasts, and protoporphyrin which is
broken down to bilirubin
Bilirubin circulates to the liver where it is conjugated to glucoronides which
are excreted into the gut via bile and converted to stercobilinogen and
stercobilin which are excreted in faeces, stercobilinogen and stercobilin are
partly reabsorbed and exerted in urine as urobilinogen and uribilin.
Globin chains are broken down to amino acids which are reutilized for
general protein synthesis in the body, intravascular haemolysis(break down
of red cells with in blood vessels ) plays little or no role in normal red cells
destruction.
Definition of haemolytic anaemias:
Haemolytic anaemias are defined as those anaemias that results from an
increase in the rate of red cells destruction.
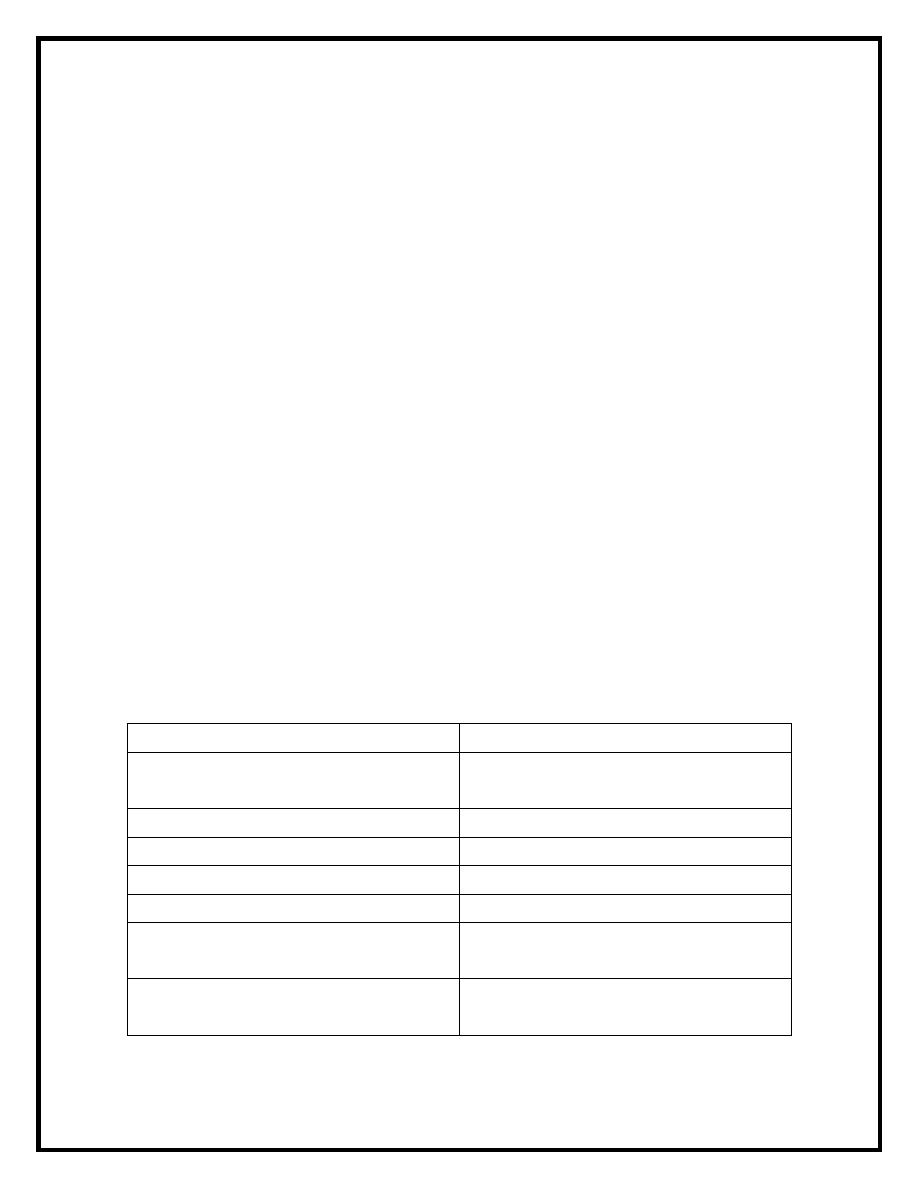
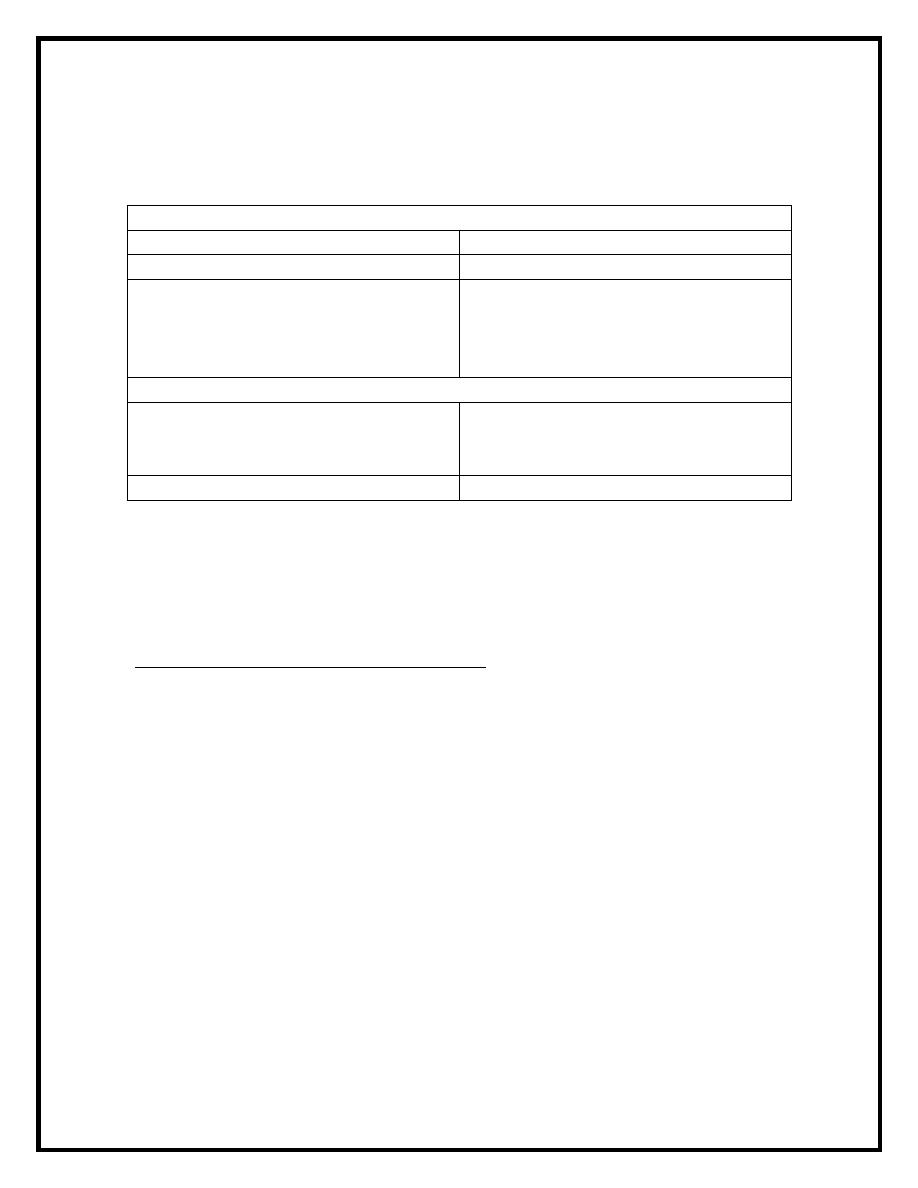
Classification of haemolytic anaemias:
Acquried
Hereditary
1-immune (autoimmune,alloimmune
and drug associated
1-membrane defects
2- red cell fragmentation syndrome
2-defective red cell metabolism.
3-march haemoglobinuria
3-genetic disorder of haemoglobin.
4- infections
5-chemical and physical agents
6- secondary to renal and liver
disease
7-paraxysmal nocturnal
haemoglobinuria
1
Clinical features :
1-pallor of the mucous membrane.
2- mild jaundice.
3- splenomegaly.
4-pigment gallstones may complicates the condition.
5-aplastic crises may occur, usually precipitated by infection with
parvovirus.
Laboratory finding :
The laboratory finding can be divided into three groups:
1- features of increased red cell break down:
a-serum bilirubin raised.
b-urine urobilinogen increased.
c-fecal stercobilinogen increased.
d- serum haptoglobin absent(haptoglobin is a protein found in
normal plasma capable of binding haemoglobin)
2-features of increased red cell production:
a-reticulocytosis.
b- bone marrow erythroid hyperplasia.
3-damged red cells:
a-morphology(spherocytes,elliptocytes)
b-osmotic fragility.
c-shortened red cell survival by
51
Cr
Intravascular and extravascular haemolysis:
These are tow main mechanisms where by red cell destroyed in
haemolytic anaemias,in extravascular haemolysis there is
excessive removal of red cells by macrophages while intravascular
haemolysis ,the red cells are directly destroyed in the circulation.
The main laboratory features of intravascular haemolysis
are:
1-haemoglobinuria(free haemoglobin in the plasma)
2-haemosidrinuria(iron storage protein in the urine)
3-methaemoglobinaemia.
2
Hereditary haemolytic anaemias:
1-membrane defects:
: the mode of inheritance is
Hereditary spherocytosis(HS)
-
a
autosomal dominant,rarly it may be autosomal recessive,it results
from defects in red cell membrane cytoskeleton .
Clinical features:
●Anaemia :can be present at any age.
Fluctuating jaundice.
●
Splenomegaly occurs in most patients.
●
Pigment gall stones are frequent.
●
Aplastic crisis precipitated by parvovirus infection.
●
Investigations:
1-usually low haemoglobin.
2-reticulocytosis.
3-the blood film shows spherocytes.
4-Osmotic fragility test is increased.
5-direct antiglobulin test (coombs test )is negative.
Treatment:
The principle form of treatment is splenectomy ,folic acid is given in sever
cases to prevent folate deficiency.
: this has similar clinical and laboratory features to
hereditary elliptocytosis
-
b
HS, except for the appearance of blood film which has a characteristic
elliptical cells ,but it is clinically mild disorder and occasionally require
splenectomy.
2- Defective red cells metabolism
glucose 6 phosphate dehydrogenase deficiency(G6PD)
-
a
G6PD function is reduction of nicotineamide adenine dinucleotide
phosphate (NADP) while oxidizing glucose6phospate,it is the only source
of NADP in the red cells and as NADP is needed for the production of
reduced glutathione which protect the red cell membrane and haemoglobin
from oxidant stress. .
3
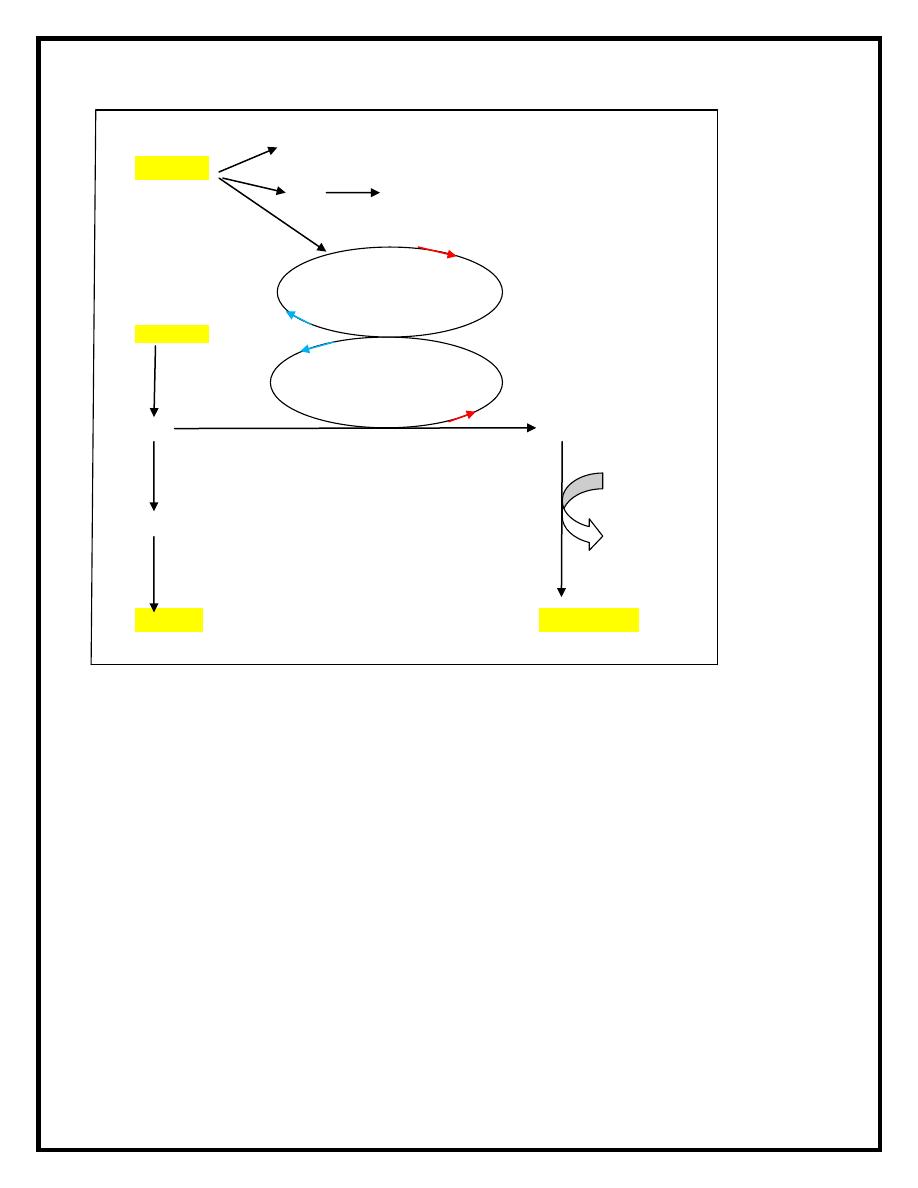
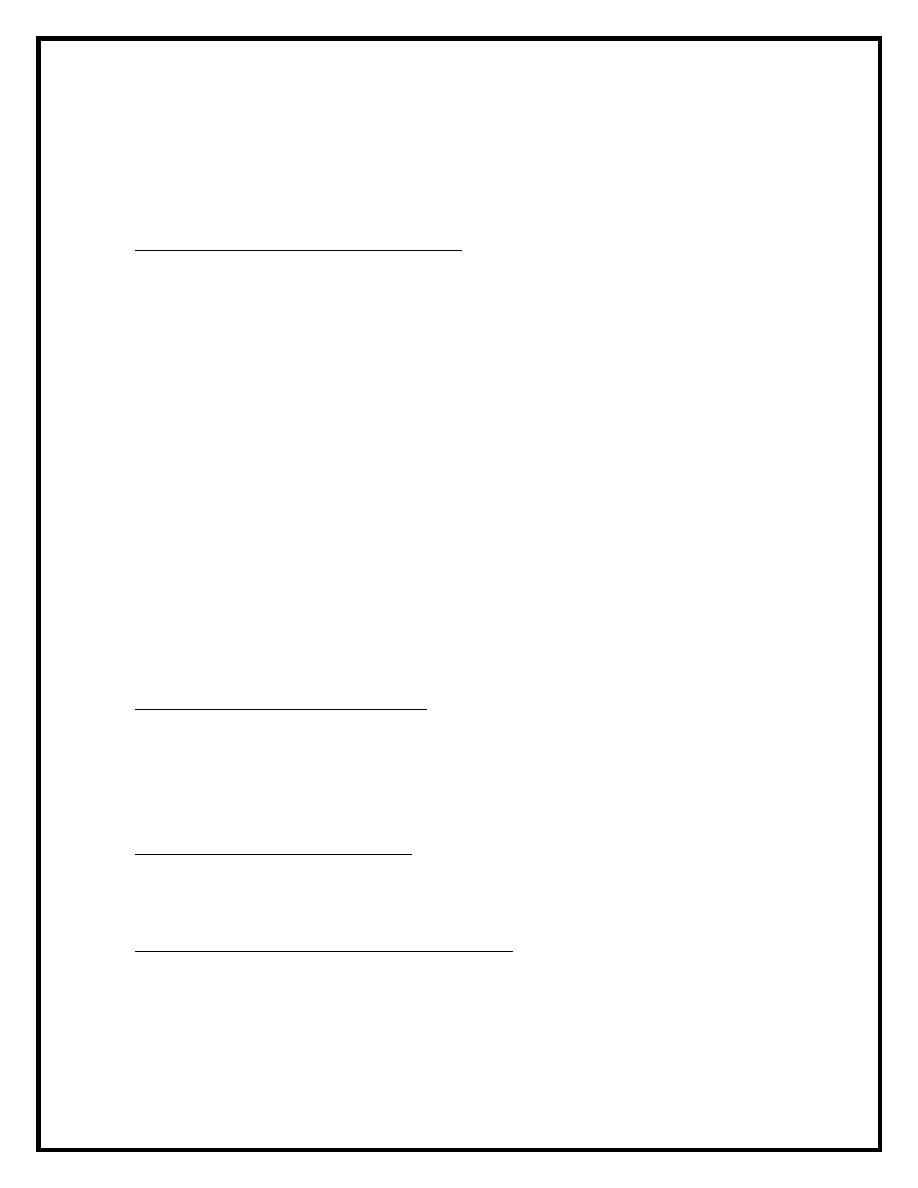
Red cell membrane damage
Oxidant
Hb Heinz body
GSH GSSG
GLUCOSE
NADP NADPH
G6P 6PG
G6PD
F6P
P
-
Pentose 5
Lactate
The inheritance of G6PD is sex-linked ,affecting males and carried by
females who show approximately half the normal red cellG6PD values, there
is a wide variety of normal genetic variants of the enzyme G6PD ,the most
common being type B in western and type A in Africans, in addition more
than 400 variants caused by point mutations or deletion of the enzyme.
The degree of deficiency varies often being mild 10-15 % of normal activity
in black African, more sever in Orientals and most sever in Mediterranean.
Clinical features :
G6PD deficiency is usually a symptomatic, the main syndrome occurs are:
♦ Acute haemolytic anaemia in response to oxidant stress for examples:
drugs such as antimalarial drugs, sulphonamide and sulphones,analgesia and
antihelminthic drugs , other oxidant stress fava beans and infection. The
acute haemolytic syndrome is caused by rapidly developing intravascular
NADP
NADPH
4
haemolysis and haemoglobinuria ,the anaemia may be self limiting as new
young red cells are made with near normal enzyme level.
♦ Neonatal jaundice.
♦Rarely congenital non spherocytic haemolytic anaemia.
Diagnosis:
Between crises the blood count is normal, the enzyme deficiency is detected
by screening test or by direct enzyme assay on red cells, during the crises the
blood film shows contracted and fragmented red cells and Heinz body seen ,
which is denatured and oxidized haemoglobin .there are also features of
intravascular haemolysis.
Treatment :
The offending drugs is stopped , the underlying infection is treated, a high
urine output is maintained and blood transfusion is undertaken for sever
anaemia.
: inherited as autosomal recessive , the severity
pyruvate kinase deficiency
-
b
of the anaemia varies widely , jaundice is usual and gall stones is frequent,
frontal bossing may be present .
Laboratory finding:
● blood film shows poikilocytosis, distorted cells (prickle cells) .
● auto haemolysis test is increased.
●enzyme assay to make the diagnosis .
Treatment: Splenectomy may alleviate the anemia but does not cure it, and
is indicated in those patients who need frequent transfusion.
5
Acquired haemolytic anaemia:
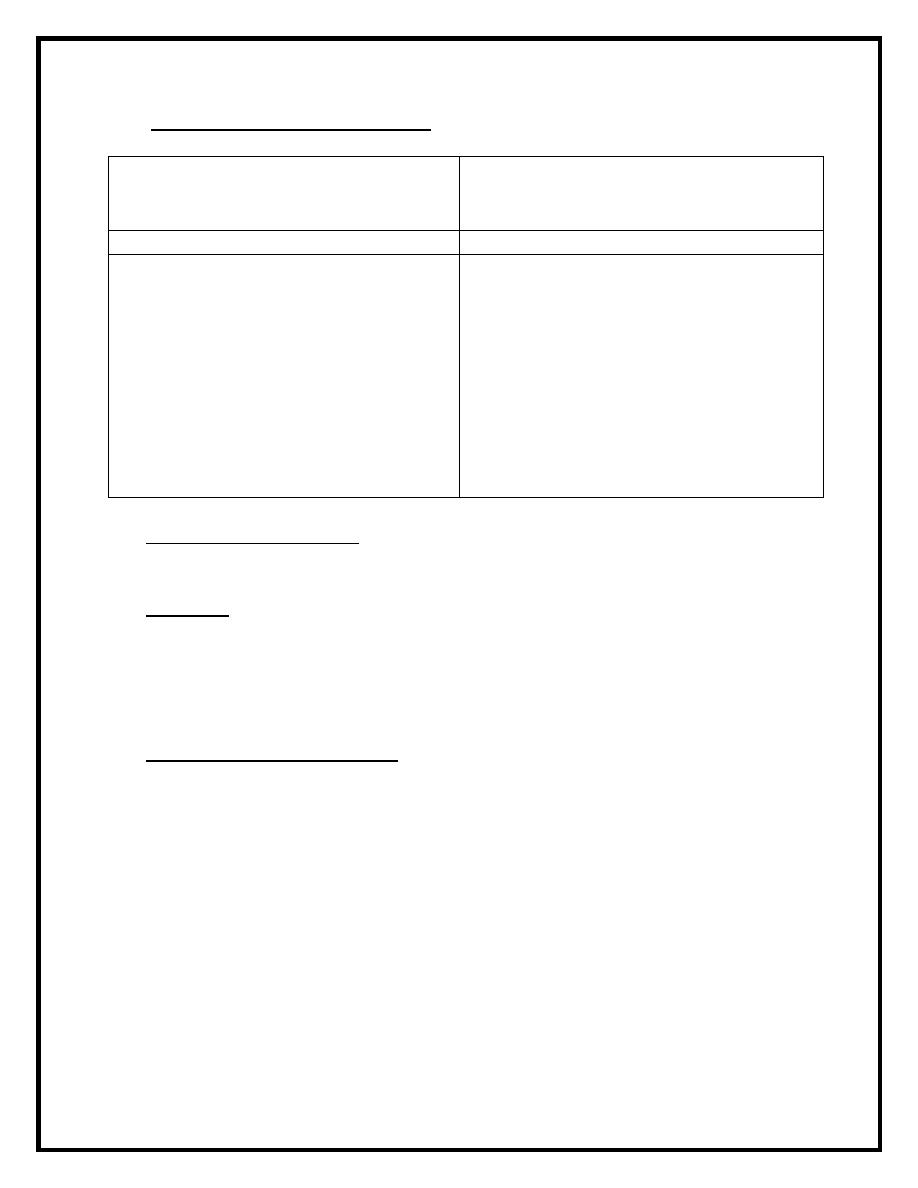
♦ Immune haemolytic anaemia: classification
A-Autoimmune
Cold type:
Warm type:
Idiopathic
Idiopathic
Secondary : Lymphoma,
infections(mycoplasma pneumonia
and infectious mononucleosis),
paroxysmal cold haemoglobinuria.
Secondary : SLE, CLL, Lymphoma,
drugs(methyldopa)
B-Alloimmune
1- Induced by red cells antigens
Haemolytic transfusion reaction ,
Haemolytic disease of newborn.
2- Induced by drugs
Autoimmune haemolytic anaemias: are caused by antibody production by the
body against its own red cells. They are characterized by appositive direct
antiglobulin test( coombs test ) and divided into warm and cold type
according to whether the antibody reacts more strongly with red cells at
37
o
C or 4
o
C.
Warm autoimmune haemolytic anemia :the red cells are coated with
immunoglobulin(Ig) usually immunoglobulin G (IgG) alone or with
complement, and are therefore taken up by macrophages which have
receptors for immunoglobulin ,part of the red cell membrane is lost so it
becomes progressively more spherical and ultimately prematurely destroyed
,predominantly in the spleen.
Clinical features :
The disease occur any age in either sex and present as haemolytic anaemia in
varying severity ,the spleen enlarge and the disease tends to remit and
relapse , it may occur alone or with other disease or arise a result of
methyldopa therapy .
Laboratory finding:
The peripheral blood film shows prominent spherocytosis and the direct
antihuman globulin test is positive as a result of IgG or IgG with
complement on the cells .
Treatment :
1-Remove the underlying cause (methyldopa).
2- corticosteroid ,(prednisolone) is the first line of treatment.
6
3-splenectomy may be of value in those who fail to respond well to steroid.
4-immunsupression may be tried after other measure have failed .
5-monoclonal antibodies ( anti CD20) has produced prolong remission.
6- folic acid is given in few cases.
7-blood transfusion may be needed in sever cases.
Cold autoimmune haemolytic anaemia: in these syndromes the autoantibody
attaches to red cells mainly in peripheral circulation where the blood
temperature is cooled, the antibody is usually IgM and bind to red cells
at4
o
C.IgM antibody is high efficient in fixing the complement and both
intravascular and extravasculer haemolysis can occur.
Clinical features:
The patient may have chronic haemolytic anaemia aggravated by the cold
and often associated with intravascular haemolysis, mild jaundice and
splenomegaly may present, the patient may develops acrocyanosis(purplish
skin discoloration) at the tips of nose, ears and fingers due to agglutination
of red cells in small blood vessels.
Laboratory finding:
Are similar to those in warm type but spherocytosis is less marked.
Treatment :
1-Keep the patient warm.
2- Treatment of the underlying cause.
3-Alkalyting agents such chlorambucil in chronic cases.
4-monoclonal antibody.
5-splenectomy and steroid are usually not helpful.
Paroxysmal cold haemoglobinuria:
It is a rare syndrome of intravasculer haemolysis after exposure to the cold,
it is caused by IgG antibody with specificity for the P blood group antigens
which bind the red cells in the cold and lysis by complement in the warm
condition. Viral infection and syphilis is predisposing causes and the
condition is self limiting.
Alloimmune haemolytic anaemia:
In those anaemias the antibody produced by one individual reacts with red
cells of another. Two important situations are transfusion of incompatible
blood and rhesus haemolytic disease of newborn.
Drugs induced immune haemolytic anaemia:
Drugs may cause immune haemolytic anaemia by three mechanisims:
1-antibody directed against a drug-red cell membrane complex(pencillin).
2-deposition of complement via a drug-protein(antigen)-antibody complex
on to red cell surface(quinidine)
3-true autoimmune haemolytic anaemia(methyldopa).
7
♦ Red cell fragmentation syndrome , caused by:
1-Cardiac haemolysis:(arise through
physical damage to red cells on
abnormal surface)
a-prosthetic heart valve
b-arterial grafts
2- arterioveneous malformation
3-microangiopathic : (caused by red
cells passing through abnormal small
vessels).
a-thrombotic thrombocytopenic purpura
(TTP)
b-haemolytic uraemic sundrom(HUS)
c-disseminated intravascular
coagulation(DIC)
d-malignant disease.
e-vasculitis.
f-pre-eclampsia/HELLP syndrome.
♦March haemoglobinurea: Is caused by damage to red cells between the
small bones of the feet, usually during prolonged marching or running.
♦Infections may cause haemolysis in variety of ways :
a-precipitate acute haemolytic crises in G6PD deficiency.
b-cause microangiopathic haemolytic anaemia(meningococcal septicemia)
c-malaria may cause haemolysis by extravascular destruction of parasitized
cells and direct intravascular haemolysis.
♦Chemical and physical agents:
a-drugs (dapsone and salazopyrin) cause intravascular haemolysis in high
doses.
b-chemical poisoning by lead can cause sever haemolysis.
c-sever burn damage red cells causing spherocytosis.
8
