General Pathology of Infectious Diseases
Dr.Zahraa Osama YehyaDepartment of Pathology
Ninevah College of Medicine
Mechanism of Bacterial injury(Pathogenesis)
1- Release toxins that kill cells. (exotoxin & endotoxin).2- Release lytic enzymes, includes proteases, hyaluronidase, coagulase & fibrinolysins that destroy the tissue & facilitate the spread of bacteria .
3- Elicit an inflammatory reaction that may destroy not only the bacteria but also the infected tissue.
4-Elicit an immune reaction that may damage the tissues carrying the same antigen as the bacterium (“cross reactivity”).
Bacterial infection is divided into:1- Acute.2- Chronic.
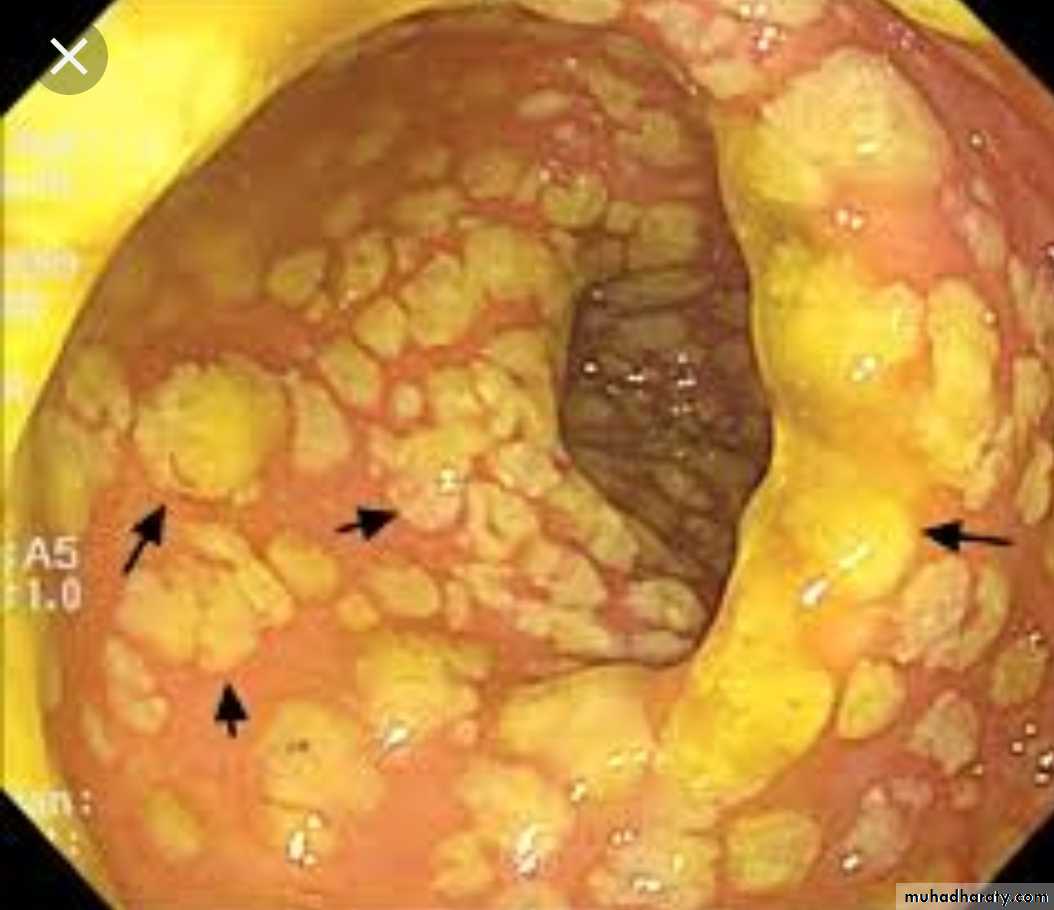
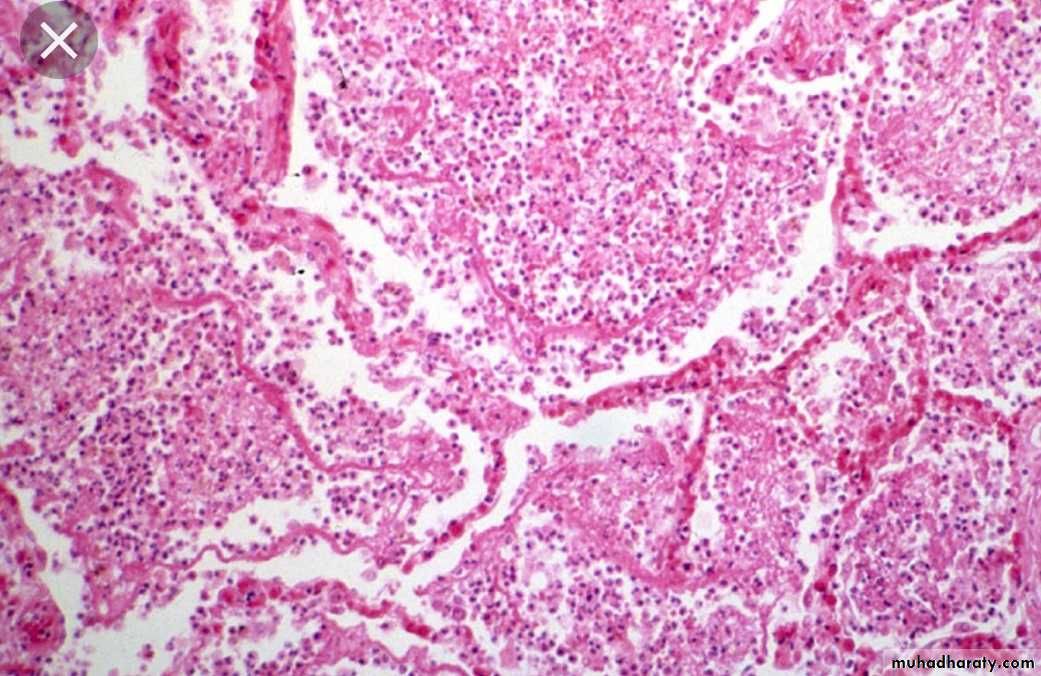
Acute Bacterial InfectionMorphological paterrns1-Catarrhal: affect mucus membrane.
Acute cattarhal gastritis
2- Serous: affect serous cavities and produce serous fluid.
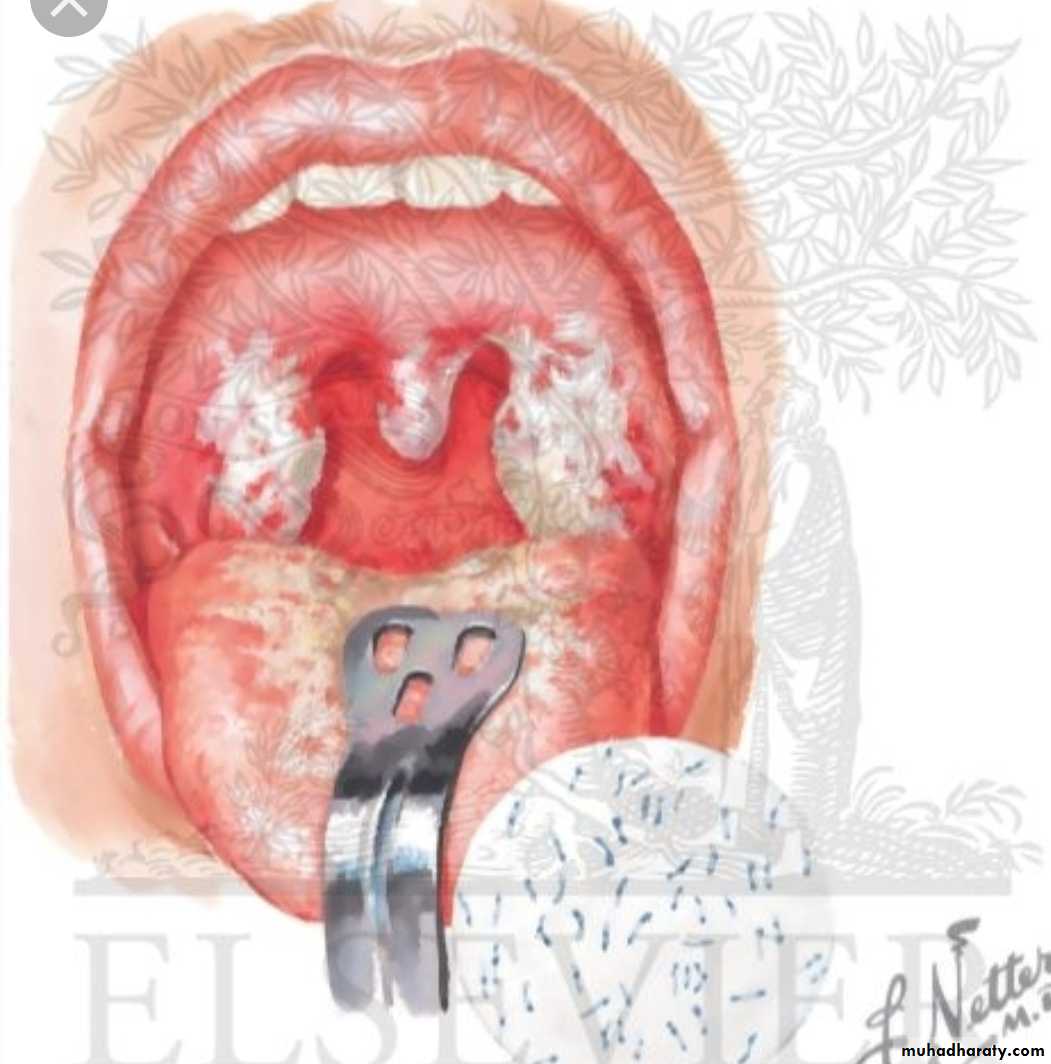
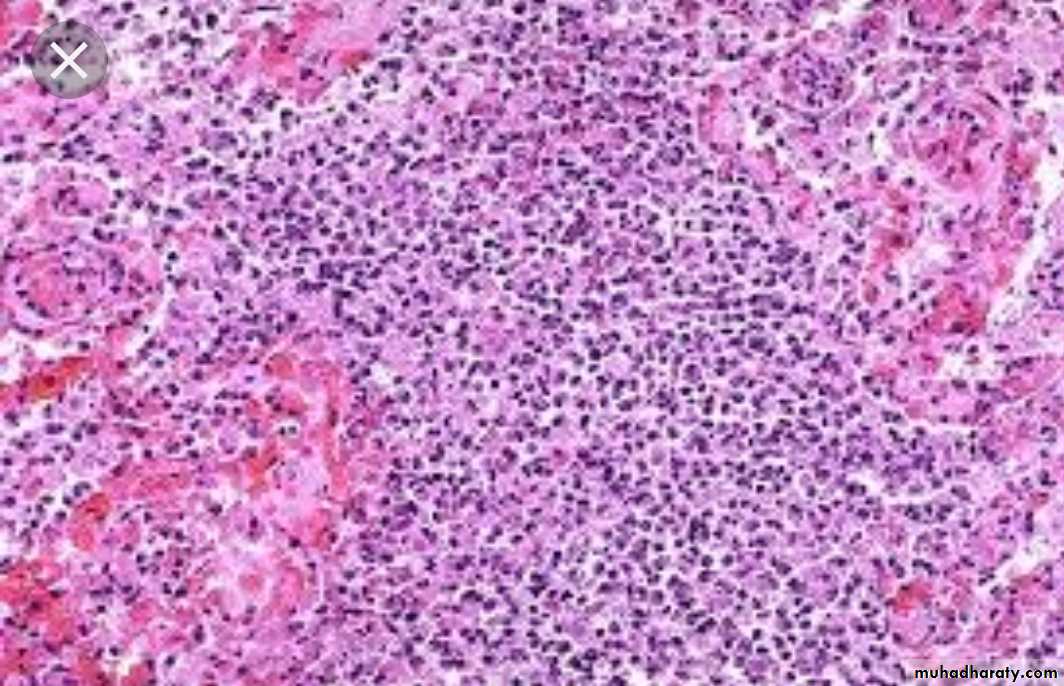
3- Pseudomembranous : characterized by formation of peudomembrane as in diphtheria.4- Pyogenic or suppurative: pus producing . e.g. Abscess
Pus is a creamy fluid consist of neutrophil, pus cell (dead neutrophil) necrotic tissue, bact. & fluid.
Localized collection of pus in tissue is called abscess
M.O stimulate T-lymphocytes to secret IL-1 & TNF which stimulate complement ,This attract neutrophil which secret lytic enzyme , destroy tissue & form abscessBacterial infection of the blood
Classified into:Bacteraemia
Septicaemia
Pyaemia
Toxicaemia
Bacteraemia
Presence of small numbers of bacteria in the blood WITHOUT multiplication.
Patients have subclinical or minor symptoms & lesion.
E.g., Strept. viridans in blood after vigorous brushing of teeth with dental sepsis.These bacteria are destroyed rapidly in blood because of antibodies, complement, & circulating macrophages.
It is important because it may settle in various parts of the body & cause localized lesion e.g., endocarditis by Strep. viridans.
Septicaemia
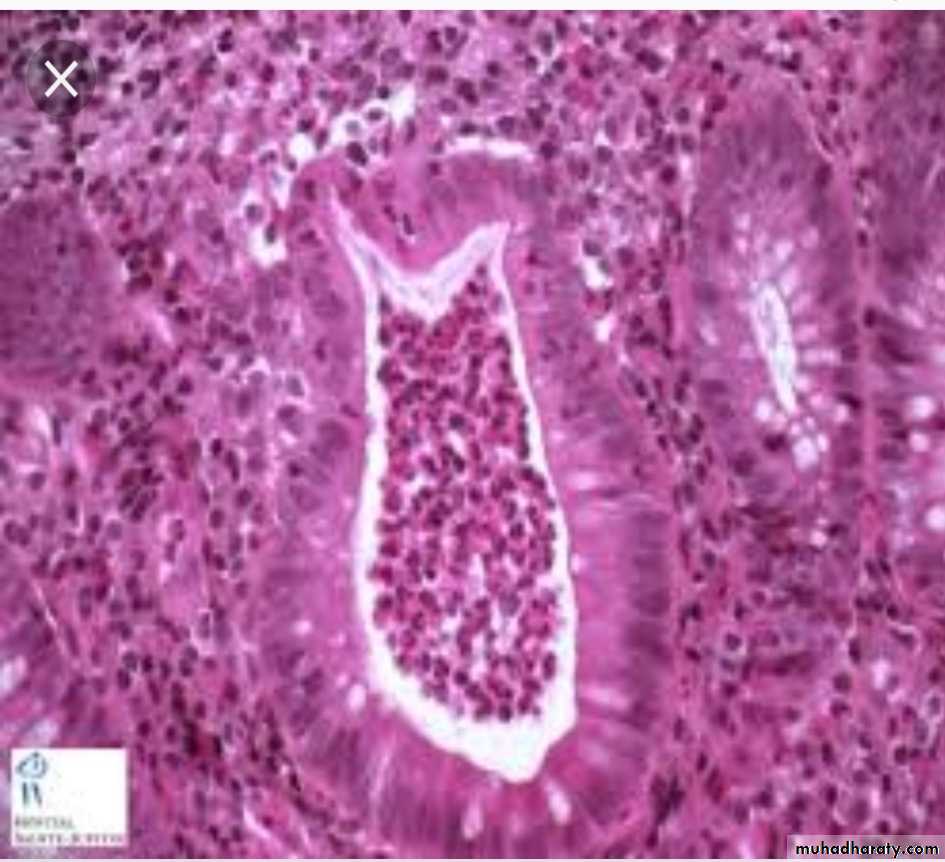
Multiplication of highly pathogenic bacteria in the blood e.g., pyogenic cocci, endotoxin producing gram –ve bacilli. It results in serious consequences which may end in death.Multiple small hemorrhages due to capillary endothelial damage, multiple minute metastatic foci of bacterial growth.
Patients usually presented with Tachycardia. Hypotension. Splenomegaly & shock
PyaemiaAs bacteria invade & multiply in a thrombus causing necrosis and pus formation. Small fragments of the soften septic thrombus may then break away & be carried off in the blood resulting in the developing of pyaemic abscesses in various organs:
Toxaemia
Presence of toxin in blood e.g. Diphtheria
Gangrene
Digestion of dead tissue by saprophytic bacteria in living body
(necrosis with putrefaction)Types of gangrene
PrimarySecondary
The difference lies in the cause of the tissue necrosis of each type
Primary gangreneGas gangreneIt is brought about by infection with pathogenic bacteria which both kill the tissue by secreting potent exotoxins & then invade & digest the dead tissue.
the causative m.o. are
Cl. (perfringens ) welchiiCl. oedematiens
Cl. Septicum
(all are anaerobic )
These organisms are intestinal commensals in man and animals and because they are anaerobic they can’t multiply in oxygenated environment , so they need dead tissue in dirty wound or lacerated wounds in order to multiply and cause gas gangrene.
Pathogenesis
Cl. produce different strong types of exotoxins.Cl. welchii ferments sugar producing H2 & CO2 which collect as bubbles in the dead tissue and can easily be detected by palpation (crepitant ).
These lead to specific changes in the tissue affected by gangrene., black discoloration and bad odor at the affected site like the skin and subcutaneous tissue, intestine, appendix & uterus (puerperal period )
Secondary Gangrene
Types:Wet gangrene
Dry gangrene
1) Wet gangrene
The infected tissues are edematous due to presence of large amount of fluid and large amount of subcutaneous fat.This type occurs rapidly.
The line of demarcation between dead and living tissue is indistinct.
The gangrene may extend proximally beyond the site of infection.
Diabetic foot is the most common example.
2) Dry gangrene
This type occurs in leg due to gradual cut of blood supply either due to atherosclerosis or vasculitis in the lower limbs.The line of demarcation between dead and living tissue is clear .
The lesion remains localized .
Ischemic necrosis of the lower limb is the most common example.
QUIZ
Chronic Bacterial infectionTuberculosis
The single most important infectious cause of death on earth after HIV.Caused by Mycobacterium tuberculosis & Mycobacterium bovis.
Gm +ve bacilli .
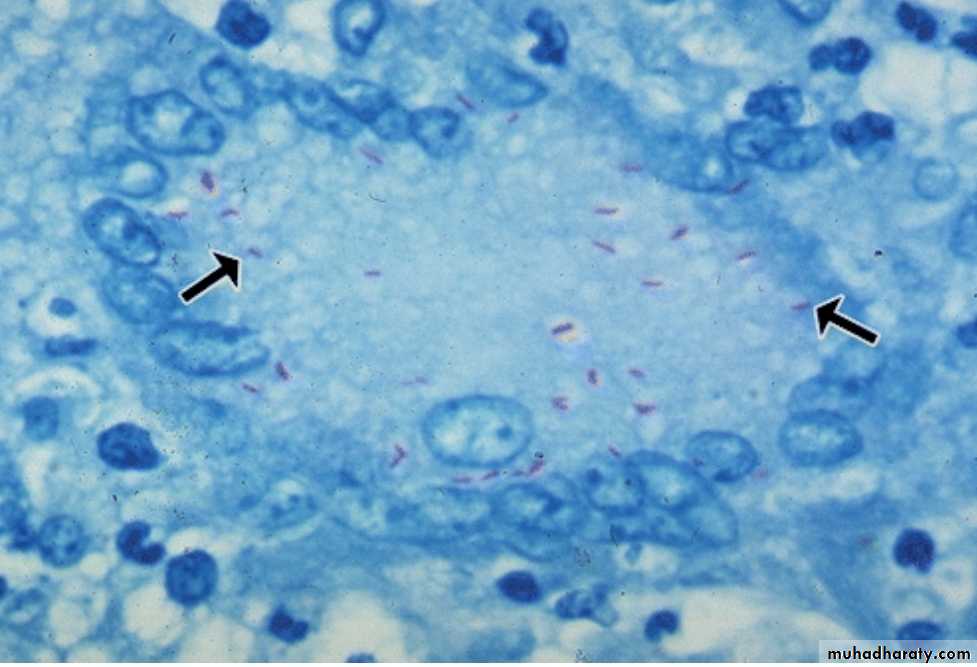
T.B bacilli have a waxy cell wall (mycolic acid) which make them acid and alcohol fast (AFB).Because mycobacterium grows 20-100 times slower than other bacteria, it takes 4-6 weeks to obtain a colony of mycobacterium tuberculosis.
Predisposing factors for T.B :
PovertyMalnutrition
Chronic diseases
Immunosuppression
Over crowding
Transmission of TB
Four possible entry sites exist : -• Respiratory tract by inhalation, from open TB lesion.
• Alimentary tract by ingestion of infected milk , food.
• Skin by inoculation.
• Congenital infection (very rare).
Pathogenesis of Tuberculosis
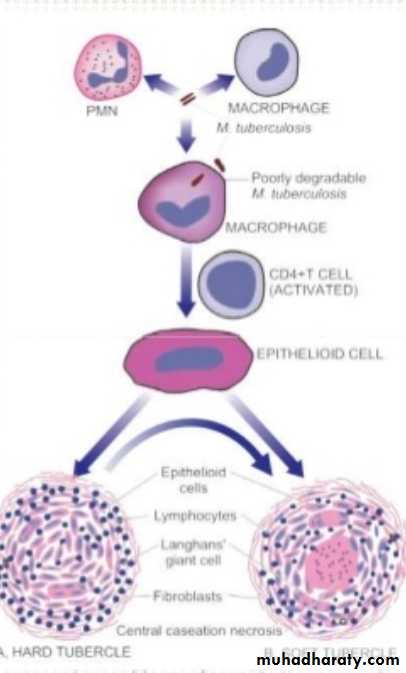
T.B. bacilli produce NO exotoxin or endotoxin. the m.o. escapes killing by being inside the macrophage, proliferate inside the macrophage & prevent fusion of phagosome & lyzosome (phagolysosome).The main lesion is due to cell mediated immunity, the m.o. stimulate the macrophage to secrete TNF-α which causes fever & tissue damage.
Cell mediated immunity confers resistance to mycobacteria and at the same time result in development of hypersensitivity to mycobacterial antigen which is responsible for granuloma formation and caseation.
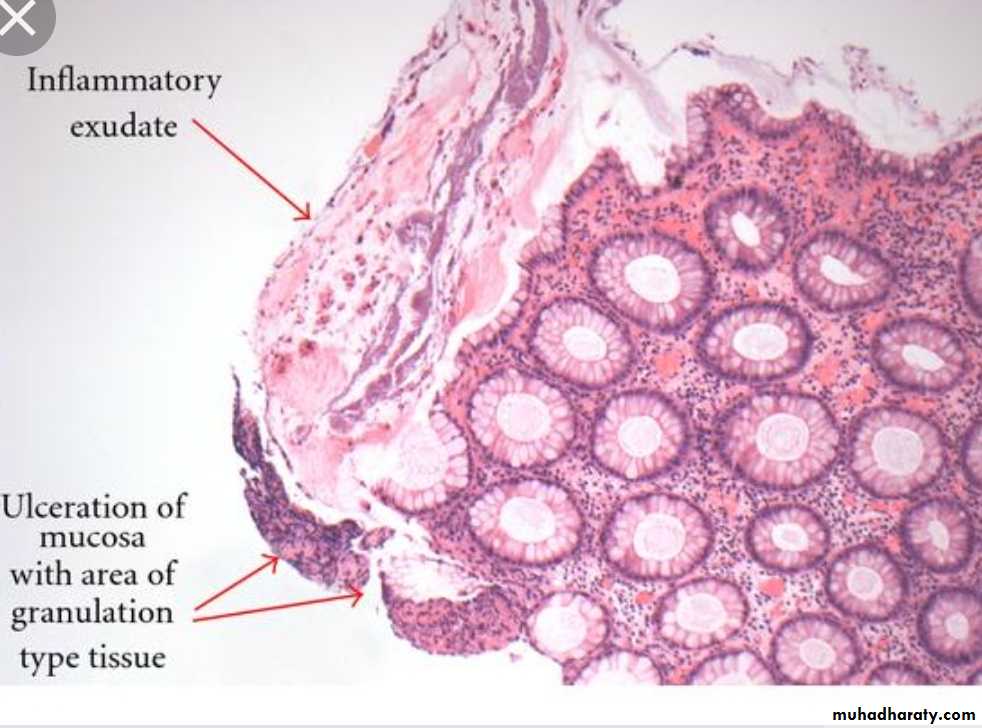
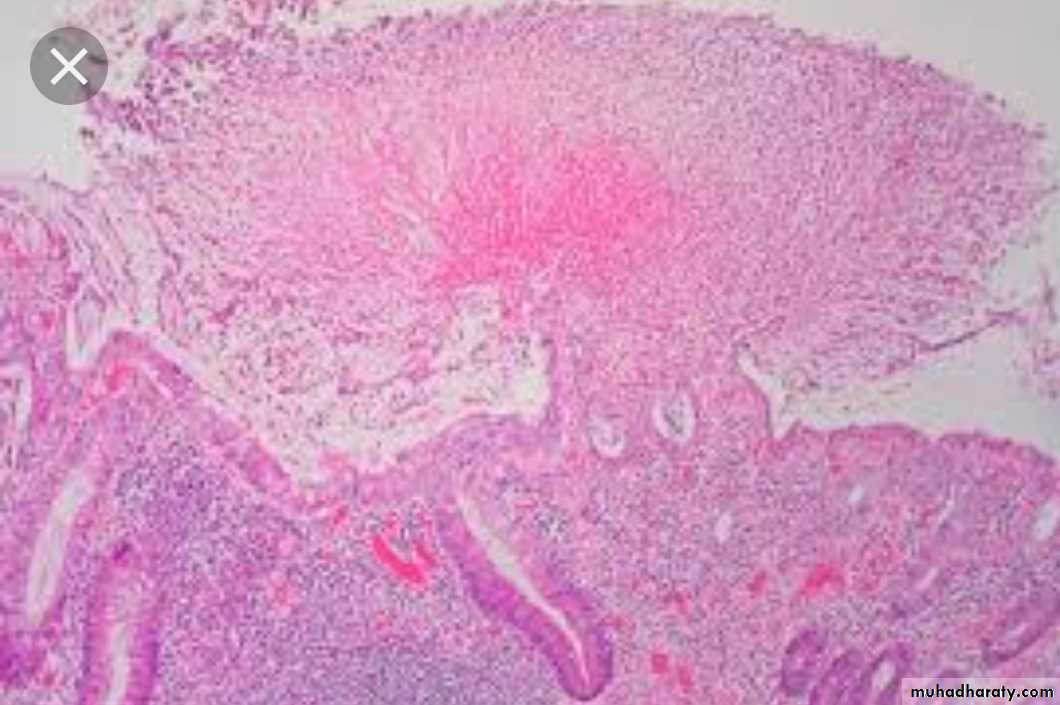
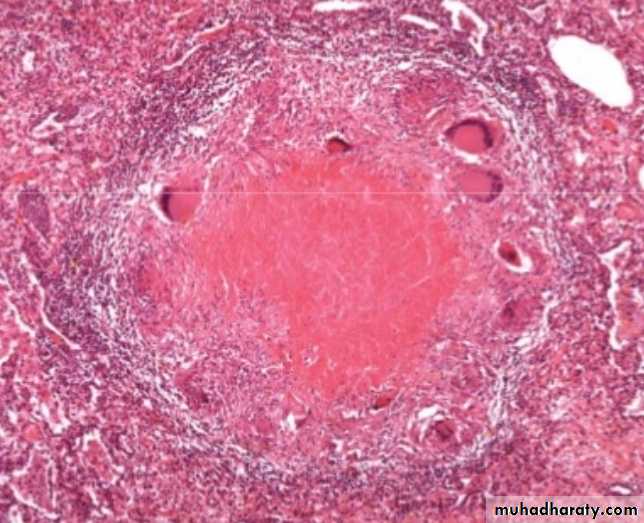
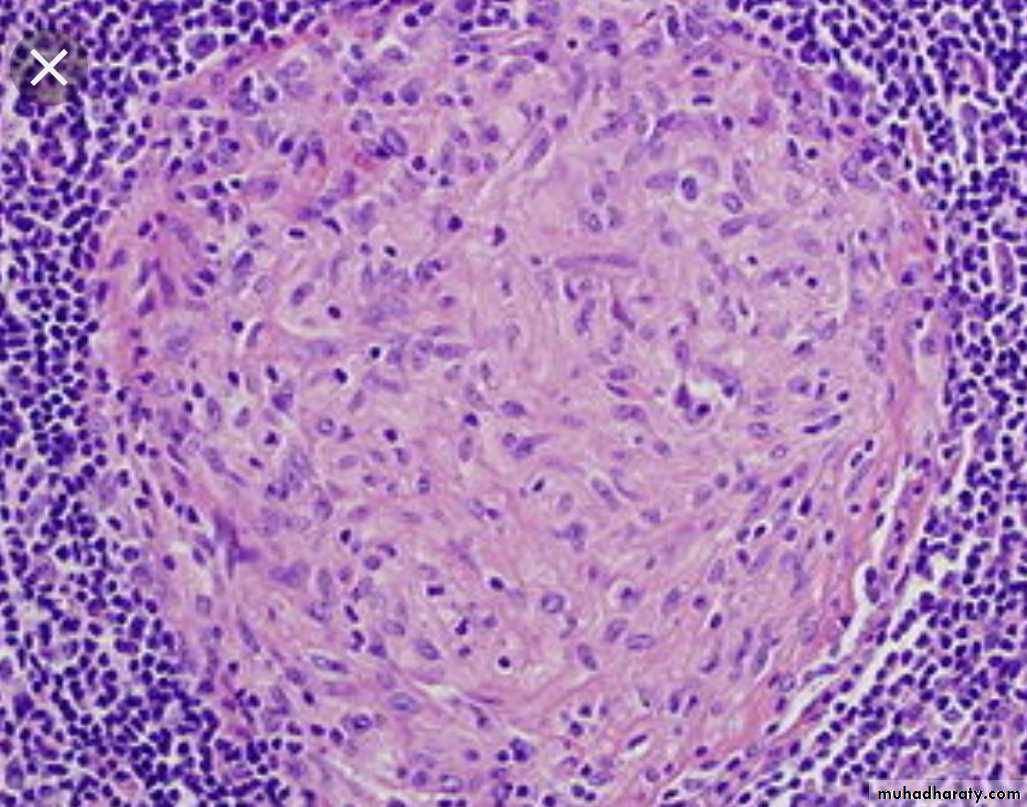
On the initial exposure to the m.o. there is non-specific inflammatory response that resembles inflammation to any form of bacteria, 2-3 weeks later the reaction becomes granulomatous and the center becomes caseous forming typical tubercle
Granuloma
In 3 weeks time, specifically primed T-lymphocytes (T-helper cell) are produced in response to tuberculoprotein.T-helper cells produce INF-y
INF-y is the critical mediator that enable the macrophage to control mycobacterial infection.INF-y also orchestrates formation of the granuloma & caseous necrosis.
INF-y activate macrophages to form epitheloid cells, some unite to form giant cells resulting in the characteristic picture of T.B. lesion.Activated macrophages secret TNF which attract more monocytes.
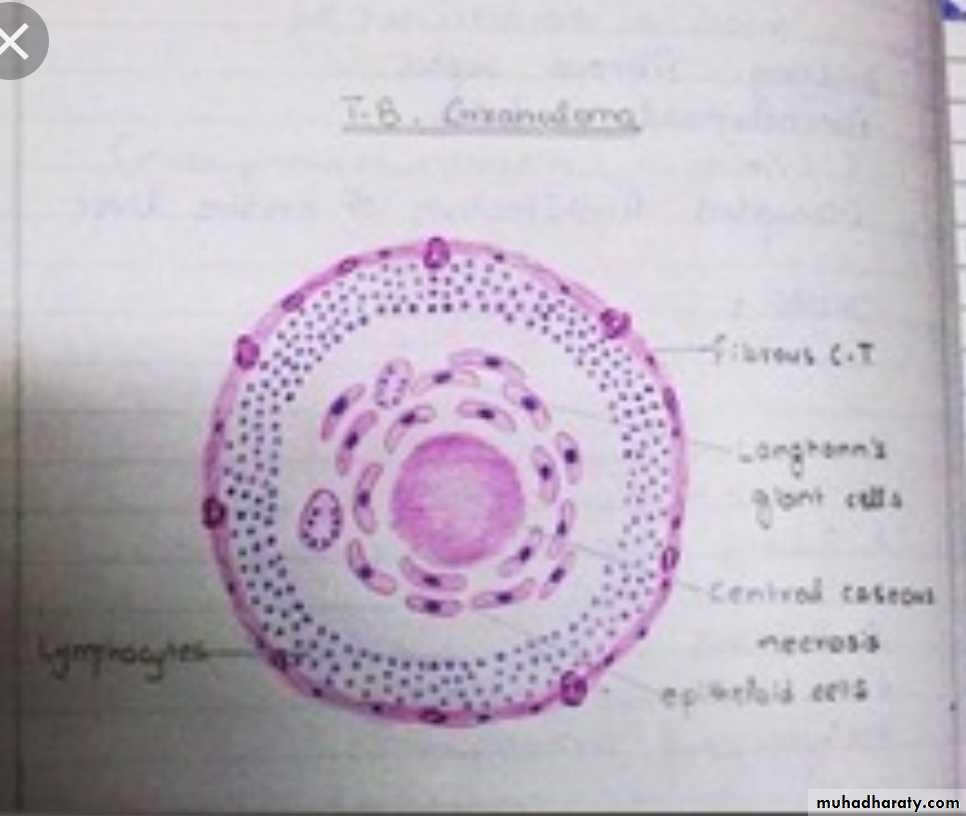
The infection may be terminated at this stage or it may progress to caseous necrosis formation.So the final lesion of TB consist of central area of amorphous, a cellular caseous necrosis, surrounded by macrophages, referred to as epithelioid cells, some macrophages fuse to from multinucleated giant cells, the nuclei of which may be distributed peripherally (Langhans giant cells) these are surrounded by rim of chronic inflammatory cells rich in lymphocytes & at the periphery there is fibrosis.