General Pathology of Infectious Diseases
Dr.Zahraa Osama YehyaDepartment of Pathology
Ninevah College of Medicine
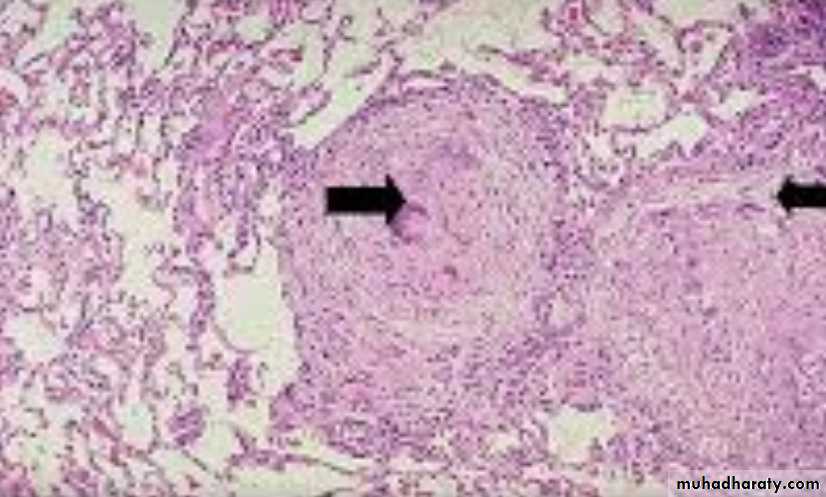
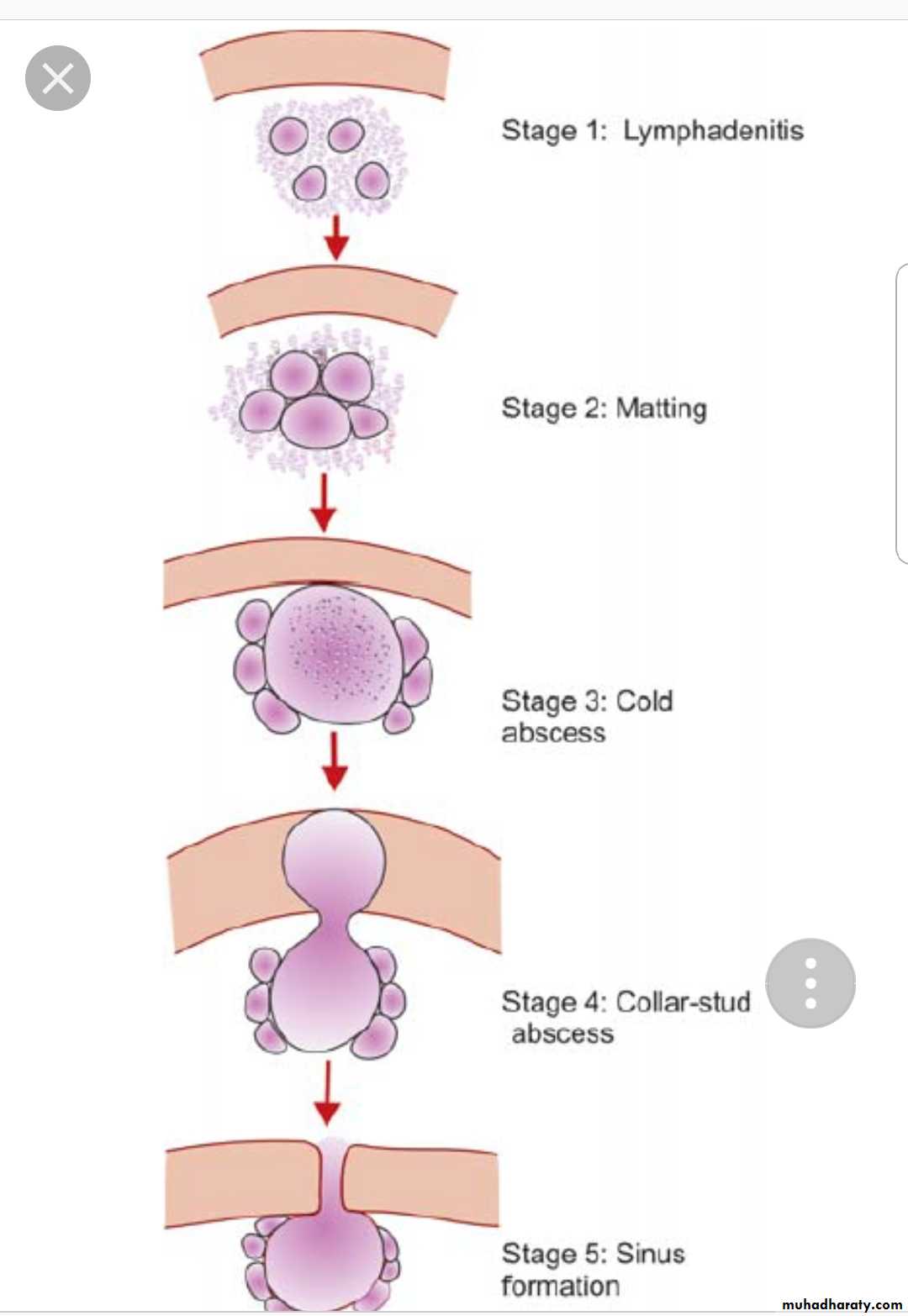
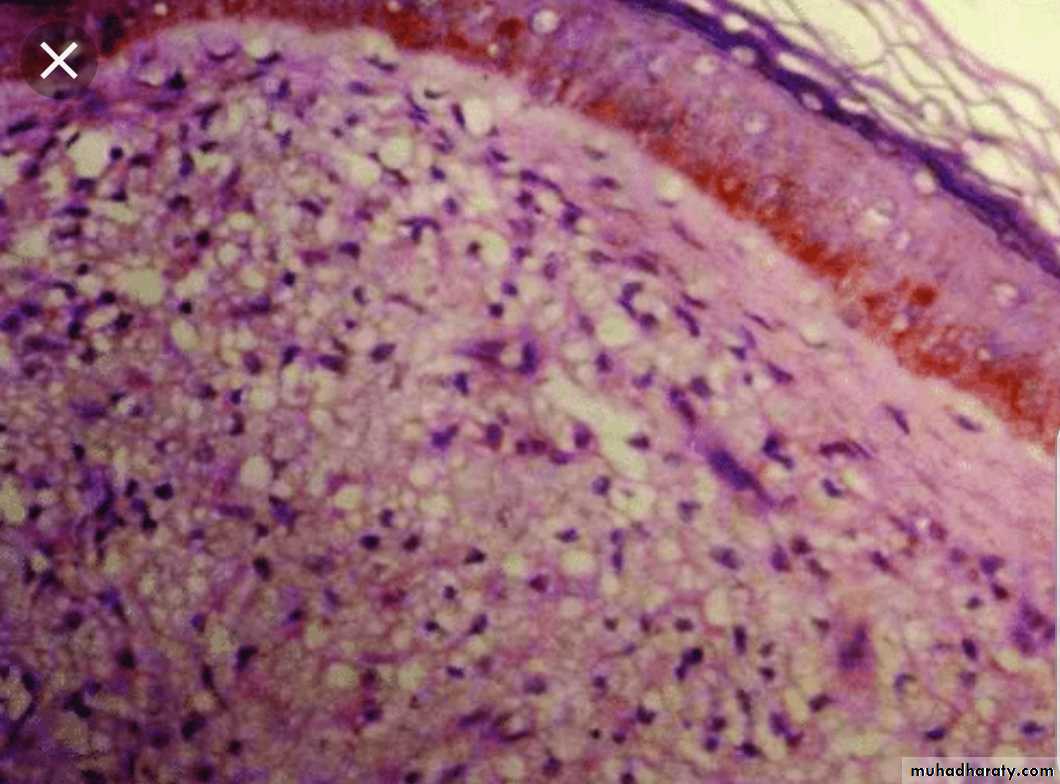
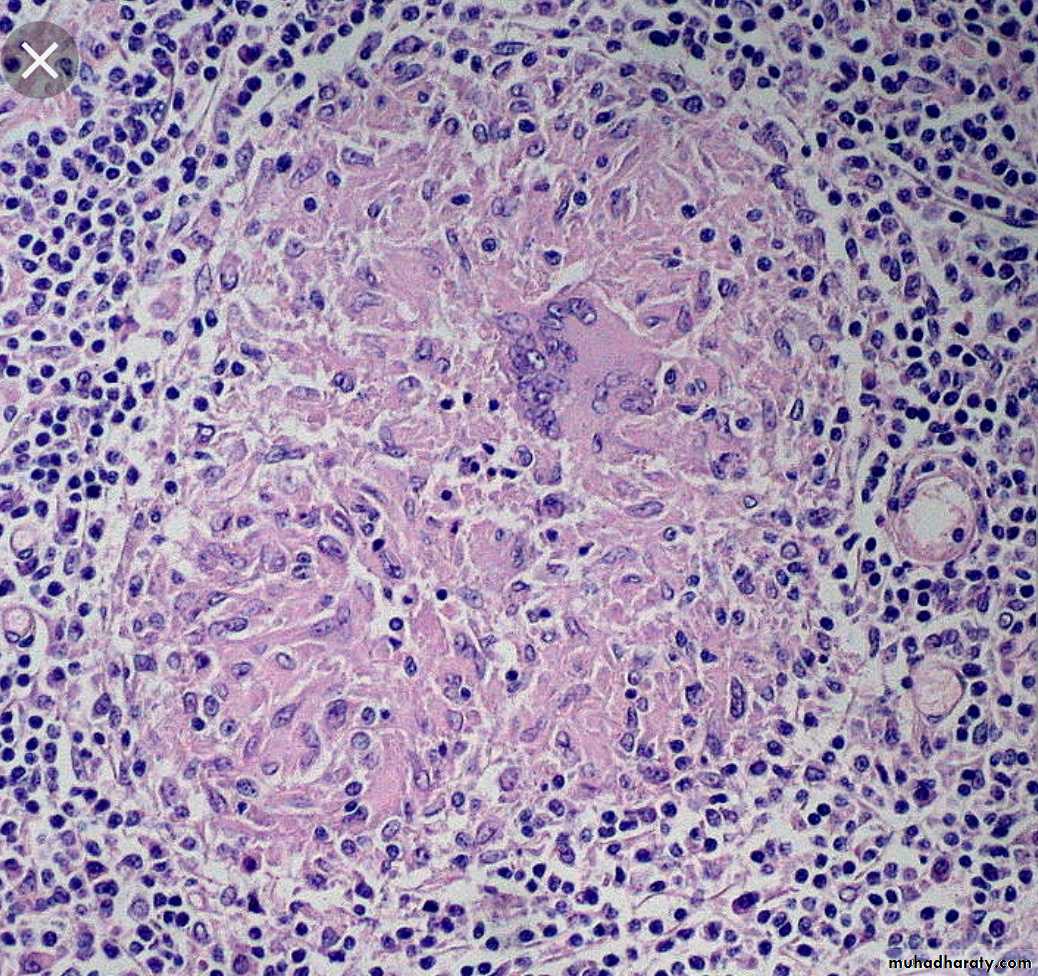
Tubercular lymphadenitis
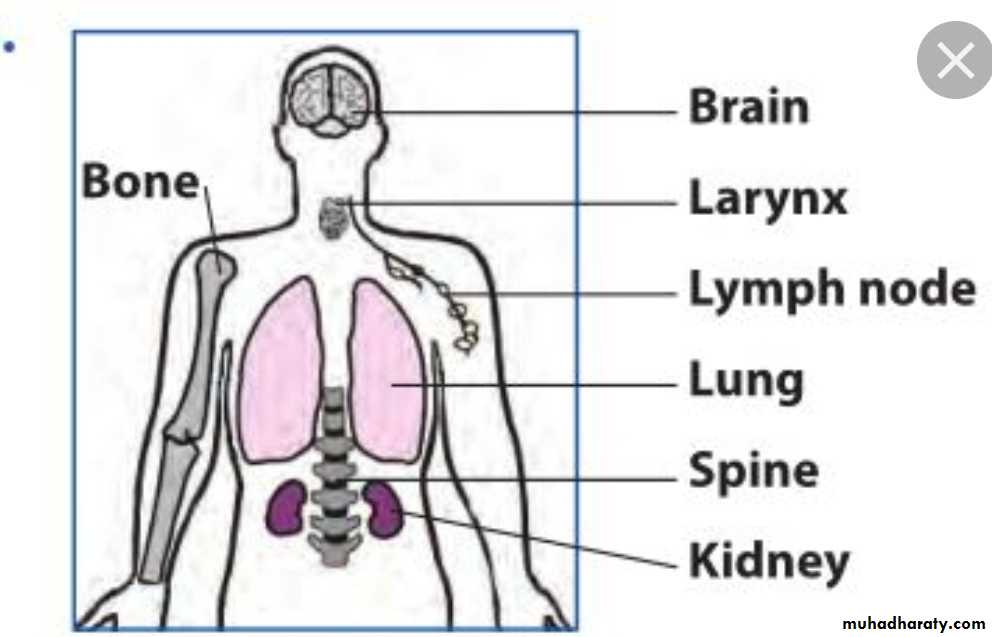
TB usually affects the lungs but may involve any organ or tissue in the body
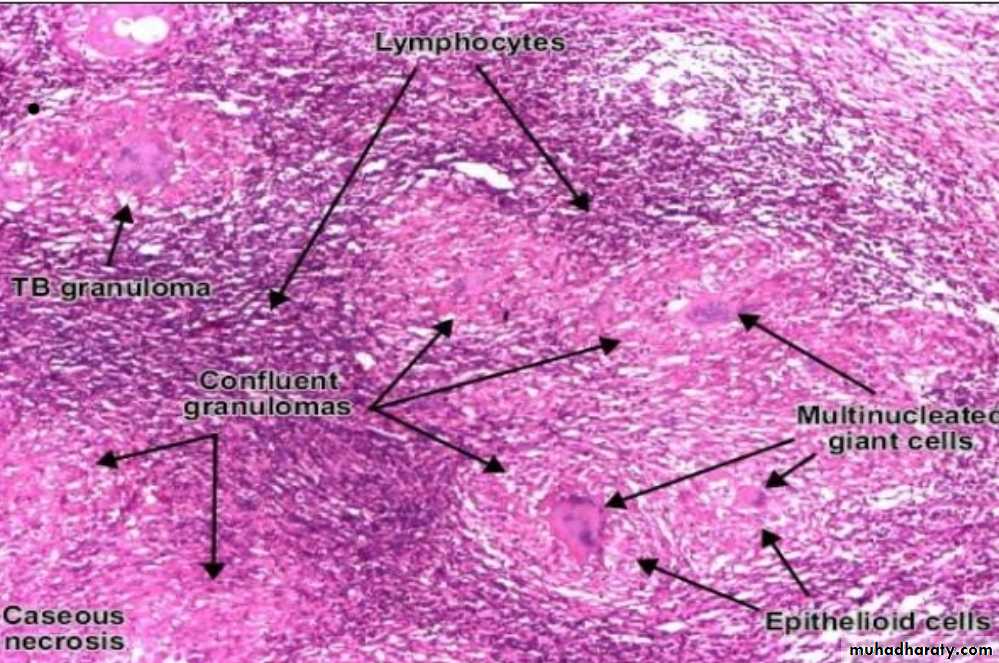
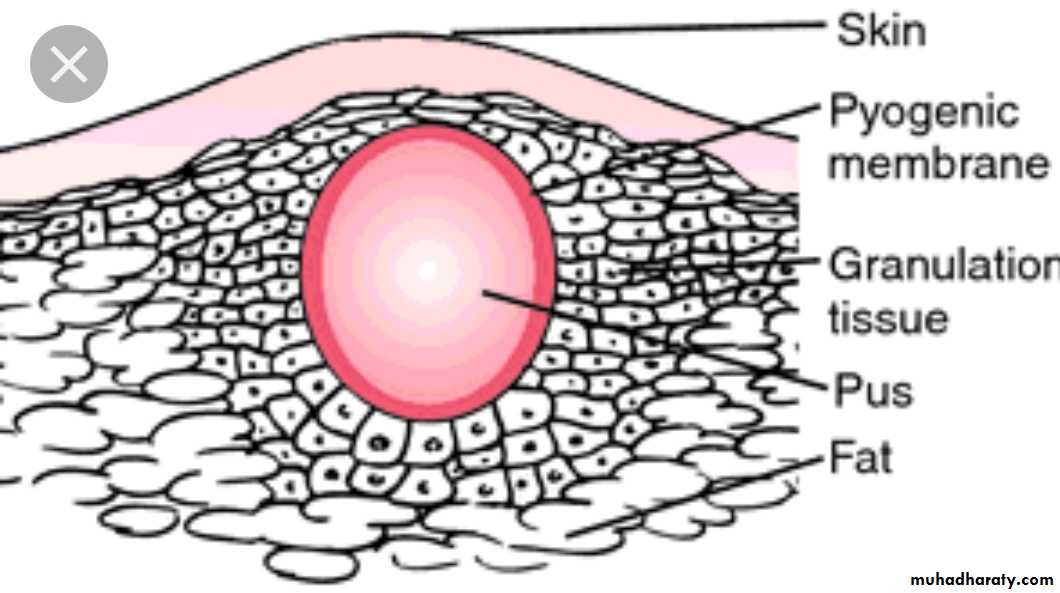
The caseous materials may be infiltrated by heavy neutrophilis result in cold abscess. It is called that because there are no signs of acute inflammation (hotness, redness, …..etc).
Healing when present is by progressive fibrosis
Organisms may remain viable in apparently healed lesions only to be reactivated years later if host resistance decreasesSpreadOf TB
Organisms may spread from the site of entry in the usual ways:
Locally: into adjacent tissues.
Lymphatic: to regional lymph nodes.
Natural passages e.g. (respiratory, alimentary, urinary & genital tract).Blood (veins & arteries) to produce either:
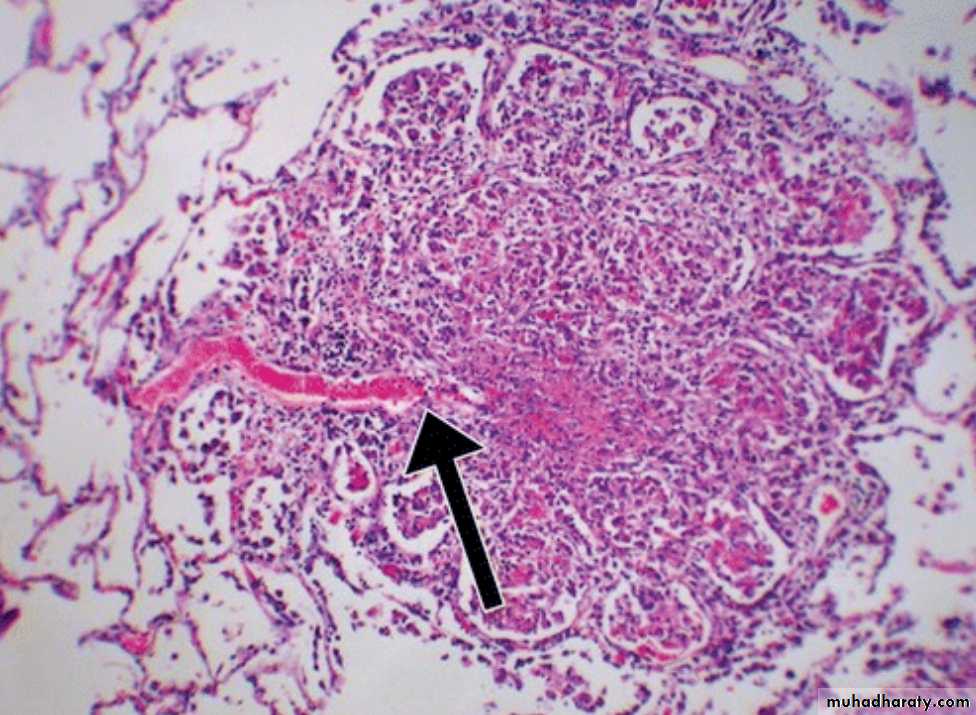
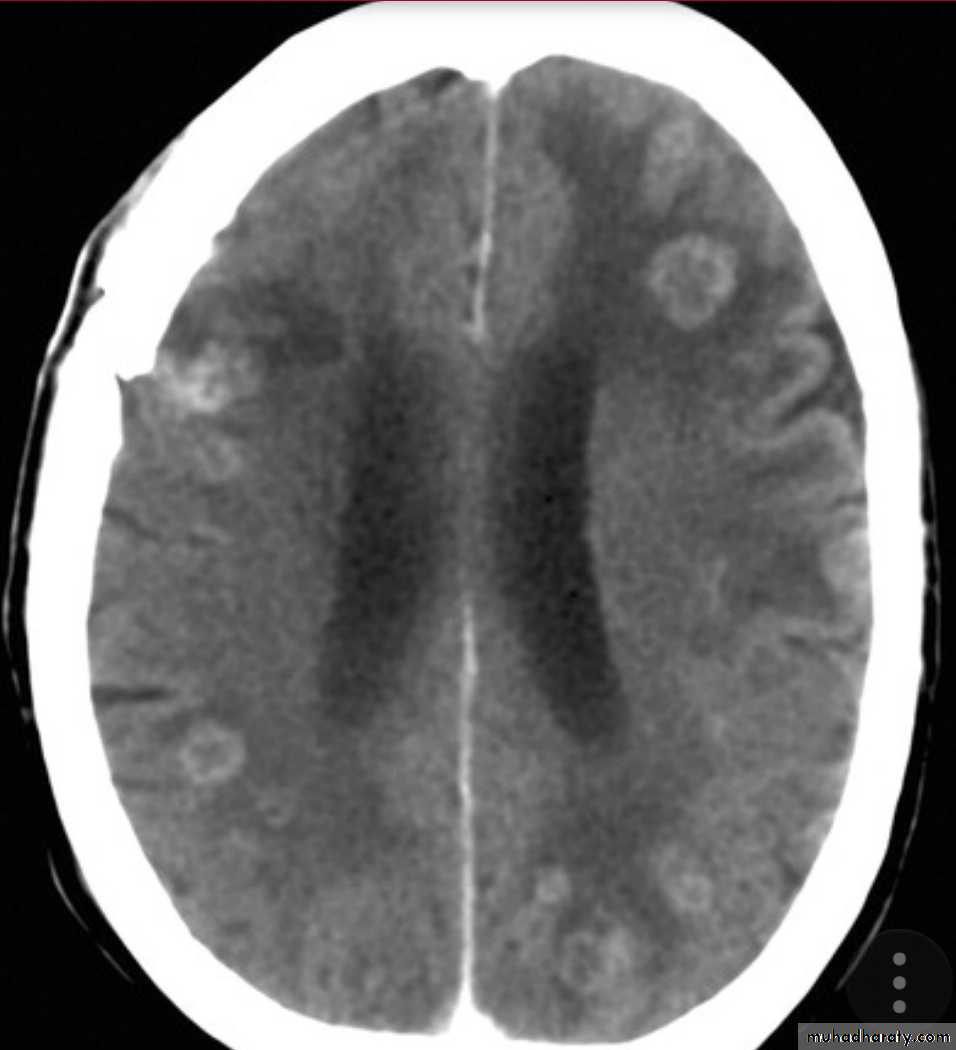
1- Miliary tuberculosis with multiple tubercles in numerous organs & tissues.2- Isolated metastatic organ lesions e.g., in kidney, bone, vertebra, joint & epididymis.
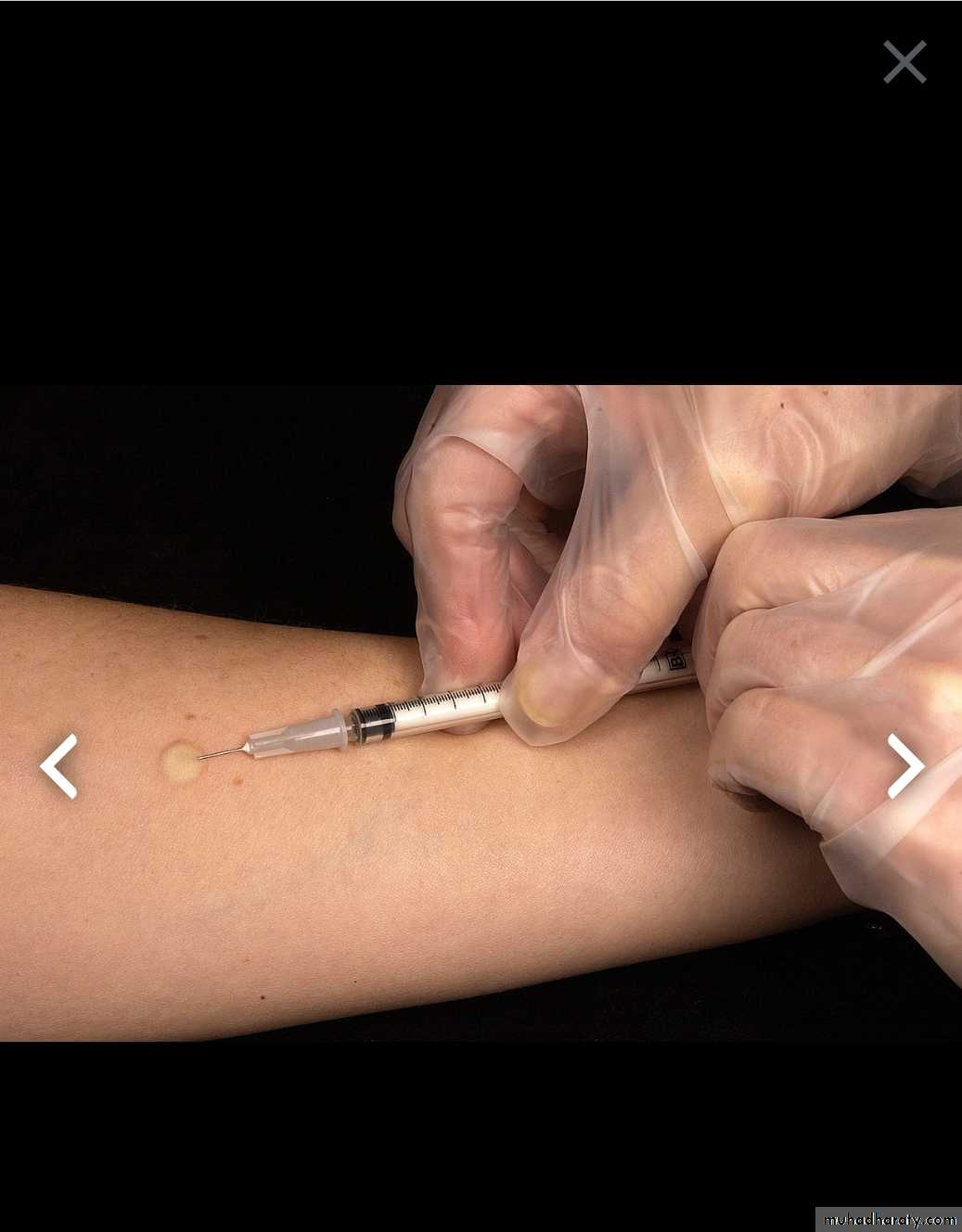
Immunity to TB can be induced artificially by intra dermal injection of attenuated mycobacterial strains of bovine type (BCG vaccine).
Skin test for TB (Mantoux test ) Tuberculin testPPD test (Purified Protein Derivative) test
It is an intradermal injection of tuberculoprotein . The test become positive in about 2-4 weeks after infection by TB bacilli
A positive skin test appear within 12-24 hours & peaks in 48- 72 hours after intradermal injection of tuberculoprotein as a 10 mm firm indurated nodule with surrounding redness.
A +ve result indicate hypersensitivity to TB (recent or old infection)
Primary tuberculosis
* It follows initial exposure to TB bacilli in non-immunized individuals of any age.
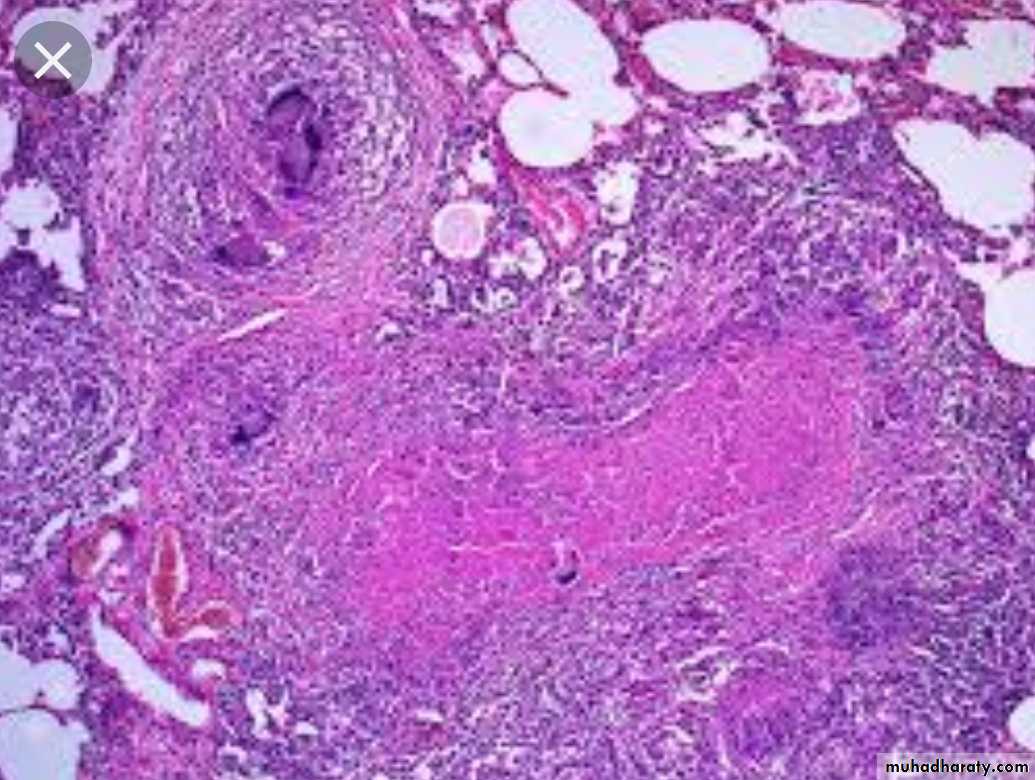
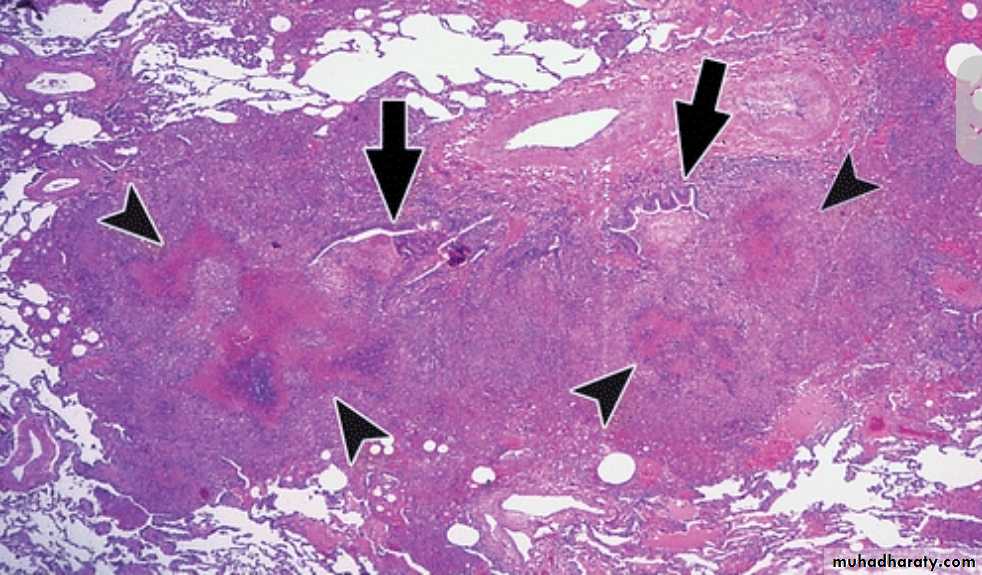
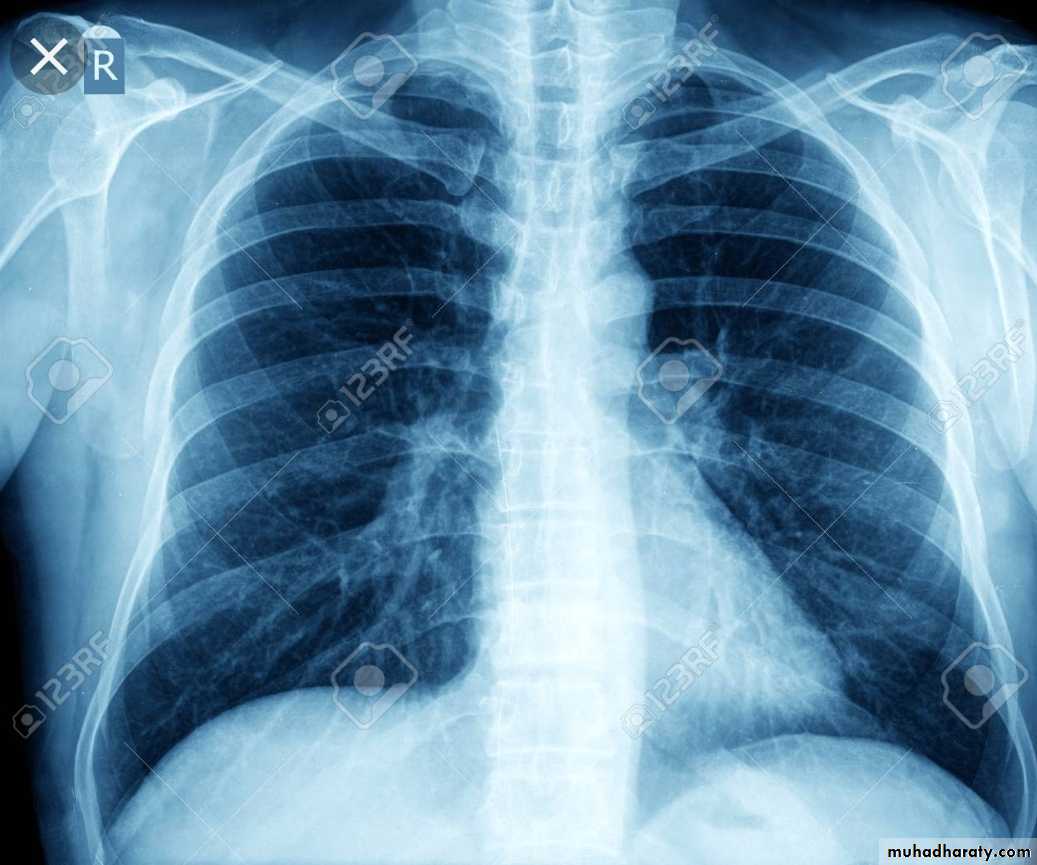
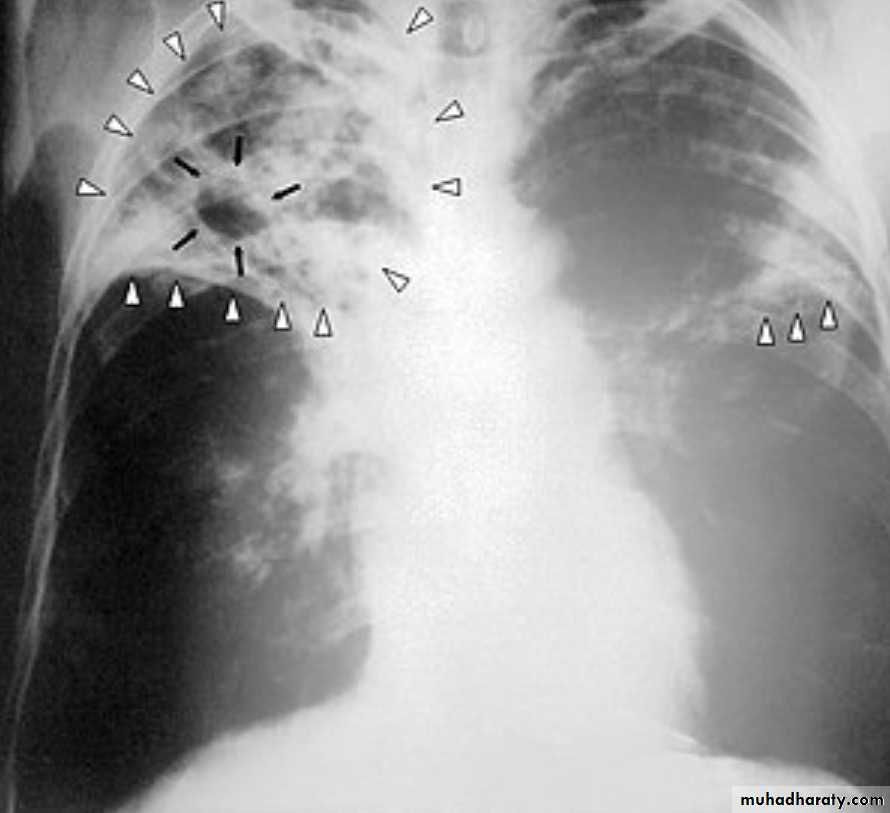
* Grossly: it forms a small sub pleural parenchymal lesion in the mid zone of the lung (Ghon focus) & spread to the hilar lymph nodes, both lesions are called Primary complex (Ghon complex).
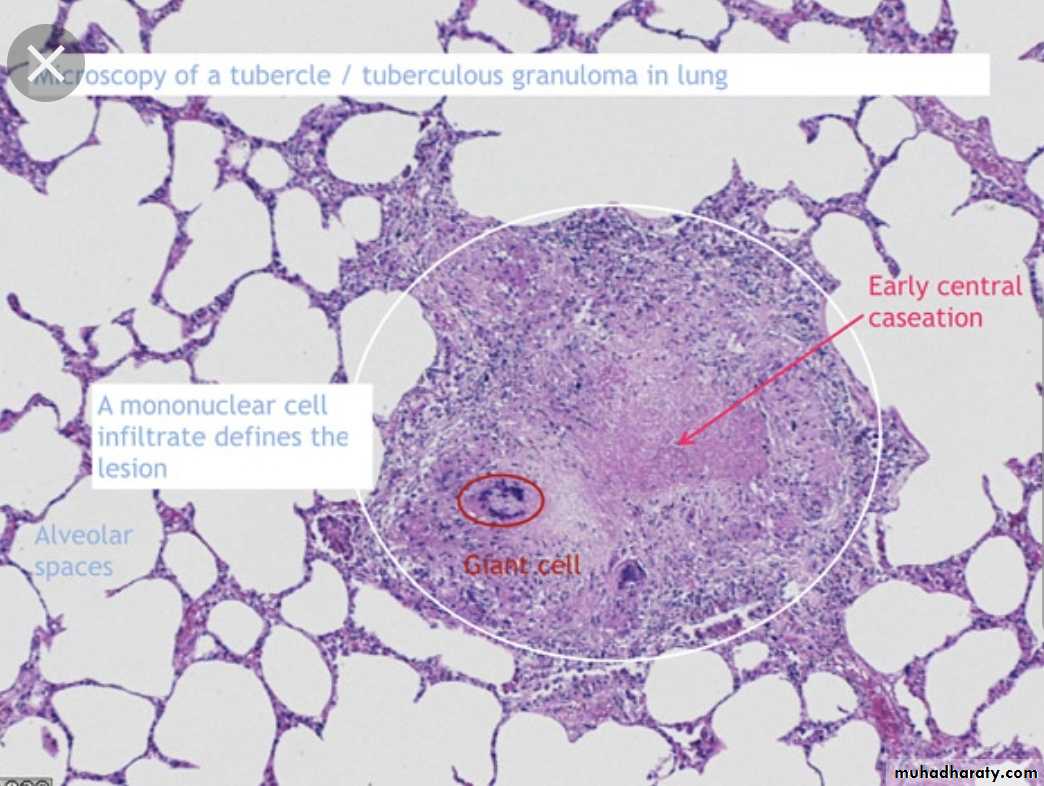
* Microscopically: consist of epitheloid granuloma with central necrosis.
Most of the cases (95%) after treatment heal by fibrosis
Some may enter into dormant state
Few may spread into the body forming progressive primary TB.Secondary TB
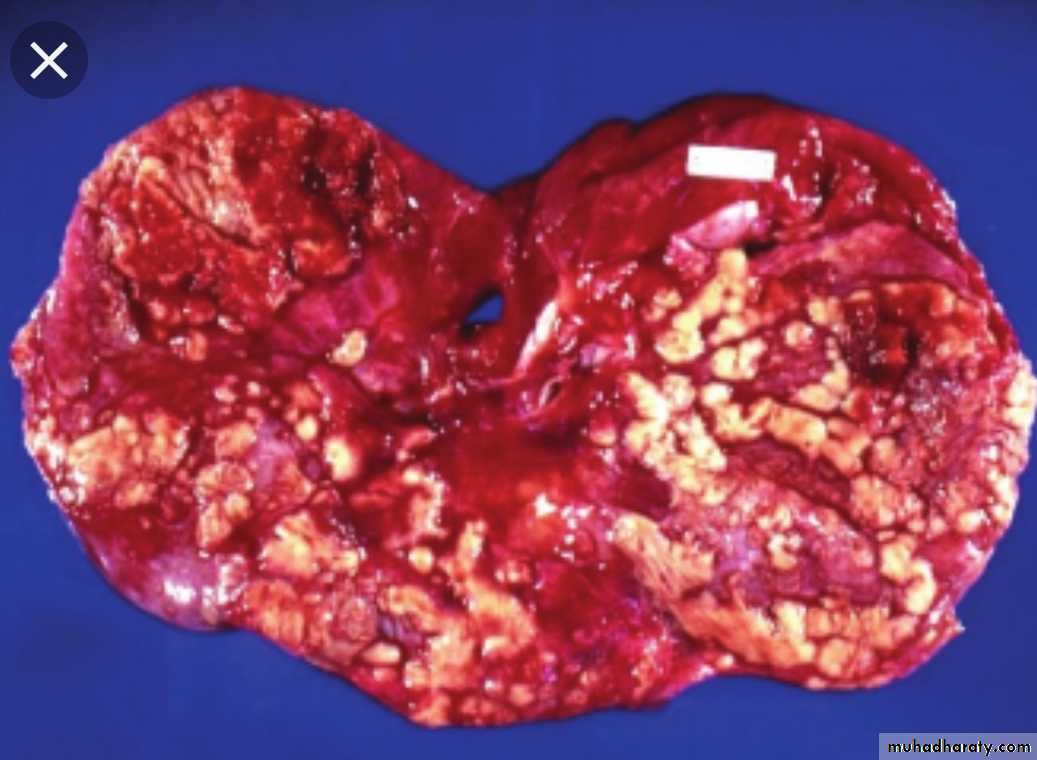
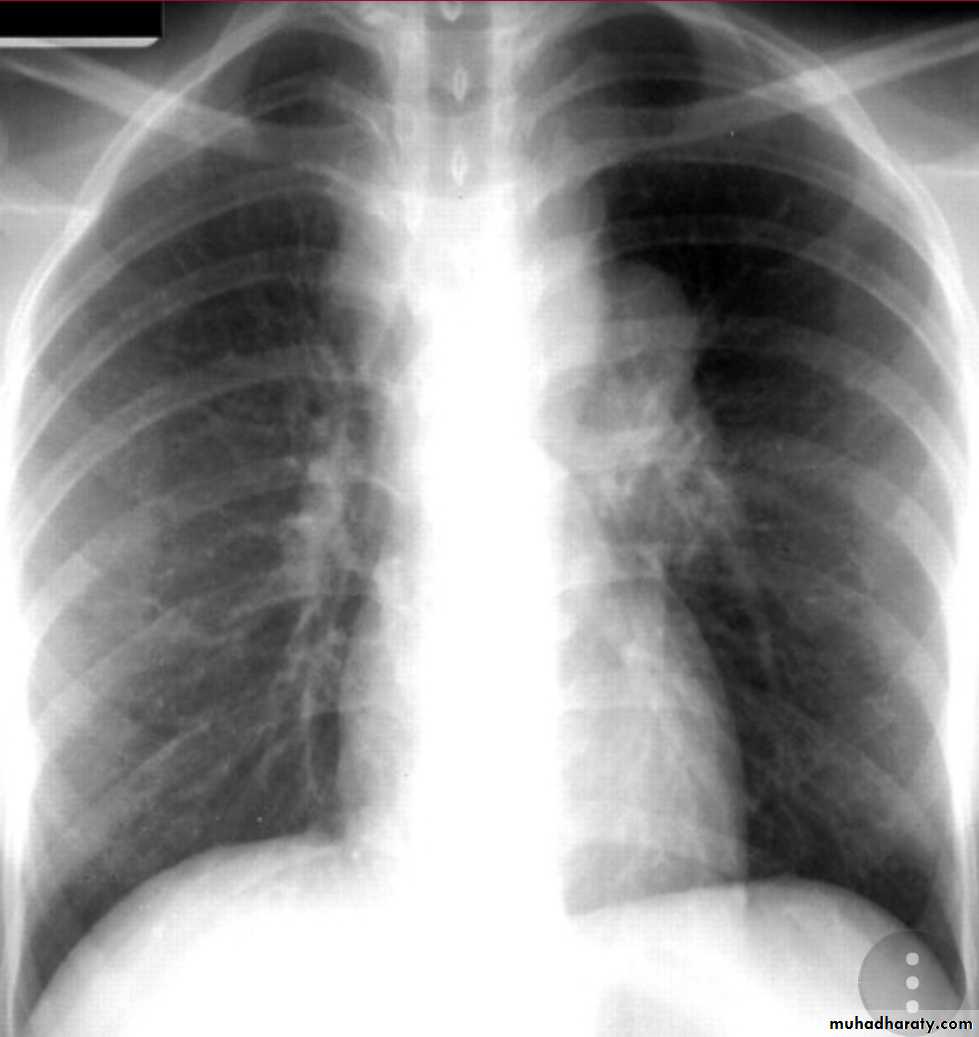
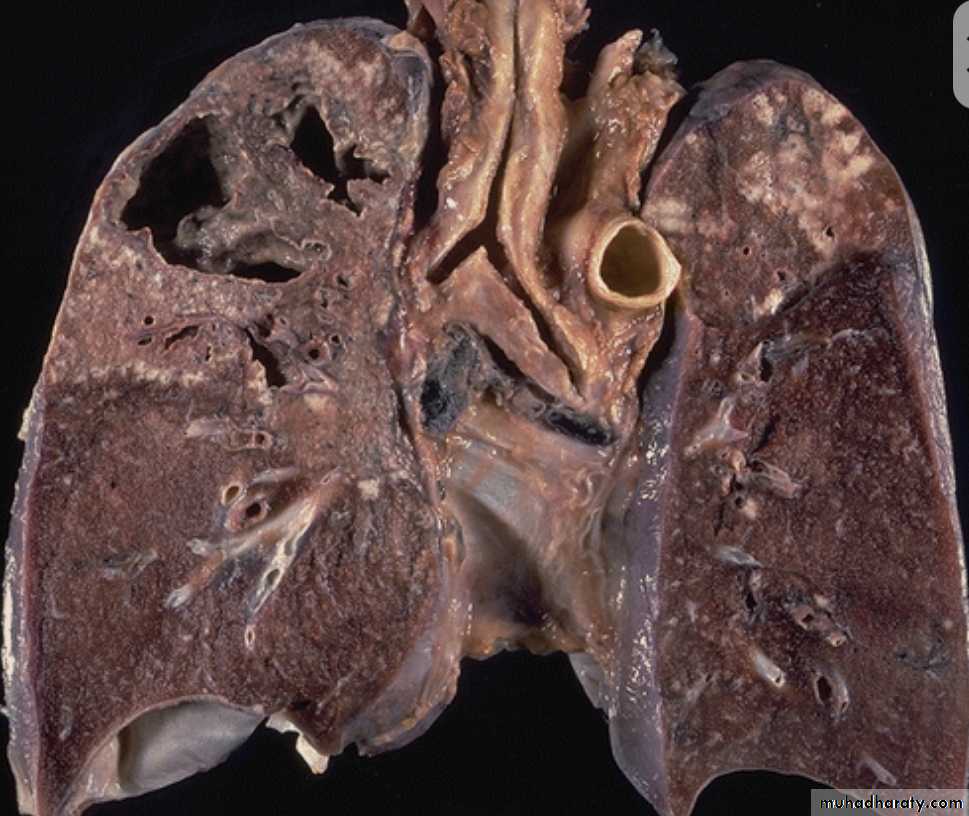
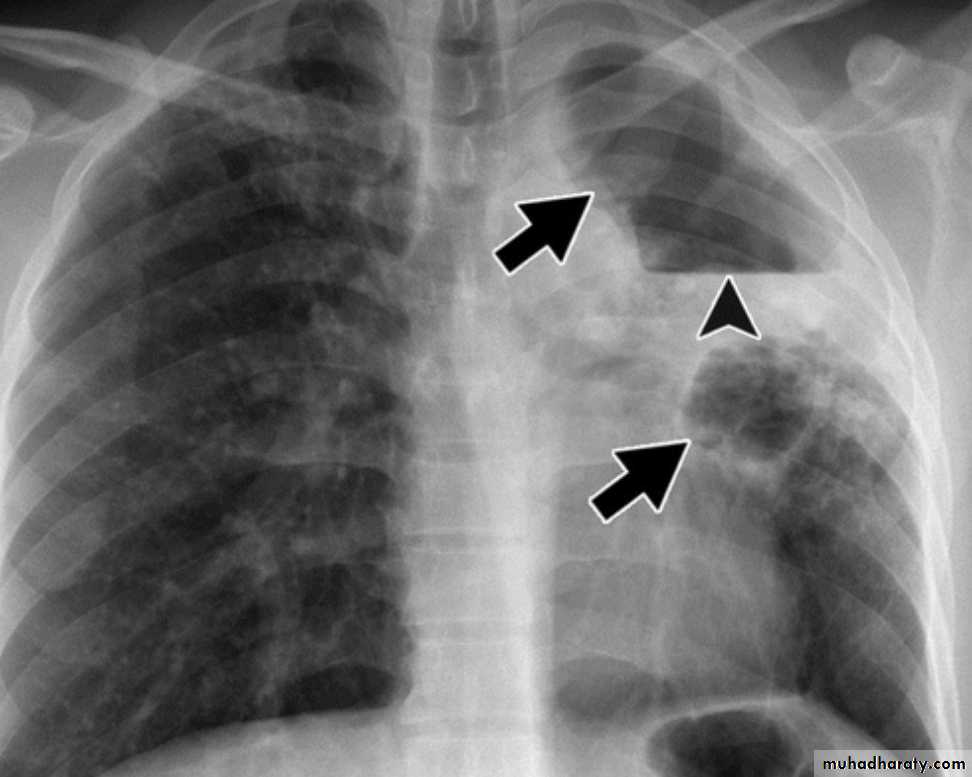
Either occurs as a reinfection by mycobacterium TB or reactivation of primary infection when there is impairment in the immunity of the patient.Grossly: usually occurs at the apex of the lung with minimal lymph node involvement. There is marked damage in the lung parenchyma with cavity formation
Microscopically: Epitheloid granulomas with central necrosis & cavity.
Healing by fibrosis or may spread forming progressive secondary TB
Progressive TBEither from primary or secondary TB.
* T.B. bacilli can be coughed into the larynx forming laryngeal TB.* or swallowed into the G.I.T causing intestinal TB.
* or enter through bronchial tree leading to tuberculous bronchopneumonia or spread into the pleural cavity leading to pleural effusion.
* or enter through the lymphatic channel or blood stream causing Miliary TB. or isolated organ TB.
Clinical Features
FeverWeight loss
Night sweating
Cough
Heamoptysis
Diagnosis
I- History.II- Clinical Examination.
III- Investigation include :
X- ray,
detection of the m.o in the specimen (sputum. urine, in biopsy) by the use of Ziehl-Neelsen staining & / or culture.
Biopsy of the infected tissue.
PCR amplification of T.B. bacilli DNA allows for even more rapid diagnosis.
* Positive skin test (Mantoux) indicates hypersensitivity to tuberculoprotein but NOT an active disease.
Treatment
Adequate & appropriate antituberculous drugs used for months.
Prevention
Immunization to Bacillus Calmette-Guerin (BCG vaccine) is recommended for all children in countries with high prevalence of TB.
LEPROSY(Hansen ,S Disease)
Causative agent: Mycobacterium lepraeThe disease affect skin & peripheral nerves
Infection require long period of close contact with patients.
Mode of infection is not clear, probably by inhalation.
Spread by blood stream
localize in peripheral nerves
Pathogenesis of leprosy
Lepra bacilli produce no exotoxin or endotoxin, the lesion is produced by :destructive granuloma
interferance with metabolism of schwann cells
Host response
Most of the patients get rid of the bacilli by natural resistance• If the host mounts T-cell immunity, tuberculoid leprosy with epitheloid granulomas occurs.
• If the host is anergic (lacking the normal immune response), lepromatous leprosy occurs
• Indeterminate leprosy: between 1 & 2.
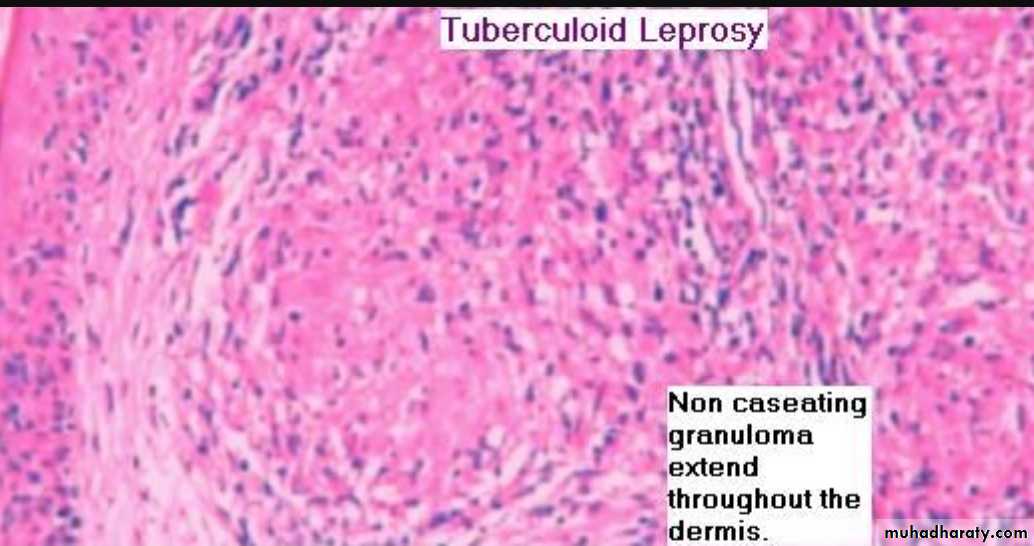
Tuberculoid leprosy
Localized skin lesion, consist of asymetrical anasthetic macule and palpable, lesions enlarge to become irregular in shape with indurated elevated hyperpigmented margins and depressed pale centers.Nerves are enclosed within the granulomatous reactions causing sometimes destruction of the nerve (small one) and this may be complicated by ulceration and deformity of the area supplied by the damaged nerve.
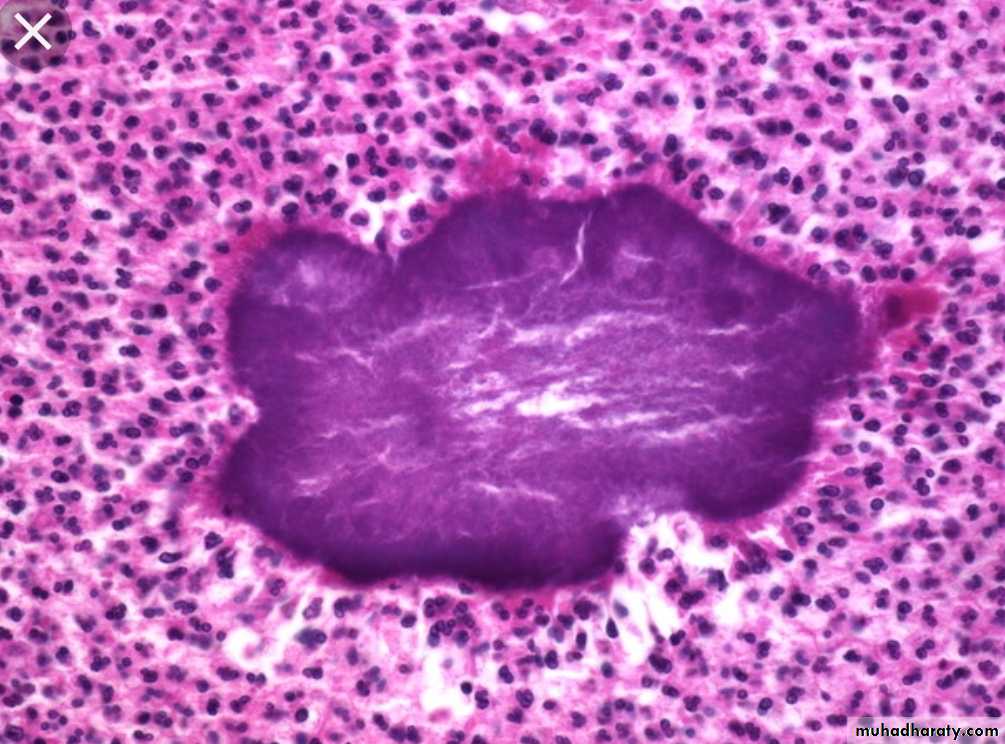
Microscopically: granulomatous reactions resembling tubercle containing epitheloid macrophage, giant cells, T-Lymphocytes (CD4 & CD8) & few surviving bacilli (paucibacillary disease)
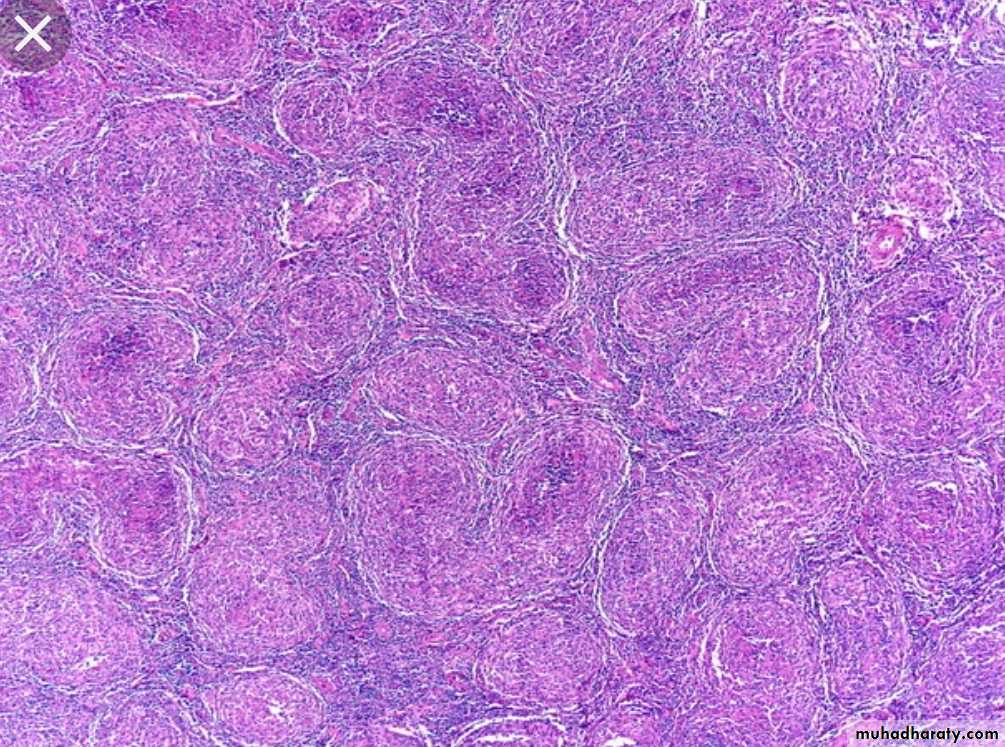
Lepromatous leprosy
Macular, papular, or nodular skin lesion seen in the skin of the face, ears, wrists, elbow & knees. Disease progression causes coalesce of the facial lesions (Leonine facies), the lesions are anesthetic or hypo-esthetic.Involvement of eye, URT down to the larynx , testis etc.
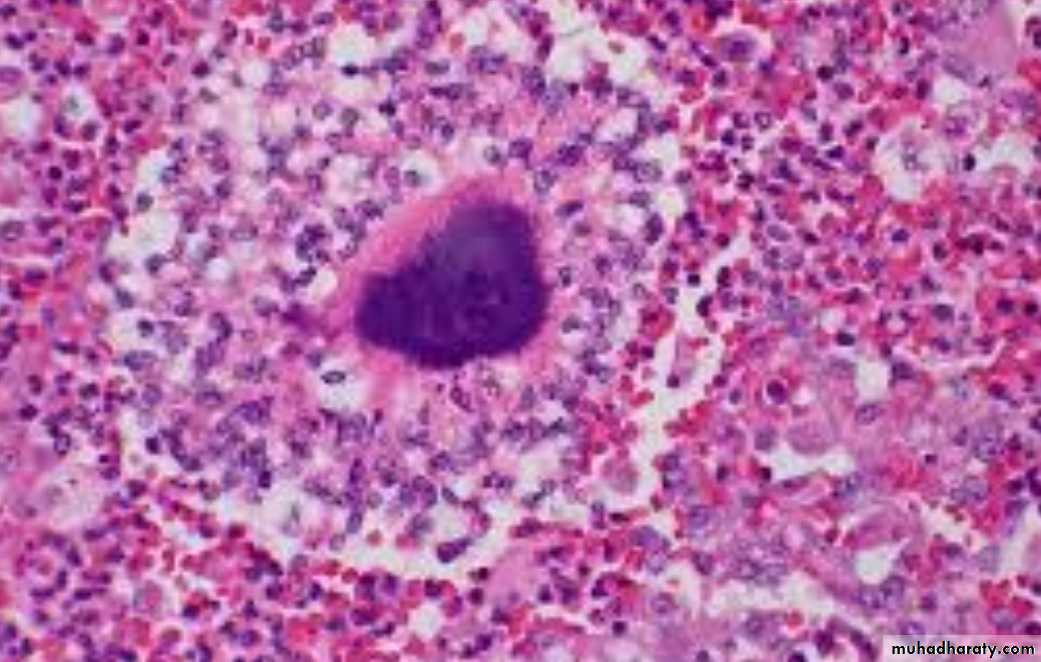
Peripheral nerves are involved symmetrically with trophic changes in hands and Feet.Microscopically: diffuse lesions containing foamy macrophages stuffed with large numbers of bacilli (lepra cells), lesions are also found in lymph nodes & in advanced cases in the liver spleen, testes (sterility) …
Amyloidosis may complicate lepromatous leprosy
Actinomycosis
Caused by Actinomyces israelliiVirtually anaerobic, gram-positive, long filamentous bacteria.
Closely related to mycobacteria with some similarity to fungi.It can be found as a commensal m.o. in the mouth , G.I.T., female genital tract. Only occasionally they invade the tissues it produce infection.
1- Cervicofacial lesion (70%).
2- Abdomial lesion (around iliocecal region or appendix) (15% ).3- Pulmonary lesion (10%).
4- Subcutaneous lesion (5%).
5- Gynecological infection in female with IUCD.
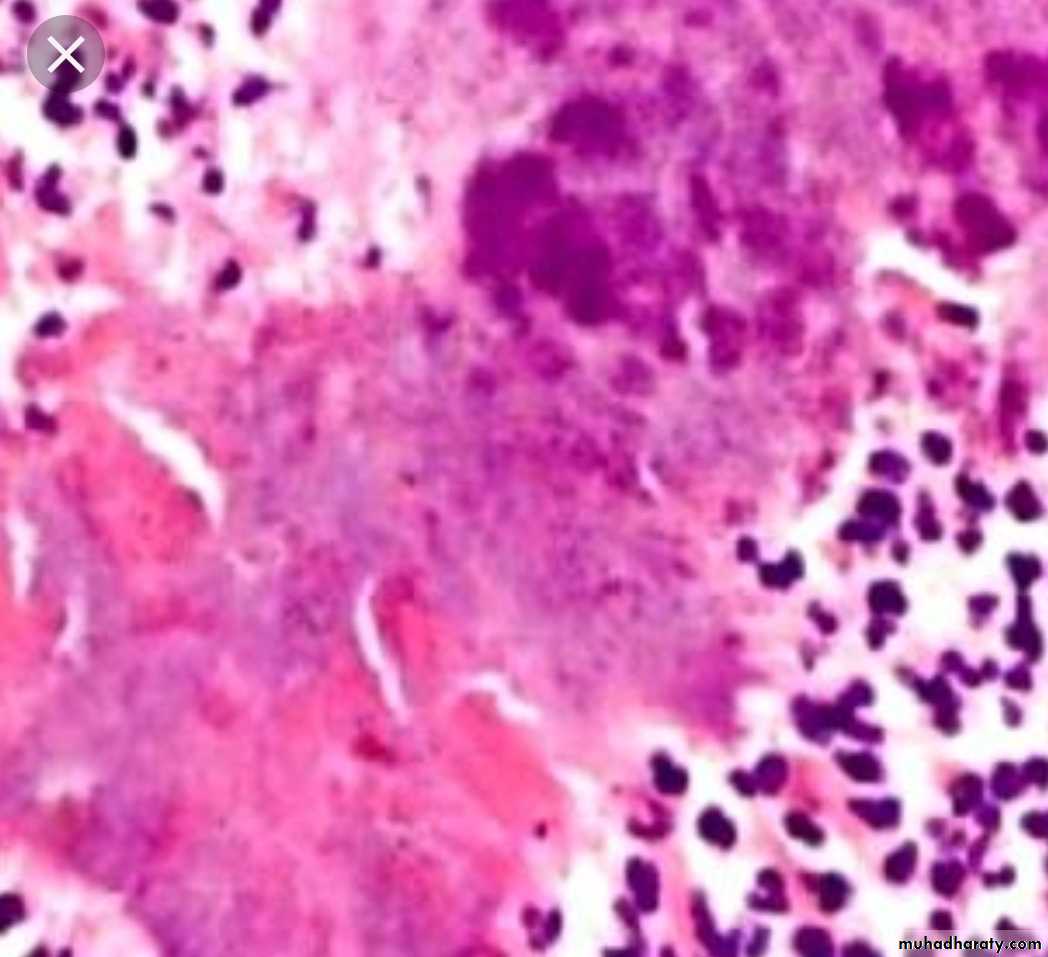
Pathology
Infection produces firm masses containing numerous abscesses ( honeycomb abscesses) bearing colonies as yellowish granules (sulfur granules) with sinuses & fistulae.