Macrocytic Anaemia ( Megaloblastic and Non-Megaloblastic)
In macrocytic anaemia the red cells are abnormally large (mean corpuscular volume, MCV
>100fL).
—
There are several causes of marocytosis but they can be broadly subdivided into
megaloblastic and non megaloblastic based on the appearance of developing
erythroblasts in
the bone marrow and red cells morphology in the peripheral blood
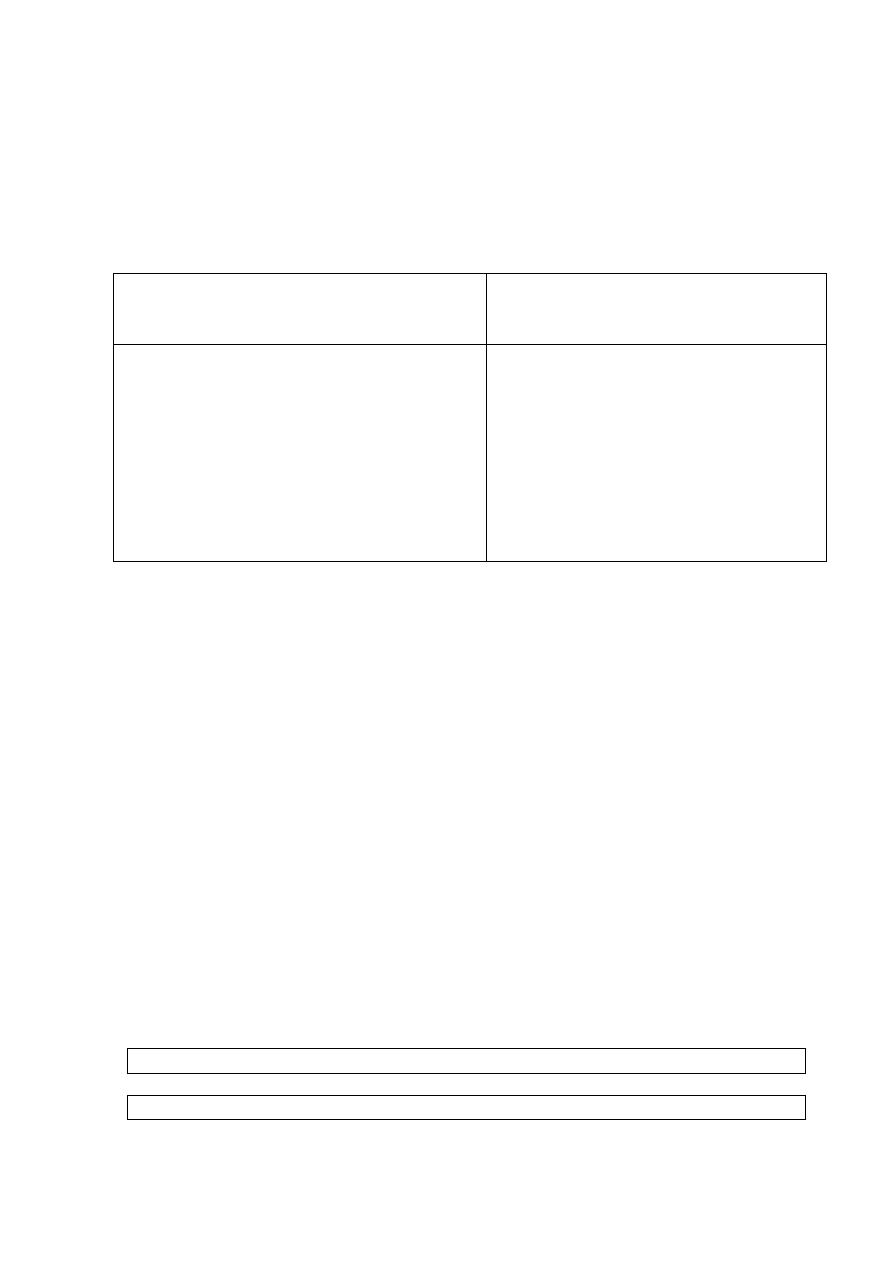
Causes of macrocytosis (MCV>100Fimto liter )
Non megaloblastic
Not related to B12/folate deficiency
Megaloblastic:
Impaired DNA formation due to lack of, B12 or
folic
acid
Physiological: Pregnancy and Infants
Pathological: Alcohol, Liver disease,
MDS, Myxodema
Reticulocytosis (Acute haemolytic anaemia)
Neonates
Round red cells shape
Normal bone marrow
Vitamin B12 deficiency, Folale deficiency
Defective Vitamin B12 or folate metabolism
Transcobalamin II deficiency
Defects of DNA synthesis
Ovale red cells shape
Megaloblastic maturation of bone marrow
hemopoietic precursors
Megaloblastic anaemias (MGBA)
Are anaemia with large RBC (ovalocytes,MCV>100fl) in the peripheral, and large
erythroid cells (megaloblast) in the bone marrow. Usually associated with leukopenia
with hyper segmented neutrophils and thrombocytopenia
Megaloblastic anemias result from conditions in which nucleic acid synthesis is
abnormal, due to vitamin B12 and Folate deficiency result in failure or delayed of
mitotic division
Biochemichal basis of megaloblastic anaemia:
Vitamin B12 and Folic acid play role as cofactors in the conversion of deoxy—uridine
monophosphate (dUMP) to deoxy—thymidine (dTMP), an essential step in the synthesis of
DNA
Folate is required in one of its coenzyme forms, 5,IO-methylene tetrahydrofolate (THF)
polyglutamate, in the synthesis of thymidine monophosphate from its precursor
deoxyuridine monophosphate.
Vitamin BI2 is needed to convert methyl THF, which enters the cells from plasma, to THF,
from which polyglutamate forms of folate are synthesized.
Dietary folates are all converted to methyl THF (a monoglutamate) by the small intestine.
Dietary folates (In the small intestine) → MTHF in the plasma → in the cells cytoplasm reduced to THF by B12 as Co—enzyme
THF
→5, 10-methylene THF →dUMP→DTMP→DTDP→DTTP→DNA Synthesis
When DNA synthesis is delayed causing delayed nuclear maturation and decrease number of
mitotic division result in decrease of red cells production, and erythropoiesis changes from
normoblastic to megaloblastic .
Also Megaloblast late erythroid precursors cells undergo intramedullary (in the bone
marrow) death or hemolysis and this will aggravate the anaemia and producing mild
elevation in serum indirect bilirubin (jaundice) and lactate dehydrogenase.
Causes of folate deficiency.
Causes of vitamin B12
deficiency
A. Nutritional: old age, poverty, goat's milk
B. Malabsorption: gluten-induced enteropathy
extensive jejunal resection or Crolm's disease
C. Excess utilization
1,Physiological: Pregnancy and lactation.
2. Patilological
Haematological diseases: chronic haemolytic
anaemias, Leukaemia.
Inflammatory diseases , psoriasis, exfoliative
dermatitis,
Drugs, Anticonvulsants,
alcoholism,
Nutritional (vegans)
Malabsorption
A. Gastric causes
1.Pernicious anaemia
2,Total or partial gash'ectomy
B. Intestinal causes
diverticulosis, blind-loop,
Ileal resection and Crohn's
disease
Congenital selective
malabsorption with proteinuria
Fish tapeworm
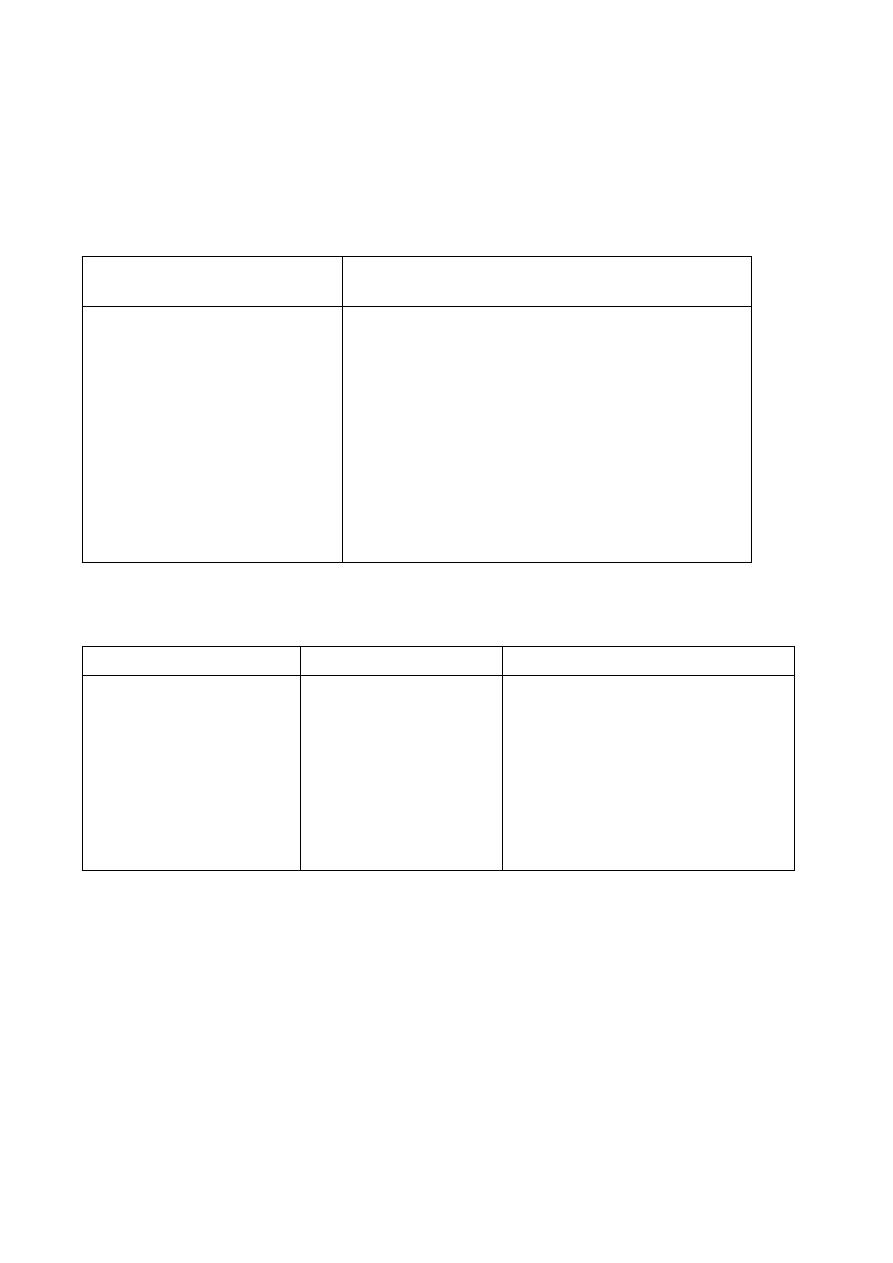
B12 and folic Acid nutritional aspects
Folic acid
B12
200-250 µg/day
liver, greens and yeast
Easily destroyed
100-150 µg/day
10-12 mg (sufficient for 4 months)
Duodenum and jejlUlum
Conversion to methyltetrahydrofolate
7-30µg/day
Vegetable diet ,Animal
Little effect
1-2 µg/day
2-3 mg (sufficient for 2-4
years)
Ileum
Intrinsic factor
Normal daily dietary intake
Main foods
Effect of Cooking
Minimal daily requirement
Body stores
Absorption Site
Mechanism
Laboratory feature of megaloblastic anaemia:
A. Hematologial:
1; low Hct, low Hb, Low red cells count, High MCV>100
low WBC (neutrophils), low platelets
2. Peripheral blood show: . Macrocytes with ovale shape red cells, hypersegmented
neutrophils (>5lobes), low platelets count
Low reticulocytes count which is also seen in IRON deficiency anaemia, aplastic
anaemia , anaemia of chronic disorders and pernicious anaemia.
3. Bone marrow hypercellular with hemopoietic precursors show:
a. Erythroid precursors macroerythroblast show open stippled chromatin and mature
hemoglobin in the cytoplasm. (nuclear cytoplasmic asynchrony).
b. Myeloid precursors show giant meatamyelocytes and band cells,
c. megakaryocytes show hypepolyploidy (increase number of nuclear lobes >16 lobe)
B. Biochemichal investigations
1. increase indirect bilirubin and LDH (lactate dehydrogenase)
2. Increase homocystein in blood and urine
3. Assay of serum B12/folate, and red cells folate
a. In B12 deficiency result low serum B12 and normal serum folate,
low red cells folate
b. In folate deficiency result normal serum B12 and low serum folate ,
low red cells folate
Investigation of B12 and folic acid
In Folate deficiency
In B12 deficiency
Test
Normal
Low
Low
Low
Normal or raised
low
Serum vitamin BI2
Serum folate
Red cell folate
Pernicious anemia: failure of B12 binding from diet or failure of it absorption
This is caused by autoimmune antibodies attack the gastric mucosa leading to atrophy of the stomach. The
wall of the stomach becomes thin, with chronic inflammatory cells infiltration, a plasma cell and lymphocytes
There is achlorhydria and absent secretion of IF (B12—binding factor)
More females than males are affected (1.6 : 1), with a peak occurrence at 60 years, and there may be
associated other autoimmune disease including the autoimmune polyendocrine syndrome (Table 4.4).
The disease is common in northern Europeans and tends to occur in families
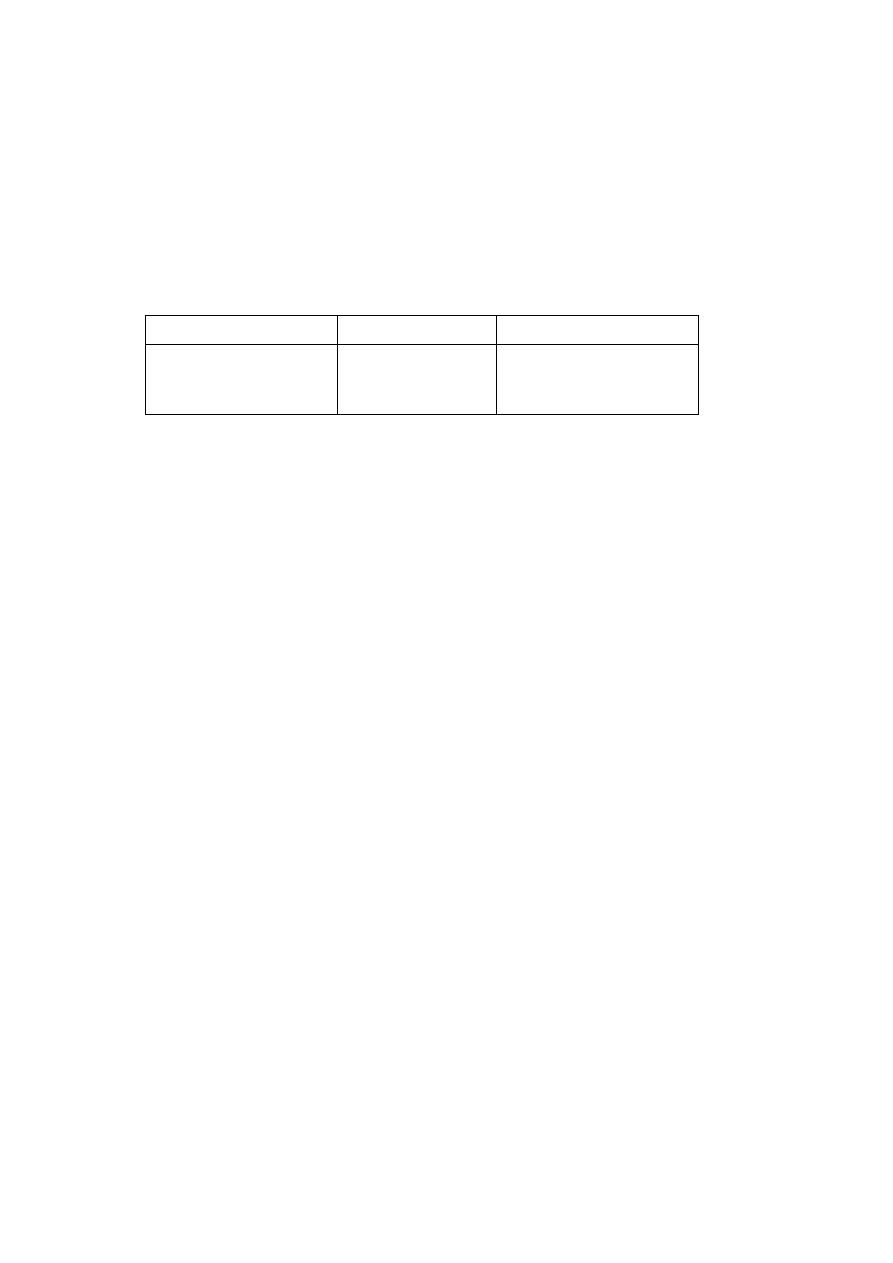
Antibodies (investigated in the serum of the patient)
1. 95% of patients show parietal cell antibody however it is not specific only for Pernicious .anemia
2. 50% type I or blocking antibody to IF which inhibits IF binding to B12 – ( it is the most specific for
pernicious anaemia)
3. 35% show a second (type II or precipitating) antibody to IF receptors which inhibits its ileal binding site.
Diagnosis of pernicious anemia:
1. Megaloblastic anemia on peripheral blood and bone marrow with positive biochemical investigations
2. Investigation of Antibody in the serum of the patients
3. Gastric endoscopy and biopsy show chronic atrophic gastritis
4. history of chronic dyspepsia and indigestion
