Femoral Shaft Fractures
Dr. Jamal Al-Saidy
M.B.Ch.B. .F.I.C.M.S
Mechanism of injury
This is usually a fracture of young adults and results from a high energy injury.
Diaphyseal fractures in elderly patients should be considered pathological until
proved otherwise.
In children under 4 years the possibility of physical abuse must be kept in mind.
A spiral fracture is usually caused by a fall in which the foot is anchored while a
twisting force is transmitted to the femur.
Transverse and oblique fractures are more often due to angulation or direct
violence.
With severe violence (often a combination of direct and indirect forces) the
fracture may be comminuted, or the bone may be broken in more than one place
(a segmental fracture).
Pathological anatomy & classification
(Winquist, Hansen et al. 1984).
In Fracture displacement often follows a predictable pattern dictated by the pull
of muscles attached to each fragment:
In proximal shaft fractures the proximal fragment is flexed,
abducted and externally rotated because of gluteus medius
and iliopsoas pull; the distal fragment is frequently
adducted.
In mid-shaft fractures the proximal fragment is again flexed
and externally rotated but abduction is less marked.
In lower third fractures the proximal fragment is adducted
and the distal fragment is tilted by gastrocnemius pull.
The soft tissues are always injured and bleeding from the perforators of the
profunda femoris may be severe. Over one litre may be lost into the tissues and,
in the case of bilateral femoral shaft fractures, the patient can become
hypotensive quickly if not adequately resuscitated.
Beware of the fracture at the junction of the middle and distal thirds of the
femoral shaft – it can be responsible for damaging the femoral artery in the
adductor canal.
Femoral shaft fractures classification:- Winquist’s classification reflects the observation
that the degrees of soft-tissue damage and fracture instability increase with increasing
grades of comminution:-
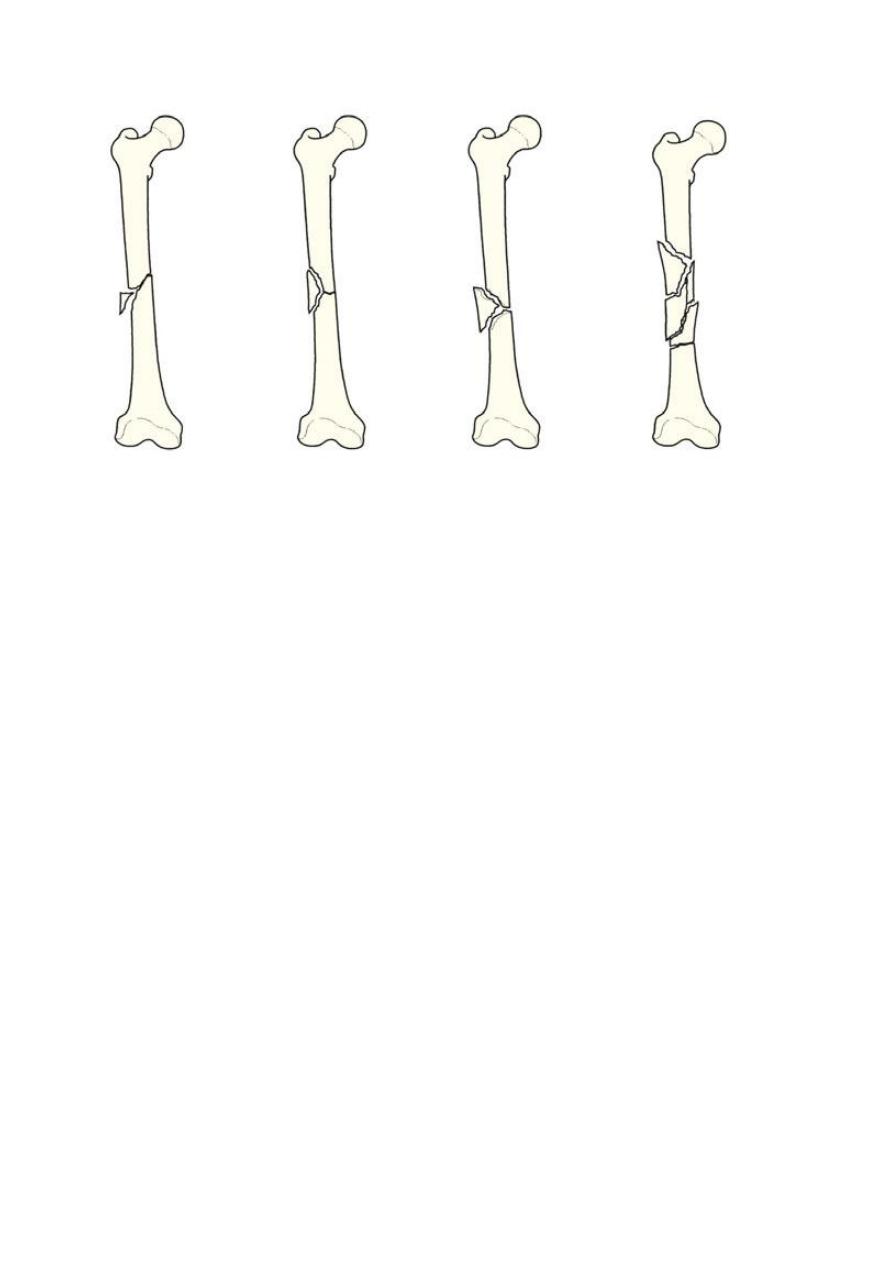
o Type 1 : there is only a tiny cortical fragment.
o Type 2 : the ‘butterfly fragment’ is larger but there is still at least 50 per cent
cortical contact between the main fragments.
o Type 3 : the butterfly fragment involves more than 50 per cent of the bone width.
o Type 4 is essentially a segmental fracture.
Clinical features
There is swelling and deformity of the limb, and any attempt to move the limb is
painful.
Careful clinical scrutiny is necessary to exclude neurovascular problems and other
lower limb or pelvic fractures.
An ipsilateral femoral neck fracture occurs in about 10 per cent of cases and, if
present, there is a one in three chance of a significant knee injury as well.
The combination of femoral shaft and tibial shaft fractures on the same side,
producing a‘floating knee’, signals a high risk of multi-system injury in the
patient.
The effects of blood loss and other injuries, some of which can be life-
threatening, may dominate the clinical picture.
X-ray
It may be difficult to obtain adequate views in the Accident and Emergency Room
setting, until better facilities and easier patient positioning are possible.

But never forget to X-ray the hip and knee as well.
Chest x-ray is useful as there is a risk of adult respiratory distress syndrome
(ARDS) in those with multiple injuries.
Emergency treatment
Traction with a splint is first aid for a patient with a femoral shaft fracture and It
is applied at the site of the accident, and before the patient is moved.
A Thomas splint, or one of the modern derivations of this practical device, is
ideal: the leg is pulled straight and threaded through the ring of the splint; the
shod foot is tied to the cross-piece so as to maintain traction and the limb and
splint are firmly bandaged together.
This temporary stabilization helps to control pain, reduces bleeding and makes
transfer easier.
Shock should be treated; blood volume is restored and maintained, and a
definitive plan of action instituted as soon as the patient’s condition has been
fully assessed.
Definitive treatment
The patient with multiple injuries The association of femoral shaft fractures with
other injuries, including head, chest, abdominal and pelvic trauma, increases the
potential for developing fat embolism, ARDS and multi-organ failure.
The risk of systemic complications can be significantly reduced by early
stabilization of the fracture, usually by a locked intramedullary nail.
It is thought the trauma of surgery and blood loss induces inflammatory changes
that may increase both morbidity and mortality – this phenomenon is called ‘the
second hit’, referring to a second episode of trauma, albeit surgical, on the
patient.
Consequently, in the multiplyinjured patient, particularly one with severe chest
trauma, prompt stabilization with an external fixator may be wise; the fixator can
be exchanged for an intramedullary nail when the patient’s condition stabilizes.
The timing of this second procedure is problematic, the safe to perform ‘
second hit’ interventions around 5–7 days after admission, the earlier the
operation is performed, the lower the risk.
In the patient who spends a protracted period in the intensive care unit, it may
be safer to use external fixation as definitive treatment, perhaps with a return to
theatre later to allow insertion of new pins to increase the stability of the
construct.
Treatment Of Isolated Femoral Shaft Fracture
Traction:-
Traction can reduce and hold most fractures in reasonable alignment, and Joint
mobility can be ensured by active exercises. The drawback is the length of time
spent in bed (10–14 weeks for adults)
plaster Spica or in the case of lower 1/3rd fractures – Functional Bracing when
the fracture is‘sticky’, usually around 6–8 weeks.
o Indications for traction are
(1) fractures in children
(2) contraindications to anaesthesia
(3) lack of suitable skill or facilities for internal fixation.
o It is a poor choice for elderly patients, for pathological fractures and for
those with multiple injuries.
o Methods of traction
1) Skin traction for young children
2) (‘Gallows traction’) in infants less than 12 kg in weight are
most easily managed by suspending the lower limbs from
overhead pulleys, but no more than 2 kg weight should be
used and the feet must be checked frequently for circulatory
problems
3) Skeletal traction for adults and older adolescents: through a
pin or Kirschner wire behind the tibial tubercle. Traction (8–10
kg for an adult) is applied over pulleys at the foot of the bed.
the advantages for that is allowing freer movement in bed,
Once the fracture is sticky (at about 8 weeks in adults) traction can
be discontinued and the patient allowed up and partial
weightbearing in a cast or brace. until the fracture has consolidated
(16–24 weeks).
Traditional Plate and screw fixation : Plating is an easy way of obtaining accurate
reduction and firm fixation but may be associated with a high complication rate, this is
usually occurred when the plates are applied through a wide open exposure of the
fracture site . Such extensive surgery damaged the healing potential and led to tardy
union and implant failure.
Minimally invasive plate osteosynthesis (MIPO) However, the plates are inserted
through short incisions and placed in a submuscular plane, rather than deep to
periosteum; an indirect (closed) reduction of the fracture is done.
o [The main indications for plates are
(1) fractures at either end of the femoral shaft, especially those with
extensions into the supracondylar or pertrochanteric areas
(2) a shaft fracture in a growing child.
(3)a fracture with a vascular injury which requires repair.
Intramedullary nailing
o Intramedullary nailing is the method of choice for most femoral shaft fractures.
o It should not be attempted unless the appropriate facilities and expertise are
available.
o The Stability is improved by using interlocking screws through a perforators near
each end so that can be inserted transversely at the proximal and distal ends;
this controls rotation and length, and ensures stability even for Subtrochanteric
and distal third fractures.
o Open medullary nailing is a feasible alternative where facilities for closed nailing
are lacking.
External fixation
The main indications for external fixation are:-
(1) treatment of severe open injuries
(2) management of patients with multiple injuries
(3) severe bone loss by the technique of bone transport.
(4) treating femoral fractures in adolescents.
Treatment of open femoral fractures
o Open femoral fractures should be carefully assessed for
(1) Skin loss
(2) Wound contamination
(3) Muscle ischaemia
(4) Injury to vessels and nerves.
o The immediate treatment is similar to that of closed fractures; in addition, the
patient is started on intravenous antibiotics.
o The wound will need cleansing: it should be extended t, the contaminated areas
and dead tissue must be excised and the entire area should be washed
thoroughly.
o Stabilization of open femoral shaft fractures is best achieved with locked
intramedullary nails unless there is heavy contamination or bone loss – in which
case external fixation (if necessary with the capacity to deal with bone loss
through distraction osteogenesis) is preferable.
Complex injuries
Femoral fractures Associated With Vascular Injury
o Warning signs of an associated vascular injury are
(1) excessive bleeding or haematoma formation
(2) paraesthesia, pallor or pulselessness in the leg and foot.
o Do not accept ‘arterial spasm’ as a cause of absent pulses
o The fracture level on x-ray will indicate the region of arterial damage and
arteriography may only delay surgery to re-establish perfusion.
o The warm ischaemia times is greater than 2–3 hours by the time it must not be
exceeds 4– 6 hours, and so the salvage may not be possible and the risk of
amputation rises. This means that diagnosis must be prompt and reestablishing
perfusion a priority; fracture stabilization is secondary.
Femoral fracture Associated With Knee Injury
o Frequently accompanied by injury to the ligaments of the knee.
o Direct blows to the knee from the dashboard of a car in an accident will damage
knee ligaments as well as break the femoral shaft and femoral neck – this triad
of problems should be recognized.
o
‘
Floating Knee
’
o Ipsilateral fractures of the femur and tibia may leave the knee joint ‘floating’.
This is a very serious situation, and both fractures will need immediate
stabilization.
Combined Neck And Shaft Fractures
o The most important thing is diagnosis: always examine the hip and obtain an x-
ray of the pelvis
Pathological Fractures
o Fractures through metastatic lesions should be fixed by intramedullary nailing.
o A short life expectancy is not a contraindication.
o ‘Prophylactic fixation’ is also indicated if a lytic lesion is
(a) Greater than half the diameter of the bone
(b) Longer than 3 cm on any view
(c) Painful, irrespective of its size.
o Paget’s disease, fibrous dysplasia or rickets may present a problem. The femur
is likely to be bowed and an osteotomy to straighten the femur may be
necessary to allow a nail to be inserted fully .
Periprosthetic Fractures
o Femoral shaft fractures around a hip implant are uncommon; they may happen .
o If the prosthesis is worn or loose, it should be removed and replaced by one with
a long stem, thereby treating both problems.
o If the primary implant is neither loose nor worn it can be left in place and the
fracture treated by plate fixation with structural allografts bridging the fracture.
Complications Of Femoral Shaft Fractures
EARLY
o Shock :- One or two litres of blood can be lost even with a closed
fracture, and if the injury is bilateral shock may be severe. Prevention is
better than cure; most patients will require a transfusion.
o Fat embolism and ARDS:- Fracture through a large marrow- filled cavity
almost inevitably results in small showers of fat emboli being swept to
the lungs. This can usually be accommodated without serious
consequences, but in some cases (and especially in those with multiple
injuries and severe shock, or in patients with associated chest injuries) it
results in progressive respiratory distress and multi-organ failure (adult
respiratory distress syndrome). Blood gases should be measured if this is
suspected and signs such as shortness of breath, restlessness or a rise in
temperature or pulse rate should prompt a search for petechial
haemorrhages over the upper body, axillae and conjunctivae. Treatment
is supportive, with the emphasis on preventing hypoxia and maintaining
blood volume.
o Thromboembolism :- Prolonged traction in bed predisposes to
thrombosis. Movement and exercise are important in preventing this,
but high-risk patients should be given prophylactic anticoagulants as
well. Vigilance is needed and full anticoagulant treatment is started
immediately if thigh or pelvic vein thrombosis is diagnosed.
o Infection:- In open injuries, and following internal fixation, there is
always a risk of infection. Prophylactic antibiotics and careful attention
to the principles of fracture surgery should keep the incidence below 2
per cent.
LATE
o Delayed union and non-union:- The time-scale for declaring a delayed
or non-union can vary with the type of injury and the method of
treatment. If there is failure to progress by 6 months, as judged by serial
x-rays, then intervention may be needed.
o Malunion :- Fractures treated by traction and bracing often develop
some deformity; no more than 15 degrees of angulation should be
accepted. Even if the initial reduction was satisfactory, until the x-ray
shows solid union the fracture is too insecure to permit weightbearing;
the bone will bend and what previously seemed a satisfactory reduction
may end up with lateral or anterior bowing. and therefore post-
operative assessment is important and so correction may be needed.
Shortening is seldom a major problem unless there was bone loss; if it
does occur, treatment will depend on the amount and its clinical impact
– sometimes all that is needed is a built-up shoe.
o Joint stiffness:- The knee is often affected after a femoral shaft fracture.
The joint may be injured at the same time, or it stiffens due to soft-
tissue adhesions during treatment; hence the importance of repeated
evaluation and early physiotherapy.
o Refracture and implant failure:- Fractures which heal with abundant
callus are unlikely to be refracture. By contrast, in those treated by
internal fixation, callus formation is often slow and meager. With
delayed union or non-union, the integrity of the femur may be almost

wholly dependent on the implant and sooner or later it will fail. If a
comminuted fracture is plated, bone grafts should be added and
weightbearing delayed so as to protect the plate from reaching its
fatigue limit too soon. Intramedullary nails are less prone to break. the
break usually occurs through the screw-hole closest to the fracture.
Treatment consists of replacing the nail and adding bone grafts. In
resistant cases, the fracture site may need excising (as viability of the
bone ends is poor) followed by distraction osteogenesis which
simultaneously stabilizes the limb and deals with the length discrepancy.
THANK YOU
Dr. Jamal Al-Saidy
M.B.Ch.B. .F.I.C.M.S
