HEAD ACHE &FACIAL PAIN
Dr. Lana Shabur Talabani• INTRODUCTION
• Headache is the most common reasons why a patient seek for medical attention.• Is the symptom of pain anywhere in the region of the head or neck
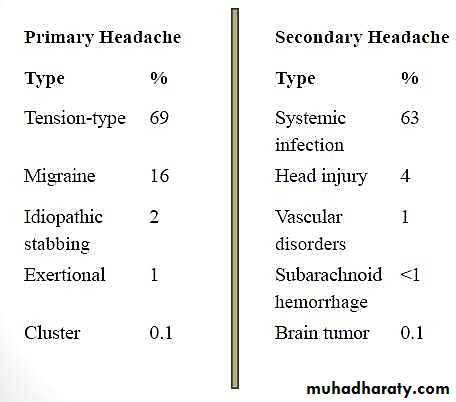
• It classified into primary and secondary headache.
• CLASSIFICATION
• PRIMARY HEADACHE• SECONDARY HEADACHE
• Or idiopathic headaches
• The headache itself is• the disease
• Benign
• Recurrent
• No organic lesion in the background
• Treat the headache
• Or symptomatic headaches
• The headache is only a symptom of an underlying disease
• Treat the underlying disease
• CAUSE OF HEADACHE
• PRIMARY HEADACHE• PRIMARY HEADACHE
• Tension-type• Cluster type
• Migraine (with or without aura)• Sinus
• Thunderclap headache - sudden onset (SAH)• PRIMARY HEADACHE
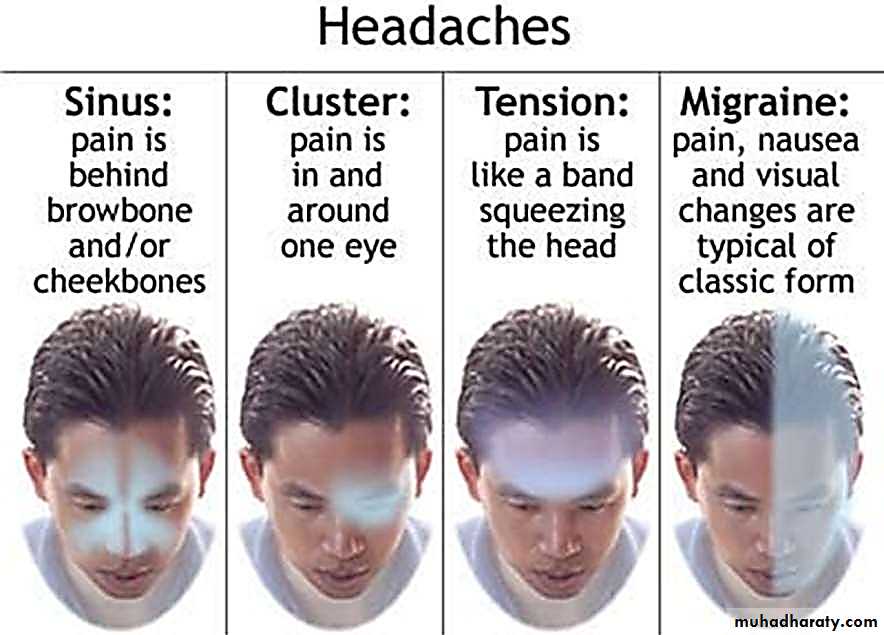
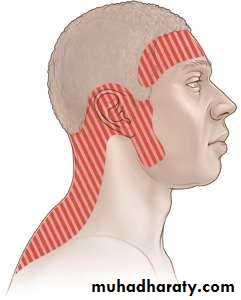
• TENSION HEADACHE
• Dull pain, tightness, or pressure around your forehead or the back of your head and neck.• Diffuse pain in tight head-band pattern
• Bilateral, non-pulsating
• Muscle aches and trouble focusing
• Mild photophobia or phonophobia
• 10 attacks lasting 30 min–7 days
• Not aggravated by routine physical activity
• CLUSTER HEADACHE
• The pain is sharp, burning or piercing sensation• Unilateral pain behind eye
• Short, excruciating (15 min-3 hrs)
• Usually occur in the middle of the night
• Occur daily for 2-3mths then remit for months-years
• Red, watering eyes, blocked nose, sweaty face
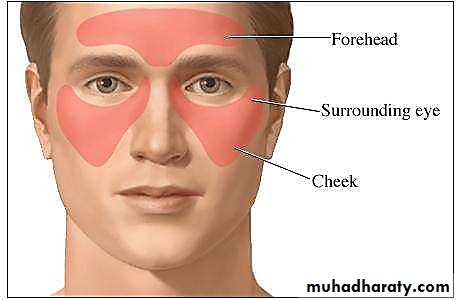
• SINUS HEADACHE
• Sinus headaches are headaches that may feel like an infection in the sinuses (sinusitis).• Pain, pressure and fullness in your cheeks, brow or forehead
• Evidence of discharge from the nose
• Worsening pain if you bend forward or lie down
• Stuffy nose
• Fatigue
• MIGRAINE HEADACHE
• A neurologic disorder characterised by idiopathic, paroxysmal, recurrent attacks of headache lasting from 2-72 hours• Migraine can occur with or without aura (flickering lights, spots or zig-zag lines, fortification blind spots)
• Neurological, Gastrointestinal, Autonomic involvement
• Typical characteristics:
• Unilateral (sometimes bilateral)
• pulsating quality
• Accompanied by nausea & vomiting or photophobia & phonophobia
• Aggravated by physical activity
• MIGRAINE HEADACHE
• Migraine triggers:• Hormonal Changes in women – Fluctuation of Estrogen
• Pregnancy or menopause
• Hormonal medication – oral contraceptives & hormonal replacement therapy
• Foods / Food additives / Drinks
• Stress / Intense physical activities
• Changes in wake-sleep pattern
• Medication
• MANAGEMENT
• Migraine
• Improved by lifestyle changes
• Medications are either to prevent or reduce symptoms once a migraine starts.
• Beta-blockers, antidepressants, anticonvulsants and NSAIDs
• Tension-type headaches
• NSAIDs (ibuprofen, naproxen), acetaminophen or aspirin.• For chronic tension type headaches, amitriptyline.
• Cluster headaches
• Subcutaneous, Sumatriptan and Triptan nasal sprays.• High flow oxygen therapy also helps with relief.
• For people with extended periods of cluster headaches, preventive therapy can be necessary.
• Verapamil is recommended as first line treatment
• SECONDARY HEADACHE
• SECONDARY HEADACHE• Secondary to structures of the head and neck
• sinusitis, glaucoma, temporomandibular joint (TMJ) pain, tooth pain.
• Secondary to chronic diseases
• Hypertension
• Anaemia
• Secondary to psychiatric disorder
• somatisation, psychosis.
• Infections
• Meningitis
• Encephalitis
• Raised ICP
• Brain tumour
• Haemorrhagic stroke
• Head (SAH) and/or neck trauma
• Secondary to a substance, or its withdrawal
• carbon monoxide, alcohol, medication-overuse headache
• HOW TO APPROACH?
• HISTORY
• Onset
• Progression• Frequency
• Duration
• Location
• Character
• Severity
• Aura
• Eye/ear/nose symptoms
• Precipitating factors / Relieving factors
• Effective treatment
• Other medical problems
• PHYSICAL EXAMINATION
• GENERAL• Vital signs
• Funduscopic examination (papilledema)• CV assessment (assess risk of CVA)
• Palpation of the head and face (sinusitis)
• Complete neurologic examination (focal neurologic signs)
• Evidence of meningeal irritation ( Neck flexion, Kernig sign, Brudzinski sign)
• RED FLAGS
• Headache beginning > 50 years of age (temporal arteritis, mass lesion)• Sudden onset of headache (SAH, haemorrhage into a mass lesion or vascular malformation, mass lesion especially post. Fossa mass)
• PHYSICAL EXAMINATION
• RED FLAGS• Headaches increasing in frequency and severity (mass lesion, subdural hematoma, medication overuse)
• New onset headache in patient with risk factors for HIV infection or cancer (Brain abscess, meningitis, metastasis)
• Headache with signs of systemic illness (e.g. fever, seizures, stiff neck, rash indicating meningitis)
• Focal neurologic signs (mass lesion, vascular malformation, stroke, collagen vascular disease evaluation)
• Papilledema (mass lesion, pseudotumor cerebri, meningitis)
• Headache subsequent head trauma (ICH, subdural hematoma, epidural hematoma, post-traumatic headache)
• INVESTIGATION
• LABORATORY• Random use of laboratory testing in the evaluation of acute headache is not warranted.
• CBC when systemic or intracranial infection is suspected• ESR when temporal arteritis is a possibility.
• Neuroimaging
• Neuroimaging is not usually warranted in patients with primary headaches.
• CT scanning is recommended to identify acute haemorrhage• MRI studies are recommended to evaluate the posterior fossa.
Lec 9
• FACIAL PAIN
• DEFINITION• Pain in the facial area may be due to neurological or vascular causes, but equally well may be dental in origin.
• All the neurological and vascular causes of facial pain (excluding headaches) are rare compared to the dental and temporomandibular causes.
• NEUROPATHIC AND VASCULAR PAIN
• Trigeminal neuralgia
• Post-herpetic neuralgia
• Giant cell arteritis
• TRIGEMINAL NEURALGIA
• TRIGEMINAL NEURALGIA• A disorder of the trigeminal nerve that causes episodes of sharp, stabbing pain in the cheek, lips, gums, or chin on one side of the face.
• People with this pain often wince or twitch, which is where trigeminal neuralgia gets its French nickname ‘tic douloureux’, meaning "painful
• twitch”.
• Commonly in middle aged or elderly people
• Female > Male
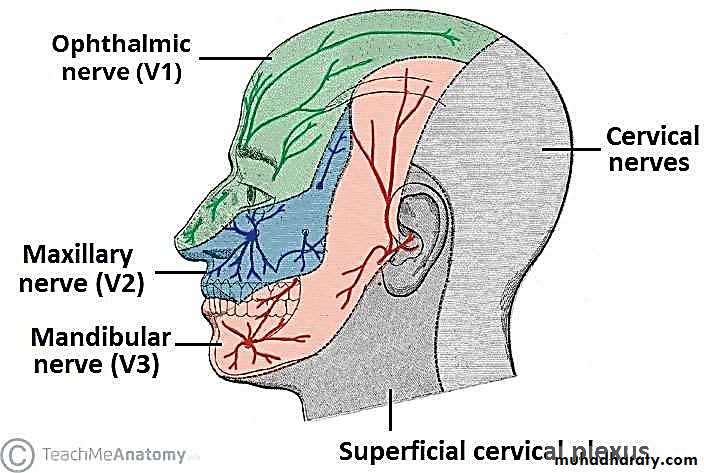
• TRIGEMINAL NERVE
• AETIOLOGY
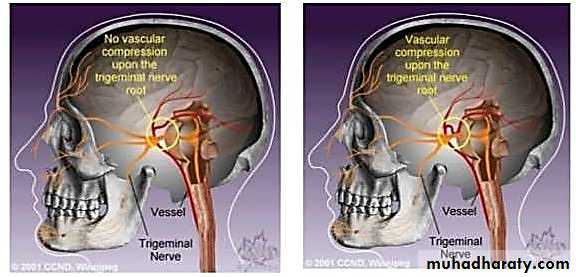
• Usually, the problem is contact between a normal blood vessel — in this case, an artery or a vein — and the trigeminal nerve at the base of your brain. This contact puts pressure on the nerve and causes it to malfunction.• AETIOLOGY
• Can occur as a result of aging, or it can be related to multiple sclerosis or a similar disorder that damages the myelin sheath protecting certain nerves. Less commonly, trigeminal neuralgia can be caused by a tumor compressing the trigeminal nerve.• AETIOLOGY
• TRIGGERS
• Shaving• Touching your face
• Eating
• Drinking
• Brushing teeth
• Talking
• Putting on makeup
• Encountering a breeze
• Smiling
• Washing face
• DIAGNOSIS
• Trigeminal Neuralgia is mainly diagnosed clinically
• History – Type, location and triggering factors
• Neurological examination
• MRI
• TREATMENT
MEDICAL TREATMENT• Carbamazepine (Tegretol / Carbtal)
• Phenytoin sodium (Dilantin)
• Valproic acid
• 1. Microvascular decompression
SURGICAL TREATMENT
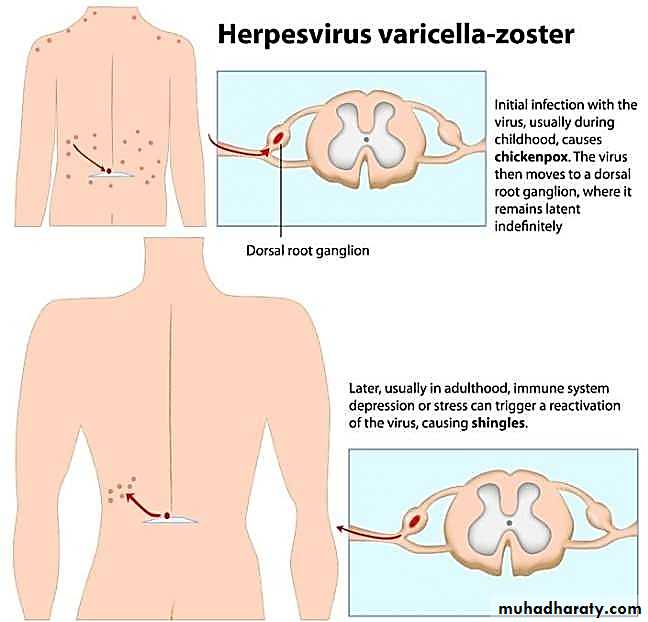
• POST-HERPETIC NEURALGIA
• POST-HERPETIC NEURALGIA• If the pain is caused by shingles continues and persists for more than 90 days (3 months) after the bout of shingles is over – it is known as post- herpetic neuralgia (PHN)
• Post herpetic neuralgia is a painful condition that affects the nerve fibres and skin.
• POST-HERPETIC NEURALGIA
• Age
• Common is > 50 years
• Site
• Ophthalmic nerve is commonly affected
• Complications
• Parasthesia (loss of sensation)• PATHOPHYSIOLOGY
• Shingles
• Further nerve damage by the virus• Changes in the nervous system
• Post-herpetic neuralgia
• SIGNS AND SYMPTOMS
• SIGNS• Pain is variable, from discomfort to very severe, and may be described as burning, stabbing, or throbbing and constant.
• Area of previous herpes zoster may show evidence of cutaneous scarring
• Sensation may be altered over the areas involved, in the form of either hypersensitivity or decreased sensation.
• In rare cases, the patient might also experience muscle weakness, tremor,
• or paralysis if the nerves involved also control muscle movement.
• SYMPTOMS
• MANAGEMENT
• PREVENTION
• Varicella vaccine to prevent chickenpox – lessen the risk of the varicella
• zoster virus lying dormant in the body and reactivating later as shingles.
TREATMENT
• Painkillers
• Anticonvulsants – calm nerve impulses and stabilizing abnormal electrical activity in the nervous system caused by injured nerves
• Lidocaine skin patches – relieve itching, burning and pain from
• inflamation
• Antidepressants – affects key brain chemical such as serotonon and norepinephrine which influence how body interprets pain.
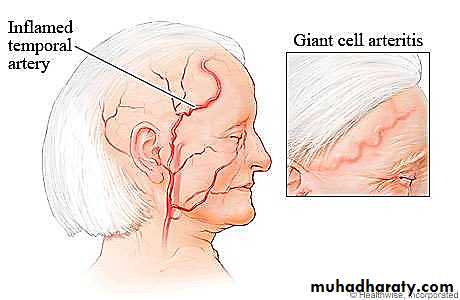
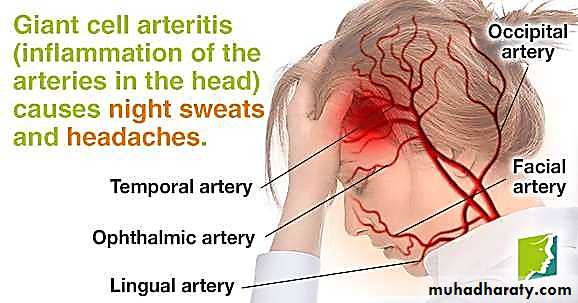
• GIANT-CELL ARTERITIS
• GIANT CELL ARTERITIS• Also called temporal arteritis – an inflammatory disease of blood vessels and the cause is unknown.
• SYMPTOMS
• Headache• Pain over the temples
• Flu-like symtoms (fever, fatigue, loss of apetite)
• Double vision or visual loss
• Pain in jaw and tongue
• INVESTIGATIONS
• Erythrocyte sedimentation rate ESR – raised• CRP – elevated
• Platelets – elevated
• DIAGNOSIS
• The gold standard for diagnosing temporal arteritis is biopsy which involves removing a small part of the vessel under local anesthesia and examining it microscopically for giant cells infiltration.• positive
• negative• TREATMENT
• Corticosteroid (prednisolone) must be started as soon as diagnosis is suspected to prevent irreversible blindness secondary to ophthalmic artery occlusion• OTHER CAUSES OF FACIAL PAIN
• Dental (tooth abscess) – one side, jaw, sensitive to touch• Cluster headache – one side, stuffy nose, tearing around the eye, 30 minutes to 2 hours.
• Sinusitis – dull pain around the eyes and cheekbones worse bending forward
• Migraine – aura, pain on one or both sides, nausea, throbbing or pounding headache
• Post stroke pain – constant, moderate, or severe pain caused by damage to the brain. This means that after a stroke, your brain does not understand normal messages sent from the body in response to touch, warmth, cold, and other stimuli. Instead, the brain may register even slight sensations on your skin as painful.• APPROACH TO FACIAL PAIN DIAGNOSIS
• HISTORY AND EXAMINIATION• To make an accurate diagnosis, it is essential to listen to the history and allow time for the patient to complete their opening statement
• History needs to include details on:
• Family history (any genetic predisposition) 2.Social history
• 3.Significant life events 4.Drug history
• 5.Past medical history
• HISTORY
• Timing: onset, duration and periodicity• Location and radiation
• Quality and severity
• Relieving and aggravating factors
• Effect of prolonged chewing, eating, brushing teeth, touching the face, etc
• Associated factors
• Taste, salivary flow, clenching, nasal, eye or ear symptoms
• Other pain conditions
• Headaches, migraines, etc.
• Impact of pain
• e.g. sleep, mood, concentration, quality of life
• PERIODICITY AND LOCATION
• Chronic continuous pain
• Bilateral
• Unilateral• Temporomandibular disorders
• Persistent orofacial muscle pain• Burning mouth syndrome
• Idiopathic orofacial pain
• Post hepatic neuralgia
• Post traumatic trigeminal pain• Referred pain
• Post stroke pain
• Giant cell arteritis• Chronic migraine
• Cancer pain• Neuropathic
• Vascular
• Musculoskeletal Primary headache Mixed / unknown
• PERIODICITY AND LOCATION
• Episodic pain• Bilateral
• Unilateral• Tension type headache
• Medication overuse headache• Classical trigeminal neuralgia
• Glossopharyngeal nauralgia
• Episodic migraine
• Neuropathic
• Vascular• Musculoskeletal Primary headache Mixed / unknown
• EXAMINATION
• Extraoral examination is confined generally to the head and neck region.
• Inspection
• Any colour changes, swellings and skin lesions.• Palpation
• Any enlargement of salivary glands• Prominent temporal arteries with or without pulsation (Giant cell arteritis) Any tenderness
• EXAMINATION
• Examination includes the muscles of mastication, head and neck muscles for tenderness and trigger points, muscle hypertrophy, and movement of the temporomandibular joint including crepitus.• The cranial nerves need to be examined.
• Intraoral examination (dental)• COMPARISON
• DisorderLocation / radiation
• Timing
• Quality / severity
Aggravating factors
• Burning, tingling,
Post herpetic
Site of herpes zosterContinuous
• itchy, tender, can be
Light touch, eating
neuralgia
• extraoral and
• sharp at times
intraoral• moderate to severe
• Paroxysmal attacks• of 2 s to minutes,
Unilateral trigeminal• refractory period
• Sharp, shooting
• Light touch washing,
nerve most common
between attacks,
• electric shock like,
• cold wind, eating,
Trigeminal neuralgia
second and third
10–30 attacks daily,
• frightful, but in
• brushing teeth,
divisions extraoral
• may remit for• some aching,
• many attacks are
and intraoral
weeks, months.• burning after pain,
• evoked but some
• Other types can
• moderate to very• can be spontaneous
• have a longer pain
• severe
• that can last for
hours• COMPARISON
• Disorder• Location / radiation
• Timing
• Quality / severity
• Aggravating factors
Giant cell arteritis
• Temporal region jaw area may be bilateral• Continuous often sudden onset
• Dull aching throbbing but can be very severe if tongue claudication is occurring• Chewing