FUNGAL INFECTION
Prepared by : Mustafa moniem sayedSupervised by : Dr Ali Alzubaydi
What Is Fungus
Fungus is a member of large group eukaryoticEukaryotic is an organism whose cells contain complex structures enclosed with membranes
Cell wall of a fungus contains chitin .
Oral Candidosis
Candida spp are fungi that have a wide distribution and that frequently form part of the commensal flora of the human body. Swabs taken from the skin, gut, vagina, or mouth of an apparently healthy individual all may show the presence of Candida species and, in particular, Candida albicans .Oral candidosis
Candida Species Involved In Oral CandidosisC. albicans*(most frequently isolated species)C. tropicalisC. pseudotropicalis
C. glabrataC. kruseiC. parapsilosis
Symptoms of oral candidosis
Oral mucosal inflammation manifesting as an uncomfortable feeling,
Pain,
Erythema
Erosion
Taste abnormalities
Hyperplasia of the oral mucosa.
General Clinical features
Creamy white lesions on the tongue, inner cheeks, and sometimes on the roof of the mouth, gingivae and tonsilsSlightly raised lesions with a cottage cheese-like appearance
Redness, burning or soreness that may be severe enough to cause difficulty eating or swallowing
Slight bleeding if the lesions are rubbed or scraped
Cracking and redness at the corners of the mouth
A cottony feeling in the mouthLoss of taste
Redness, irritation and pain under dentures (denture stomatitis)
Oral thrush
Classification of oral candidosids
Primary oral candidoses (group 1)
Acute: pseudomembranous, erythematous
Chronic: pseudomembranous, erythematous, hyperplastic
Candida-associated lesions: Candida-associated denture-induced stomatitis, angular cheilitis, median rhomboid glossitis
Secondary oral candidosis (group 2)Oral manifestations of systemic mucocutaneous candidosis
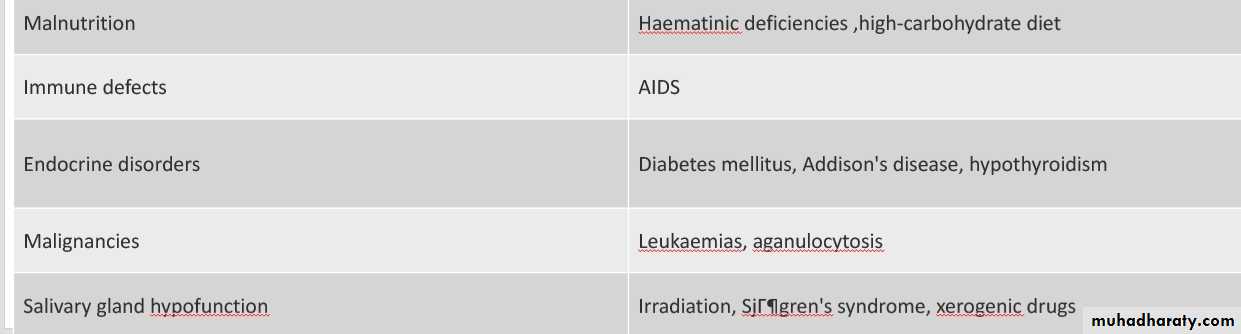
Predisposing factor for oral candidosis
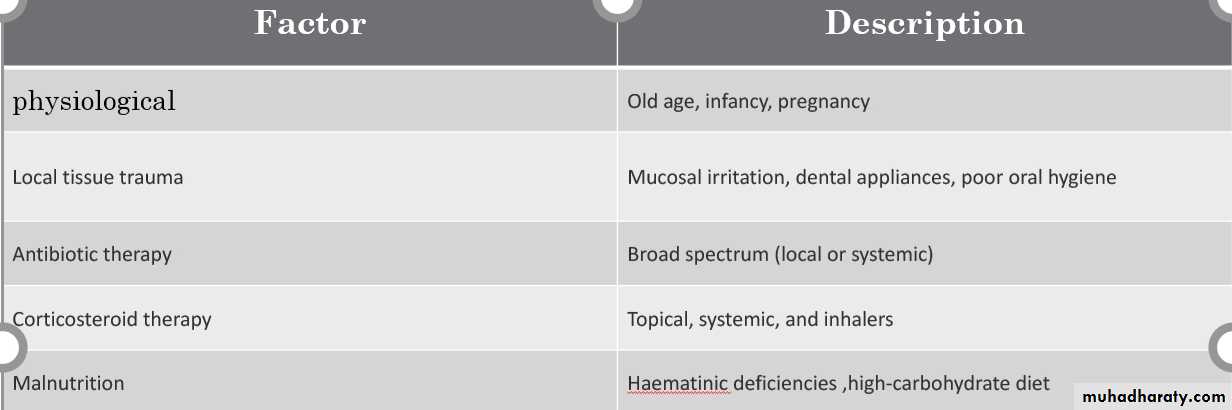
The laboratory diagnosis of candidosis
Oral lesionswab
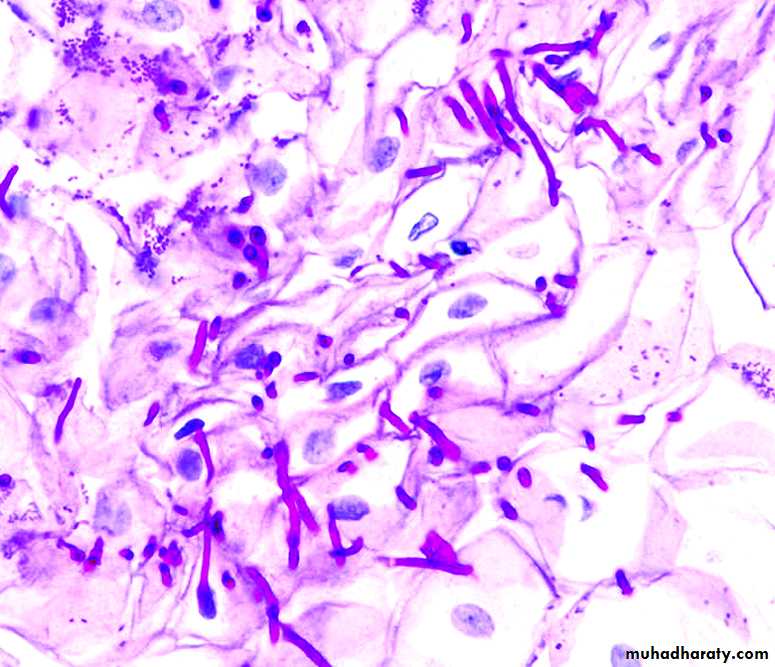
smear
Oral rinse
biopsy
Pseudomembranous
+
±
+
-
Erythematous
+
±
+
-
Hyperplastic
±
±
-
+
Candida-associated denture stomatitis (palate and denture)
+
+
+
-
• Angular cheilitis
+
+
-
-
Oral swab
Pseudomembranous candidiasis (oral thrush):
Characterized by white curd like pseudomembrane seen on the buccal mucosa, throat, tongue, or gingivaeRemoval of the membrane reveals an underlying erythematous mucosa
Acute erythematous candidiasis (acute atrophic oral candidiasis)
Present with burning sensation in the mouth or the tongue
The tongue may be bright red
Commonly seen after antibiotic therapy or inhaled steroid therapy
Chronic erythematous candidiasis (denture stomatitis or chronic atrophic candidiasis)
Seen as localized erythema in places where ill-fitting or inadequately cleaned dentures are wornChronic hyperplastic candidiasis
Seen as white patches or plaques which are firmly adhered to buccal mucosa, tongue, palate
Usually distributed on both sides
• Management
• Biopsy
• Eradication of predisposing factors, such as smoking
• Institution of appropriate antifungal therapy
Median rhomboid glossitis
Atrophic filiform papillae is seen in a symmetrical area anterior to the cicumvallate papillae of the tongue (1)Angular cheilitis
Seen as erythematous fissuring at corners of the mouth
Topical therapy
systemic therapyPseudomembranous candidiasis,erythrematous hyperplastic
• Amphotericin lozenges (10 mg)
• Nystatin pastilles (100 000 units)4 times daily , 1-4 weeks
• Fluconazole, 50–100 mg daily for 2 -3 weeks
• ittraconazole 150 mg daily for 2 weeks• Candida-associated denture stomatitis*
Amphotericin or nystatin (as above) remove denturesIf compliance poor:Miconazole gel applied to palatal surface of denture
4 times daily for 1-4 weeksMiconazole lacquer
Chlorhexidine 0.2% rinse, 4 times daily (do not use with nystatin)
• Systemic therapy is occasionally required
• Candida-associated angular cheilitis*Nystatin cream; apply to corners of mouth 3-4times daily, until resolutionIf microbial report not available or in case of mixed infection΅
Miconazole cream (or gel); apply 3-4 times daily to angles