• 18-11-2018
Medical Parasitology3rd class
HaemoflagellatesTrypanosomiasis
• Dr. Abdul Rahman Dahham, PhD
• Department of Microbiology• College of Medicine
• Nineveh University
1
Kingdom: Animalia
Phylum: ProtozoaSubphylum: Mastigophora
Class: Zoomastigophora
Order: kinetoplastida
Family: Trypanosomatidae
Genus: Trypanosoma
Species:
Trypanosoma brucei gambiense
Trypanosoma brucei rhodesiense
Trypanosoma cruzi
2
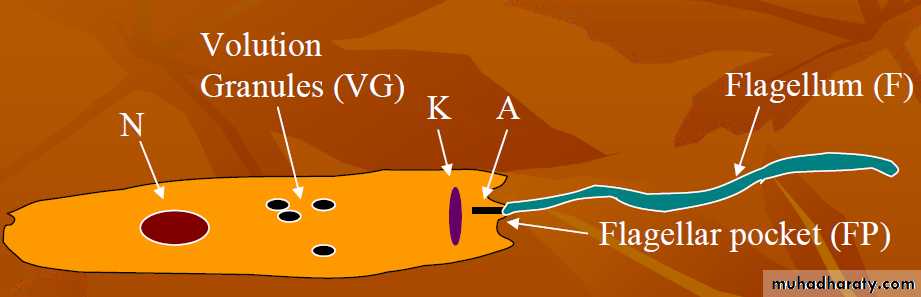
The family Trypanosomatidae is defined as having a single nucleus, a single flagellum, and a leaf-like or rounded body.
Members of this family are all parasitic, inhabiting the blood and (or) fixed tissues of all classes of vertebrates.
Family Trypanosomatidae:
3
tsetse fly
Reduviid (Triatomine) bug
Most species spend one stage of their life cycle in a vertebrate and another in a blood-sucking invertebrate, which functions as a vector.
4
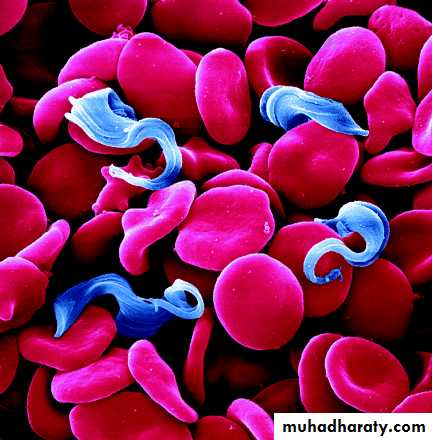
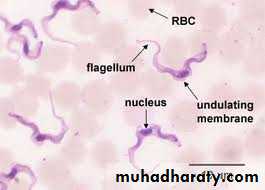
Human African trypanosomiasis, its a vector-borne parasitic disease, its actively motile, fusiform protozoa, flattened from side to side, the flagellum project from the anterior end, large single oval nucleus with central karyosome and long undulating membrane, transmitted to humans by tsetse fly (Glossina genus) bites which have acquired their infection from human beings or from animals harboring the human pathogenic parasites.
5
Trypanosomiasis “sleeping sickness”
Trypanosoma brucei gambiense
(West & central African Trypanosomiasis)Trypanosoma brucei rhodesiense
(East & south African Trypanosomiasis)Trypanosoma cruzi
(South American Trypanosomiasis)6
Three species pathogenic for humans:
Trypanosoma brucei gambiense (T.b.g.): found in west and central Africa.
Represents for over 95% of reported cases of sleeping sickness and causes a chronic infection.A person can be infected for months or even years without symptoms of the disease.
When symptoms emerge, the patient is already in an advanced disease (CNS is affected).7
Trypanosoma brucei rhodesiense (T.b.r.):
found in eastern and southern Africa.this form represents under 5% of reported cases causes an acute infection.
First signs and symptoms are observed a few months or weeks after infection. The disease develops rapidly and invades the central nervous system.8
Hosts
Definitive host: the main vertebrate host is man.Intermediate host: tsetse fly of the genus Glossina a blood sucking fly (largest fly of medical importance).
Habitat: Trypanosomes found in blood circulating system.
In Trypanosoma cruzi: pigs is final host but Cats ,dogs and reduviid bug are reservoir host.
Infective Stage:-Trypomastigote shape
9
Mode of transmission :-
The disease transmitted through the bite of an infected tsetse fly in Trypanosoma gambiense and Trypanosoma rhodesiense, reduviid in Trypanosoma cruzi.Mother-to-child infection: the trypanosome can cross the placenta and infect the fetus.
Accidental infections, occurred in laboratories due to pricks from contaminated needles.10
Trypanosoma cruzi
Chagas disease, or American trypanosomiasis, is caused by the parasite Trypanosoma cruzi.Infection is most commonly acquired through contact with the feces of an infected triatomine bug (or "kissing bug"), a blood-sucking insect that feeds on humans and animals.
11
12
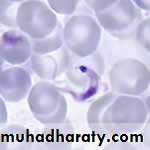
Morphology- exhibits a characteristic “C” shape with an undulating membrane and anteriorly extending flagellum; the amastigote is oval, averages 3 to 5 microns in diameter and contains a nucleus and rod-shaped kinetoplast.
Epidemiology of Trypanosoma cruzi
Chagas disease is endemic throughout much of Mexico, Central America, and South America where an estimated 8 to 11 million people are infected.The triatomine bug thrives under poor housing conditions (for example, mud walls, thatched roofs), so in endemic countries, people living in rural areas are at greatest risk for acquiring infection
13
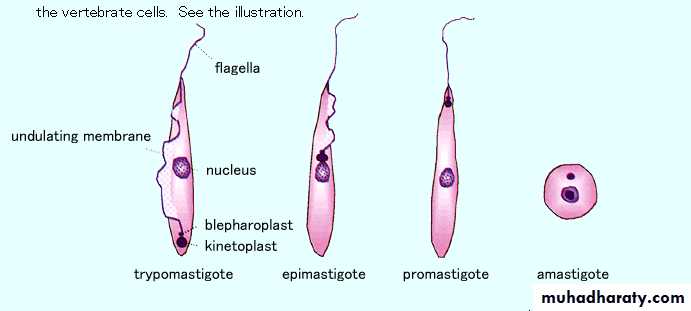
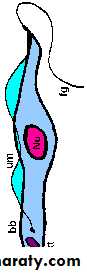
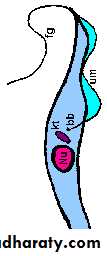
There are four morphological forms of clinical significance associated with the hemoflagellates:
Amastigote
PromastigoteEpimastigote
Trypomastigote
Hemoflagellates
morphologic forms14
• • 14
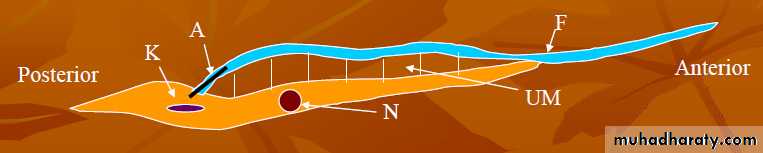
• Trypomastigote
• Epimastigote• Promastigote
• Amastigote
• FORM
15
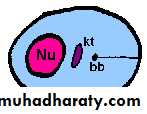
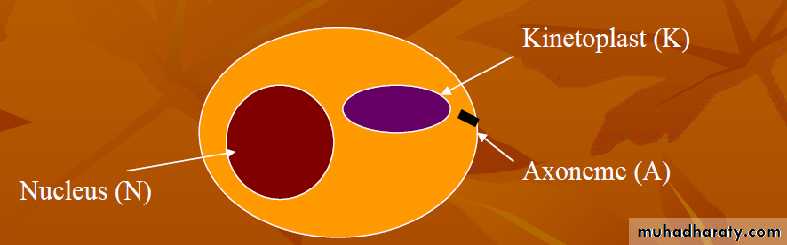
Amastigote
Slightly oval (2-3 X 3-4 microns).Axonemes are like microtubules that are associated with future flagellate motility.
Found inside reticulo-endothelial cells.
Multiplies by longitudinal binary fission.
There is generally a small zone between the K and A.
16
Promastigote
May have various shapes from short and fat to long and thin.Occasionally see volutin granules (VG) that represent waste products in the cytoplasm.
17
Epimastigote
Varies in length (12 -75 microns).K is always anterior to the nucleus.
F pulls the body through tissues.
Epimastigote has an undulating membrane where the promastigote doesn’t.
The undulating membrane causes the body to undulate.
18
Trypomastigote & Metacyclic Tryposmastigote
This is the Trypanosome.The K is posterior to the N vs the Epimastigote with the N posterior to the K.
Binary fission of the Promastigote, Epimastigote and Trymastigote are the same (K first followed by the A, F, the N and then the cell).
Metacyclic Tryposmastigote is the same as the tryposmastigote but is the infectious stage in the vector.
19
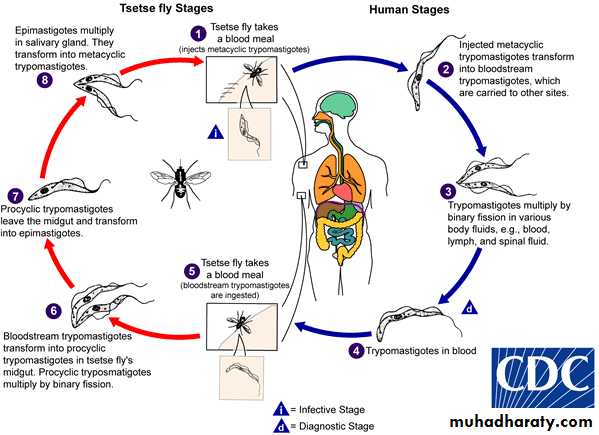
Development inside the vector
Two types of development in the insect vector: anterior station and posterior station.Anterior Station Development
Involves division of trypomastigotes in the midgut of the vector followed by migration of the parasite forward into the upper digestive tract (eg. salivary glands).Metacyclic trypomastigotes are then passed to the vertebrate host when the vector feeds.
20Anterior station development occurs with the salivarian trypanosomes (eg. Trypanosoma brucei gambiense) transmitted by vectors such as the tse-tse fly.
21
Posterior Station Development
Parasite development in the hindgut of the invertebrate vector.
In the hindgut the parasite transforms into epimastigotes and metacyclic trypomastigotes, which then move back through the digestive tract and are passed to the vertebrate host in the vector faeces.
This form occurs in the (Trypanosoma cruzi) transmitted by insects such as the reduvid kissing bugs.
22
Life cycle
2324
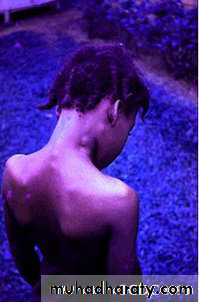
Clinical presentation
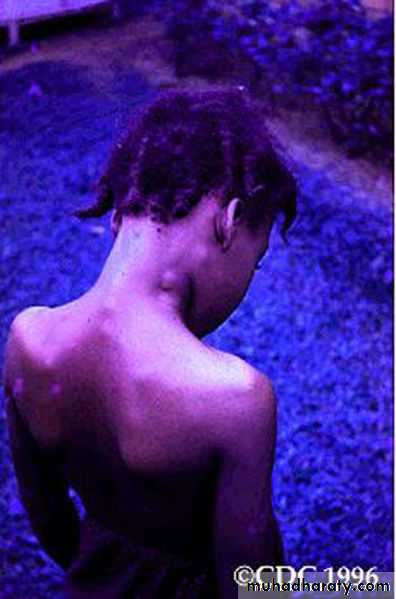
Stage 1 (early, or hemolymphatic stage)Indurate chancre at bite site.
Skin lesions (trypanids) in light-skinned patients.
Lymphadenopathy: Axillary and inguinal lymphadenopathy are more common in patients with East African trypanosomiasis.
Cervical lymphadenopathy is more common in patients with West African trypanosomiasis.
25The classic Winterbottom sign is clearly visible (ie, enlarged, nontender, mobile posterior cervical lymph node).
Fevers, tachycardia, irregular rash, edema, and weight loss.
Organomegaly, particularly splenomegaly (T brucei gambiense African trypanosomiasis)26
27
• chancre
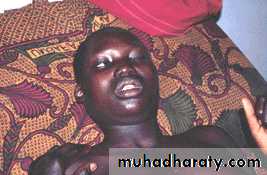
Stage 2 (late, or CNS stage)
Sleeping sickness stage because trypanosomes have crossed the blood-brain barrier.The CNS symptoms of West African trypanosomiasis have a slower onset of, ie, months to a year.
Personality changes, headaches and withdrawal from the environment.
28Simple tasks become harder to accomplish as individual experience nocturnal insomnia and daytime lethargy.
irritability, tremors, increased muscle rigidity and tonicity, occasional ataxia, and hemiparesis, but rarely overt meningeal signs. Stupor and coma (giving rise to the name sleeping sickness).
East African trypanosomiasis usually has a faster onset, ie, weeks to a month, and does not exhibit a clear distinction between the two stages.
29
• Winterbottom’s stage
stage CNS
30Laboratory Studies
In African trypanosomiasis (sleeping sickness), the most significant laboratory abnormalities include: anemia, hypergammaglobulinemia, elevated erythrocyte sedimentation rate (ESR), thrombocytopenia, hypoalbuminemia.A definitive diagnosis of infection requires actual detection of trypanosomes in blood, lymph nodes, CSF, skin chancre aspirates, or bone marrow.
31
Lymph node aspiration: is commonly used as a rapid test for trypanosomes. It requires immediate search for parasites because they are mobile for only 15-20 minutes. Used in T brucei gambiense trypanosomiasis.
Blood smear: A wet smear of unstained blood or Giemsa-stained thick smear (more sensitive) is used to evaluate for mobile trypanosomes, again for 15-20 minutes.
Wright and Leishman stains are inadequate. This technique is most sensitive in early stages of disease, when the number of circulating parasites is highest (≥5000/mL), particularly in T brucei rhodesiense trypanosomiasis.
32
Better assays are now available, including the hematocrit centrifugation technique for buffy coat examination and the miniature anion-exchange centrifugation technique (mAECT), which filters out the red cells but not the trypanosomes. This test can be used to detect parasitemia levels as low as 5 parasites/mL; the test can be repeated on subsequent days to increase the yield when results are negative.
33
Culture of CSF, blood, bone marrow aspirate, or tissue specimens can be performed in liquid media.
CT scanning and MRI of the head: reveal cerebral edema and white matter enhancement, respectively, in patients with late-stage African trypanosomiasis.
Other tests developed but not frequently used clinically include antibody detection in the CSF and intrathecal space (low sensitivity),
34
Serologic antibody detection: The standard serologic assay to diagnose West African trypanosomiasis is the card agglutination test for trypanosomiasis (CATT). The CATT can be conducted in the field without electricity, and results are available in only 10 minutes. It is highly sensitive (96%) but less specific because of cross-reactivity with animal trypanosomes.
Antigen detection tests based on enzyme-linked immunosorbent assay (ELISA) technology have been developed. They have shown inconsistent results and are not yet commercially available.
Polymerase chain reaction (PCR).
35Treatment
Stage I
Pentamidine: 7-10 injections for T. b. gambiense infection.
Side effects include: Painful injections with risk of hypotension and shock, pancreatic, renal or hepatic dysfunction; bone marrow suppression and polyneuropathy.
Suramin – multiple doses on varying days for T. b. rhodesiense infection.
Side effect include: renal impairment, peripheral neuropathy and bone marrow suppression.
36
• Stage II
• Melarsoprol (arsenical compound) slow IV injection. Side effects include: encephalopathy.• Eflornithine – infusion for 2 weeks every 6 hours. Drug is expensive and more effective against T. b. gambiense.
37