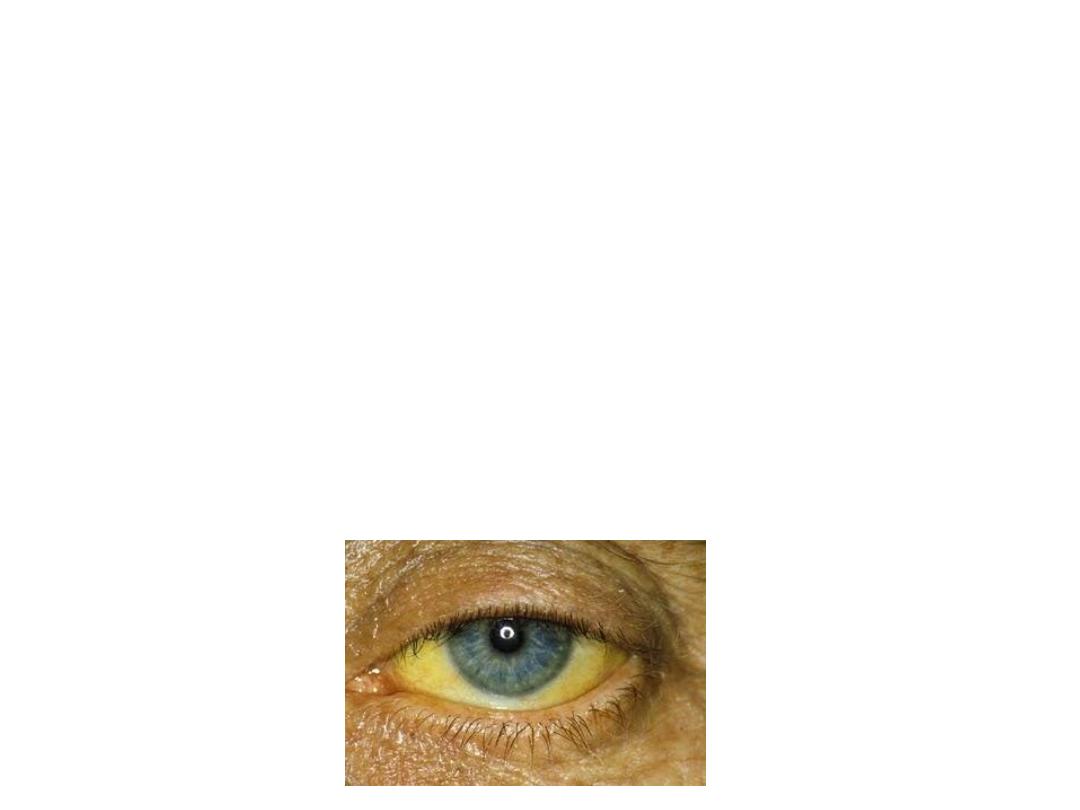
Liver Disease in Pregnency
( Jaundice in Pregnancy)

Obstetric Cholestasis:
• Cholestasis is an impairment of bile flow which
may clinically present with fatigue, pruritus
and, in its most overt form, jaundice.
• Obstetric cholestasis is uncommon condition,
specific to pregnancy
• Aetiology relate to genetic predisposition to the
cholestatic effect of estrogen (
Increased
estrogen levels lead to increased cholesterol
secretion and supersaturation of bile).
• The importance of this condition is its
association with sudden IUFD, mostly at term.

Presentation
• It is most commonly present in the third
trimester at around 32 weeks
• Itching can vary from mild to intense and
persistent, affecting the whole body
particularly the palms & soles.
• There is no rash.
• There may be associated dark urine, pale stool,
steatorrhea & malaise.
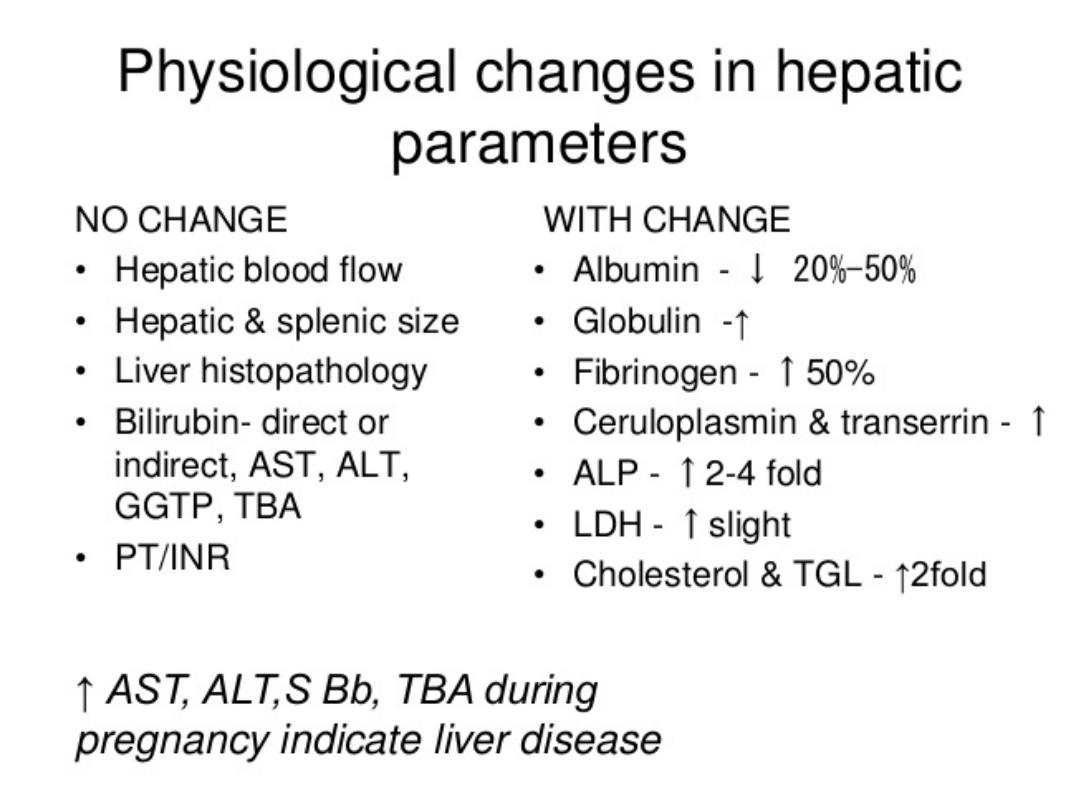
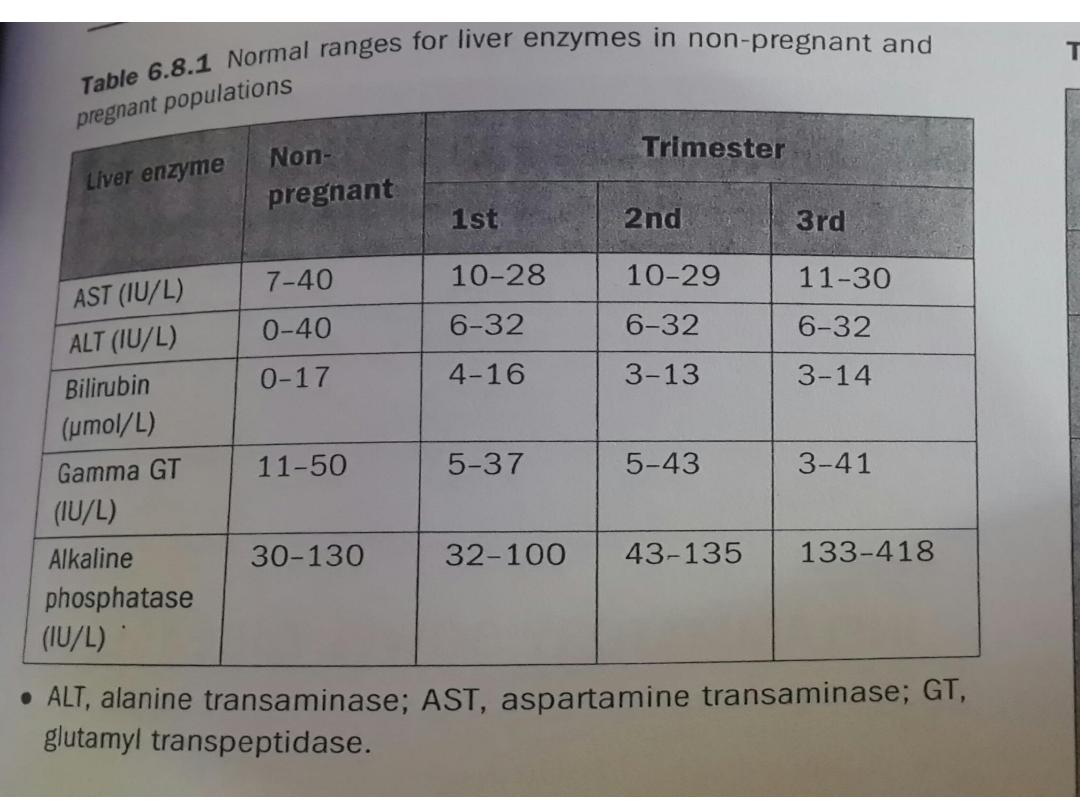
• Hepatic transaminases are only mildly
elevated. Bile acids may be elevated.

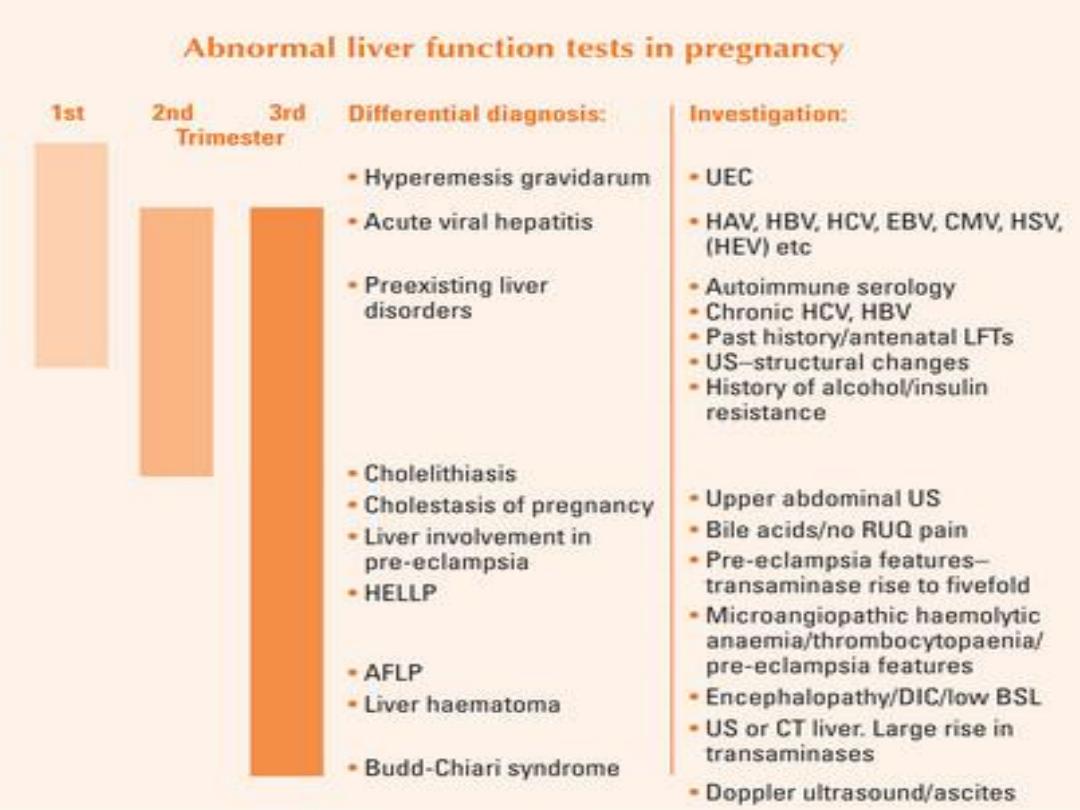
• differential diagnosis include:
• extrahepatic obstruction with gall stones
• acute & chronic viral hepatitis
• primary biliary cirrhosis
• chronic active hepatitis.
• Pre-eclampsia
• HELLP syndrome
• Acute fatty liver of pregnancy
• Sepsis
• Drug-induced hepatitis

• Investigations should include:
• LFT
• Serum Bile acids
• Full blood count
• Clotting profile
• Renal function
• serology for hepatitis A, B, C, Ebstien-Bar
virus & cytomegalovirus
• liver autoantibodies (anti- mitochondrial
antibodies, & anti-smooth muscle antibody).
• liver ultrasound & ultrasound for fetal growth
& amniotic fluid

Complications:
• postpartum haemorrhage
• premature labour
• meconium-stained liquor
• fetal distress in labour
• intra-uterine death.

Management:
• Pruritus may be troublesome and is thought
to result from elevated serum bile salts.
• Control of pruritis: a combination of
antihistamines & emollients , if no response
ursodeoxycholic acid used.
• Vitamin K (water soluble form) should be
given to the mother from the time of
diagnosis to reduce the risk of postpartum
haemorrhage.

• LFT & clotting time should be monitored
regularly.
• Fetal surveillance with CTG &
ultrasound.
• delivery should be induced at 37-38
weeks.

• Following delivery, LFT returns to
normal. Should be monitored at 6 weeks
postpartum
• Symptoms may recur with estrogen
containing oral contraceptives which
should be avoided.
• Recurrence in subsequent pregnancy is
very high

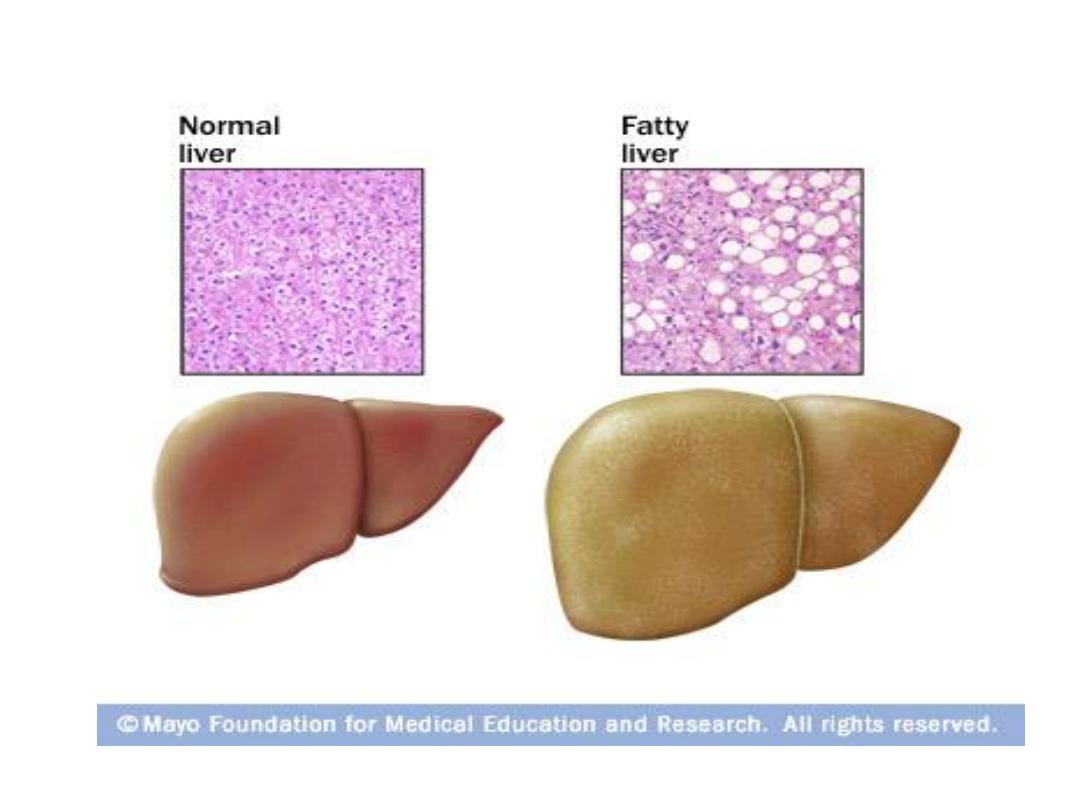
Acute Fatty Liver of pregnancy:
• AFLP is closely related to pre-eclampsia
(genetic defect in fatty acid oxidation).
• presents in the third trimester with
abdominal pain, nausea, vomiting,
anorexia & jaundice.
• aetiology is unknown but histologically
perilobular fatty infiltration of liver cells
is noted.
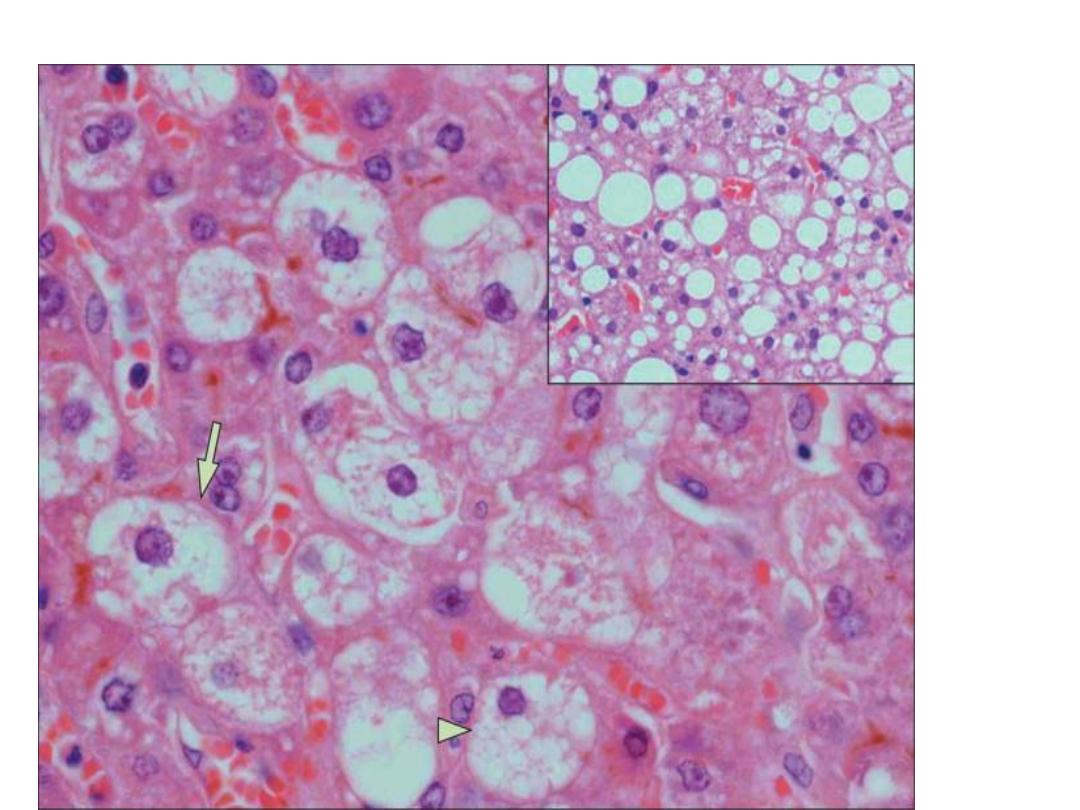

• Following the onset, there is a rapidly
worsening cascade of problems.
• markedly deranged LFT, renal
impairment, raised uric acid, raised white
blood cells, hypoglycaemia &
coagulopathy.
• Perinatal & maternal mortality &
morbidity are increased. Maternal death
result from hepatic encephalopathy or
overwhelming haemorrhage.

Management:
• Relies on early diagnosis.
• intensive care unit & multidisciplinary team.
• Delivery should be expedited, this will be by
CS under GA, following correction of
hypoglycaemia or coagulopathy with 50%
dextrose, vitamin K , fresh frozen plasma &
platelets.
• Management after delivery is conservative.
Referral to liver unit is indicated if liver
function still abnormal or there are features of
hepatic encephalopathy.

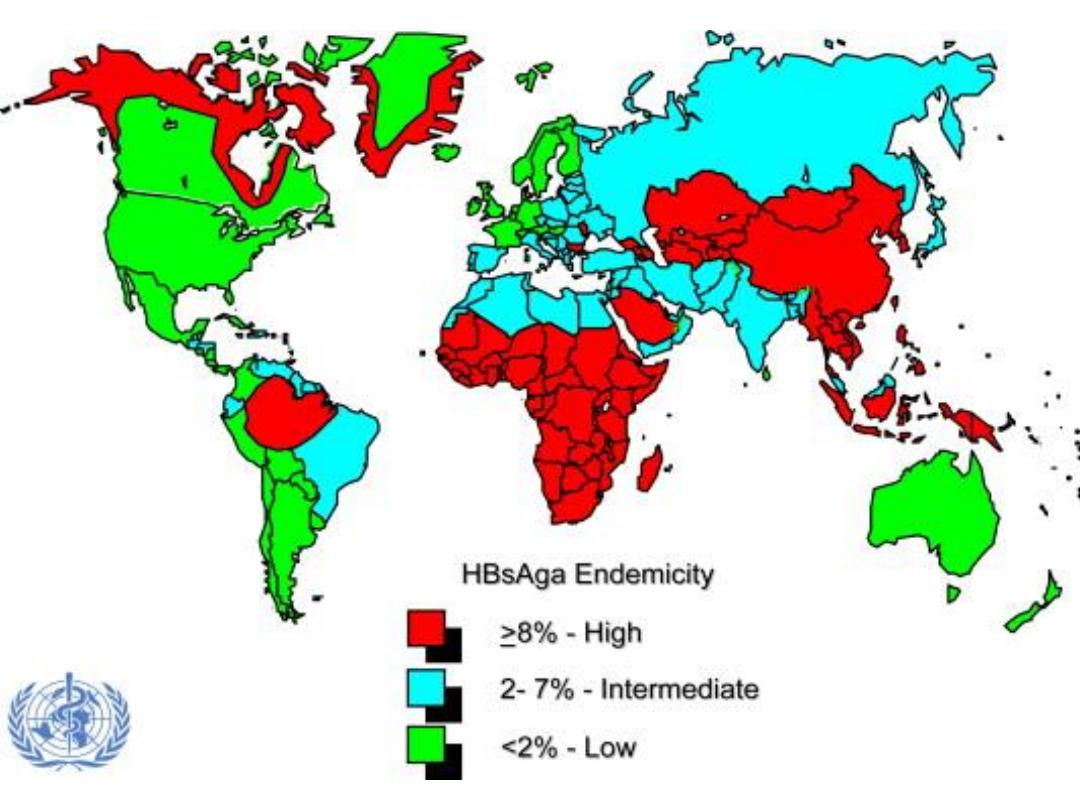
Viral Hepatitis & Pregnancy:
• most common cause of jaundice in
pregnancy .
• None of the hepatitis viruses are known
to be teratogenic .
• The course of most viral hepatitis
infections is unaltered by pregnancy
except with hepatitis E which exhibit
markedly increased fatality rates.

Treatment:
• may benefit from pharmacologic therapy for
chronic HBV and chronic HCV infections.
• Interferon does not have an adverse effect on
the embryo or fetus while the use of ribavirin
during pregnancy is contraindicated.
• Post-exposure Prophylaxis for Susceptible
Pregnant Women: HBV immunoglobulin,
HAV vaccine, and HBV vaccine are approved
for use during
pregnancy.

Vertical Transmition:
• HAV is not transmitted to the fetus in utero
but may be transmitted to the neonate during
delivery or during the postpartum period
(fecal-oral route .
• The risk of HBV vertical transmission is 10 %
in mothers with negative HBeAg and positive
HBsAb while it is 90% in those with positive
HBeAg. Neonatal HBV infection increase with
increasing gestation.
• Universal screening of pregnant women for
HBsAg is performed to reduce perinatal
transmission of hepatitis B virus.

• Neonatal prophylaxis: Infants of HBsAg-
positive mothers should receive hepatitis
B immune globulin immunoprophylaxis
at birth and hepatitis B vaccine at one
week, one month and six months after
birth .
• This regimen reduces the incidence of
hepatitis B virus vertical transmission to
zero to 3%.
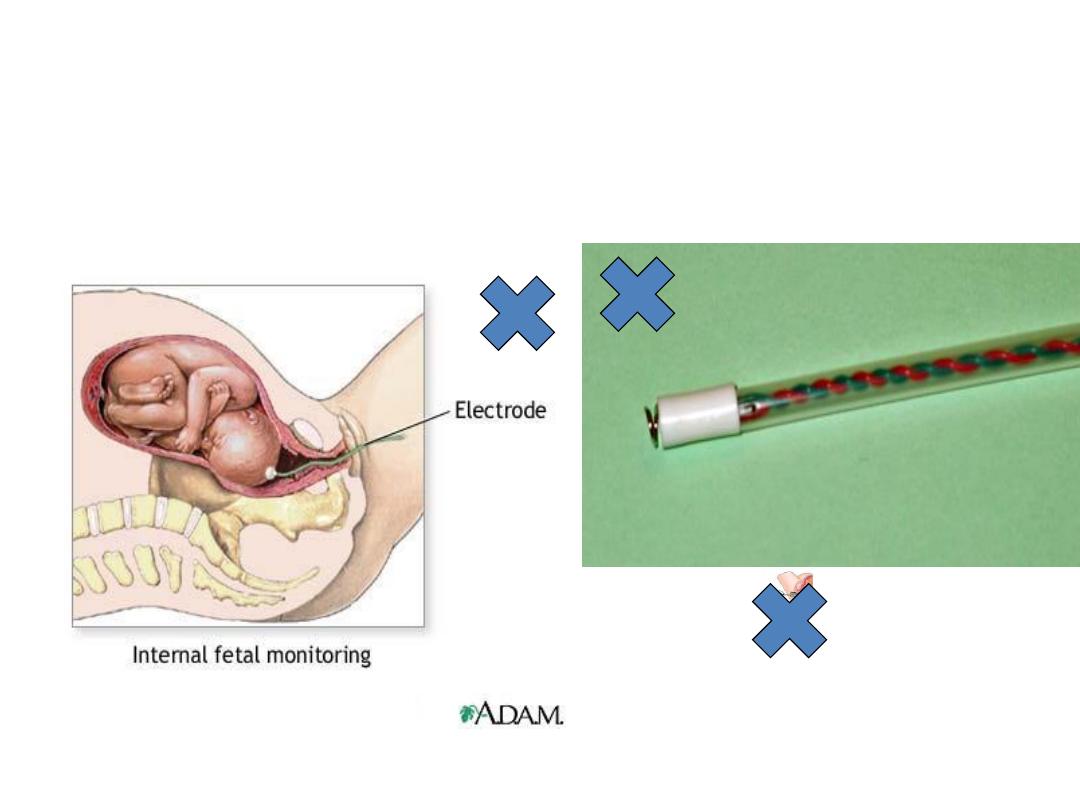
• Delivery by cesarean section is not recommended.
• Intrapartum fetal scalp electrode & fetal blood
sampling should be avoided.
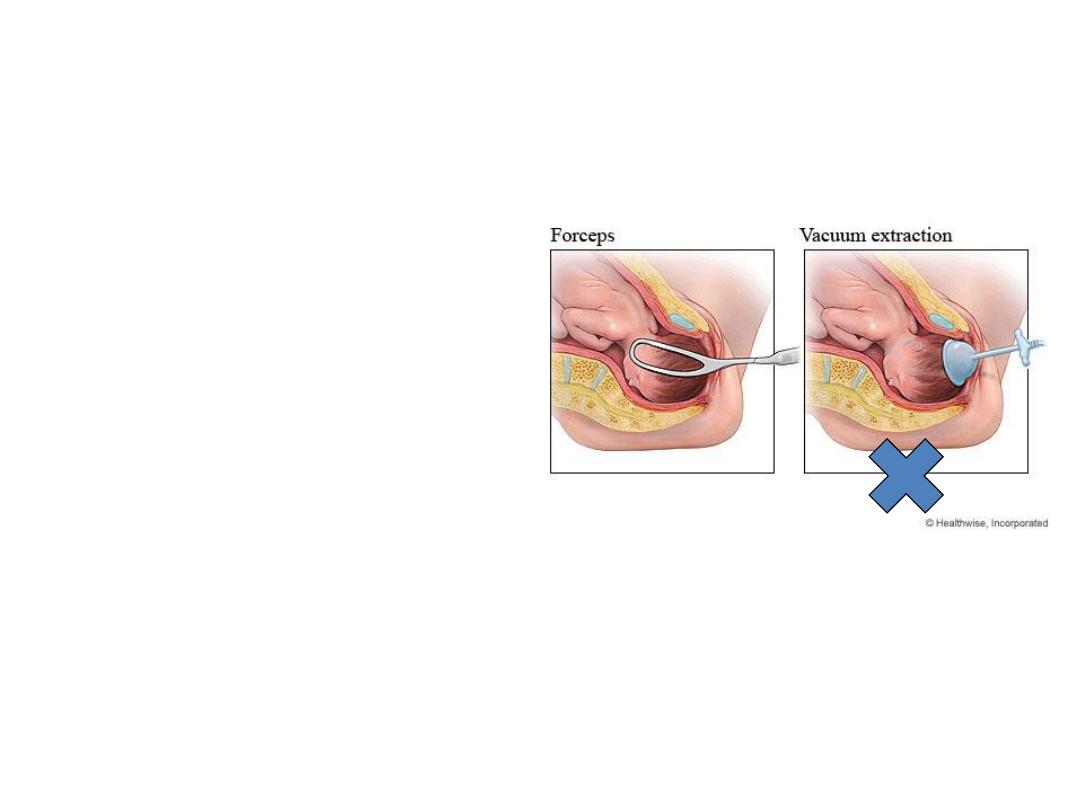
• If instrumental delivery is needed,
forceps rather than ventouse is
appropriate.
• With appropriate hepatitis B
immunoprophylaxis, breast-feeding poses
no additional risk for maternal to child
transmission

Asthma in Pregnancy

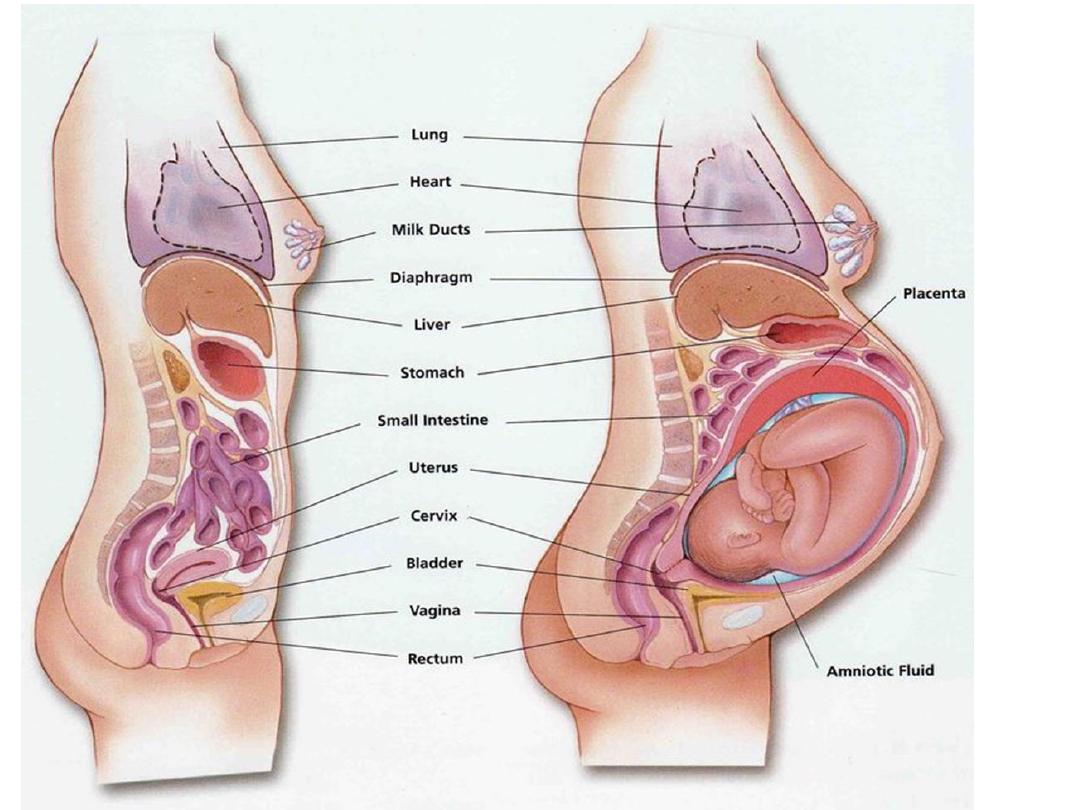
Physiological changes in pregnancy
• Dyspnea is experienced by approximately half of all
pregnant women by 20 weeks gestation because of
high progesterone levels which acts via the
Hypothalamus to increase respiratory drive.
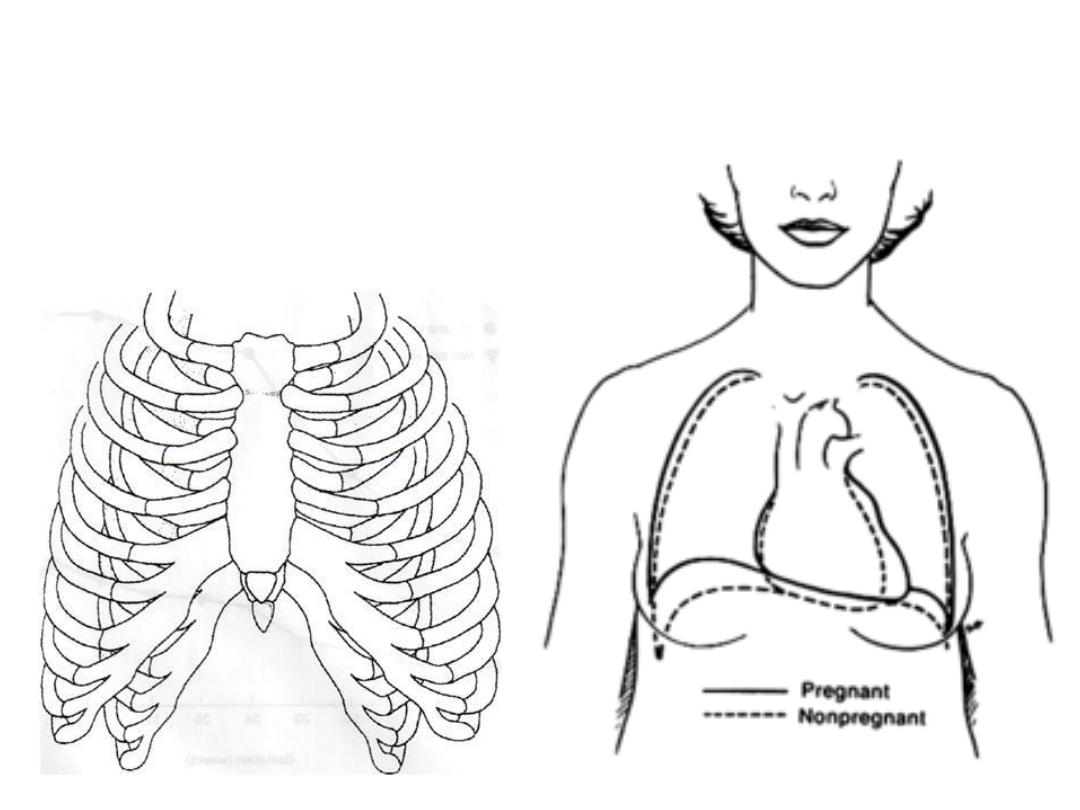
• Anatomically, the lower chest wall circumference
increases by 5-7 cm, the diaphragm is elevated 4-5
cm by term & the costal angle widens. These
changes occur due to the pressure from the expanding
uterus & the relaxation of thoracic ligaments.

Asthma in Pregnancy
• The prevalence of asthma in pregnancy is about 3 –12 per
cent.
Effect of pregnancy on asthma severity:
• asthma remains stable in one-third of women, worsens in
another third and improves in the remaining third.
• most episodes occur between 24 and 36 weeks of pregnancy
• The potential benefit of pregnancy-induced immune system
modulation & progesterone-mediated bronchodilatation
may be opposed by the reluctance of patient & physician to
treat asthma for the fear of harming the fetus through drug
exposure.

The effect of asthma on pregnancy:
• Severe & poorly controlled asthma have a
detrimental effect on pregnancy including:
• intrauterine growth restriction
• hypertensive disorders
• preterm labour
• intrauterine fetal death.

• Labour and delivery : are not usually affected by
asthma and attacks are uncommon in labour.
• Postpartum, there is no increased risk of exacerbations
and those whose asthma deteriorated during pregnancy
have usually returned to pre-pregnancy levels by three
months after birth.

Management of asthma in pregnancy:
• Same as in non-pregnant patient. Prevention is the
key & known triggers of exacerbations should be
avoided .
• Short-acting & long-acting beta2-agonists, inhaled
steroids & theophylline can be used in pregnancy.
These drugs will suffice for mild to moderate
asthmatics
• Epinephrine should be avoided in the pregnant
patient. it can lead to possible congenital
malformations, fetal tachycardia, and
vasoconstriction of the uteroplacental circulation

• Women with more severe asthma who have
stabilized on leukotriene receptor antagonist
may continue them through out pregnancy.
• Prednisolone is the oral steroid of choice in
pregnancy, as 88 % of it is metabolized by the
placenta, limiting fetal exposure.
The teratogenic risk & possible harmful fetal
effects of maternal steroid treatment remain an
area of controversy.

Managing pregnancy in asthmatic patients:
• Well-controlled mild to moderate asthmatics will
have a normal out come with standard antenatal
care. For those with poorly controlled or severe
asthma , care should be multidisciplinary.
• Baseline investigations, such as peak flow
measurements should be obtained at booking.
• Medical treatment should be optimized, with
repeated reassurance about the use of necessary
drugs in pregnancy.
• Women taking Prednisolone should be screened
for glucose intolerance

Labour & delivery:
• Parenteral steroid cover may be needed for those who are on
regular steroids
• regular medications should be continued throughout labour .
• bronchoconstrictors, such as ergometrine or prostaglandin
F2α, should be avoided.
• Adequate hydration is important.
• regional anaesthesia favoured over general, to decrease the
risk of bronchospasm, provide adequate pain relief and to
reduce oxygen consumption and minute ventilation.

• Breast feeding is not contraindicated with any
of the medications used although high-dose
oral steroid use ( ≥ 40 mg per day )carries a
risk of neonatal adrenal suppression
