Hemodynamic disorders
Dr. Zainab Waleed AzizUniversity of Ninevah
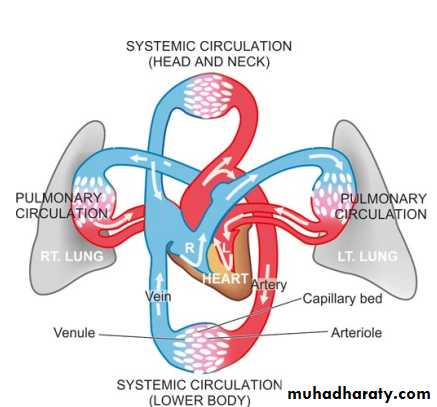
The principles of blood flow are called haemodynamicsHaemodynamic disturbances are considered under 2 broad headings:
I. Disturbances in the volume of the circulating blood. These include:hyperaemia and congestion
Haemorrhage
shock.
II. Circulatory disturbances of obstructive nature. These are:
thrombosis
Embolism
infarction
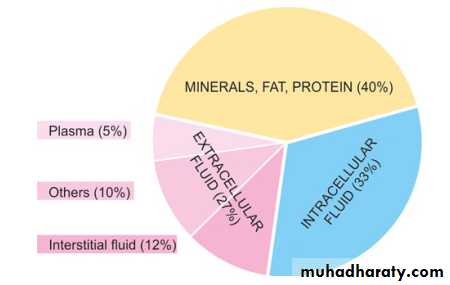
60% of lean body weight is water
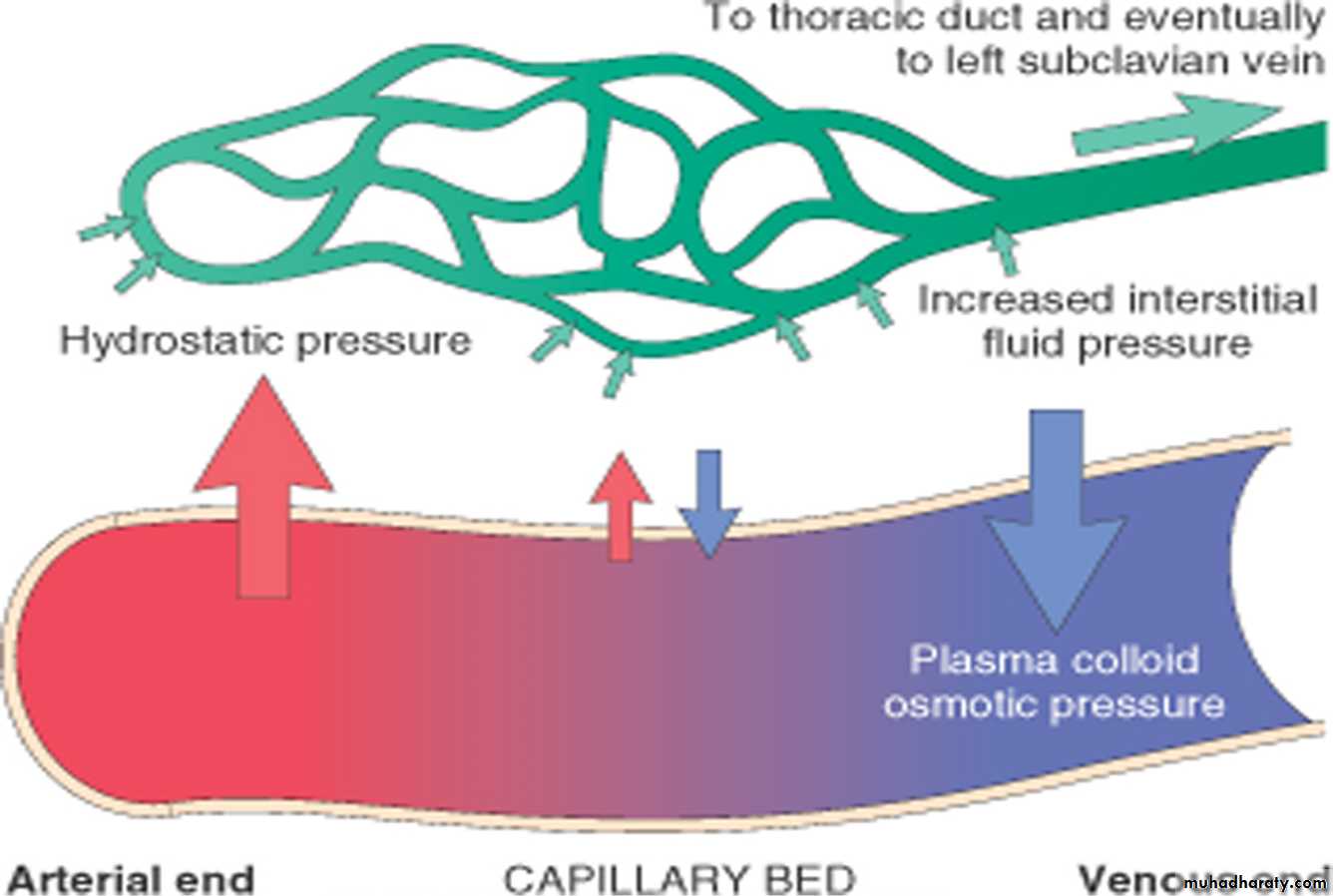
There are 2 opposing factors which govern the movement of the fluid between vascular & interstitial spaces:Normally , At the arterial end the hydrostatic pressure is greater than the osmotic pressure → fluid is forced out the capillaries , of the microcirculation.
The reverse occurs at the venous end & the fluid is attracted into the vessels.
So the exit of fluid into the interstitium from the arteriolar end of the microcirculation is nearly balanced by inflow at the venular end; a small residual amount of excess interstitial fluid is drained by the lymphatics, then to the blood stream via thoracic ductEdema
DefinitionAn abnormal and excessive accumulation of “free fluid” in the interstitial tissue spaces and serous cavities.
Free fluid in interstitial space: Commonly termed as oedema, the fluid lies free in the interstitial space between the cells and can be displaced from one place to another.
Free fluid in body cavities: Commonly called as effusion.
• Ascites ( peritoneal cavity)
• Hydrothorax or pleural effusion ( pleural cavity)
• Hydropericardium or pericardial effusion (pericardial cavity).
Pathogenesis of edema
Edema is caused by mechanisms that interfere with normal fluid balance of plasma, interstitial fluid and lymph flow. 1. Increased capillary hydrostatic pressure2. Decreased plasma oncotic pressure 3. Lymphatic obstruction4. Increased capillary permeability5. Sodium and water retention
INCREASED CAPILLARY HYDROSTATIC PRESSURE
A rise in the hydrostatic pressure at the venular end of the capillary, which is normally low , to a level more than the plasma oncotic pressure results in minimal or no reabsorption of fluid at the venular end, consequently leading to oedema.Examples:i) cardiac disease e.g. congestive cardiac failure, constrictive pericarditis.
ii) Ascites of liver disease e.g. in cirrhosis of the liver.iii) Passive congestion e.g. in mechanical obstruction due to thrombosis of veins of the lower legs, varicosities, pressure by pregnant uterus, tumours etc.
DECREASED PLASMA ONCOTIC PRESSURE
A fall in the total plasma protein level results in loweringof plasma oncotic pressure in a way that it can no longer counteract the effect of hydrostatic pressure of bloodExamples :i) Oedema of renal disease e.g. in nephrotic and nephriticsyndrome.ii) Ascites of liver disease e.g. in cirrhosis of the liver.iii) Oedema due to other causes of hypoproteinaemia e.g. inproteinlosing enteropathy
LYMPHATIC OBSTRUCTION
Normally, the interstitial fluid in the tissue spaces escapes by way of lymphatics. Obstruction to outflow of these channels causes localized edema, known as lymphoedema
Examples:i) Removal of axillary lymph nodes in radical mastectomy for carcinoma of the breast causing lymphoedema of the affected arm.ii) Pressure from outside on the main abdominal or thoracic duct such as due to tumours iii) Inflammation of the lymphatics as seen in flariasis (infection with Wuchereria bancrofti) results in chronic lymphoedema of scrotum and legs known as elephantiasis.iv) Milroy’s disease or hereditary lymphoedema is due to abnormal development of lymphatic channels. It is seen in families and the edema is mainly confined to one or both the lower limbs
INCREASED CAPILLARY PERMEABILITY
Capillary endothelium injury by toxins and their products (e.g. histamine, anoxia, venoms, certain drugs and chemicals) increase the capillary permeability causing leakage of plasma proteins into interstitial fluid. This, in turn, causes reduced plasma oncotic pressure and consequently producing edema called Inflammatory edema.Sodium and water retention
Derangement in normal regulatory mechanism of sodium and water balance result in increased capillary hydrostatic pressure which leads to the edema.Example is edema of renal disease e.g. in nephrotic and nephritic syndrome.
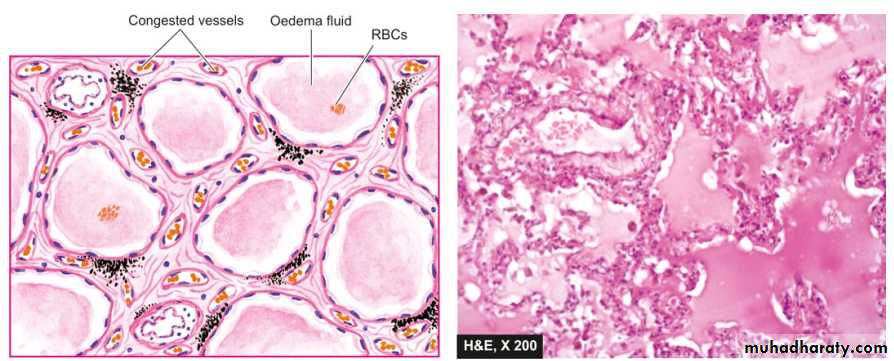
Morphology of edema
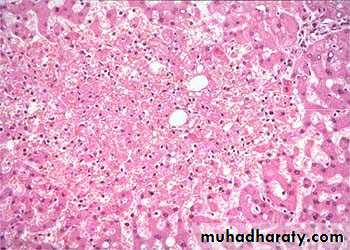
Grossly, the affected organ is enlarged and heavy.Microscopically, edema fluid may appear homogeneous, pale, eosinophilic, or may be deeply eosinophilic and granular.
Clinical classification of edema:
• Localised when limited to an organ or limb e.g. cerebral oedema, pulmonary oedema.2. Generalised (anasarca or dropsy) when it is systemic in distribution, particularly noticeable in the subcutaneous tissues e.g. renal oedema, cardiac oedema, hepatic oedema.
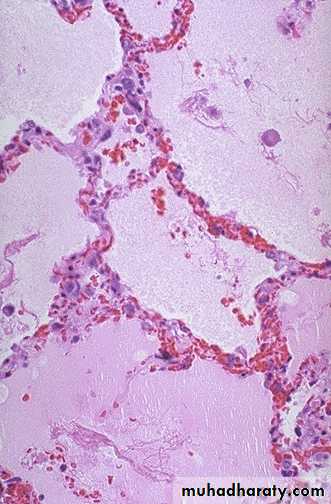
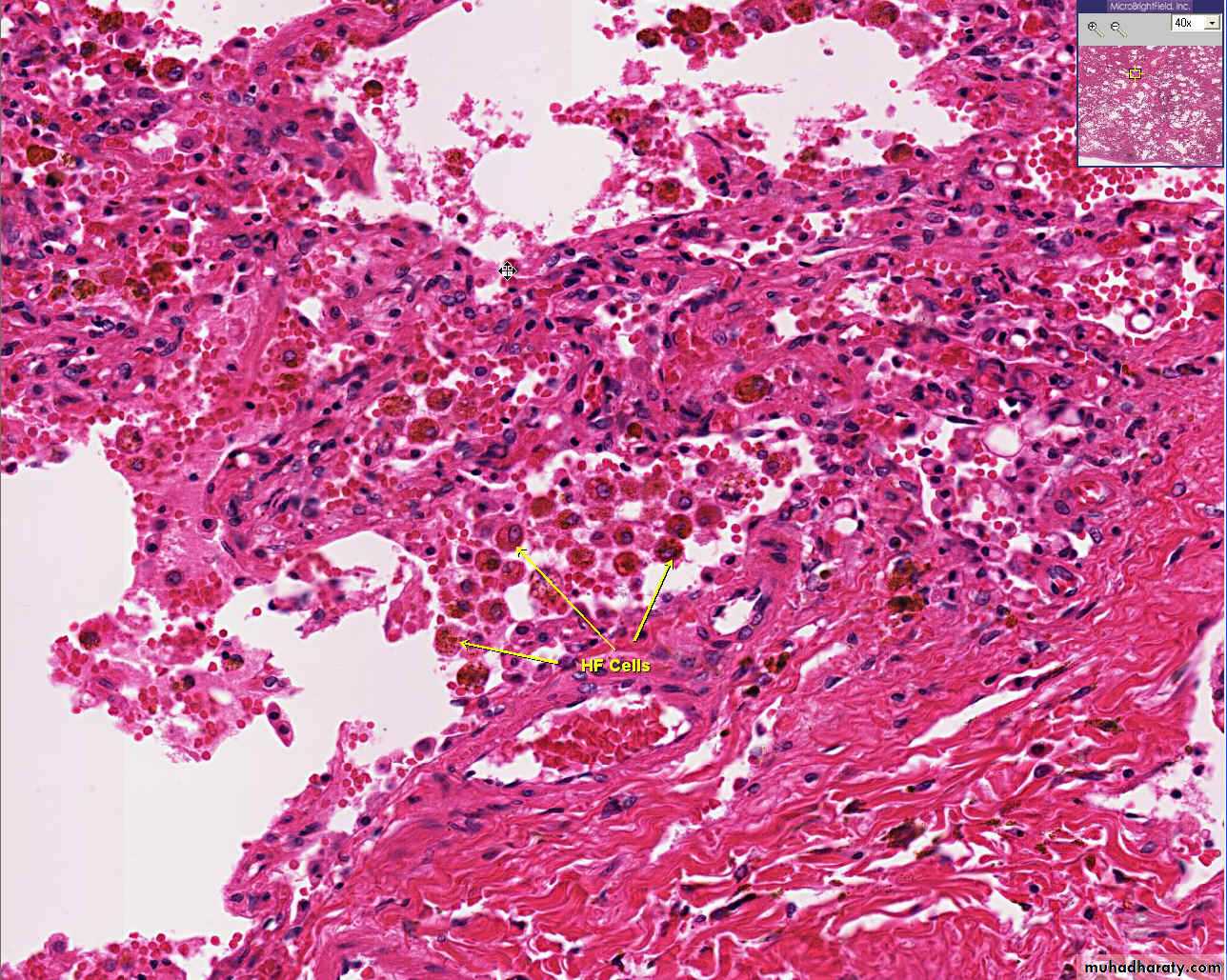
Pulmonary oedema. The alveolar capillaries are congested. The alveolar spaces as well as interstitium contain eosinophilic, granular, homogeneous and pink proteinaceous oedema fluid alongwith some RBCs and inflammatory cells.
Nature of accumulated fluid:
Transudateprotein poor fluid results from disturbance of Starling forces.
specific gravity < 1.012
protein content < 3 g/dl
Example: nephrotic syndrome
Exudate
protein rich fluid results from damage to the capillary wall.
specific gravity > 1.012
protein content > 3 g/dl
Example : inflammation
Hyperemia and congestion
Both terms indicate a localized increase in the volume of blood in a particular tissue.Hyperemia
- An active process resulting from an increased inflow of blood into a tissue because of arteriolar vasodilation.- commonly occurs in:
exercising skeletal muscle or acute inflammation.
- Affected tissue becomes red as there is engorgement with oxygenated blood.
Congestion
- A passive process resulting from impaired outflow of blood from a tissue.occurs systemically as in: cardiac failure
or locally as in isolated venous obstruction.
- Affected tissue appears blue-red due to accumulation of deoxygenated blood.
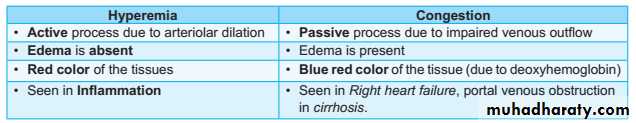
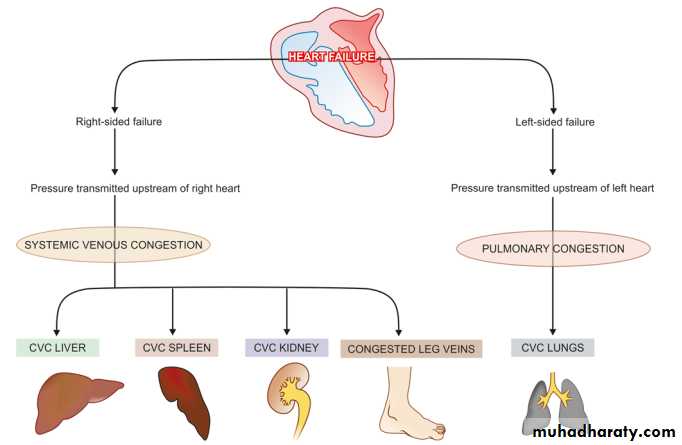
Hyperemia and congestion
Schematic representation of mechanisms involved in chronic venous congestion (CVC) of different organs.
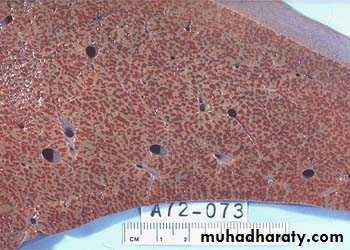
Cut surface:
hemorrhagic & wetMorphological changes in venous congestionGrossly:
The lung has a red, hyperemic cut surface, reflecting passive congestion, due to increased hydrostatic pressure, as seen in cases of left heart failure. The transudate, mixed with air in the alveoli, gives the cut surface a frothy appearance
Microscopically
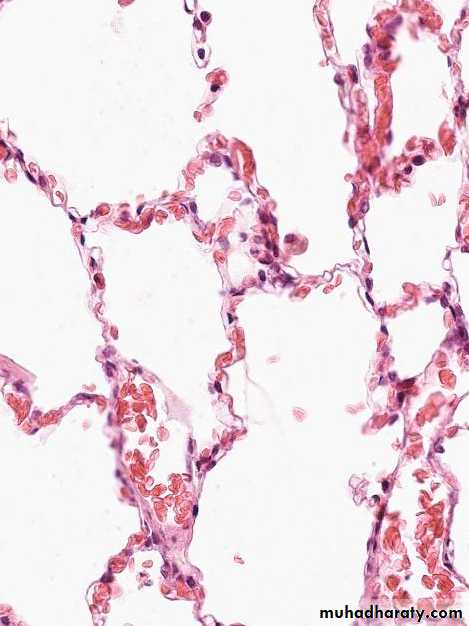
• Pulmonary congestion1. Acute pulmonary congestion:
Alveolar capillaries engorged with blood with transudate inside of the alveoliACUTE CONGESTION, LUNG
Thickened & fibrotic septa
Alveolar spaces contain hemosiderin-laden macrophages resulting in an appearance termed brown indurations.2. Chronic pulmonary congestion:
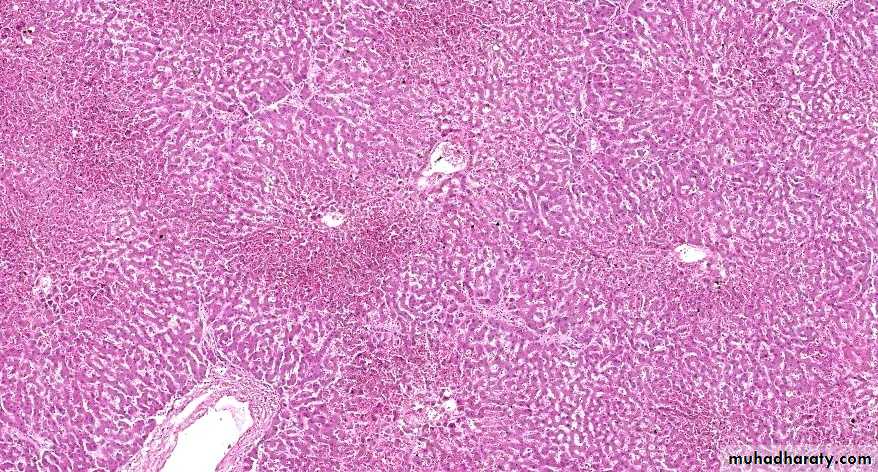
1) Acute hepatic congestion:
Central vein & sinusoids are distendedThere may be even central hepatocyte degeneration.
Peripheral hepatocytes better oxygenated & develop only fatty changes.
• Hepatic congestion
Acute Passive Congestion, Liver
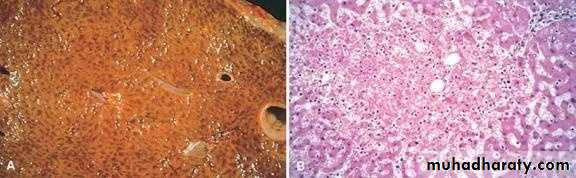
- Central lobules grossly depressed because of loss of cells & appear red brown the surrounding zones uncongested tan, sometimes fatty liver, (nutmeg liver).- Hemosiderin laden macrophages
- This can progress to cirrohisis, and therefore if the congestion is cardiac in origin, the type of cirrhosis is called cardiac cirrhosis.
2) Chronic passive congestion of liver:
CHRONIC PASSIVE CONGESTION, LIVERHemorrhage
Hemorrhage is extravasation of blood from vessels into the extravascular space.Causes:
1. Chronic congestion (capillary bleeding).
2. Hemorrhagic diatheses.
3. Vascular injury (trauma, atherosclerosis, inflammation, neoplastic erosion of vessel wall ).
Patterns of hemorrhage include:
1. External bleeding.2. Internal bleeding (enclosed within a tissue) ”hematoma”.
**Petechiae: are small (1-2 mm) hemorrhagic spots.
**Purpuras: slightly larger than petechiae (3-5 mm).**Ecchymoses(bruises): are larger (1-2cm) subcutaneous hematomas
3. hemothorax, hemoperitoneum, hemopericardium, hemarthrosis refer to large accumulations of blood in pleural cavity, peritoneal cavity, pericardial cavity, and joint space respectively.
• Volume of blood loss.
• rate of bleeding.
3. Site of hemorrhage.
4. Duration (acute versus chronic or recurrent).
Hemostasis and thrombosis
Normal hemostasis: a sequence of events that maintain blood in a fluid, clot-free state in normal vessels while inducing the rapid formation of a localized fibrin-platelet hemostatic plug at a site of vascular injury.The process involves:
• vascular endothelium• Platelets
• coagulation system.
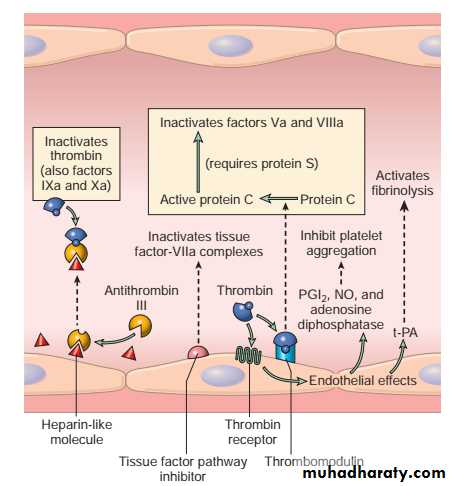
Vascular endothelium
An intact endothelium has the following functions:i) maintaining normal blood flow.
ii) Anti-thrombotic effect :
Antiplatelet effects:
**The endothelium secret PGI2 & nitric oxide (vasodilators & inhibitor of platelet aggregation).
**also elaborate ADPase which degrade ADP & inhibits platelet aggregation.
Anticoagulant effects: These effects are mediated by Membrane-associated heparin-like molecules and by thrombomodulin → activation of anticoagulant protein (protein C).
Fibrinolytic effects: endothelium synthesize tissue plasminogen activator (t-PA), promoting fibrinolytic activity to clear any fibrin deposits.
iii) Prothrombotic effect by the release of :
Thromboplastin or tissue factor (factor III) which activates clotting pathway.Von Willebrand factor that causes adherence of platelets to the subendothelium.
Platelet activating factor which is activator and aggregator of platelets.
Inhibitor of plasminogen activator that suppresses Fibrinolysis.
Anticoagulant activities of normal endothelium.
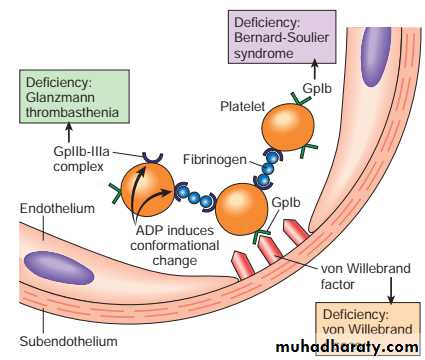
Platelets
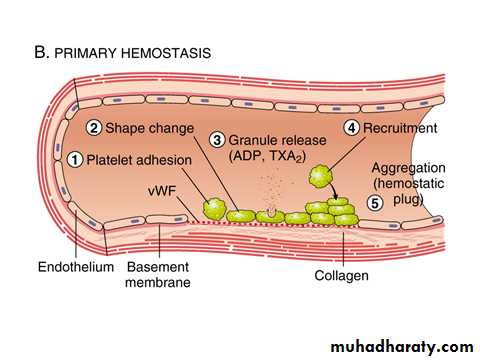
Platelets play a critical role in hemostasis by forming the primary plug that initially seals vascular defects and by providing a surface that binds and concentrates activated coagulation factorsAfter a traumatic vascular injury, platelets encounter constituents of the subendothelial connective tissue, such as vWF and collagen.
On contact with these proteins, platelets undergo a sequence of reactions that culminate in the formation of a platelet plug:
Adhesion
Activation and shape change with markedly increased surface area.
Secretion platelets secrete granule products (calcium, ADP, TXA2).
Aggregation: ADP & TXA2 are a potent mediators of platelets aggregation.
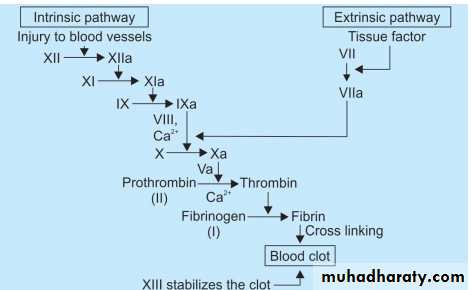
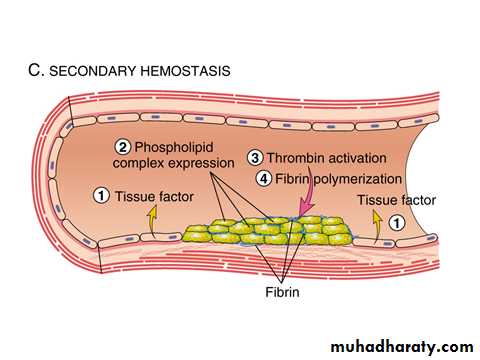
Coagulation cascade
Coagulation cascade: is essentially a series of enzymatic conversions, turning inactive pro-enzymes into active enzymes and culminating in thrombin formation.Thrombin converts soluble fibrinogen into insoluble fibrin.
Beside inducing coagulation, activation of the clotting cascade also sets into motion a fibrinolytic cascade that limits the size of the final clot.
The clotting system can be activated by intrinsic or the extrinsic pathway.
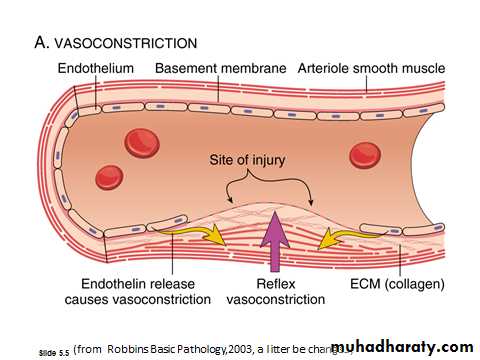
The sequence of events leading to hemostasis at a site of vascular injury:
A. Arteriolar vasoconstriction:Occurs immediately and markedly reduces blood flow to the injured area.
Mediated by
• reflex neurogenic mechanisms.
• local secretion of factors such as endothelin, a potent endothelium derived vasoconstrictor.
This effect is transient.
B. Primary hemostasis: (formation of the platelet plug)
Disruption of the endothelium exposes subendothelial von Willebrand factor (vWF) and collagen, which promote platelet adherence and activation.Activation of platelets results in a dramatic shape change as well as the release of secretory granules.
Within minutes platelets recruitment and aggregation to form a primary hemostatic plug
C. Secondary hemostasis: (deposition of fibrin).
Tissue factor is also exposed at the site of injury.
It is a procoagulant glycoprotein that is normally expressed by subendothelial cells in the vessel wall.
Tissue factor activate the extrinsic pathway of clotting system that leads to thrombin generation.
Thrombin cleaves circulating fibrinogen into insoluble fibrin, creating a fibrin meshwork, and also is a potent activator of platelets, leading to additional platelet aggregation at the site of injury.
This sequence, referred to as secondary hemostatic plug
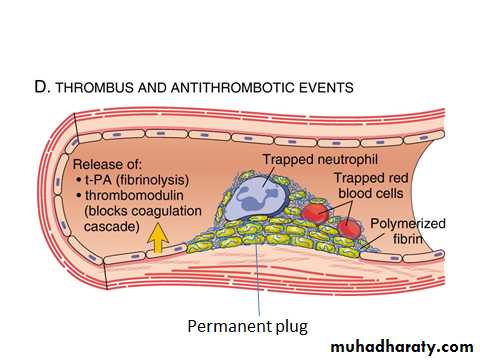
D. Clot stabilization, resorption and antithrombotic events .
Fibrin and platelet aggregates undergo contraction to form a solid, permanent plug that prevents further hemorrhage.
At this stage, counter regulatory mechanisms (e.g., tissue plasminogen activator, t-PA) activate the fibrinolytic system and limit clotting to the site of injury and eventually lead to clot resorption and tissue repair.
D. clot stabilization, resorption and antithrombotic events
Thrombosis:
Pathologic form of hemostasis.Defined as the pathologic formation of intravascular fibrin-platelet thrombus.
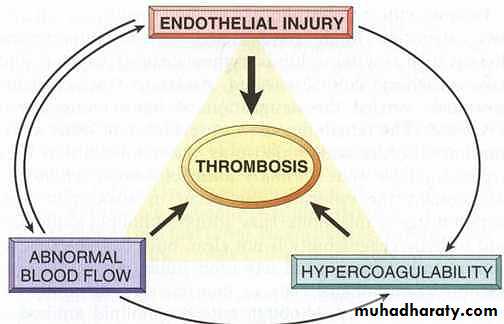
Three primary influences predispose to thrombus formation (Virchow triad);Components of Virchow’s triad
• Endothelial injury: It can be due to the factors likevasculitis, hypertension, turbulent flow, bacterial endotoxins,hypercholesterolemia, radiation etc.
Endothelial injury heart or in the arterial thrombisis.
• Alterations in the normal blood flow: Both turbulence and stasis contribute to the development of thrombosis.
Turbulence arterial thrombosis
Stasis venous thrombosis.
• Disruption of laminar flow and bring platelets into contact with endothelium
• Preventing dilution of activated clotting factors by fresh-flowing blood.
• Retarding the inflow of clotting factor inhibitors.
• Promote endothelial cell activation.
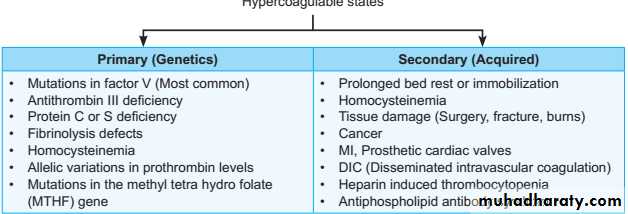
3. Blood hypercoagulability: It can be either primary or secondary hypercoagulable state.
Morphology:
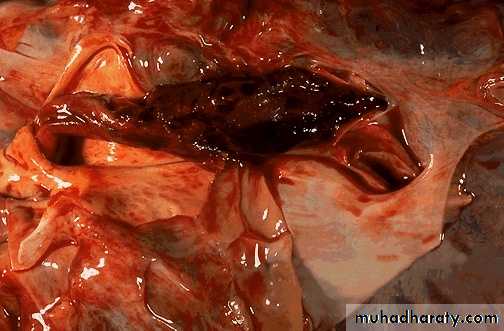
Thrombi may develop anywhere in the cardiovascular system.Grossly and microscopically have apparent laminations (lines of Zahn) produced by alternating pale layers of platelets admixed with some fibrin and darker layers containing more red blood cells.
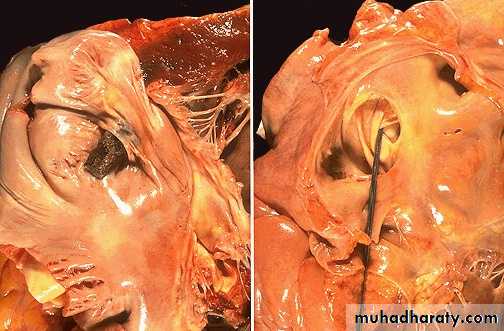
Right atrial mural thrombus with lines of Zahn
Mural thrombus with lines of Zahn
Microscopic appearance of thrombus' the line of Zahn’.
• Types of thrombus:
• Arterial thrombi (pale thrombus):• gray white in color
• firmly attached to the wall
• begin at site of injury or turbulence
• usually occlusive, Occur in coronary, cerebral or femoral arteries.
• Venous thrombi (red thrombus):
• red in color
• less firmly attached to the wall
• begin at site of stasis
• invariably occlusive, occur in lower extremities (90%).
• Mural thrombi : are thrombi arise in heart chambers or aortic lumen.
• Vegetations: are thrombi formed on heart valves as in infective endocarditis
Post mortem clot: it is gelatinous with dark red dependent portion and yellow ”chicken fat” supernatant , lack lines of Zahn and not attached to blood vessel ,in contrast thrombi almost always have point of attachment.Fate of the thrombus:
1. Resolution (removal by fibrinolytic action).2. Organization and re-canalization.
3. Propagation to obstruct a critical vessel or branch.
4. Embolization in part or in whole.
Thrombi are significant because:
• They cause obstruction of vessels.• Artery → infarction, vein → congestion
2. They are possible sources of emboli.
Disseminated Intravascular Coagulation:
• DIC is not a specific disease but rather a complication of a large number of conditions associated with systemic activation of thrombin (e.g. obstetric complications, infections, advanced malignancy, massive tissue injury).• It is characterized by widespread formation of thrombi in the microcirculation.
• The multiple thrombi will lead to rapid consumption of platelets and coagulation proteins (consumption coagulopathy) that results in activation of fibrinolytic mechanisms.
Embolism
Definition:
An embolus is a detached intravascular solid, liquid or gaseous mass that is carried by blood to sites distant from its point of origin.
After traveling via the blood, the embolus can obstruct a vessel
The potential effect of embolism is ischemic necrosis (infarction).
Types of embolism:1. Thrombo-embolism(99%).
2. Fat.3. Gas (air, nitrogen).
4. Amniotic fluid.
5.Atherosclerotic debris.
6. Tumor fragments.
7. Bone marrow.
8. Foreign body (bullet).
Thromboembolism
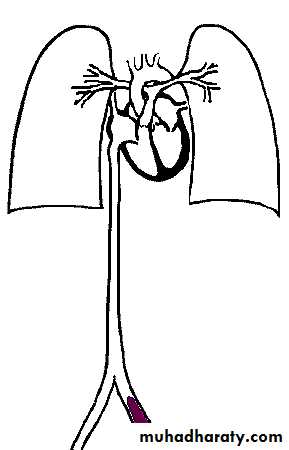
Based on its sites of origin & impaction, thromboembolism can be divided into:1. Pulmonary thrombo-embolism:
The most common and fatal form of venous thromboembolism in which there is occlusion of pulmonary arterial tree by thromboemboliIn
more than 95% of instances, venous emboli originate from DVT, (above the level of the knee).
Depending on the size of the embolus:
1. It may occlude the main pulmonary artery.
2. Impact across the bifurcation (saddle embolus).3. Or pass out into the smaller branching arterioles. Frequently there are multiple emboli.
Rarely, an embolus may pass through an inter-atrial ( patent foramen ovale) or inter-ventricular defect to gain access to the systemic circulation (paradoxical embolism).
• Pulmonary embolism
Saddle embolus of main pulmonary trunkPulmonary embolus obstructing the main pulmonary artery
Paradoxical embolus through a patent foramen ovaleMicroscopic appearance of a pulmonary thromboembolus in a large pulmonary artery. There are interdigitating areas of pale pink and red that form the "lines of Zahn" characteristic for a thrombus .
Major consequences of pulmonary embolism
1.Sudden death, cardiovascular collapse or acute Rt. ventricular failure (more than 60% of pulmonary circulation is obstructed).2. pulmonary hemorrhage, obstruction of medium-sized arteries
3. Infarction, obstruction of small end-arterioles4. pulmonary hypertension → Rt. ventricular failure, multiple emboli over time.
2. Systemic thrombo-embolism:
They may originate from:
• Intra-cardiac mural thrombi (about 80% of emboli).
• Left ventricular wall infarcts• Left atrial dilation and fibrillation
2. Atherosclerotic plaques
3. Aortic aneurysm.
4. Valvular vegetation.
5. Venous thrombi ( Paradoxical emboli).The main sites involved are;
In contrast to venous emboli which lodge primarily in one vascular bed (lung), arterial emboli can travel to wide variety of sites:1. Lower extremities (75%).
2. Brain (10%).3. Intestines.
4. Kidneys.
5. Spleen.
3. Fat embolism
it may result from;
1. Fractures of long bones (most common).
2. Soft tissue trauma and burns (rare).
4. Gas embolism
Air embolism may enter the circulation during:1. Obstetric procedures.
2. Chest wall injury.More than 100 ml of air are required to produce a clinical effect, bubbles can coalesce to form frothy mass sufficiently large to occlude major vessels.
***Decompression sickness***
Is a particular form of gas embolism occurring in individuals who are exposed to sudden changes in atmospheric pressure (deep sea divers).When air is breathed at high pressure, increased amounts of gas (particularly nitrogen) become dissolved in the blood and tissues. If the diver ascends (depressurizes) too rapidly, the nitrogen expands in the tissues and
Bubbles out of solution in the
blood to form gas emboli.
Clinically, the diver suffers from;
• Muscle and joint pain.2. Infarctions in various tissues.
3. Respiratory distress(chokes).
5. Amniotic fluid embolism:
The underlying cause is the infusion of amniotic fluid or fetal tissue into the maternal circulation via a tear in the placental membranes or rupture of uterine veins during labor.
1. Sudden severe dyspnea.
2. Cyanosis.
3. Hypotensive shock.
4. Seizure and coma.
5. If the patient survives, pulmonary edema and DIC develop.
Infarction :
It is an area of ischemic necrosis caused by occlusion of either the arterial supply or the venous drainage in a particular tissue.Causes:
1. Thrombosis or embolism (99%).2. Local vasospasm.
3. Expansion of atheroma due to hemorrhage in plaque
4. Extrinsic compression of a vessel e.g. tumor, twisting, edema, hernia).
5. Traumatic rupture of blood supply.
Morphology of infarction
Infarcts are classified on the basis of their color and the presence or absence of infection, into;
1) Red (hemorrhagic).
2) White (anemic)And
1) Septic.
2) Sterile.Red infarcts: occur in the following situations;
1. Venous occlusion (ovarian torsion).2. Loose tissue (lung).
3. Tissues with dual circulation(lung, small intestine).
4. Previously congested tissues.
5. Re-established blood flow to site of necrosis.
White infarcts: Occur in
1. arterial occlusions.
2. solid organs with end-arterial circulation (e.g. heart, spleen, kidney).
Pulmonary infarction ( wedge- shaped area & has begun to organize at the margins) caused by a medium-sized thromboembolus to the lung.
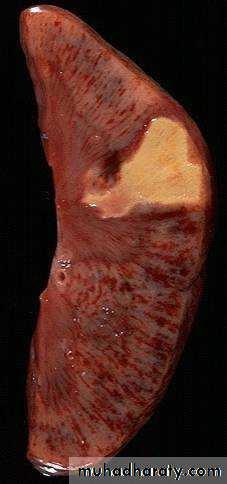
(Infarctions of the spleen (wedge –shaped pale areas caused by obstruction of spleenic artery
Coagulative necrosis (infarction) of kidney
Clinical correlationThe consequences of a vascular occlusion can range from no or minimal effect, to death of a tissue or even the individual.
Factors That Influence Development of an Infarct.
1. Nature of the vascular supply.2. Rate of development of occlusion.
3. Tissue vulnerability to hypoxia.
4. Oxygen content of blood
Shock :
Also called cardio-vascular collapse, is defined as systemic hypo-perfusion caused by reduction either in cardiac output or in the effective circulating blood volume.The end results are:
1. Hypotension.
2. Impaired tissue perfusion.
3. Cellular hypoxia.
Initially, there will be a reversible cellular injury, persistence of the shock eventually causes irreversible tissue injury and can lead to the death of the patient.
Types of shock :
1. Cardiogenic.2. Hypovolemic.
3. Septic.
4. Neurogenic.
5. Anaphylactic.
Cardiogenic shock
Myocardial pump failure: which may be caused by :
1-Intrinsic myocardial damage (MI , ventricular arrhythmias )
2-Extrinsic compression (cardiac tamponade)
3-Out flow obstruction (pulmonary embolism)
Principle mechanism is failure of myocardial pump →sudden fall in C.O.P
Hypovolemic shock
result from:loss of blood or plasma volume as in hemorrhage, fluid loss from sever burns, vomiting &diarrhea or trauma.
Principle mechanism: inadequate blood or plasma volume→ low Cardiac Output
Septic shock
Is caused by microbial infections.Most commonly(70%) this occurs in the setting of G- infections (endotoxic shock) but it can also occur after G+ bacteria septicemia or even fungal sepsis.
The toxins produced by these bacteria causes peripheral vasodilatation & pooling of blood; endothelial activation /injury, leukocyte induced damage and DIC.
Neurogenic shock:
occurs following an anesthetic accident or spinal cord injury. Loss of vascular tone
and peripheral pooling of blood.
Anaphylactic shock:
initiated by type 1 hypersensitivity reaction (Ig E mediated) → systemic vasodilatation & ↑vascular permeabilityShock is the final common pathway for a number of potentially lethal clinical events.
Stages of shockShock is a progressive disorder that, if uncorrected, leads to death. shock tends to evolve through 3 stages.
1-Initial non-progressive stage:
During which reflex compensatory mechanisms are activated &perfusion of vital organs is maintained which include: neurohumoral mechanisms help to maintain the cardiac output & blood pressure.These compensatory mechanisms include:
baroreceptors reflexesrelease of catecholamines
activation of renin –angiotensin axis
release of antidiuretic hormone (ADH)
generalized sympathetic stimulation
The net effect is tachycardia, peripheral vasoconstriction and renal conservation of fluid .
Cutaneous vasoconstriction is responsible for pallor of skin in shock .
Coronary & cerebral vessels are less sensitive to the sympathetic response & thus maintain relatively normal caliber, blood flow →oxygen delivery to the vital organs .
Septic shock initially cause cutaneous vasodilatation and thus the patient presents with warm & flushed skin.
2-progressive phase:
characterized by tissue hypoperfusion and onset of worsening circulatory and metabolic imbalances, including lactic acidosis.if tissue hypoxia is persistent →intracellular aerobic respiration is replaced by anaerobic glycolysis, with excessive production of lactic acid →metabolic lactic acidosis →↓tissue pH and blunts the vasomotor response →arteriolar dilatation and pooling of blood in the microcirculation →worsen the C.O.P ,anoxic injury to the endothelial with subsequent DIC.
.
With this wide tissue hypoxia, vital organs are affected and begin to fail ; clinically the patient may become confused & urinary output declines
3-irreversible stage:
cellular and tissue injury so severe that even if the hemodynamic defects are corrected, survival is not possible.The patient has complete renal shutdown due to acute tubular necrosis.
Morphology:
The cellular and tissue changes are those of hypoxic injury. Most particularly involved organs are;brain, heart, lungs, kidneys, adrenals and gastro-intestinal tract.
Clinical features: they depend on the precipitating insult.
In hypovolemic and cardiogenic shock, the patient presents with hypotension; a weak, rapid pulse, tachypnea; and cool, clammy, cyanotic skin.
In septic shock, the skin initially is warm and flushed due to peripheral vasodilation.
Prognosis :
Varies with the origin of shock and its duration.The best is in a young patient with hypovolemic shock, and the worst is in an old patient with cardiogenic shock and that with septic shock.